Abstract
Background
Using Smartphone technology and text messaging for health is a growing field. This type of technology is well integrated into the lives of young adults. However, few studies have tested the effect of this type of technology to promote weight loss in young adults
Objective
The purpose of this study was to test the effectiveness of a behaviorally-based Smartphone application for weight loss combined with text messaging from a health coach on weight, body mass index, and waist circumference in young adults as compared to a control condition.
Methods
Sixty-two young adults, aged 18-25 years, were randomized to receive: 1) a Smartphone application + health coach intervention and counseling sessions or 2) control condition with a counseling session. All outcomes measures were tested at baseline and 3 months. These included weight, BMI, waist circumference, dietary habits, physical activity habits, and self-efficacy for healthy eating and physical activity.
Results
The sample was 71% female and 39% white, with an average age of 20 years and average BMI of 28.5kg/m2. Participants in the Smartphone + health coach group lost significantly more weight (p=0.026) and had a significant reduction in both BMI (p=0.024) and waist circumference (p<0.01) compared to controls.
Conclusions
The results of this weight loss trial support the use of Smartphone technology and feedback from a health coach on improving weight in a group of diverse young adults.
Introduction
Overweight and obesity are a major public health concern in the United States (US). According to data published in 2014 by the National Health and Nutrition Examination Survey, more than one-half of US adults (60.3%) aged 20-39 years are overweight or obese with a body mass index ≥ 25. (1) Weight gain is specifically a concern in college-aged individuals. Although the common theory that college freshman gain 15 pounds has been disproven on most accounts (2), studies have shown that many students do in fact gain weight. (3-4) A survey conducted in 2014 by the American College Health Association reported that greater than 34% of undergraduate students are overweight or obese and this number increases to 40% when surveying graduate students. (5) Being overweight greatly increases one’s risk for stroke, heart disease, type 2 diabetes, and some forms of cancer. (6) Therefore, interventions to combat weight gain during these years are needed for healthy outcomes later in life.
The behaviors of college-aged individuals put them at risk for weight gain. Specifically, poor eating habits, decreased physical activity, decreased fruit and vegetable consumption and increased alcohol consumption all contribute to weight gain. (7-8) The American College Health Association reports that 65% of students consume less than 2 servings of fruit/vegetables combined per day and that greater than 50% of students report consuming alcohol in the past 9 days. (5) Of those consuming alcohol, 24% of students reported having 7 or more drinks the last time they drank. (5)
Technology is well integrated into the lives of young adults. Currently, 85% of young adults, aged 18-29 years, own a Smartphone. Among those young adults owning a Smartphone, 100% use their smartphone to send and receive text messages. (9) Additionally, 77% of young adults have used their Smartphone to look up health information. (9) A recent focus group study conducted by the first author identified that young adults are interested in utilizing Smartphone technology for weight loss, however they know very little about the availability of different applications to assist with weight loss. (10)
Interventions for weight loss in this population have proven to be successful using various strategies. One study utilized technology and showed greater weight loss in a group that received a social networking site and text messages (−2.4kg) compared to a social networking site alone (−0.63kg). (11) Another study utilizing the Internet reported increased fruit and vegetable consumption, although no differences in weight were noted. (12)
Smartphone technology can provide many tools to help one lose weight. However, there is limited knowledge on the use of Smartphone technology for weight loss in young adults. Therefore, the purpose of this study was to test the effectiveness of a behaviorally-based Smartphone application combined with text messaging from a health coach on weight, body mass index (BMI), and waist circumference in young adults as compared to a control condition.
Methods
The Young Adult Weight Loss Study was a randomized, controlled trial in which participants were randomly assigned to intervention or control. Assessments were completed at baseline and 3 months between 2014-2015. All participants provided informed written consent at baseline. The protocol was approved by the Johns Hopkins University Institutional Review Board. Study data were collected via paper/pencil questionnaires and a web-based program for dietary recall. The Research Electronic Data Capture (REDCap), a secure, web-based application, was used to store data.
