Abstract
Background: Hepatitis A (HAV) incidence has decreased in the United States, yet regional disparities persist. The role of international travel has become increasingly important in HAV transmission. We compared the relative burden of HAV in border and non-border regions in Arizona and examined the role of travel in sustaining HAV transmission.
Methods: HAV vaccination coverage was calculated by age and region, using Arizona State Immunization Information System data. Incidence, demographics, and risk factors of cases reported through Arizona’s infectious disease surveillance system between 2006 and 2011 were analyzed.
Results: Hepatitis A incidence was higher in the border region of Arizona. Compared with the rest of Arizona, one-dose coverage in children <15 years was lower in the border region until 2008. Second dose coverage was lower in the border region, particularly among Spanish speakers. International travel among cases was generally high; however, in the border region cases were more likely to visit Mexico or South/Central America (94% vs. 80%, P value = 0.01) and be Hispanic (68% vs. 42%, P value = 0.0003).
Conclusions: Rates of HAV continue to be higher in the Arizona border region; the risk appears particularly high among Hispanics with recent travel in the Americas. Border surveillance should be emphasized, along with vaccination of all travelers, to continue to decrease and control HAV.
Keywords: Hepatitis A, United States–Mexico border, travel, vaccination
Introduction
Infectious agents do not adhere to political boundaries. Travel, trade, and immigration between countries with disparate incidence of disease can be a primary source of infection in the lower-incidence country.1 Areas most at risk for disease importation are those with the highest influx of visitors. These can be large cities and hubs of international air travel, or more localized border areas with high rates of ground travel between nations.2-5 Hepatitis A is no exception. Recent evidence suggests that hepatitis A cases in the United States are primarily exposed when traveling outside of the United States and Canada.6 Arizona’s shared border with the northern Mexican state of Sonora, where hepatitis A infection is higher, may make Arizona particularly vulnerable to imported cases of hepatitis A.
Since the United States licensed hepatitis A vaccine in 1995, the rate of hepatitis A has fallen from 12 cases per 100 000 to 0.4 cases per 100 000 in 2011.7 Arizona, the state with the highest hepatitis A infection rates in the country in the pre-vaccine era, initiated childhood vaccination campaigns early.8 In addition to vaccination efforts by the Indian Health Service and state and local health departments, the state’s largest county, Maricopa, instituted a hepatitis A vaccination requirement for enrollment in childcare or preschool, in response to studies that indicated childcare was a primary risk factor for hepatitis A transmission.9,10 By 2011, uptake of the 2 doses required for adequate immune response was comparable in Arizona (51.2%) to the general US population (52.2%), among children aged 19–35 mo.11 Despite similar immunization coverage, Arizona’s hepatitis A incidence remained at 1.2 per 100 000 in 2011, triple that of the United States.7,12
The risk profiles of hepatitis A across the country have changed as cohorts of vaccinated children age in the population, and the average age of cases has increased.12 Less childhood exposure has increased the proportion of unvaccinated adults who are susceptible.13 Higher adult coverage could be an effective intervention strategy but vaccination programs targeted at adults generally have less success than those aimed at children which are often linked to childcare or school entry requirements.14 Current adult hepatitis A immunization recommendations target historically high risk populations: men who have sex with men (MSM), intravenous drug users (IDU), laboratory personnel working with hepatitis A virus (HAV) or HAV-infected primates, individuals with chronic liver disease or those who receive clotting factor concentrates, individuals traveling to intermediate- to high-risk countries, and household contacts of international adoptees from intermediate- to high-risk countries. Vaccination coverage of adults is difficult to calculate in Arizona, as reporting to the immunization system is not mandatory for adult vaccinations. As adult recommendations focus on very specific risk groups, and the vaccine was licensed in 1995, coverage in Arizona adults too old to have received the vaccine as children may be low (<40%), as has been indicated in nationwide studies14.
Previous analysis demonstrated that international travel has replaced household contact and childcare exposure as the primary reported risk factor for transmission of hepatitis A among Arizona cases. More than 50% of cases with interview data reported international travel within the exposure period, and only 10% and 4% reported household or childcare contact, respectively.12
In contrast, Mexico has not incorporated hepatitis A vaccination into the childhood vaccine schedule,15 and the state of Sonora, Mexico, has rates of hepatitis A that are 30 times higher than those of Arizona.16 Traffic is high across the Arizona portion of the United States–Mexico border, with an estimated 24.5 million crossings from Mexico into the United States through Arizona in 2009.17
A better understanding of the factors associated with exposure is needed to develop control strategies and identify reasons why the disparity in hepatitis A rates persists between Arizona and the rest of the United States. We examined Arizona hepatitis A cases reported during 2006 through 2011 to identify (1) differences in hepatitis A incidence rates; (2) demographic differences; and (3) differences in international travel patterns as well as differential vaccination rates between the Arizona border region and the rest of the state.
