Abstract
Background: We studied completeness and timeliness of vaccination and determinants for low and delayed uptake in children born between 2008 and 2009 in Zhejiang province in eastern China.
Methods: We used data from a cross-sectional cluster survey conducted in 2011, which included 1146 children born from 1 Jan 2008 to 31 Dec 2009. Various vaccination history, social-demographic factors, attitude and satisfaction toward immunization from caregivers were collected by a standard questionnaire. We restricted to the third dose of HepB, PV, and DPT (HepB3, PV3, and DPT3) as outcome variables for completeness of vaccination and restricted to the first dose of HepB, PV, DPT, and MCV(HepB1, PV1, DPT1, and MCV1) as outcome variables for timeliness of vaccination. The χ2 test and logistic regression analysis were applied to identify the determinants of completeness and timeliness of vaccination. Survival analysis by the Kaplan–Meier method was performed to present the timeliness vaccination.
Results: Coverage for HepB1, HepB3, PV1, PV3, DPT1, DPT3, and MCV1 was 93.22%, 90.15%, 96.42%, 91.63%, 95.80%, 90.16%, and 92.70%, respectively. Timely vaccination occurred in 501/1146(43.72%) children for HepB1, 520/1146(45.38%) for PV1, 511/1146(44.59%) for DPT1, and 679/1146(59.25%) for MCV1. Completeness of specific vaccines was associated with mother’ age, immigration status, birth place of child, maternal education level, maternal occupation status, socio-economic development level of surveyed areas, satisfaction toward immunization service and distance of the house to immunization clinic. Timeliness of vaccination for specific vaccines was associated with mother’ age, maternal education level, immigration status, siblings, birth place, and distance of the house to immunization clinic.
Conclusion: Despite reasonably high vaccination coverage, we observed substantial vaccination delays. We found specific factors associated with low and/or delayed vaccine uptake. These findings can help to improve strategies such as Reaching Every District (RED), out-reach vaccination services and health education to reach children who remain inadequately protected.
Keywords: completeness, timeliness, coverage, vaccination, determinants, children
Introduction
Vaccination is regarded as one of the greatest public health achievements of the 20th century and one of the most cost-effective preventive services for children.1 Vaccination have substantially reduced the global burden of infectious diseases. The major contributor to this successful achievement is the Expanded Program of Immunization (EPI) of the World Health Organization (WHO) and Global Alliance Vaccine Initiative (GVAI),2 which was launched in 1974 as a worldwide alliance of collaborating nations and its goal was to expand immunization service and coverage.
The Chinese EPI was initiated since 1978, which has provided efforts to accommodate the needs of children at risk of vaccine-preventable diseases. Since 2008, the Chinese EPI stipulates that children aged <7 y should be vaccinated with the following vaccines3: a birth dose of Bacillus Calmette–Guerin (BCG), 4 doses of polio vaccine (PV), 4 doses of diphtheria-tetanus-pertussis (DTP), 3 doses of hepatitis B vaccine (HepB), 2 dose of measles containing vaccine (MCV), 2 dose of Japanese Encephalitis vaccine (JEV), one dose of hepatitis A vaccine (HepA), 2 dose of meningococcal polysaccharide vaccine-type A (MPV-A), one dose of MPV-type A and C(MPV-AC), and one dose of diphtheria-tetanus vaccine (DT). The target of immunization coverage rate is set at 90% for all the vaccines, which is required to reach herd immunity and interrupt community transmission for all vaccine preventable disease.4
The success of EPI dose not only depend on effective vaccination series, but also high immunization coverage.5 Estimate of immunization coverage that based on vaccination status of children in specific age or with specific demographic characteristic. For example, first dose of MCV(MCV1) is used to monitor progress toward the Millennium Development Goals and third dose of DPT coverage is used as an indicator of health system performance in other countries.6 Pinpointing the non-vaccination determinants is important for achieving the EPI target. The utilization of EPI service depends on numerous determinants such as provision of immunization service including accessibility of vaccination service, number of immunization staff, availability of vaccine and syringes, and cold chain.7,8 Once a child enters the vaccination system, various determinants are important for the initiation and completion such as caregivers’ education, experience with previous immunization service, adequate information on vaccination, immigration, socioeconomic status, and so on.9 Failure to be vaccinated on time would also increase the susceptible period of children, thus limiting the herd immunity. This problem was illustrated in a large measles epidemic in the USA during 1989–1991, where delayed vaccination of MCV was identified as one of the main cause.10 Clark11 analyzed coverage of vaccination in 45 low-income and middle-income countries(not including China), with a median of 60% for timely DPT3 and 74% for timely vaccination of MCV1. More recently, Akmatov12 analyzed timeliness of vaccination in 31 countries and showed substantial vaccination delays, with a median of 41% for timely DPT3 and 51% for timely vaccination of MCV1. However, previous studies have shown that vaccination coverage may be associated with factors mentioned above, but fewer studies have attempt to investigate determinants associated with timely vaccination and whether these are similar to those associated with coverage, especially on a sub-national level.