Setting and Participants
Participants were recruited in and around the Johns Hopkins University campuses using many strategies including posters/flyers, Facebook, email announcements, and word of mouth. Individuals between 18-25 years of age with a BMI between 25-40kg/m2 who owned an iPhone or Android phone were eligible to participate. Participants were not required to be a college undergraduate or graduate student. Interested individuals contacted the primary investigator to set up a telephone screening, if the individual qualified, they were asked to set-up a baseline visit. Participants were excluded if they were currently participating in another structured weight loss program, were taking weight loss medications, were diagnosed with Type I diabetes, or currently pregnant or planning to become pregnant in the next 3 months. Individuals were also excluded if they currently exercised more than 150 minutes/week at moderate intensity, or have had symptoms of disordered eating in the previous 6 months. Symptoms of disordered eating were defined as answering yes to any question assessing binging/purging, laxative/diet pill use, and treatment for an eating disorder from the EAT-26 questionnaire. (13) Randomization to Smartphone + Health Coach or control by blocks of 4 occurred after data were collected at the baseline visit. All participants received a $25 gift card for participation.
Outcome measures
Data on the outcome measures were collected on all participants at baseline and 3 months. Body weight was measured using the Tanita BS-549 scale with the participant in light clothing. Height was measured using a wall stick measurement. BMI was then calculated using weight in kilograms/height in meters squared. Waist circumference was measured two times and then averaged according to the obesity guidelines. (14)
Physical activity was evaluated with the Godin Leisure-Time Exercise Questionnaire. The survey is self-administered and assesses strenuous, moderate, and mild activity over a 7-day period. (15) This survey method has been proven to be both valid and reliable in adults, with test-retest scored ranging from 0.74-0.81. (16) Nutrition data was collected using the National Cancer Institute’s ASA-24. The ASA-24 is a web-based, automated self-administered 24-hour recall of foods and was filled out on the participant’s computer. The ASA-24 provides analysis on calories, nutrients, and food group estimates. (17) It has been proven to be valid in an adult population, with the ASA-24 performing very close (87% matching) to standardized interviewer-administered 24-hour food recalls. (17) Information obtained from the ASA-24 included caloric intake, food pyramid equivalents, and nutrients from all foods reported according to the Food and Nutrient Database for Dietary Studies. (17)
Self-efficacy for healthy eating and exercise were evaluated with two questionnaires. Both of the self-efficacy scales were self-administered by the participant. The Self-Efficacy for Healthy Eating was a 13-item questionnaire that explores a person’s belief in their ability to make better food choices in given situations. A reliability coefficient of 0.87 indicated high internal consistency on the scale tested in a group of adults, ages 19-64 years. (18) Self-efficacy for physical activity was assessed using a 14-item questionnaire called the Self-Efficacy for Exercise Scale. This questionnaire assessed an individual’s belief in their ability to exercise in given situations. This scale was determined to be reliable and valid in a population of adults, with an internal consistency of 0.90 and a test-retest correlation was 0.67. (19)
Interventions
The behavioral intervention was based on self-efficacy theory, a construct of social cognitive theory (SCT), which was used in our prior pilot study that focused on Smartphone applications for weight loss in adults. (20) Self-efficacy theory states there are four ways to increase one’s self-efficacy: mastery experience, social modeling, social support, and verbal persuasion. (21) These 4 mechanisms were built into the intervention, which focused on increasing the participant’s self-efficacy to achieve better health outcomes related to weight loss. The goals for both groups were to lose 1-2 pounds per week and increase participation in physical activity. Participants were encouraged to exercise at least 150 minutes per week at moderate intensity, which would meet the Physical Activity Guidelines for Americans. (22) Both groups received a one-time counseling session prior to randomization. This was a 20-minute session that discussed healthy eating, limiting alcohol and sugar sweetened beverages, and increasing physical activity. Following this session, participants were randomized to one of two groups, control or Smartphone + Health Coach (intervention) for the three month study period.
Smartphone +Health Coach Group
Participants in this group were given an additional 30-40 minute counseling session on energy balance, nutrient density of foods, sugar-sweetened beverage consumption, and physical activity; therefore, they had two sessions total during their baseline visit. Participants were encouraged to identify specific goals that their health coach could help them achieve.
Participants were also guided to download and use the Lose it! application. This application is a free, commercially available Smartphone application that is focused on nutrition and physical activity self-monitoring. Participants were encouraged to log all food and exercise into the daily log in the application. They were instructed to follow the caloric budget set by the application using the Mifflin equation. The application also offered social networking through a “friend” feature, which allowed individuals to view peer weight loss and physical activity participation, and also allowed the interaction between peers. Participants were encouraged to use this feature.
