Abstract
Background
Persons with heart failure (HF) are required to make decisions on a daily basis related to their declining health and make urgent decisions during acute illness exacerbations. However, little is known about the types of decisions patients make.
Objective
To critically evaluate the current quantitative literature related to decision-making among persons with HF and identify research gaps in HF decision-making research.
Methods
A systematic search of literature about decisions persons with HF make was conducted using the PubMed, CINAHL, and PsychINFO databases. The following inclusion criteria were used: sample comprised of at least 50% HF participants, concrete decisions were made, and a quantitative study design was used. Two authors performed title, abstract, and full text reviews independently to identify eligible articles.
Results
Twelve quantitative articles were included. Study samples were predominately older, White, male, and married. Two thirds of the articles focused on decisions related to the end of life topics (i.e., resuscitation decisions, advanced care planning). The other one third focused on decisions about care seeking, participant’s involvement in treatment decisions during their last clinic visit, and self-care behaviors.
Conclusions
Within the HF literature, the term decision is often ill-defined or not defined. Limitations in methodological rigor limit definitive conclusions about HF decision-making. Future studies should consider strengthening study rigor and examining other decision topics such as inclusion of family in making decisions as HF progresses. Research rigorously examining HF decision-making is needed to develop interventions to support persons with HF.
Keywords: decision-making, heart failure, palliative care, review literature as topic
Introduction/Background
Approximately 5.1 million people in the United States have heart failure (HF),1 with the prevalence expected to increase to more than 8 million people by 2030.1 Persons living with HF are expected to adequately manage their illness independently in the community. Due to the unique HF trajectory—unlike a typical chronic or acute illness2—and the complex nature of HF management,3 persons with HF may find making decisions related to their illness particularly challenging. Not only are persons with HF required to make decisions on a daily basis related to their steady decline in health, but also make urgent decisions during acute exacerbations of illness.
Although the terms decision and preference are used interchangeably in the literature, for this review we defined decision-making as a dependent variable where a concrete outcome was measured in a past or hypothetical situation (i.e., Do Not Resuscitate/DNR orders, resuscitation wishes, care-seeking, and life style choices). Preferences are defined as the tendency to “consider something desirable or undesirable”.4 Preferences are conceptualized