As a developed province in China, Zhejiang province is located in east China and has a total area of 104 141 Km2 with a population of 70 million residents. A review of surveillance data from the Zhejiang provincial Center for Disease Control and Prevention (CDC) found that the reported coverage of all vaccines was almost 99% every year since 2005.13 However, these figures did not always reflect the real situation and there were outbreaks of vaccine-preventable diseases such as measles in recent years.14 A study conducted by Zhejiang provincial CDC in Yiwu city in Zhejiang province showed that the estimate of timely vaccinated for MCV1 was only 47.5%, with one month after the recommended age.15 Obviously, there is still scope and the need to increase coverage and timeliness of vaccination.
The objective of this study was to estimate the immunization coverage in children aged 2–3 y in Zhejiang province. We also aimed to assess the timeliness of vaccination and identify the determinants for not being vaccinated and determinants for being vaccinated late with respect to different geographic, demographic, and socioeconomic status.
Results
A total of 1146 children were surveyed, of whom 609 were born in 2008. The socio-demographic characteristics and caregiver's attitude and satisfaction toward immunization were shown in Table 1.
Table 1. Socio-demographic characteristics and caregiver's attitude and satisfaction toward immunization of 1146 target children born between 2008 and 2009 in Zhejiang province in eastern China.
| Variable | No. | % |
|---|---|---|
| Socio-demographic characteristics | ||
| Child’s gender | ||
| Female | 560 | 48.87 |
| Male | 586 | 51.13 |
| Mother’s age (y) | ||
| <30 | 834 | 72.77 |
| ≥30 | 312 | 27.23 |
| Mother’s occupation | ||
| Housewife | 861 | 75.13 |
| Working | 285 | 24.87 |
| Mother’s education level | ||
| Under senior middle school | 673 | 58.73 |
| Senior middle school or above | 473 | 41.27 |
| Immigration status of child | ||
| Resident | 710 | 61.95 |
| Migrant | 436 | 38.05 |
| Siblings | ||
| 1 | 819 | 71.46 |
| ≥2 | 327 | 28.54 |
| Place of delivery | ||
| Home | 35 | 3.05 |
| Hospital | 1111 | 96.95 |
| Socio-economic developing level | ||
| Low | 384 | 33.51 |
| Middle | 380 | 33.16 |
| High | 382 | 33.33 |
| The caregiver's attitude and satisfaction toward immunization | ||
|---|---|---|
| Caregivers’ awareness of importance of immunization | ||
| Yes | 1137 | 99.21 |
| No | 9 | 0.78 |
| Satisfaction with immunization service | ||
| Yes | 941 | 82.11 |
| No | 205 | 17.89 |
| Distance of the house to immunization clinics | ||
| <5 km | 883 | 77.05 |
| ≥5 km | 263 | 22.95 |
Vaccination coverage
Of the 1146 children, 56 did not have any written vaccination certificate and were classified as not being vaccinated. Vaccination coverage was for 93.22% for HepB1, 90.15% for HepB3, 96.42% for PV1, 91.63% for PV3, 95.80% for DPT1, 90.16% for DPT3, and 92.70% for MCV1.
Determinants for completeness of vaccination
We found that child born in hospital was more likely to complete the series of vaccines. This determinant was 1.70-times higher for PV3, 1.86-times higher for DPT3 and 2.18-times higher for HepB3 (Table 2). Resident child was more likely to be vaccinated for PV3. Child whose mother had a higher education level, child from a higher socio-economic developing area and child whose mother was satisfied with clinical immunization service would have a better coverage for DTP3. Child with an elder mother, migrant child, child living ≥5 km from the nearest immunization clinic as well as child whose mother was unsatisfied with clinical immunization service would be more likely to drop the HepB3.
Table 2. Univariable and multivariable analysis on determinants for completeness of vaccination for PV3, DPT3 and HepB3 among children born between 2008 and 2009 in Zhejiang province in eastern China.