Individualized text messages were delivered to the participant’s Smartphone from a health coach. The participants were asked to not text their health coach back. Based on data from a focus group study conducted by the first author, the participants could choose any frequency of messages they wanted to receive from a health coach, anywhere from 1 time per week up to 3 times per day. (9) The Smartphone application provided the health coach with the ability to monitor and track all participant progress on a real-time basis and text messages focused on current diet or physical activity status (see Table 1). Texts were sent from the health coach’s cell phone at the specified time and frequency of the participant.
Table 1.
Example Text Messages
| Nutrition/Exercise Focus | Example Text Message |
|---|---|
| Physical Activity Guidelines for Americans | I noticed you came very close to meeting your goal of 150 minutes of exercise last week. Great job! Let’s work hard to meet that 150 minute goal this week |
| Physical Activity Social Support | Working out with a group can be fun and motivating! Reach out to friends today and do something you all enjoy! |
| Breakfast Consumption | Did you know that people who skip breakfast tend to snack more during the day? Try eating a balanced breakfast each morning! |
| Nutrient Density/Sugar-Sweetened Beverages | Drinking your calories does not provide a nutrient rich diet! Keep up the good work of drinking zero calorie beverages! |
Control Group
The control group was asked to not utilize any Smartphone applications focused on weight loss for the duration of the study. They received the Lose It! application with a training session at their 3-month visit.
Statistical Analysis
The study was powered to detect statistically significant differences in weight loss between the two groups. Using an effect size of 0.8, calculated from a similar study (10), an alpha of 0.05, and a power of 80%, the sample size was determined to be 51. The sample size was increased by 15% to allow for attrition, to give a total sample size of 60, or 30 per group. Group differences in baseline sociodemographic and anthropometric characteristics were examined using Wilcoxin rank-sum tests and chi-squared or Fisher’s Exact tests. The primary outcomes were changes from baseline to three months in weight in kilograms, BMI and waist circumference in centimeters. Secondary outcomes were changes in diet, physical activity, and self-efficacy for diet and physical activity. A completers analysis was performed using generalized linear models, which were used to test for group differences, time effects, and interactions between group*time. All statistical analyses were done using Statistical Analysis System (SAS).
Results
Baseline Characteristics