as a precursor (or an independent variable) to making an actual decision and part of the process in making decisions.4 For example an individual who is considering the options of (a) writing an advanced directive and (b) not writing an advanced directive will have a preference for one of the options. This is different from an individual who makes a decision to have an advanced directive, which means he/she has written and formalized an advanced directive for medical use.
In the last ten years, the medical field has shifted its focus from a provider-driven, hierarchical decision-making model to a more patient-centered, and shared decision-making model. The number of studies on patient medical decision-making has also doubled in major databases such as PubMed. However, it is still unclear what type of decisions have been explored within the HF literature. Therefore, the purpose of this article is to critically evaluate the current quantitative literature related to decision-making among persons with HF and identify research gaps in HF decision-making research.
Methods
Selection of Articles
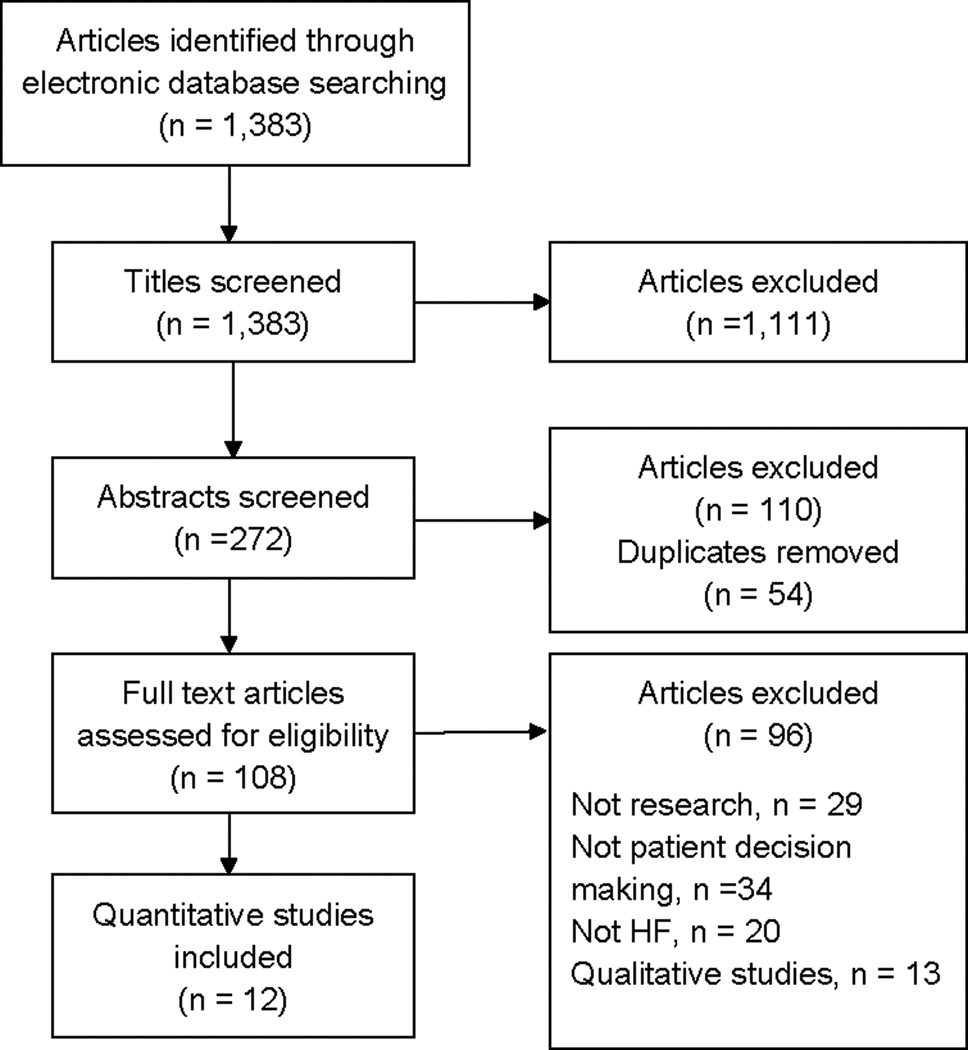
A systematic search of literature about decisions person with HF make was conducted in January 2014. The search was conducted in the PubMed, CINAHL, and PsychINFO databases using the following criteria: articles published from the beginning of the database to January 2014, in the English language, and about humans. The search terms used for each database can be found in appendix A. The initial search resulted in 1,383 articles from all three databases (not excluding duplicates). Two of the authors (XX and XX) then performed title, abstract, and full text reviews independently to identify eligible articles. Articles were included if they met the following inclusion criteria: sample comprised of greater than or equal to 50% persons with HF, concrete decisions (either actual or hypothetical scenarios) were made by persons with HF, and a quantitative study design. Articles were excluded if they were case studies, did not report on the percent of HF participants in the sample, and only included information about patient preferences. A total of 12 articles met the inclusion criteria and were included in this review. Figure 1 depicts the article selection process.
Figure 1.
Article Selection Process
Results
Articles overview
Of the 12 research reports, 5 were surveys, 1 was a chart review, 2 were secondary analyses of data, 2 were interventions, and 2 used multiple methods (i.e. chart review and survey, mixed methods). Researchers recruited study participants from inpatient hospital visits (n=9, 75%), outpatient clinics (n=2, 17%), and chart reviews (n=1, 8%). Sample sizes ranged from 8 to 539 totaling 1,715 participants. Participants were generally older adults (54-81 years old), male (42%-94%), White (60%-95%), and married (45%-69%). Table 1 summarizes study characteristics.
Table 1.