Results
Case data
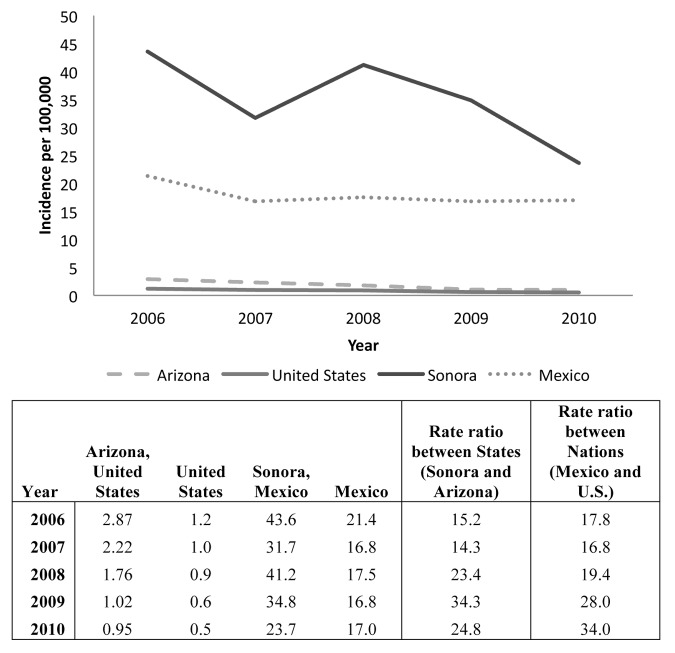
Incidence over the five-year period of 2006–2010 was highly discrepant between the United States and Mexico and between Arizona and Sonora (Fig. 1). In 2010, the incidence rate ratio was 34 between Mexico and the United States and 25 between Sonora and Arizona.
Figure 1. Relative incidence of hepatitis A, 2006–2010: Arizona, United States, Sonora, and Mexico.
From 2006–2011, 625 confirmed hepatitis A cases were reported in Arizona. The number and incidence rate of reported cases decreased each year, with higher rates in 2006 than in subsequent years (Table 1). Rates were higher in Hispanics than non-Hispanic whites (RR 2.05, 95% CI 1.79–2.34) and in the border region than the rest of the state (RR 1.64 [95% CI 1.45–1.84]). The mean and median ages of cases were 35.4 y (95% CI 34–37) and 32 y, respectively.
Table 1. Descriptive statistics of hepatitis A cases reported 2006–2011, Arizona.
| Number of cases (%) | Rate / 100 000 population | Relative Risk (95% Confidence interval) | ||
|---|---|---|---|---|
| Region | Border | 193 (31%) | 2.33 | 1.64 (1.45, 1.84)* |
| Non-border | 432 (69%) | 1.42 | Reference | |
| Year reported | 2006 | 179 (29%) | 2.87 | Reference |
| 2007 | 143 (23%) | 2.22 | 0.77 (0.66, 0.91)* | |
| 2008 | 115 (18%) | 1.76 | 0.61 (0.52, 0.72)* | |
| 2009 | 67 (11%) | 1.02 | 0.35 (0.29, 0.43)* | |
| 2010 | 61 (10%) | 0.95 | 0.33 (0.27, 0.41)* | |
| 2011 | 60 (10%) | 0.93 | 0.32 (0.26, 0.40)* | |
| Race/ethnicity | White, non-Hispanic | 224 (36%) | 0.97 | Reference |
| Hispanic | 215 (34%) | 1.99 | 2.05 (1.79, 2.34)* | |
| Other: Total | 48 (8%) | 1.04 | 1.07 (0.86, 1.31) | |
| • Asian | 14 (2%) | 1.31 | 1.07 (0.93, 1.83) | |
| • African American | 9 (1%) | 0.58 | 0.60 (0.37, 0.85)* | |
| • American Indian | 23 (4%) | 1.14 | 1.18 (0.87, 1.52) | |
| • Other | 2 (0.3%) | N/A | N/A | |
| Unknown | 138 (22%) | N/A | N/A | |
|
Age Mean = 35.4 (95% CI 34–37) Median = 32 |
<1 y | 6 (1%) | 1.06 | 1.08 (0.56, 1.78) |
| 1–4 y | 9 (1%) | 0.39 | 0.39 (0.23, 0.61)* | |
| 5–14 y | 70 (11%) | 1.27 | 1.30 (1.00, 1.70) | |
| 15–24 y | 142 (23%) | 2.63 | 2.68 (2.15, 3.39) * | |
| 25–64 y | 347 (56%) | 1.76 | 1.80 (1.49, 2.21) * | |
| ≥65 y | 50 (8%) | 0.98 | Reference | |
| Sex | Female | 303 (48%) | 1.57 | Reference |
| Male | 321 (51%) | 1.66 | 1.06 (0.95, 1.19) |
Indicates a significant difference in population rates compared with the reference group for CI not including a null value of 1.