Baseline characteristics of participants by group are shown in Table 2. Of the 62 participants enrolled, 71% were female, 33.8% were Asian, and 12.9% were African American. The overall median age was 20.0 (18.0-25.0) years and median BMI was 28.5 (25.0-40.4). Although the sample included both non-college and college students, only 10% of study participants were not current undergraduate or graduate students. There were no significant differences in baseline characteristics between the two groups.
Table 2.
Baseline Sample Characteristics by Treatment Group
| Characteristics | Total | Control | Smartphone + Health Coach |
P value |
|---|---|---|---|---|
| n | 62 | 31 | 31 | |
| Age, years, median (range) | 20.0 (18.0-25.0) | 20.0 (18.0-24.0) | 20.0 (18.0-25.0) | 1 |
| Race, n (%) | ------- | ------- | ------- | 0.7917 |
| White | 24 (38.7) | 12 (38.7) | 12 (38.7) | |
| Black | 8 (12.9) | 5 (16.1) | 3 (9.7) | |
| Asian | 21 (33.8) | 9 (29.0) | 12 (38.7) | |
| Other | 9 (14.5) | 5 (16.1) | 4 (12.9) | |
| Sex, n (%) | ------- | ------- | ------- | 0.6322 |
| Male | 18 (29.0) | 8 (25.8) | 10 (32.3) | |
| Female | 44 (71.0) | 22 (71.0) | 21 (67.7) | . |
| BMI, kg/m2, median (range) | 28.5 (25.0-40.4) | 26.6 (25.0-39.7) | 29.0 (25.2-40.4) | 0.0898 |
| Waist Circumference, cm, median (range) |
93.8 (81.0-120.0) | 93.5 (81.0-120.0) | 95.8 (82.5-120.0) | 0.294 |
| Type Of Smartphone | ------- | ------- | ------- | 0.3493 |
| iPhone | 49 (79.0) | 23 (74.2) | 26 (83.9) | |
| Android Phone | 13 (21.0) | 8 (25.8) | 5 (16.1) |
BMI: Body mass index
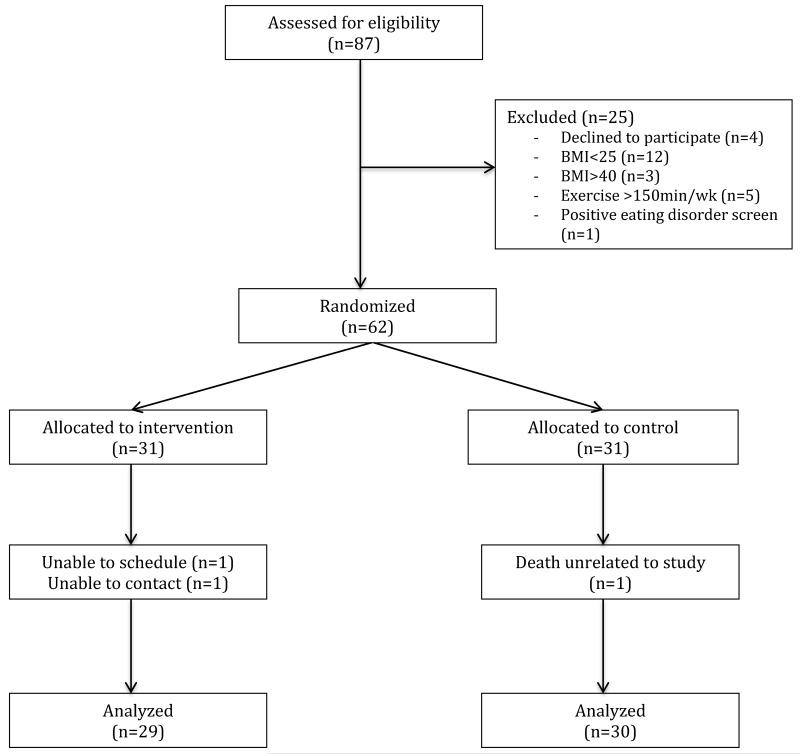
Recruitment and Retention: Figure 1 is the CONSORT diagram reporting the participant flow through the study. We assessed 87 individuals for eligibility.
Figure 1.
Study Flow Diagram
A total of 66 individuals met the criteria to participate. Of those, 4 (6%) declined to participate. The primary reason for refusal was lack of interest in participating in a study for 3 months. A total of 62 individuals were randomized to one of the two groups, which represented 71% of those who originally expressed interest in participating.
Fifty-nine (95%) returned at three months for follow-up measurements. Retention rates were similar in the two groups, 97% in the control group and 94% in the intervention group.
Weight, BMI, and Waist Circumference
Changes from baseline to 3 months can be found in Table 3. The control group gained a slight amount of weight (0.3kg) from baseline to 3 months, while participants in the Smartphone + Health Coach group lost a significant amount (−1.8kg, p<0.01); the difference in weight change between groups was statistically significant (p=0.026). The Smartphone group also had a significant decrease in BMI (p<0.01) and waist circumference (p<0.01). The differences in BMI and waist circumference changes between groups were also statistically significant (p=0.024 for BMI, p<0.01 for waist circumference). 7 (24%) of participants in the Smartphone group that completed the study lost enough weight to change their weight status; 5 (17%) moved into the normal weight category and 2 (7%) went from the obese category to overweight.
Table 3.