Study Summaries
| Ref Quality rating* |
Purpose | Design Setting |
Sample | Dec | Main Results |
|---|---|---|---|---|---|
| Dev et al., 2012 | Determine association of HF patient resuscitation orders with individual characteristics | Secondary analysis of data from an RCT Time points: 1, 2, 3, 6 months post discharge Setting: United States Canada |
DNR group N= 26 Median age: 64 Male: 65% White: 77% Married: not reported Education: not reported HF patients: 100% Full code group N=349 Median age: 56 Male: 74% White: 60% Married: Not reported Education: Not reported HF patients: 100% |
Resuscitation orders | DNR patients were older, more likely to have comorbid conditions, lower exercise capacity (6 min walk distance), and longer initial hospitalizations than Full Code patients DNR patients had a higher 6 month mortality (34% higher, p<0.0001; 6.88 hazard ratio) |
| Levenson et al., 2000 | Characterize patient experiences with HF in last 6 months of life | Secondary analysis of data of a prospective cohort study Time points: 3–6 months, 1–3 months, 3 days-1 month before death Info about last 3 days of life came from after death interviews with surrogates Setting: United States |
N=539 Mean age: Not reported Male: 64% White: 78% Married: Not reported Education: Not reported HF patients: 100% |
Resuscitation orders | Written DNR orders increased as death approached: 30%, 36%, 57%, respectively at 3–6 months, 1–3 months, and 3 days–1 month before death DNR orders more likely to be written at baseline for patients who died within first year of enrollment (P<0.001) |
| Formiga et al., 2004 | Determine CPR and end of life care wishes | Descriptive, cross-sectional survey Setting: Spain |
N= 80 Mean age: 79 Male: 42% White: Not reported Married: 45% Education: Not reported HF patients: 100% |
Resuscitation orders Location of death |
Who decides on resuscitation: patient 39%, doctor 17%, family 2%, all together 42% If cardiac arrest, 40% did not want to be resuscitated If recovery is unlikely patients wanted to be treatment at home (50%) versus the hospital (40%) |
| Formiga et al., 2007 | Evaluate end of life circumstances | Chart review & cross-sectional caregiver survey one month post-patient death Setting: Spain |
Patients, N=102 Mean age: 81 Male: 43% White: Not reported Married: Not reported Education: Not reported HF patients: 64% |
Resuscitation orders Location of death |
94% of HF patients had DNR instructions on medical record Who made decision to die in hospital: patient (26%), family (31%), doctor (15%), joint (30%) |
| Agård et al., 2000 | Examine patient understanding, attitudes, decision-making towards CPR | Concurrent mixed methods Setting: Sweden |
N=40 Mean age: 75 Male: Not reported White: Not reported Married: Not reported Education: Not reported HF patients: 100% |
Resuscitation orders | Physician (37%), patient (12%), patient and physician (47%) decide on performing CPR |
| Evangelista et al., 2012 | Assess impact of palliative care intervention on health perceptions, attitudes, knowledge, and completion of advance directives | One group, pre-post-test design Time points: Baseline 3 months Intervention: Referral to outpatient palliative care specialist consultation Setting: United States |
N=36 Mean age: 54 Male: 72% White: 61% Married: 69% HS or less: 64% HF patients: 100% |
Advance directives | 47% of the participants completed advanced directives at 3 months follow-up (19% increase) (p=0.016) At 3 month follow up, Whites and those who discussed advance directives with family members were more likely to complete advance directives (all p<0.05) |
| Habal et al., 2011 | Determine patients’ awareness, comprehension, and utilization of advanced directives |
Descriptive, cross-sectional, survey (part of convergent mixed methods study) Setting: Canada |
N= 41 Mean age: 57 Male: 83% White: Not reported Married: Not reported Education: Not reported HF patients: 100% |
Estate will Substitute decision maker ICD deactivation |
76% had a will 88% had a substitute decision maker with spouse being most common (n=26) For ICD patients: If condition deteriorated, 47% wanted defibrillator turned off; 26% wanted to keep it activated; 16% undecided; 11% did not want to answer question |
| Kobza & Erne, 2007 | Evaluate ICD deactivation wishes | Retrospective chart review Setting: Switzerland |
N=8 Mean age at death: 67 Male: 88% White: Not reported Married: Not reported Education: Not reported HF patients: 100% |
ICD deactivation | No patients wanted ICD deactivated 6 patients felt active withdrawal meant giving up hope for a cure |
| Altice & Madigan, 2012 | Evaluate contributions of symptom recognition and clinical factors to care-seeking decision delays | Descriptive, cross-sectional survey Setting: United States |
N=75 Mean Age: 75 Male: 52% White: 85% Married: 48% HS or less: 69% HF patients: 100% |
Care-seeking | 93% of patients experienced dyspnea symptoms and described it as reason to seek care Patients with more acute symptoms were more likely to seek emergent care (p=0.04) Patients with more chronic symptoms were more likely to proactively seek care (p=0.001) |
| Jurgens, 2006 | Explore relationships among somatic awareness, uncertainty, symptom pattern, age, sex, history of HF, and care-seeking delay patterns | Descriptive, cross-sectional survey Setting: United States |
N=201 Mean age: 70 Male: 56% White: 95% Married: 49% HS or less: 63% HF patients: 100% |
Care-seeking | 78% participants sought care because of dyspnea Older adults, patients with a history of HF admissions, and acute symptoms decreased delay in care seeking |