Vaccination status by region
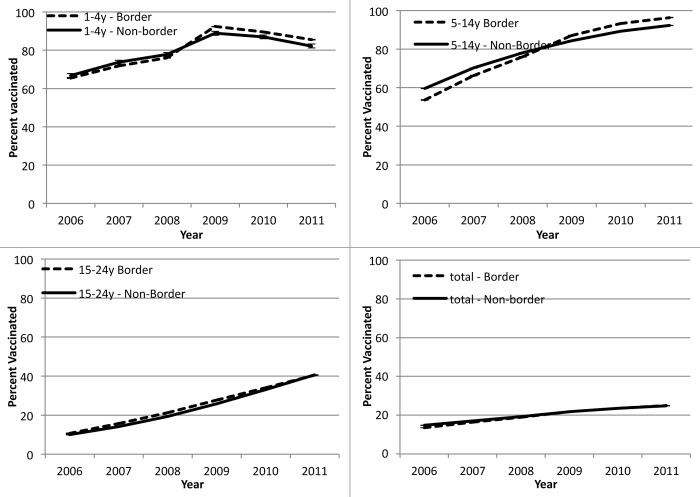
In younger age groups, the differences in coverage with at least one dose of hepatitis A vaccine were minimal between the border and non-border region across the 6 years. Reported one-dose coverage in the border region for age groups 1–4 y and 5–14 y was slightly lower (95% CI difference 1–4%, P < 0.05) than in the non-border region from 2006 through 2008, after which the coverage in the border region exceeded that in the non-border region (95% CI difference 3–4%, P < 0.05) (Fig. 2). Coverage in 15–24 y olds was slightly higher (95% CI difference 1.5–3%, P < 0.05) in the border region until 2010 at which point it was equivalent to the non-border region. In the older age groups (25–64 y and 65+ years), reported vaccination coverage in the border region was consistently higher than that in non-border region (95% CI difference 1–1.5%, P < 0.05), although very low across these age groups (<3%) (data not shown). Two-dose coverage followed the same pattern as one-dose coverage, although there was no difference in coverage for 15–24 y olds (data not shown).
Figure 2. One-dose coverage with hepatitis A vaccine, Arizona, 2006–2011, by age group and region (border and non-border).
Vaccination status by primary language spoken
Overall, Spanish speakers in Arizona were more likely to get their children a second dose of hepatitis A vaccine than English speakers in 2006–2011 (OR 1.30 [95% {CI 1.27–1.32}]). By region, reported two-dose coverage for all ages combined was slightly lower in the border region (OR 0.97 [95% CI {0.95–0.99}]). Stratifying by both language and region demonstrates that in the border region, two-dose uptake among Spanish speakers was less than among English speakers (OR 0.92 [95% CI {0.87–0.97}]) while in the non-border region two-dose coverage was more likely among Spanish speakers (OR 1.37 [95% CI {1.35–1.41}]).
Cases by region
Comparing cases in the border and non-border regions (Table 2), cases in the border region were significantly more likely to be Hispanic (57% vs. 24%, P value < 0.0001) and of younger age (mean age 32.5 vs. 36.7 y, P value = 0.01). Risk factor data was available for 450 (72%) cases; 88% in the border region vs. 65% in the non-border region. Reports of 2 risk factors were slightly higher in the non-border region: sexual or household contact with a hepatitis A case (11% vs. 4%, P value = 0.01); and being identified by the health department as part of a foodborne outbreak of hepatitis A (4% vs. 0%, P value = 0.01). International travel was similar across regions (48% and 56%, P value = 0.11). Of cases with a “yes” or “no” answer to at least one risk factor, over one-third of cases (158, 35%) did not have an identified risk factor, with no difference by region.