PRE- and POST- Intervention Measurements of Body Size and Self-Reported Behaviors
| Control | Smartphone + Health Coach | ||||||
|---|---|---|---|---|---|---|---|
| Body Size | PRE | POST | P1 | PRE | POST | P2 | P3 |
| Weight, kg, median (range) |
75.8 (63.0- 103.7) |
77.3 (66.0-106.2) |
0.764 | 82.8 (61-117.5) |
80.1 (57.1- 120.7) |
<0.01 | 0.026 |
| BMI, kg/m2, median (range) |
27.9 (25.0-39.7) | 27.6 (25.1-37.7) |
0.811 | 29.8 (25.5-40.2) |
28.4 (24.7-41.3) |
<0.01 | 0.024 |
| Waist Circumference, cm, median (range) |
93.3 (81-120) | 92.3 (81-117) |
0.964 | 95.8 (82.5-120) |
92.3 (77-122) |
<0.01 | <0.01 |
| Self-Reported Behaviors | |||||||
| Self-Efficacy (Healthy Eating), raw score (range) |
102 (60-130) | 109 (77-130) |
0.273 | 100 (66-120) |
106 (73-128) |
0.032 | 0.190 |
| Self-Efficacy (Exercise), raw score (range) |
87.5 (54-131) | 92 (42-124) |
0.258 | 86 (25-127) |
97 (30-140) |
0.151 | 0.541 |
| Physical Activity, 7 Day Recall, raw score (range) |
34 (3-108.5) | 36 (6.0-92) |
0.099 | 32 (0-72) |
43 (15-81) |
<0.01 | 0.503 |
Variables summarized as median (range) and compared from PRE-POST using Wilcoxon rank-sum test; between group interaction tested using repeated-measures ANOVA
Comparison of POST vs. PRE in Control group (Group effect in GLM for Control only)
Comparison of POST vs. PRE in Smartphone group (Group effect in GLM for Treated only)
Comparison of degree of change between groups (Group*Time Interaction with All Subjects)
Self-Reported Behaviors
Changes in self-reported behaviors can also be found in Table 3. The Smartphone + Health Coach group improved significantly in healthy eating self-efficacy (p=0.032). They also improved in overall physical activity performed (p<0.01), however, the differences were not significant when compared to the control group. Although both groups showed improvement in self-efficacy for physical activity, neither change was statistically significant. A comparison of degree of change between groups was also performed (Group*Time Interaction with All Subjects) adjusting for self-efficacy for healthy eating and exercise. When adjusting for self-efficacy for healthy eating, the data show that it is a slight mediator for change in weight with a p value shifting from p=0.026 for non-adjusted to p=0.052 when adjusted. Tests were also run for BMI and waist circumference, but there was no shift in p value, suggesting that self-efficacy for healthy eating does not entirely account for the treatment group effect.
A total of 37 (63%) participants completed the diet questionnaire at follow-up, 22 (73%) control and 15 (52%) smartphone + health coach. Table 4 displays the results from the ASA-24. The Smartphone group consumed significantly more fiber than the control condition at follow-up (p=0.049). There were no additional significant differences between the two groups at follow-up. However, participants in the Smartphone group consumed slightly more protein, more vegetables, more fruit, fewer total carbohydrates, and fewer added sugars than participants in the control arm.
Table 4.
Diet Quality of Study Participants During Follow-Up
| Total Study Population n=37 |
Control n=22 |
Smartphone + Health Coach n=15 |
P- Value |
|
|---|---|---|---|---|
| Diet Parameter, median (range) |
||||
| Calories | 1356.7 (586- 3288) |
1282.2 (831-3288) | 1670.5 (586-2689) | 0.221 |
| Protein | 61.1 (24.2-137.5) | 58.7 (24.2-110.3) | 78.5 (28.3-137.5) | 0.080 |
| Total Fat | 47.7 (14.0-129.9) | 44.8 (22.2-129.9) | 53.7 (14.0-111.5) | 0.394 |
| Total Carbs | 175.9 (73.3- 453.7) |
176.7 (73.3-453.7) | 170.0 (85.9-312.0) | 0.816 |
| Total Sugar | 61.8 (10.7-180.7) | 60.5 (14.8-180.7) | 65.0 (10.7-163.3) | 0.378 |
| Total Fiber | 14.6 (2.1-61.7) | 13.0 (2.1-61.7) | 18.4 (7.2-31.7) | 0.049 |
| Water | 1638.8 (717- 4277) |
1541.3 (851-4277) | 1684.1 (717-3869) | 0.816 |
| Total Sodium | 2781.4 (1223- 4784) |
2720.3 (1272-4542) | 2792.9 (1223- 4784) |
0.631 |
| Saturated Fat | 14.6 (2.6-43.9) | 13.3 (6.6-43.9) | 18.2 (2.6-41.2) | 0.506 |
| Total Vegetables | 1.1 (0.0-6.1) | 1.0 (0.0-6.1) | 1.2 (0.5-4.2) | 0.193 |
| Total Fruit | 0.7 (0.0-5.0) | 0.5 (0.0-5.0) | 0.9 (0.0-4.0) | 0.219 |
| Total Dairy | 1.1 (0.0-5.2) | 0.9 (0.0-5.2) | 1.4 (0.0-2.9) | 0.768 |
| Added Sugars | 7.1 (0.0-28.6) | 8.2 (0.7-28.6) | 5.6 (0.0-23.6) | 0.077 |
Continuous variables summarized as median (range) and compared between groups using Wilcoxon rank-sum test
Application Use and Text Messaging
The number of text messages sent varied from 1 per day to 3 times per day. No participants requested less than one message per day. Overall, 22 (71%) participants requested 3 messages per day, 4 (13%) requested two per day, and 5 (16%) requested 1 per day. All text messages were delivered to participants successfully; no error messages were received and all messages were labeled as delivered. Also, no issues were reported by participants.