| Rodriguez et al., 2008 | Assess involvement in treatment decisions | Descriptive, cross-sectional, telephone survey Setting: United States |
N=90 Mean Age: 70 Male: 94% White: 86% Married: 57% HS or less: 61% HF patients: 100% |
Treatment decisions | Involvement in medical decision-making during last clinic visit: 46% expressed some opinion, 20% suggested a certain kind of care, 20% expressed doubt about provider's recommendations, 10% insisted on a particular kind of care Preference in level of involvement in decisions making explained 17% of variation in level of Involvement in last clinic visit |
| Jaarsma et al., 2000 | Test the effect of education and support intervention on HF self-care behavior | Randomized control Trial Time points: Baseline, 1, 3, and 9 months post discharge Intervention: Education and support from hospitalization to home Setting: Netherlands |
N=128 Mean age: 73 Male: 60% White: Not reported Married: 56% Education: Not reported HF patients: 100% |
Care-seeking Self-care behavior decisions |
Patients did not contact doctor for symptoms because of limited knowledge and awareness of symptoms Did not follow fluid restrictions, adapt lifestyle, weight oneself, exercise, and/or take medications properly due to false perceptions, job restrictions, lack of knowledge, or physical disability |
A = High, B = Good, C = Low
Eleven studies were conducted exclusively among persons with HF, and one study included 64% HF participants. Two thirds of the articles focused on decisions related to the end of life such as resuscitation decisions (n=5), advanced care planning (n=2), ICD deactivation (n=2), location of death (n=2), and identification of a substitute decision maker (n=1). The other one third of articles focused on decisions about care seeking (n=2), patient’s involvement in treatment decisions during their last clinic visit (n=1), and self-care behaviors (n=1).
Resuscitation Decisions
Resuscitation decisions such as DNR orders and CPR usage were examined in five studies. In comparison to participants without DNR orders those with DNR orders tended to have a shorter life expectancy (i.e. death within 6 months of hospitalization with a p-value<0.00015 or within one year of enrolling in a research study).6 Approximately half (40%–57%) of HF participants hospitalized for acute HF exacerbation stated they would refuse resuscitation,6,7 with more DNR orders as death approached.6 In contrast, 94% of the deceased HF participants whose medical records were reviewed (n=65) had written DNR instructions.8
The question of who should be responsible for making resuscitation decisions was addressed in two cross sectional surveys. Agard and Formiga found approximately half the participants wanted to share the responsibility with their doctor and/or family.7,9 The percent of participants who wanted to make CPR decisions independently (39% vs.12%) or depend on the doctor (17% vs. 37%) varied in the studies. A small number of participants (N=80 and 40) were recruited from two countries with different cultural backgrounds - Spain7 and Sweden9 – for the studies.
Future Planning
Of the eleven studies conducted exclusively among HF participants, two focused on decisions related to future care planning. Evangelista conducted a quasi-experimental study (N=36) to assess the completion of an advanced directive after receiving a palliative care consultation.10 Habal used a descriptive survey (N=41) to assess completion rates of wills.11 A palliative care consultation significantly increased the completion of advanced directives from 28% to 47% (p=0.016) in the first study.10 The majority of participants (76%) had completed a will in the study by Habal.11 Sample sizes were small and samples were predominantly male in both studies.
ICD deactivation
Two studies by Habal and Kobza examined if HF participants would deactivate their ICDs prior to death, had mixed results.11,12 Habal found in a cross sectional study (N=41) that 47% of participants wanted ICD deactivation11. In contrast, a retrospective chart review by Kobza and Erne (2007) revealed that none of the participants wanted ICD deactivation at the time of death. Of note, participants in both studies were in different phases of their illness trajectory. Not all the participants in Habal’s study were at the end of life,11 whereas participants in Kobza’s study were at the end of life.12 Additionally, participants in Habal’s study were given a hypothetical situation,11 while participants in Kobza’s study decided on ICD deactivation based on their current state of health.12
Location of death
Two studies by Formiga examined participants’ decisions about the location of death.7,8 When given a hypothetical scenario anticipating death, 40% of HF participants in a cross-sectional survey decided to die at the hospital.7 In a caregiver survey one month post-patient death, Formiga found only 26% of patients independently chose to die in the hospital.8 The location of death was measured differently in both studies - via participant survey using a hypothetical scenario about desired location of death7 and caregiver report on actual decisions made by the dying patient about the location of death.8
Surrogate decision maker
Persons with HF may identify a surrogate decision maker in the event they cannot make their own decisions. Habal (N=41) investigated who HF participants’ would want to be their surrogate decision maker11 and found that 88% of participants had a surrogate decision maker, with 72% identifying their spouse as the surrogate.