| Variable | Determinants for PV3 coverage | Determinants for DPT3 coverage | Determinants for HepB3 coverage | |||
|---|---|---|---|---|---|---|
| COR (95% CI) | AOR (95% CI) | COR (95% CI) | AOR (95% CI) | COR (95% CI) | AOR (95% CI) | |
| Mother’s age (y) | ||||||
| <30 | 1 | 1 | 1 | 1 | 1 | |
| ≥30 | 0.62 (0.47–0.87)* | 0.73 (0.52–1.21) | 0.79 (0.52–1.46) | 0.44 (0.23–0.63)* | 0.57 (0.22–0.82)# | |
| Maternal education level | ||||||
| < senior middle school | 1 | 1 | 1 | 1 | ||
| ≥ senior middle school | 0.89 (0.66–1.14) | 0.72 (0.51–0.93)* | 0.53 (0.29–0.75)# | 0.73 (0.37–2.24) | ||
| Immigration status of child | ||||||
| Resident | 1 | 1 | 1 | 1 | 1 | 1 |
| Migrant | 0.21 (0.13–0.76)* | 0.33 (0.20–0.68)# | 0.49 (0.28–0.84) | 0.66 (0.41–1.92) | 0.41 (0.32–0.75) | 0.52 (0.39–0.86)# |
| Mother’s occupation | ||||||
| Housewife | 1 | 1 | 1 | 1 | 1 | |
| Working | 0.45 (0.29–0.86)* | 0.62 (0.37–0.91)# | 0.66 (0.43–1.68) | 0.58 (0.33–0.89)* | 0.68 (0.41–1.29) | |
| Place of delivery | ||||||
| Home | 1 | 1 | 1 | 1 | 1 | 1 |
| Hospital | 3.12 (1.66–6.21)* | 1.70 (1.26–3.52)# | 1.55 (0.82–3.36) | 1.86 (1.27–3.93)# | 2.63 (1.13–4.30)* | 2.18 (1.72–3.55)# |
| Socio-economic developing level | ||||||
| Low | 1 | 1 | 1 | 1 | 1 | 1 |
| Middle | 2.08 (0.53–7.97) | 1.02 (0.61–2.15) | 1.25 (1.02–4.83)* | 1.04 (0.77–2.03) | ||
| High | 2.49 (1.10–4.55)* | 1.08 (0.66–3.07) | 1.93 (1.04–4.22)* | 1.84 (1.10–3.07)# | 3.32 (1.98–7.44)* | 1.57 (1.14–2.52) |
| Satisfaction with immunization service | ||||||
| Yes | 1 | 1 | 1 | 1 | 1 | |
| No | 0.57 (0.43–1.73) | 0.46 (0.22–0.94)* | 0.64 (0.49–0.94)# | 0.42 (0.26–0.87)* | 0.59 (0.39–0.86)# | |
| Distance of the house to immunization clinics | ||||||
| <5 km | 1 | 1 | 1 | 1 | ||
| ≥5 km | 0.79 (0.42–2.77)* | 1.02 (0.78–3.65) | 0.68 (0.35–0.72)* | 0.73 (0.25–0.81)# | ||
COR, crude OR; AOR, Adjusted OR. *P< 0.10, #P< 0.05.
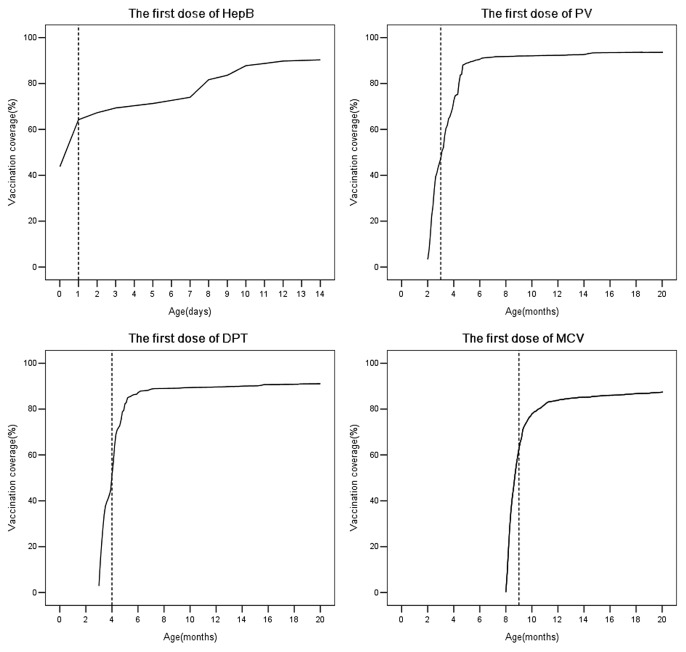
Timeliness of vaccination
The timeliness of vaccination for 4 interested vaccines was shown in Figure 1. We plotted a dash line on each figure according to the age above which vaccination was considered as delayed. Timely HepB1 vaccination was found in 501 of 1146 children (43.72%), with a median at vaccination of 1 d (95%CI: 0.86–1.14). Timely PV1 vaccination was found in 520 of 1146 children (45.38%), with a median at vaccination of 3.1 mo (95%CI: 2.99–3.20). Timely DPT1 vaccination was found in 511 of 1146 children (44.59%), with a median at vaccination of 4 mo (95%CI: 3.95–4.05). Likewise, 679 children (59.25%) had timely MCV1 vaccination and the median at vaccination was 8.7 mo (95%CI: 8.64–8.76).
Figure 1. Timeliness of the first dose of HepB, the first dose of PV, the first dose of DPT, the first dose of MCV among children born between 2008 and 2009 living in Zhejiang province in eastern China. The vertical lines correspond to the age after which children were assumed to have been vaccinated late (i.e., >1 d after birth for the first dose of HepB and >1 mo after the recommended age for other vaccines).
Determinants for timeliness of vaccination
We found that child with an elder mother was more likely to be vaccinated later for HepB1. Migrant child or child living ≥5 km from the nearest immunization clinic was more likely to be vaccinated later for PV1. Family having more than one child or child living ≥5 km from the nearest immunization clinic was associated with delayed vaccination for DPT1. Child with elder mother, migrant child or child living ≥5 km from the nearest immunization clinic was associated with delayed vaccination for MCV1 (Table 3).