Table 2. Comparison of hepatitis A cases and risk factors for cases in the border region and non-border region, 2006–2011, Arizona.
| Arizona n = 625 |
Border Region n = 193 |
Non-border Region n = 432 |
p-value for chi-square test† | ||
|---|---|---|---|---|---|
| Race/ethnicity | White, non-Hispanic | 224 (36%) | 55 (29%) | 169 (39%) | P < 0.0001* |
| Hispanic | 215 (34%) | 110 (57%) | 105 (24%) | ||
| Other | 46 (7%) | 6 (3%) | 40 (9%) | ||
| Unknown | 140 (22%) | 22 (11%) | 118 (27%) | ||
| Age: mean (95% CI); median | 35.4 (33.9–36.9); 32 | 32.5 (29.6–35.4); 28 | 36.7 (34.9–38.5); 35 | P value for t test = 0.01* | |
| Age group | <1 y | 6 (1%) | 0 (0%) | 6 (1%) | P = 0.001* |
| 1–4 y | 9 (1%) | 5 (3%) | 4 (1%) | ||
| 5–14 y | 70 (11%) | 35 (18%) | 35 (8%) | ||
| 15–24 y | 142 (23%) | 43 (22%) | 99 (23%) | ||
| 25–64 y | 347 (56%) | 93 (48%) | 254 (59%) | ||
| 65+ years | 50 (8%) | 17 (9%) | 33 (8%) | ||
| Risk factor data available | 450 (72%) | 169 (88%) | 281 (65%) | P < 0.0001* | |
| International travel | Yes | 229 (51%) | 95 (56%) | 134 (48%) | P = 0.11 |
| No | 197 (44%) | 67 (40%) | 130 (46%) | ||
| Unknown | 24 (5%) | 7 (4%) | 17 (6%) | ||
| Daycare employment, attendance, or contact | Yes | 26 (6%) | 12 (7%) | 14 (5%) | P = 0.38 |
| No | 411 (91%) | 154 (91%) | 257 (91%) | ||
| Unknown | 13 (3%) | 3 (2%) | 10 (4%) | ||
| Sexual or household contact with hepatitis A case | Yes | 37 (8%) | 7 (4%) | 30 (11%) | P = 0.01* |
| No | 301 (67%) | 122 (72%) | 179 (64%) | ||
| Unknown | 112 (25%) | 40 (24%) | 72 (24%) | ||
| Men who had sex with men (includes men only) | Yes | 16 (7%) | 2 (2%) | 14 (9%) | P = 0.07 |
| No | 122 (52%) | 43 (49%) | 79 (53%) | ||
| Unknown | 98 (42%) | 42 (48%) | 56 (38%) | ||
| Injecting drug use | Yes | 10 (2%) | 1 (1%) | 9 (3%) | P = 0.05 |
| No | 349 (78%) | 145 (86%) | 204 (73%) | ||
| Unknown | 91 (20%) | 23 (14%) | 68 (24%) | ||
| Foodborne outbreak | Yes | 10 (2%) | 0 (0%) | 10 (4%) | P = 0.01 * |
| No | 297 (66%) | 127 (75%) | 170 (61%) | ||
| Unknown | 143 (32%) | 42 (25%) | 101 (36%) | ||
| Number of risk factors identified | None | 158 (35%) | 62 (37%) | 96 (34%) | P = 0.80 |
| 1 | 256 (57%) | 96 (57%) | 160 (57%) | ||
| 2 | 32 (7%) | 10 (6%) | 22 (8%) | ||
| 3 | 4 (1%) | 1 (1%) | 3 (1%) | ||
† Chi-square tests for differences in proportions compare Border to Non-Border regions. “Unknown” answers are excluded from the chi-square analysis. *Indicates a significant difference between proportions in the border and non-border regions at α = 0.05.
Since international travel was such a prominent risk factor, we examined travel in more detail. Of cases with a positive or negative response to international travel, cases reporting Hispanic ethnicity were more likely to have traveled (121, 68%) than non-Hispanic whites (75, 41%) or other race/ethnicities (10, 42%) (P value for chi-square test <0.0001). Of the 229 cases reporting travel, 196 (86%) had traveled to Mexico or South/Central America (Table 3). The travel destination and the race/ethnicity of the traveler varied significantly between regions, with travelers in the border region more likely to report travel to Mexico or South/Central America (94% vs. 80%, P value = 0.01) and more likely to be Hispanic (68% vs. 42%, P value = 0.0003). We reviewed cases with travel to Mexico and South/Central America for specific destination information. Of the 127 (65%) cases with specific country information available for that region, 124 (98%) reported travel to Mexico. We also examined international travel in combination with other risk factors; most travelers (198, 86%) reported no other risk factors.