Care Seeking
Altice and Jurgens examined when HF participants decided to seek care prior to being hospitalized in two correlation studies.13,14 In both studies, acute symptoms such as dyspnea were a common cue which led HF participants to seek care. Participants with chronic/progressive symptoms were more likely to proactively call their care provider, while those with acute symptoms sought emergency care (p=0.007).13,14 Older age and a history of HF admissions were factors associated with decreased delay in care seeking.14
Treatment Decision
Rodriguez used a telephone survey (N=90) to examine how HF participants were involved in making medical decisions during outpatient clinic visits.15 Nearly half (46%) of participants reported expressing some opinion with an additional 30% suggesting or insisting on a specific medical treatment. The authors did not specify what “care decision” meant in the study, however. In addition, the Perceived Involvement in Care Scale subscale, used to measure participant’s involvement in decisions, had a very low Cronbach’s alpha of 0.49 in this sample.
Self-Care Behavior Decisions
Using a multifaceted intervention (education plus support program), Jaarsma examined challenges 128 HF participants faced when following recommended HF self-care behaviors.16 Participants listed the following challenges: limited knowledge on what behaviors needed to be changed after a HF diagnosis, false perceptions of what was acceptable (e.g., fluid intake), job restrictions (e.g., could not rest due to work requirements), and physical disabilities (e.g., limited eyesight). The number of challenges mentioned by the participants did not significantly differ between the control and intervention groups at 3 or 9 months.16 Jaarsma and colleagues identified participant fatigue as a major concern because participants were asked multiple times in each interview about following self-care recommendations (up to 19 times). The fatigue caused some participants to become irritated and dismissive of the questions, which may have impacted how they responded to interview questions.
Discussion
Decision science examines how persons with HF make choices regarding their health and how clinicians can help persons with HF make informed health care decisions. In order to clearly delineate recommendations for future research, the discussion section is organized according to research gaps.
Limited research on decision-making in HF
The number of articles about decisions persons with HF make was limited. Within a small set of articles available, two thirds of the studies included in the review addressed topics related to end of life decisions. There is a great need to understand the broader spectrum of decisions persons with HF make. Qualitative studies have explored decision topics not found in the quantitative literature, such as the family dynamics surrounding genetic testing in HF17 or when to begin advanced care planning.18 Other decision topics in need of further development and study include: decisions around the use of life-saving technologies such as left ventricular assistive devices (LVADS), how persons with HF make treatment decisions when multiple health care providers suggest different treatments, and how persons HF decide to enroll in palliative care. Such decisions are especially critical for clinicians to understand with rapid advances in technology for persons with HF, increasing numbers of HF treatment options, and more complex persons with HF who are often older adults with multiple comorbidities.19,20 Building on validated decision theories, such as naturalistic decision-making,21 may be a useful approach in developing future research to better understand the nature and mechanism of decision-making amongst persons with HF.
Understanding decision triggers, which cause a person with HF to make or not make decisions, would be especially helpful in developing targeted, clinical interventions to improve health behaviors and patient outcomes. Symptoms related to HF (e.g., shortness of breath) have been identified as common triggers for persons with HF to seek care from health providers.13,14 Yet, it is unclear if there are any modifiable variables (such as ability to identify and assess symptoms in a timely manner, problem solving skills, and communication skills about symptoms) which might influence participant’s decisions to engage in HF self-care. Future studies are warranted to further examine modifiable decision triggers and explore how these triggers can be integrated into clinical interventions to promote healthy behavior decisions among persons with HF, prevent inappropriate health care utilization, and reduce negative health outcomes.
Inconsistent use of the term decision
The confusing nature of how decisions are defined in HF research became apparent early in the search process. The majority of studies included in the review did not clearly conceptualize the decision being investigated. Instead, terms such as preference, attitude, wishes, and decision were used interchangeably. Some articles described decisions as preferences, even though concrete or hypothetical decisions were made by persons with HF. Consequently, it was challenging to determine if some of the articles were eligible without carefully and extensively discussing the study design and outcomes within the writing team. To advance decision science in the field of HF, it is imperative to clearly define decision and for future work to examine the decision-making process that leads preferences to become decisions.