Table 3. Univariable and multivariable analysis on determinants for timely vaccination for HepB1, PV1, DPT1 and MCV1 among children born between 2008 and 2009 in Zhejiang province in eastern China.
| Variable | Determinants for timely HepB1 coverage | Determinants for timely PV1 coverage | Determinants for timely DPT1 coverage | Determinants for timely MCV1 coverage | ||||
|---|---|---|---|---|---|---|---|---|
| COR (95% CI) | AOR 95% CI) | COR (95% CI) | AOR (95% CI) | COR (95% CI) | AOR (95% CI) | COR (95% CI) | AOR (95% CI) | |
| Mother’s age (y) | ||||||||
| <30 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| ≥30 | 0.47 (0.26–0.92)* | 0.55(0.28-0.84)# | 0.58 (0.28–3.22) | 0.54 (0.34–2.22) | 0.42 (0.28–0.93)* | 0.72 (0.60–0.87)# | ||
| Mother’s education level | ||||||||
| < senior middle school | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| ≥ senior middle school | 1.26 (0.63–3.75)* | 2.39 (0.87–4.28) | 1.52 (0.59–4.49) | 3.48 (2.25–10.71)* | 1.57 (1.33–7.84)# | 2.52 (1.34–5.87)* | 1.32 (1.06–4.14)# | |
| Immigration status of child | ||||||||
| Resident | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Migrant | 0.61 (0.42–0.86)* | 0.83 (0.67–2.62) | 0.55 (0.34–0.88) | 0.74 (0.57–0.92)# | 0.68 (0.38–1.33) | 0.59 (0.27–0.89)* | 0.71 (0.44–0.93)# | |
| Siblings | ||||||||
| 1 | 1 | 1 | 1 | 1 | 1 | 1 | ||
| ≥2 | 0.84 (0.59–3.72) | 0.63 (0.39–0.82)* | 0.72 (0.52–0.87)# | 0.57 (0.19–0.92)* | 0.69 (0.32–0.84)# | 0.73 (0.37–2.19) | ||
| Place of delivery | ||||||||
| Home | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| Hospital | 7.35 (2.06–18.69)* | 6.51 (3.77–11.04)# | 3.49 (1.96–6.13)* | 2.82 (1.39–5.09)# | 1.58 (1.03–3.63)* | 1.17 (0.83–3.22) | 1.84 (0.84–4.57) | |
| Distance of the house to immunization clinics | ||||||||
| <5 km | 1 | 1 | 1 | 1 | 1 | 1 | 1 | |
| ≥5 km | 0.92 (0.46–2.07) | 0.60 (0.45–0.79)* | 0.69 (0.51–0.92)# | 0.64 (0.52–0.87)* | 0.75 (0.52–0.96)# | 0.67 (0.56–0.80)* | 0.71 (0.58–0.91)# | |
COR, crude OR; AOR, Adjusted OR. *P< 0.10, #P< 0.05.
Discussion
Vaccination coverage was reasonably high and achieved the EPI’ s coverage goal of 90% for each vaccine in our study, but we found that almost half of the children were not vaccinated timely. These results were similar with previous studies from both developed or developing countries11,12,16,17 where vaccination delays were found despite reasonable high immunization coverage, calling for timeliness of vaccination to be considered as another indicator of the performance of EPI.14
In this study, we found migrant children were more likely not to be fully immunized and were more likely to have delayed vaccination, and it seemed that migrant children never replicated the patterns of utilization of immunization service among residents. The reasons need exploration in further research, but we attributed high missed vaccination rate and delayed vaccination to problems in vulnerability of migrants in the new sociocultural environment, demand for public health service, satisfaction, and the capacity of providing those services.
Our results showed that distance of the house to immunization clinic was associated with completeness of HepB and timeliness of all 3 vaccines except HepB1. Similar results had been found in reports from southeast Asia and Africa.18-20 Although most vaccines are provided free of charge, indirect costs related to travel may account for difference in vaccine uptake and timely vaccination between those living closer and further away from an immunization clinic.21 Additionally, going to the immunization clinic inconveniently may inhabit the household make the journey to the immunization clinic repeatedly. Since the time to immunization clinic from house is related to not only the availability of transportation but also the distance, further study is still needed to investigate the association between vaccination status and other determinants including precise information on distance, time to the immunization clinic, and availability of transportation.
There were other determinants for completeness of vaccination. First, maternal education was associated with vaccination coverage of DPT3. The possible reason for this was that education level may influence mother’s awareness and capacity to seek and take advantage of public health service including vaccination. However, there were still controversies from previous reports, for example, Koumare22 reported no difference associated with maternal literacy and vaccination coverage. Further efforts are needed to identify whether mothers’ education level was associated with children’s vaccination status and its impact factors. Second, birth delivery at hospital was associated with completeness for all 3 vaccines. The explanation associated with those may be that, mothers who gave birth at hospital were closer to the health service23 and may have a better utilization of immunization service and over 95% of the surveyed children were delivered at hospital in our study. Third, we found that child from a relative lower socio-economic development area tended to experience more drop out for DPT3. Given that our research was implemented in a developed area in east China, difference among lowest and highest socio-economic development was not significant than in studies where wealth was found to be a key determinant of vaccination status.24 Nevertheless, our research showed that even in a province that could be considered as uniformly developed, small difference in socio-economic development were related to the completeness of immunization. Fourth, having a mother with a job was significant associated with coverage for PV3. We assumed that they had not enough time to spare for primary healthcare and were less aware of the information on vaccination. Third, we found that child whose mother was unsatisfied with clinical immunization service tended to experience more drop out for DPT3 and HepB3. We assumed that the unpleasant experiences for previous immunization service would discourage parents from receiving immunization service.