Table 3. Comparison of hepatitis A cases reporting international travel (n = 229) in the border region and non-border region, 2006–2011, Arizona.
| Arizona n = 229 | Border Region n = 95 | Non-border Region n = 134 | P value for chi-square test† | ||
|---|---|---|---|---|---|
| Travel location | Mexico/South-Central America | 196 (86%) | 89 (94%) | 107 (80%) | P = 0.01* |
| Other | 28 (12%) | 6 (6%) | 22 (16%) | ||
| Unknown | 5 (2%) | 0 (0%) | 5 (4%) | ||
| Race/ethnicity | White, non-Hispanic | 75 (33%) | 19 (20%) | 56 (42%) | P = 0.0003* |
| Hispanic | 121 (53%) | 65 (68%) | 56 (42%) | ||
| Other | 10 (4%) | 3 (3%) | 7 (5%) | ||
| Unknown | 23 (10%) | 8 (8%) | 15 (11%) | ||
| Age: mean (95% CI); median | 29.0 (26.8, 31.2); 25 | 26.8 (23.4–30.3); 24 | 30.6 (27.7–33.5); 27 | P value for t test = 0.10 | |
| Additional risk factors | None | 198 (86%) | 85 (89%) | 113 (84%) | P = 0.51 |
| 1 | 27 (12%) | 9 (9%) | 18 (13%) | ||
| 2 | 4 (2%) | 1 (1%) | 3 (2%) | ||
† Chi-square tests for differences in proportions compare border to non-border regions. “Unknown” answers are excluded from the chi-square analysis. *Indicates a significant difference between proportions in the border and non-border regions at α = 0.05.
Discussion
Hepatitis A incidence in Arizona remains persistently higher than the rest of the United States, despite continued decreases in both the level of disease in the state and in the magnitude of the discrepancy with the national data since the advent of hepatitis A vaccine. The statewide incidence steadily decreased from 2006 to 2011. These overall declines, a decade after the introduction of the vaccine, are likely attributed to a concurrent change in the licensed minimum age at administration for this vaccine, from 24 mo to 12 mo, and an expansion of the vaccination recommendation to all children 12–23 mo of age. This demonstrates the importance of vaccination expansion in further reducing transmission in this high risk area.18 Distribution of risk, however, is not homogenous throughout the state; the border region experienced rates of hepatitis A during this period more than one and a half times those of the rest of Arizona.
Previous work has indicated that border regions are susceptible to incursion of transmission from neighboring countries with higher transmission rates. On the United States–Mexico border, there is a long-standing differential in hepatitis A incidence between border regions and the rest of the United States. Early studies identified associations between hepatitis A infection and low socio-economic standing and lower education.19 Given the role of sanitation in preventing hepatitis A transmission, it is not surprising that undeveloped colonias on the border generally had higher rates than urban border communities in Texas.20 But, our previous results demonstrate that high vaccination rates in other Arizona populations, notably American Indians primarily residing on tribal lands, reduced rates of hepatitis A to below that of the general population despite minimal improvement in living conditions.8,12,21
Vaccination coverage in the border region is also quite high, in fact marginally higher than non-border regions in some age groups. In the younger age groups, one-dose coverage is 81% among 1–4 y olds and 95% among 5–14 y olds. Older age groups, however, all have less than 50% recorded vaccination coverage, which may at least partially explain the increased risk of hepatitis A incidence we found in adults compared with children overall. Two-dose coverage patterns were nearly identical to one-dose coverage, though two-dose coverage rates were about half of one-dose coverage. Two doses of hepatitis A vaccine provide stronger and longer-lasting immunity than just one dose,22 examining both one-dose and two-dose coverage can further illuminate populations to target for second-dose follow-up to ensure adequate protection. Overall, individuals in the border region had very slightly lower two-dose coverage than the non-border region. Though overall in Arizona, Spanish speakers were more likely to have a reported a second dose of vaccine, in the border region English speakers were more likely to obtain a second dose. Spanish speakers may be more likely to make visits to Mexico; if two-dose coverage is lower they may be more susceptible to infection.
Cases in the border region were more likely to be Hispanic than in the non-border region. The population in the border region is more heavily Hispanic than in the non-border region (35% vs. 27%) but the margin is too small to fully explain the differences among cases. It is possible that those of Hispanic ethnicity and particularly those speaking Spanish as a primary language may be more likely to travel to see relatives south of the border, contributing to the higher burden of disease in the border region.23 Our results indeed indicate that although international travel is equally reported among cases in border and non-border regions, Mexico, and South/Central America is a more often-cited travel destination for travelers in the border region, and recent international travel is much more predominant among Hispanic cases in the state. These results mirror those of a national study which determined that international travel was implicated in just under half of all reported hepatitis A cases.6
Our study is limited by several factors. First, reported hepatitis A cases likely represent only a fraction of the cases and transmission in the community. Less than 10% of children younger than 6 years of age infected with hepatitis A display symptoms, compared with 40% to 50% of those from 6 to 14 y of age, and 70% to 80% of those older than 14 y of age. Like all surveillance data, there may be biases in the populations that seek healthcare and are reported. We do not expect, however, that under-reporting should be different across time or region. A minority of IgM-positive cases may be misclassified as confirmed cases in the event that information about symptoms could not be obtained. False positives have occurred when not coupled with symptomology as recent vaccination can also result in elevated IgM leading to the inclusion of non-cases if only IgM results are used.24 Risk factor data were unavailable for roughly a quarter of cases and were differentially available for the border region compared with the non-border region, possibly leading to bias in the risk factor analysis. Finally, we cannot identify whether cases were infected as a result of their reported risk factors, including international travel, or through local transmission or other unidentified risk factors.