Concerns about methodological rigor
Limited methodological rigor was of concern for studies included in the review. In general, studies had small sample sizes, with 67% of studies including less than 100 participants. Only 2 studies13,14 reported estimating sample sizes with a power analysis. The small samples and lack of power analyses in the majority of the articles makes the validity of the findings and conclusions drawn questionable. Similarly, half the studies (n=6) did not report the racial and/or sex breakdown or the educational level of the sample. The majority of studies reporting race, sex, and age had a sample with more than 70% Whites (n=5, 83%) and more than 50% males (n=9, 64%). Unfortunately, these sample characteristics are not comparable to general HF population characteristics where 47% of HF participants were females,1 limiting the generalizability of the study findings. The lack of studies with sufficient representation of minorities and females results in a paucity of subgroup comparisons, by ethnicity and by sex. Subgroup comparisons are important to examine due to differences in risk for HF and treatment patterns between racial/ethnic minority groups and by sex.1,14,22 In order to improve sample representativeness and increase subgroup comparisons, researchers should attempt to recruit sufficient numbers of racial/ethnic minorities and females. Additionally, future researchers should consider calculating and reporting the use of power analyses to determine adequate study sample size.
Another key methodological concern was related to study design. The majority of the studies were designed or analyzed cross-sectionally,5,7,8,10–16 limiting our understanding of if and how decisions change over time. More studies are needed to determine when and how persons with HF make key HF decisions and what influences their decisions over time. For instance, persons with decompensated HF have highly impaired cognitive functioning23, highlighting the importance of examining how persons with HF involve family members in making decisions as their illness progresses.
Lack of valid Measurement of decision-making
Out of all the studies, only three used reliable and valid instruments designed to measure decisions. In the remaining studies, the authors generated their own questions to ask about decisions. Author generation of their own decision-making questions may be due to the lack of a “gold standard” for measuring decisions. The creation of a standard measurement tool may be challenging since the types of decisions persons with HF make are heterogeneous. Nevertheless, researchers should consider systematic approaches to assess the validity and reliability of their decision measurements. Additionally, researchers should be encouraged to measure various decision concepts such as decisional conflict, regret, or satisfaction to better understand the mechanism of decision-making. Measuring these decision concepts would help explain the decision process when making concrete/hypothetical decision, allowing us to gain more insight into the entire decision-making process. There are reliable and valid instruments which measure aspects of decisions such as the Satisfaction with Decision Instrument,24 Decision Self-Efficacy Scale,25 and Decision Regret Scale.26 The use of the same decision tools in a multitude of studies, examining the same type of decision, would allow researchers to more easily compare HF decision processes and outcomes.
Limitations
Only articles published in the English language were included in this review and articles not published in databases were missed. It is possible that articles related to decisions persons with HF make may have been excluded if they did not use common decision-making terms (e.g. decision, choice) in the title or abstract. Efforts to minimize this possibility were made by working with an experienced health sciences librarian to compile a list of comprehensive database search terms, and by having two individuals identify eligible articles independently. It is also possible that some articles may have had a sample with more than 50% HF participants, but were excluded because they did not specify the type of participants recruited. We tried to minimize this possibility by carefully reviewing sampling procedures through full text reviews of articles included after the title and abstract screenings. Lastly, although all included studies examined elements of decision-making, they did not necessarily study decisions as the primary purpose of the study. However, this review offers a current state of decision science in HF.
Conclusions
A review of literature on decisions made by persons with HF revealed that the term decision is often ill-defined/not defined in the HF literature and that topics investigated so far are mostly related to end of life decisions. Limitations in methodological rigor identified in the articles also limit conclusions made in the studies and the generalizability of findings. Future research should use a clear definition of the term decision and consider further decision topics such as: changes in decision-making over time, the inclusion of family members in making decisions, decisions surrounding use of life-saving technology, use of palliative care, and modifiable factors prompting care seeking. In addition, future studies should consider strengthening study rigor through the use of techniques such as: power analysis to ensure adequate sample sizes, including sufficient numbers of females and racial/ethnic minorities in the study sample, and using reliable and valid instruments to measure decisions. Research rigorously examining HF decision-making may be used to advance HF education and interventions to support persons with HF as they navigate their illness.
What’s New?
Despite the increasing number of medical decision-making [0]studies, it is unclear what type of decisions have been explored within the HF population.
The HF decision literature lacked a clear definition of the term decision and limited topics were investigated (mostly pertained to end of life decisions) with often small, predominantly white, male samples.