There were several determinants for timeliness of vaccination. First, mother’s age was associated with timeliness vaccination of HepB3 and MCV1 in our study. This was indicated by the previous studies and one study from Africa showed that there was a linear trend for full vaccination increases with maternal age.25 The younger mother would possibly have a better utilization of medical care such as antenatal care and post-natal visits, which may lead to an increased coverage rate and the probability of timeliness of vaccination. Second, birth delivery at hospital was associated with timeliness for HepB1 in our study. Since the HepB1 is stipulated to be given within 24 h after birth in China, the timeliness for HepB1 could also be improved if the child was delivered in hospital. Third, having more than one child was a significant demographic factor for delayed DPT1 in our study. Several studies revealed that parental attention can be diverted by the presence of multiple children.26,27
We did not find any difference in completeness or timelines of vaccination by gender of the child and caregivers’ awareness of immunization. The gender ratio was 1.05:1 in our study, and the gender ratio of Zhejiang province was 1.04:1 in 2008 and 1.07:1 in 2009.28,29 The result showed that there was no gender difference in vaccinations. It was worth to emphasize that positive attitude of vaccination was not associated with vaccination coverage and timeliness of vaccination, as has been found in previous studies.30 This result may be attribute to the homogeneity of target population. In our research, there were over 99% of surveyed parents thought that vaccination was important.
There were several advantages in our study. First, our results were collected through a provincial wider investigation and multiple cluster sampling method was adopted. Geographically, this research covered a wide portion of Zhejiang province. Second, only written vaccination records were applied to avoid inaccuracies or recall bias. Immunization cards kept by caregivers or the local immunization clinics were the only resource of vaccination information in our research. Parent-linked or provider-validated immunization status measures was considered as the gold standard for measuring vaccination status in previous study.31 However, our study has several limitations. First, we did not analyze determinants associated with the providers, in particular determinants such as vaccines storage and delivery, as well as attitude of the immunization staff, all of which may affect vaccination coverage. Second, we did not collect the data on MCV vaccination records of target children during 2008–2009 as MCV campaigns were performed in Zhejiang province in the same time and this may impact our estimates of coverage and timeliness of routine MCV vaccination. Third, this was a cross-sectional research, hence, it was hard to generate cause-effect relationship of vaccination status and determinants due to the study’s design.
In conclusion, our research revealed that there were still a large proportion of children vaccinated later than the recommended age, which would increase their risk of infection and cause a negatively influence on herd immunity. Our findings suggest that the timeliness of vaccination should be considered as another important indicator of EPI performance assessment. Despite the decentralization of Zhejiang provincial immunization service system, both vaccine coverage and timeliness of vaccination could be improved further by strengthened Reaching Every District (RED) strategy32 targeted vaccination to children who remain hard to reach and out-reach vaccination services (like remind/recall services). Furthermore, health education needs to be emphasized to encourage the parents to participate in the immunization service for their children.
Materials and Methods
Target children
Target population in this study were the children born from 1 Jan 2008 to 31 Dec 2009 and lived in the surveyed areas at the time of the investigation (from 10 to 20 November, 2011), all of whom were older than 12 mo. In our study, migrant was defined as the person who lived in a county other than their hometown (even if from the same province) but had no local registration of the current living place. Migrant children who were also included if they had lived in the surveyed areas continuously for 3 mo or more at the time they were interviewed.
Study area
The survey was performed in 18 counties (total of 90 counties in Zhejiang Province), and all 215 towns within the 18 counties served as clusters. These counties were divided into 3 socioeconomic strata (high, middle, and low) by Gross Domestic Product (GDP) per capita level according to the data from Zhejiang Provincial Bureau of Statistics,33 with each stratum including 6 counties. Jianggan, Xihu, Jiangbei, Yinzhou, Shaoxing, Jiaojiang county were classified as high socioeconomic development areas for GDP per capita ≥12 000 USD; Longwan, Xiuzhou, Tongxiang, Deqing, Yuecheng, Yongkang county were classified as middle socioeconomic development areas for GDP per capita between 10 000 to 12 000 USD; Anji, Pujiang, Qujiang, Kaihua, Liandu, Qingtian county were classified as low socioeconomic development areas for GDP per capita 8000 to 10 000 USD.