All participants assigned to the Smartphone group logged exercise and diet. Over the three month time period, 6 (21%) participants logged exercise on > 50% of days and 18 (62%) logged diet on > 50% of days. Of those participants that logged on >50% of days, 3 (50%) logged physical activity on >75% of days and 7 (38%) logged diet on >75% of days. Table 5 displays the significant relationship between number of physical activity days logged and weight loss (0.03 kg weight loss per additional day of PA logging, p=0.026). The 6 participants who logged PA > 50% of the time lost 1.57 kg more than those who did not. When the threshold was reduced to 25% days logged, the 9 participants logging PA ≥25% of the time lost 1.43 kg more than those logging PA < 25% of the time. The same directional trends were observed with increased logging frequency for food, as well, but these were not significant (p=0.226), possibly due to overall good compliance with food logging.
Table 5.
Relationships Between Logging Consistency and Weight Change
| n / N | B | 95% CI | P-Value | |
|---|---|---|---|---|
| # Days Logged (PA) | - | −0.031 | (−0.05, −0.01) | 0.026 |
| Logging > 50% PA | 6 / 29 | −1.572 | (−3.31, 0.17) | 0.089 |
| # Days Logged (Food) | - | −0.021 | (−0.04, 0.01) | 0.226 |
| Logging > 50% Food | 18 / 29 | −0.702 | (−2.24, 0.74) | 0.375 |
Expected weight change per additional day of logging
Expected weight change for > 50% logging vs. < 50% logging
Discussion
To date, to the authors’ knowledge, this is the first trial focused on young adults that utilized both individualized text messages and a Smartphone application for weight loss. This trial showed that the use of a Smartphone application combined with individualized text messages is successful in helping individuals to lose weight. Individuals in the Smartphone group lost significantly more weight, had a significant decrease in BMI, and significantly decreased their waist circumference compared to the control group. However, many individuals did not meet the recommended goal in the study to lose 1-2 pounds per week. The mean weight loss in the Smartphone + Health Coach group was 4 pounds over the 3 month trial. These results are promising when examining other similar research. Although studies utilizing technology or text messaging have seen improvements in weight, many did not report any significant improvements when compared to a control condition. (23-24) It is possible that the combination of a Smartphone application with text messaging led to significant improvements in body weight in this group of young adults.
It is noteworthy that self-efficacy increased significantly for healthy eating (p=0.03) in the Smartphone + Health Coach group and both groups experienced an increase in self-efficacy for exercise, although this was not significant. It is possible there were differences in self-efficacy between males and females or based on racial category in this study, however these differences were not tested. Recent studies conducted in college aged individuals reported implications for testing the differences in self-efficacy between males and females and also indicate possible racial differences in self-efficacy for improving certain health behaviors. A study published in 2015 by Bruce et al (25) reported significantly lower self-efficacy for changing sugar sweetened beverage consumption in African American college males compared to white college males. In addition, a study examining Korean college students reported that self-efficacy for physical activity is a significant predictor of physical activity in Korean males but not in Korean females. (26) Future studies should include analyses on differences in self-efficacy but should also examine other components of social cognitive theory, such as social support or outcome expectations, which are known predictors of behaviors. (21)
An increase in logging into the Smartphone application for both physical activity and diet led to better outcomes with weight loss. It is therefore important that accountability be a focus in future interventions. Accountability in this study was exhibited through the behavior of logging into an application, however accountability could be achieved many different ways in upcoming trials. In trials that utilize technology, increasing compliance and accountability with Smartphone logging could be achieved through a counselor stressing the importance of logging during a session or more frequent reminders could be sent to participant phones.