In order to draw more definitive conclusions about HF decision-making and generalize findings for translation into practice, research rigorously examining a broader spectrum of HF decision-making is critically needed.
Acknowledgments
DISCLOSURES/FUNDING: Financial support for this study was provided by: the National Institutes of Health [NIH 1 F31 NR014750-01, NIH/NINR T32 NR012704, NIH/NINR T32 NR 007968, NIH 5TL1TR001078-02, NIH/NINR T32 NR 013456-03]; American Nurses Foundation/Southern Nursing Research Society Research Award; Sigma Theta Tau International Nu Beta Chapter Research Award, Heart Failure Society of America Nurse Research Grant; and the Jonas Nurse Leaders Scholar Program The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
Appendix A. Database Search Terms
PubMed
(("Heart Failure"[Mesh] OR "heart failure" [tiab])) AND ("Decision Making"[Mesh] OR "decision making")
Preference AND ("Heart Failure"[Mesh] OR "heart failure" [tiab])
PsychINFO
(DE "Decision Making" OR DE "Choice Behavior" OR "decision making") AND "heart failure"
(DE "Preferences" OR preferences OR preference) AND “heart failure”
CINAHL
((MH "Decision Making+") OR "decision making) AND ((MH "Heart Failure+") OR "heart failure")
(Preference OR Preferences) AND ((MH "Heart Failure+") OR "heart failure")
References
- 1.Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goldstein NE, Lynn J. Trajectory of end-stage heart failure: the influence of technology and implications for policy change. Perspect Biol Med. 2006;49(1):10–18. doi: 10.1353/pbm.2006.0008. [DOI] [PubMed] [Google Scholar]
- 3.Meyer TE, Kiernan MS, McManus DD, Shih J. Decision-making under uncertainty in advanced heart failure. Curr Heart Fail Rep. 2014;11(2):188–196. doi: 10.1007/s11897-014-0195-7. [DOI] [PubMed] [Google Scholar]
- 4.Warren C, McGraw AP, Van Boven L. Values and preferences: defining preference construction. Wiley Interdiscip Rev Cogn Sci. 2011;2(2):193–205. doi: 10.1002/wcs.98. [DOI] [PubMed] [Google Scholar]
- 5.Dev S, Clare RM, Felker GM, Fiuzat M, Warner Stevenson L, O’Connor CM. Link between decisions regarding resuscitation and preferences for quality over length of life with heart failure. Eur J Heart Fail. 2012;14(1):45–53. doi: 10.1093/eurjhf/hfr142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levenson JW, McCarthy EP, Lynn J, Davis RB, Phillips RS. The last six months of life for patients with congestive heart failure. [Accessed January 23, 2014];J Am Geriatr Soc. 2000 48(5 Suppl):S101–S109. doi: 10.1111/j.1532-5415.2000.tb03119.x. http://www.ncbi.nlm.nih.gov/pubmed/10809463. [DOI] [PubMed] [Google Scholar]
- 7.Formiga F, Chivite D, Ortega C, Casas S, Ramón JM, Pujol R. End-of-life preferences in elderly patients admitted for heart failure. QJM. 2004;97(12):803–808. doi: 10.1093/qjmed/hch135. [DOI] [PubMed] [Google Scholar]
- 8.Formiga F, Olmedo C, López-Soto A, Navarro M, Culla A, Pujol R. Dying in hospital of terminal heart failure or severe dementia: the circumstances associated with death and the opinions of caregivers. Palliat Med. 2007;21(1):35–40. doi: 10.1177/0269216306073256. [DOI] [PubMed] [Google Scholar]
- 9.Agård A, Hermerén G, Herlitz J. Should cardiopulmonary resuscitation be performed on patients with heart failure? The role of the patient in the decision-making process. [Accessed October 8, 2014];J Intern Med. 2000 248(4):279–286. doi: 10.1046/j.1365-2796.2000.00732.x. http://www.ncbi.nlm.nih.gov/pubmed/11086637. [DOI] [PubMed] [Google Scholar]