The vaccination data are also subject to several limitations. The ASIIS system is a passive surveillance system and is subject to under-reporting. Vaccinations administered in other states or countries may or may not be entered in ASIIS by Arizona care providers. Because reporting to ASIIS is not mandated for vaccines administered to adults and many adults may have received their childhood vaccinations in other states, this analysis likely underrepresents coverage among adult age groups, although vaccinations among young adults who were immunized in Arizona as children are included. While reporting of adult immunizations is low, we examine the comparison between border and non-border regions for this analysis, and have no reason to believe that reporting of adult vaccinations would differ between border and non-border regions. For these reasons, we feel the relative levels may reflect actual differences between regions, even if calculated coverage is lower than in reality. While language data was reported in only a fifth of the records, we minimized the bias by examining only the two-dose uptake. By restricting the data to those who had at least one dose already reported, we controlled for the likely differential inclusion of language in the database.
Overall, it appears that there is a strong influence of international travel, specifically to Mexico or South/Central America, as well as other factors inherent to living close to the border of a country with higher incidence of hepatitis A. This may contribute to a discrepancy in border vs. non-border rates of hepatitis A within Arizona, possibly explaining the continued excess in Arizona incidence rates compared with the rest of the country. As a means to monitor and communicate cross-border infectious disease information, the Border Infectious Disease Surveillance (BIDS) network has been put in place.25 BIDS is a sentinel surveillance system that includes hepatitis and febrile exanthems. All individuals at sentinel providers with hepatitis, defined as “illness with jaundice or dark urine, or illness ≥6 d without jaundice and ≥3 of the following: abdominal pain, alcoholic stools, nausea or vomiting, fever, anorexia,” are referred for hepatitis A, B, C, and E testing.25 Given the likely influence of border traffic on hepatitis A transmission, this disease should continue to be monitored as part of the BIDS. Furthermore, all practitioners in the United States–Mexico border region should encourage vaccination among their patients. While immunization coverage should continue to be emphasized for children in all regions, it is important that vaccinations for travelers of any age to Mexico and other endemic areas be stressed, particularly among Hispanics or frequent travelers. Innovative outreach strategies beyond the traditional travel clinic may be needed to reach these individuals through community organizations, churches, or other means. Further efforts should also be made to capture and assess the quality of existing adult immunization rates, as estimates from current vaccination reporting systems are likely gross underestimates of uptake.
Materials and Methods
Relative incidence and vaccination coverage in the border and non-border regions were calculated for each year 2006–2011. The border region was defined as residence in the 4 counties located on the Mexican border: Cochise, Pima, Santa Cruz, and Yuma. This region comprises approximately one-fifth of the Arizona population.
Case data
Publically available rates of hepatitis A for the United States were extracted from annual reports from CDC.7 Incidence rates for Mexico and the state of Sonora were obtained from the Mexican Health Department website.16 Detailed case data were obtained for cases reported to the Arizona Department of Health Services (ADHS) as described in Erhart and Ernst 2012.12 For this analysis, confirmed hepatitis A cases reported 2006 through 2011 were extracted from the ADHS surveillance database. Cases were included if they met the Council of State and Territorial Epidemiologists’ case definition for the year the case was reported: discrete onset of symptoms and either jaundice or elevated serum aminotransferase levels, along with either positive IgM antibody to hepatitis A virus or an epidemiologic link to a person with laboratory-confirmed hepatitis A.26 For risk factor analysis, only cases with at least one “yes” or “no” answer to risk factor questions were included.
Vaccination data
Vaccinations are reported to the Arizona State Immunization Information System (ASIIS) at ADHS, described more extensively in Ernst et al. 2011.8 Each year the ASIIS database is populated with Arizona birth records. Arizona providers are required to report all vaccinations administered to children. All recorded hepatitis A vaccinations were extracted from ASIIS. Records were excluded as invalid if the county of residence was unknown or out-of-state; if the year of vaccination was recorded as pre-licensure (before 1995), or post-study period (2012 or later); or if age was invalid (<0 or >107 y). Doses were also considered invalid if age at administration was <2 y before 2005 and <1 y 2005 and after, with a four-day grace period.