Study design and sampling method
The sampling method was based on the WHO-advocated cluster sampling technique.34 The immunization coverage rate of target children was assumed to be 85% according to the pilot survey done before and the desired precision was 3%. We assumed a design effect of 2 and obtained required number of surveyed children per cluster for variable numbers of clusters through the table recommended by the WHO manual (Table S1). Twenty-one children per cluster for 54 clusters were finally determined as our sample size, giving a total of 1134 target children (including both residents and migrant children). The main reason for the sample size per each cluster and the cluster number was due to all clusters could be divided equally into each counties and possible homogeneity of immunization coverage of children within a cluster but heterogeneity across different clusters, we selected as many as possible clusters as the representatives of all 215 towns.
We used a two-stage random sampling method. In the first stage, the list of 215 towns of 18 counties was obtained. Three towns per county were sampled with Probability Proportionate to Size (PPS) of target children. In the second stage, interviewers got the household list from the community authorities and randomly selected one household as the first family to be interviewed and continued by choosing each subsequent household located to the right of the previous one until 21 eligible children had been interviewed. Only one child per household was selected to avoid clustering. When 2 or more eligible children were in the same household, the youngest child was selected.
Data collection
EPI staff of Zhejiang provincial CDC were selected and trained as interviewers. Local guides were selected from public health liaisons of surveyed villages. After written consent was obtained, a standard questionnaire to caregivers was conducted. Information was collected on household characteristics and the family members (especially for children’s mothers), including vaccination status and determinants that may have been significantly associated with a missed or delayed vaccination. Vaccination status and age at vaccination were confirmed by checking the immunization card kept by caregivers or the local immunization clinics. Since parental recall of their child’s immunization history was unreliable, only written vaccination history was accepted as the proof of immunization in our study. Children without any written vaccination certificate were classified as not being vaccinated in our study.
Definition of outcome variables and explanatory variables
We defined vaccination coverage as the proportion of children who had received the vaccine of interest, regardless of the age at which the vaccine was given. We calculated the coverage of 7 vaccine doses including HepB1, PV1, DPT1, PV3, DPT3, HepB3, and MCV1, which are scheduled at birth, 2 mo, 3 mo, 4 mo, 5 mo, 6 mo, and 8 mo of age, respectively in the Chinese EPI.
If a child’s records indicated receipt of the last dose of a vaccine that requires more than one dose to complete the series, it was assumed that earlier vaccinations in the sequence have been given. This assumption has been shown to be valid.35 Hence, we restricted our analysis of determinants for completeness of vaccination to PV3, DPT3, and HepB3 as outcome variables. We restricted our analysis of determinants for timeliness of vaccination to HepB1, PV1, DPT1, and MCV1 as outcome variables. Timely vaccination was defined as vaccination occurring within one month of the recommended age for PV1, DPT1, MCV1, and within one day after birth for HepB1.
Explanatory variables included demographic characteristics of caregivers, the attitude and satisfaction with immunization, socioeconomic development level of surveyed areas, immigration status of children, etc.
Statistical methods
Our plan of analysis included 4 steps: (1) descriptive analysis, (2) univariable analysis, (3) multivariable analysis, and (4) survival analysis to analyze vaccination timing. Steps (1) and (3) were performed twice for each dose of vaccine(first to analyze determinants for non-vaccination and then to analyze determinants for late vaccination). In the univariable analysis we cross-tabulated each explanatory variables with the outcome. χ2 test was used to obtain P values and Crude Odds Ratio (COR) with 95% Confidence Interval (CI) was calculated. In the multivariable analysis, all variables that were associated with the outcome at P < 0.10 were entered into the multivariate model. Logistic regression analysis was adopted to obtain Adjusted Odds Ratio (AOR) with 95% CI. In step (4), survival analysis by the KaplanMeier method was performed to present the timeliness vaccination for dose of vaccine of interest. The overall period of observation ranged from 0–20 mo of age for PV1, DPT1, and MCV1 and 0–14 d (2 wk) of age for HepB1. The children were classified as censored if they were not vaccinated by the time of the survey. All the analyses above applied Statistics Package for Socio Science (SPSS) software, version 13.0. Statistical significance was defined by P < 0.05.
Supplementary Material
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Muhsen K, Abed El-Hai R, Amit-Aharon A, Nehama H, Gondia M, Davidovitch N, Goren S, Cohen D. . Risk factors of underutilization of childhood immunizations in ultraorthodox Jewish communities in Israel despite high access to health care services. Vaccine 2012; 30:2109 - 15; http://dx.doi.org/ 10.1016/j.vaccine.2012.01.044; PMID: 22285273 [DOI] [PubMed] [Google Scholar]
- 2.Jamil K, Bhuiya A, Streatfield K, Chakrabarty N. . The immunization programme in Bangladesh: impressive gains in coverage, but gaps remain. Health Policy Plan 1999; 14:49 - 58; http://dx.doi.org/ 10.1093/heapol/14.1.49; PMID: 10351469 [DOI] [PubMed] [Google Scholar]
- 3.Hu Y, Chen E, Li Q, Chen Y, Qi X. . Immunization Coverage and Its Determinants Among Children Born in 2008-2009 by Questionnaire Survey in Zhejiang, China. Asia Pac J Public Health 2011; Forthcoming http://dx.doi.org/ 10.1177/1010539511430995; PMID: 22186397 [DOI] [PubMed] [Google Scholar]
- 4.Ministry of Health. Implementation for expanded program on immunization. China. http://www.moh.gov.cn/publicfiles/business/htmlfiles/mohbgt/pw10805/200807/37097.htm. Accesses November 14, 2013. Published 2008.