- 10.Evangelista LS, Motie M, Lombardo D, Ballard-Hernandez J, Malik S, Liao S. Does preparedness planning improve attitudes and completion of advance directives in patients with symptomatic heart failure? J Palliat Med. 2012;15(12):1316–1320. doi: 10.1089/jpm.2012.0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Habal MV, Micevski V, Greenwood S, Delgado DH, Ross HJ. How aware of advanced care directives are heart failure patients, and are they using them? Can J Cardiol. 2011;27(3):376–381. doi: 10.1016/j.cjca.2010.12.067. [DOI] [PubMed] [Google Scholar]
- 12.Kobza R, Erne P. End-of-life decisions in ICD patients with malignant tumors. Pacing Clin Electrophysiol. 2007;30(7):845–849. doi: 10.1111/j.1540-8159.2007.00771.x. [DOI] [PubMed] [Google Scholar]
- 13.Altice NF, Madigan EA. Factors associated with delayed care-seeking in hospitalized patients with heart failure. Heart Lung. 2012;41(3):244–254. doi: 10.1016/j.hrtlng.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 14.Jurgens CY. Somatic awareness, uncertainty, and delay in care-seeking in acute heart failure. Res Nurs Health. 2006;29(2):74–86. doi: 10.1002/nur.20118. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez KL, Appelt CJ, Switzer GE, Sonel AF, Arnold RM. Veterans’ decision-making preferences and perceived involvement in care for chronic heart failure. Heart Lung. 37(6):440–448. doi: 10.1016/j.hrtlng.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Jaarsma T, Abu-Saad HH, Dracup K, Halfens R. Self-care behaviour of patients with heart failure. [Accessed February 9, 2014];Scand J Caring Sci. 2000 14(2):112–119. http://www.ncbi.nlm.nih.gov/pubmed/12035274. [PubMed] [Google Scholar]
- 17.Etchegary H, Pullman D, Simmonds C, Young T-L, Hodgkinson K. “It had to be done”: Genetic testing decisions for Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) Clin Genet. 2014 Sep; doi: 10.1111/cge.12513. [DOI] [PubMed] [Google Scholar]
- 18.Lowey SE, Norton SA, Quinn JR, Quill TE. Living with advanced heart failure or COPD: Experiences and goals of individuals nearing the end of life. Res Nurs Heal (RES NURS Heal. 2013;36(4):349–358. doi: 10.1002/nur.21546. [DOI] [PubMed] [Google Scholar]
- 19.Van Deursen VM, Urso R, Laroche C, et al. Co-morbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail. 2014;16(1):103–111. doi: 10.1002/ejhf.30. [DOI] [PubMed] [Google Scholar]
- 20.Stewart GC, Givertz MM. Mechanical circulatory support for advanced heart failure: patients and technology in evolution. Circulation. 2012;125(10):1304–1315. doi: 10.1161/CIRCULATIONAHA.111.060830. [DOI] [PubMed] [Google Scholar]
- 21.Riegel B, Dickson VV. A situation-specific theory of heart failure self-care. J Cardiovasc Nurs. 2008;23(3):190–196. doi: 10.1097/01.JCN.0000305091.35259.85. [DOI] [PubMed] [Google Scholar]
- 22.Meyer S, van der Meer P, van Deursen VM, et al. Neurohormonal and clinical sex differences in heart failure. Eur Heart J. 2013;34(32):2538–2547. doi: 10.1093/eurheartj/eht152. [DOI] [PubMed] [Google Scholar]
- 23.Kindermann I, Fischer D, Karbach J, et al. Cognitive function in patients with decompensated heart failure: the Cognitive Impairment in Heart Failure (CogImpair-HF) study. Eur J Heart Fail. 2012;14(4):404–413. doi: 10.1093/eurjhf/hfs015. [DOI] [PubMed] [Google Scholar]
- 24.Holmes-Rovner M, Kroll J, Schmitt N, et al. Patient Satisfaction with Health Care Decisions: The Satisfaction with Decision Scale. Med Decis Mak. 1996;16(1):58–64. doi: 10.1177/0272989X9601600114. [DOI] [PubMed] [Google Scholar]
- 25.Bunn H, O’Connor A. Validation of client decision-making instruments in the context of psychiatry. [Accessed October 10, 2014];Can J Nurs Res. 1996 28(3):13–27. http://www.ncbi.nlm.nih.gov/pubmed/8997937. [PubMed] [Google Scholar]
- 26.Brehaut JC, O’Connor AM, Wood TJ, et al. Validation of a decision regret scale. [Accessed December 18, 2013];Med Decis Making. 2003 23(4):281–292. doi: 10.1177/0272989X03256005. http://www.ncbi.nlm.nih.gov/pubmed/12926578. [DOI] [PubMed] [Google Scholar]