Case analysis
Incidence rate of hepatitis A was calculated and compared by year, age, race/ethnicity, sex, and border region. Demographic and risk factor differences, including gender, race/ethnicity, language spoken, international travel, daycare association, MSM, IDU, and food-borne outbreak were assessed using chi-square tests. Country of travel for international travel was determined overall and by border region.
Vaccination coverage analysis
One- and two-dose coverage for border and non-border regions of Arizona, by age group, were calculated as described in Ernst et al. 20118 for each year 2006–2011. To examine differences between the border and non-border regions, 95% CI bounds were calculated for the yearly estimates and differences between the upper and lower bounds of the CI in the 2 regions were assessed. To examine receipt of a second dose for individuals with multiple doses administered, we matched a second valid dose to the first dose, examined timing between doses, and retained second doses that met the minimal interval of 6 mo, with a 4-d grace period. If the second dose was administered at less than the minimum interval, we excluded the second dose and replaced it with a third dose, if available. We compared receipt of the second dose of vaccine by border non-border region. Additionally, we restricted the analysis to those who had at least one vaccination recorded and calculated the odds of receiving a second dose if primary language was English vs. Spanish.
Human subjects
Human subject approval was sought from the University of Arizona and the Department of Health Services and was deemed exempt.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Amariei R, Willms AR, Bauch CT. . The United States and Canada as a coupled epidemiological system: an example from hepatitis A. BMC Infect Dis 2008; 8:23; http://dx.doi.org/ 10.1186/1471-2334-8-23; PMID: 18307785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bentley JW, Robson M, Sibale BB, Nkhulungo E, Tembo Y, Munthali F. . Travelling Companions: Emerging Diseases of People, Animals and Plants Along the Malawi-Mozambique Border. Hum Ecol 2012; 40:557 - 69; http://dx.doi.org/ 10.1007/s10745-012-9503-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Budd L, Bell M, Warren A. . Maintaining the sanitary border: air transport liberalisation and health security practices at UK regional airports. Trans Inst Br Geogr 2011; 36:268 - 79; http://dx.doi.org/ 10.1111/j.1475-5661.2010.00424.x [DOI] [Google Scholar]
- 4.Dávila Cornejo M, Aramburu Celigueta C, Morte Esteban S, Vera Gil I, Iglesias García MJ, González Gutiérrez-Solana O. . [Health control at International Borders: the role of foreign health during the containment phases of the pandemic (H1N1) 2009]. Rev Esp Salud Publica 2010; 84:507 - 16; PMID: 21203716 [DOI] [PubMed] [Google Scholar]
- 5.Hwang GM, Mahoney PJ, James JH, Lin GC, Berro AD, Keybl MA, Goedecke DM, Mathieu JJ, Wilson T. . A model-based tool to predict the propagation of infectious disease via airports. Travel Med Infect Dis 2012; 10:32 - 42; http://dx.doi.org/ 10.1016/j.tmaid.2011.12.003; PMID: 22245113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klevens RM, Miller JT, Iqbal K, Thomas A, Rizzo EM, Hanson H, Sweet K, Phan Q, Cronquist A, Khudyakov Y, et al. . The evolving epidemiology of hepatitis a in the United States: incidence and molecular epidemiology from population-based surveillance, 2005-2007. Arch Intern Med 2010; 170:1811 - 8; http://dx.doi.org/ 10.1001/archinternmed.2010.401; PMID: 21059974 [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Viral Hepatitis Statistics and Surveillance. Atlanta, GA, 2012. [Google Scholar]