- 5.Linkins RW, Salmon DA, Omer SB, Pan WK, Stokley S, Halsey NA. . Support for immunization registries among parents of vaccinated and unvaccinated school-aged children: a case control study. BMC Public Health 2006; 6:236; http://dx.doi.org/ 10.1186/1471-2458-6-236; PMID: 16995946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lim SS, Stein DB, Charrow A, Murray CJ. . Tracking progress towards universal childhood immunisation and the impact of global initiatives: a systematic analysis of three-dose diphtheria, tetanus, and pertussis immunisation coverage. Lancet 2008; 372:2031 - 46; http://dx.doi.org/ 10.1016/S0140-6736(08)61869-3; PMID: 19070738 [DOI] [PubMed] [Google Scholar]
- 7.Odusanya OO, Alufohai EF, Meurice FP, Ahonkhai VI. . Determinants of vaccination coverage in rural Nigeria. BMC Public Health 2008; 8:381; http://dx.doi.org/ 10.1186/1471-2458-8-381; PMID: 18986544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Topuzoglu A, Ozaydin GA, Cali S, Cebeci D, Kalaca S, Harmanci H. . Assessment of sociodemographic factors and socio-economic status affecting the coverage of compulsory and private immunization services in Istanbul, Turkey. Public Health 2005; 119:862 - 9; http://dx.doi.org/ 10.1016/j.puhe.2005.01.015; PMID: 15949829 [DOI] [PubMed] [Google Scholar]
- 9.Semali IA, Tanner M, de Savigny D. . Decentralizing EPI services and prospects for increasing coverage: the case of Tanzania. Int J Health Plann Manage 2005; 20:21 - 39; http://dx.doi.org/ 10.1002/hpm.794; PMID: 15799455 [DOI] [PubMed] [Google Scholar]
- 10.The National Vaccine Advisory Committee. . The measles epidemic. The problems, barriers, and recommendations. JAMA 1991; 266:1547 - 52; http://dx.doi.org/ 10.1001/jama.1991.03470110093039; PMID: 1880887 [DOI] [PubMed] [Google Scholar]
- 11.Clark A, Sanderson C. . Timing of children’s vaccinations in 45 low-income and middle-income countries: an analysis of survey data. Lancet 2009; 373:1543 - 9; http://dx.doi.org/ 10.1016/S0140-6736(09)60317-2; PMID: 19303633 [DOI] [PubMed] [Google Scholar]
- 12.Akmatov MK, Mikolajczyk RT. . Timeliness of childhood vaccinations in 31 low and middle-income countries. J Epidemiol Community Health 2012; 66:e14; http://dx.doi.org/ 10.1136/jech.2010.124651; PMID: 21551179 [DOI] [PubMed] [Google Scholar]
- 13.Chen Y, Chen E, Li Q. . Evaluation on surveillance of routine immunization coverage rate in Zhejiang province,2005-2009. Dis Surveill 2011; 26:33 - 5 [Google Scholar]
- 14.Zhao Y, He H, Chen E. . Epidemiological characteristics of measles in Zhejiang province. Zhejiang Journal Prevention Medicine 2010; 22:1 - 3 [Google Scholar]
- 15.Hu Y, Li Q, Luo S, Lou L, Qi X, Xie S. . Timeliness vaccination of measles containing vaccine and barriers to vaccination among migrant children in East China. PLoS One 2013; 8:e73264; http://dx.doi.org/ 10.1371/journal.pone.0073264; PMID: 24013709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dannetun E, Tegnell A, Hermansson G, Törner A, Giesecke J. . Timeliness of MMR vaccination--influence on vaccination coverage. Vaccine 2004; 22:4228 - 32; http://dx.doi.org/ 10.1016/j.vaccine.2004.04.018; PMID: 15474712 [DOI] [PubMed] [Google Scholar]
- 17.Akmatov MK, Kretzschmar M, Krämer A, Mikolajczyk RT. . Timeliness of vaccination and its effects on fraction of vaccinated population. Vaccine 2008; 26:3805 - 11; http://dx.doi.org/ 10.1016/j.vaccine.2008.05.031; PMID: 18565626 [DOI] [PubMed] [Google Scholar]
- 18.Bhuiya A, Bhuiya I, Chowdhury M. . Factors affecting acceptance of immunization among children in rural Bangladesh. Health Policy Plan 1995; 10:304 - 12; http://dx.doi.org/ 10.1093/heapol/10.3.304; PMID: 10151848 [DOI] [PubMed] [Google Scholar]
- 19.Ndiritu M, Cowgill KD, Ismail A, Chiphatsi S, Kamau T, Fegan G, Feikin DR, Newton CR, Scott JA. . Immunization coverage and risk factors for failure to immunize within the Expanded Programme on Immunization in Kenya after introduction of new Haemophilus influenzae type b and hepatitis b virus antigens. BMC Public Health 2006; 6:132; http://dx.doi.org/ 10.1186/1471-2458-6-132; PMID: 16707013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Le Polain de Waroux O, Schellenberg JR, Manzi F, Mrisho M, Shirima K, Mshinda H, Alonso P, Tanner M, Schellenberg DM. . Timeliness and completeness of vaccination and risk factors for low and late vaccine uptake in young children living in rural southern Tanzania. Int Health 2013; 5:139 - 47; http://dx.doi.org/ 10.1093/inthealth/iht006; PMID: 24030114 [DOI] [PubMed] [Google Scholar]
- 21.Kitamura T, Komada K, Xeuatvongsa A, Hachiya M. . Factors affecting childhood immunization in Lao People’s Democratic Republic: a cross-sectional study from nationwide, population-based, multistage cluster sampling. Biosci Trends 2013; 7:178 - 85; PMID: 24056168 [PubMed] [Google Scholar]
- 22.Koumaré AK, Traore D, Haidara F, Sissoko F, Traoré I, Dramé S, Sangaré K, Diakité K, Coulibaly B, Togola B, et al. . Evaluation of immunization coverage within the Expanded Program on Immunization in Kita Circle, Mali: a cross-sectional survey. BMC Int Health Hum Rights 2009; 9:Suppl 1 S13; http://dx.doi.org/ 10.1186/1472-698X-9-S1-S13; PMID: 19828057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hu Y, Li Q, Chen E, Chen Y, Qi X. . Determinants of childhood immunization uptake among socio-economically disadvantaged migrants in East China. Int J Environ Res Public Health 2013; 10:2845 - 56; http://dx.doi.org/ 10.3390/ijerph10072845; PMID: 23839061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cui FQ, Gofin R. . Immunization coverage and its determinants in children aged 12-23 months in Gansu, China. Vaccine 2007; 25:664 - 71; http://dx.doi.org/ 10.1016/j.vaccine.2006.08.027; PMID: 17049682 [DOI] [PubMed] [Google Scholar]
- 25.Fosu GB. . Childhood morbidity and health services utilization: cross-national comparisons of user-related factors from DHS data. Soc Sci Med 1994; 38:1209 - 20; http://dx.doi.org/ 10.1016/0277-9536(94)90186-4; PMID: 8016686 [DOI] [PubMed] [Google Scholar]
- 26.Hull BP, McIntyre PB. . Timeliness of childhood immunisation in Australia. Vaccine 2006; 24:4403 - 8; http://dx.doi.org/ 10.1016/j.vaccine.2006.02.049; PMID: 16569467 [DOI] [PubMed] [Google Scholar]
- 27.Luman ET, Barker LE, Shaw KM, McCauley MM, Buehler JW, Pickering LK. . Timeliness of childhood vaccinations in the United States: days undervaccinated and number of vaccines delayed. JAMA 2005; 293:1204 - 11; http://dx.doi.org/ 10.1001/jama.293.10.1204; PMID: 15755943 [DOI] [PubMed] [Google Scholar]
- 28.Zhejiang Provincial Bureau of Statistics. Zhejiang statistics year book. China Statistics Press 2008. [Google Scholar]
- 29.Zhejiang Provincial Bureau of Statistics. Zhejiang statistics year book. China Statistics Press 2009. [Google Scholar]
- 30.Baba K, Okuno Y, Tanaka-Taya K, Okabe N. . Immunization coverage and natural infection rates of vaccine-preventable diseases among children by questionnaire survey in 2005 in Japan. Vaccine 2011; 29:3089 - 92; http://dx.doi.org/ 10.1016/j.vaccine.2010.09.022; PMID: 20870055 [DOI] [PubMed] [Google Scholar]
- 31.Rodewald L, Maes E, Stevenson J, Lyons B, Stokley S, Szilagyi P. . Immunization performance measurement in a changing immunization environment. Pediatrics 1999; 103:889 - 97; PMID: 10103327 [PubMed] [Google Scholar]
- 32.Enkhtuya B, Badamusuren T, Dondog N, Khandsuren L, Elbegtuya N, Jargal G, Surenchimeg V, Grundy J. . Reaching every district - development and testing of a health micro-planning strategy for reaching difficult to reach populations in Mongolia. Rural Remote Health 2009; 9:1045; PMID: 19368489 [PubMed] [Google Scholar]
- 33.Zhejiang Provincial Bureau of Statistics. Zhejiang statistics year book. China Statistics Press 2011. [Google Scholar]
- 34.World Health Organization. Immunization Coverage Cluster Survey-Reference Manual. Geneva, Switzerland, 2005. [Google Scholar]
- 35.Hull BP, Lawrence GL, MacIntyre CR, McIntyre PB. . Estimating immunisation coverage: is the ‘third dose assumption’ still valid?. Commun Dis Intell Q Rep 2003; 27:357 - 61; PMID: 14510061 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.