- 8.Ernst KC, Pogreba-Brown K, Rasmussen L, Erhart LM. . The effect of policy changes on hepatitis A vaccine uptake in Arizona children, 1995-2008. Public Health Rep 2011; 126:Suppl 2 87 - 96; PMID: 21812173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ernst KC, Pogreba-Brown K, Rasmussen L, Erhart LM. . The effect of policy changes on hepatitis A vaccine uptake in Arizona children, 1995-2008. Public Health Rep 2011; 126:Suppl 2 87 - 96; PMID: 21812173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Venczel LV, Desai MM, Vertz PD, England B, Hutin YJ, Shapiro CN, Bell BP. . The role of child care in a community-wide outbreak of hepatitis A. Pediatrics 2001; 108:E78; http://dx.doi.org/ 10.1542/peds.108.5.e78; PMID: 11694662 [DOI] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention (CDC). . National, state, and local area vaccination coverage among children aged 19-35 months--United States, 2011. MMWR Morb Mortal Wkly Rep 2012; 61:689 - 96; PMID: 22951450 [PubMed] [Google Scholar]
- 12.Erhart LM, Ernst KC. . The changing epidemiology of hepatitis A in Arizona following intensive immunization programs (1988-2007). Vaccine 2012; 30:6103 - 10; http://dx.doi.org/ 10.1016/j.vaccine.2012.07.029; PMID: 22835739 [DOI] [PubMed] [Google Scholar]
- 13.Steffen R. . Changing travel-related global epidemiology of hepatitis A. Am J Med 2005; 118:Suppl 10A 46S - 9S; http://dx.doi.org/ 10.1016/j.amjmed.2005.07.016; PMID: 16271541 [DOI] [PubMed] [Google Scholar]
- 14.Lu PJ, Byrd KK, Murphy TV. . Hepatitis A vaccination coverage among adults 18-49 years traveling to a country of high or intermediate endemicity, United States. Vaccine 2013; 31:2348 - 57; http://dx.doi.org/ 10.1016/j.vaccine.2013.03.011; PMID: 23523408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization. Immunization profile - Mexico. Geneva, Switzerland: World Health Organization, 2012. [Google Scholar]
- 16.Centro Nacional de Vigilancia Epidemiologica y Control de Enfermedades. Incidencia de Enfermadad per Grupo de Edad y Entidad Federativa, 2012. [Google Scholar]
- 17.Mwaniki-Lyman L, Christopherson R. Arizona-Sonora Region: Border Crossings. Tucson, AZ: Eller College of Management, 2010. [Google Scholar]
- 18.Centers for Disease Control and Prevention (CDC). . Hepatitis a vaccination coverage among children aged 24-35 months - United States, 2006 and 2007. MMWR Morb Mortal Wkly Rep 2009; 58:689 - 94; PMID: 19574951 [PubMed] [Google Scholar]
- 19.Doyle TJ, Bryan RT. . Infectious disease morbidity in the US region bordering Mexico, 1990-1998. J Infect Dis 2000; 182:1503 - 10; http://dx.doi.org/ 10.1086/315876; PMID: 11010841 [DOI] [PubMed] [Google Scholar]
- 20.Leach CT, Koo FC, Hilsenbeck SG, Jenson HB. . The epidemiology of viral hepatitis in children in South Texas: increased prevalence of hepatitis A along the Texas-Mexico border. J Infect Dis 1999; 180:509 - 13; http://dx.doi.org/ 10.1086/314861; PMID: 10395871 [DOI] [PubMed] [Google Scholar]
- 21.Native American Tribal Rights JP. How Arizona's Looming Water-Shortage Threatens Tribal Sovereignty. Law School. Buffalo, NY: State University of New York, 2012. [Google Scholar]
- 22.Wang XY, Xu ZY, Ma JC, von Seidlein L, Zhang Y, Hao ZY, Han OP, Zhang YL, Tian MY, Ouyang PY, et al. . Long-term immunogenicity after single and booster dose of a live attenuated hepatitis A vaccine: results from 8-year follow-up. Vaccine 2007; 25:446 - 9; http://dx.doi.org/ 10.1016/j.vaccine.2006.08.004; PMID: 16949710 [DOI] [PubMed] [Google Scholar]
- 23.Jong EC. . United States epidemiology of hepatitis A: influenced by immigrants visiting friends and relatives in Mexico?. Am J Med 2005; 118:Suppl 10A 50S - 7S; http://dx.doi.org/ 10.1016/j.amjmed.2005.07.017; PMID: 16271542 [DOI] [PubMed] [Google Scholar]
- 24.Castrodale L, Fiore A, Schmidt T. . Detection of immunoglobulin M antibody to hepatitis A virus in Alaska residents without other evidence of hepatitis. Clin Infect Dis 2005; 41:e86 - 8; http://dx.doi.org/ 10.1086/497073; PMID: 16206092 [DOI] [PubMed] [Google Scholar]
- 25.Weinberg M, Waterman S, Lucas CA, Falcon VC, Morales PK, Lopez LA, Peter C, Gutiérrez AE, Gonzalez ER, Flisser A, et al. . The U.S.-Mexico Border Infectious Disease Surveillance project: establishing bi-national border surveillance. Emerg Infect Dis 2003; 9:97 - 102; http://dx.doi.org/ 10.3201/eid0901.020047; PMID: 12533288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. 2012 Case Definitions: Nationally Notifiable Conditions Infectious and Non-Infectious Case. Atlanta, GA, 2012. [Google Scholar]