There are several strengths to note in this study. Strengths of the study include the randomized design powered to detect significant differences between groups, use of a commercially available Smartphone application, and an attrition rate of only 5%. In addition, the study population was diverse, 38 (62%) participants were from a minority group and 21 (33%) identified as Asian and 8 (13%) identified as African American.
Study limitations include the small sample size and limited generalizability of the study population in that most were attending college at a single university on the east coast. Also, the study was of short duration (3 months) with no extended follow-up. Finally, it cannot be determined whether differences between groups were due to the health coach text messaging or the Smartphone application.
Conclusion
This randomized controlled trial using a Smartphone application for weight loss combined with individualized text messages has provided valuable information that the combination of self-monitoring via an application and feedback from a health coach is successful in helping young adults lose weight. The study had a meaningful impact on weight, BMI, and waist circumference. In future trials, a sample that includes equal amounts of individuals attending college and those not attending college could strengthen the generalizability of the results. Smartphone technology seems to be an appropriate resource to utilize when working with the young adult population and it has the potential to greatly impact the serious public health problem of obesity.
Acknowledgments
Research in this publication was supported by the National Institute of Nursing Research of the National Institute of Health under award numbers 1T32NR012704 and F31NR013811. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Funding: – T32 Cardiovascular Research Training Grant
Grant Number: 1T32NR012704-01
F31, National Research Service Award
Grant Number: F31 NR 013811
Footnotes
Disclosure: No conflicts of interest
Contributor Information
Janna D. Stephens, Ohio State University, College of Nursing. Columbus OH, United States.
Allison M. Yager, Johns Hopkins University, School of Nursing. Baltimore MD, United States.
Jerilyn Allen, Johns Hopkins University, School of Nursing. Baltimore MD, United States.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holm-Denoma JM, Joiner TE, Vohs KD, Heatherton TF. The “freshman fifteen” (the “freshman five” actually): predictors and possible explanations. Health Psychology. 2008;27(supplement 1):S3–S9. doi: 10.1037/0278-6133.27.1.S3. [DOI] [PubMed] [Google Scholar]
- 3.Economos CD, Hildebrandt ML, Hyatt RR. College freshman stress and weight change: differences by gender. American Journal of Health Behavior. 2008;32(1):16–25. doi: 10.5555/ajhb.2008.32.1.16. [DOI] [PubMed] [Google Scholar]
- 4.Gropper SS, Newton A, Harrington P, Simmons KP, Connell LJ, Ulrich P. Body composition changes during the first two years of university. Preventive Medicine. 2011;52(1):20–22. doi: 10.1016/j.ypmed.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 5.American College Health Association . American College Health Association- National College Health Assessment II: Undergraduate Students. Reference group executive summary Spring 2014. Hanover, MD: 2014. [Google Scholar]
- 6.Burton BT, Foster WR, Hirsch J, VanItallie TB. Health implications of obesity: NIH consensus development conference. Int J Obes Relat Metab Disord. 1985;9:155–169. [PubMed] [Google Scholar]
- 7.Kasparek DG, Corwin SJ, Valois RF, Sargent RG, Morris RL. Selected health behaviors that influence college freshman weight change. Journal of American College Health. 2008;56(4):437–444. doi: 10.3200/JACH.56.44.437-444. [DOI] [PubMed] [Google Scholar]
- 8.Lloyd-Richardson EE, Lucero ML, DiBello JR, Jacobson AE, Wing RR. The relationship between alcohol use, eating habits and weight change in college freshmen. Eating Behaviors. 2008;9(4):504–508. doi: 10.1016/j.eatbeh.2008.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Smith A. [Accessed on April 20th 2015];U.S. Smartphone Use in 2015. 2015 Apr 1; http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/
- 10.Stephens JD, Moscou-Jackson G, Allen JK. Young adults, technology and weight loss: A focus group study. Journal of Obesity. 2015 doi: 10.1155/2015/379769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Napolitano M, Hayes S, Bennett G, Ives A, Foster GD. Using facebook and text messaging to deliver a weight loss program to college students. Journal of Obesity. 2013;21(1):25–31. doi: 10.1002/oby.20232. [DOI] [PubMed] [Google Scholar]
- 12.Lachausse RG. My student body: effects of an internet-based prevention program to decrease obesity among college students. J Am Coll Health. 2012;60(4):324–30. doi: 10.1080/07448481.2011.623333. doi: 10.1080/07448481.2011.623333. [DOI] [PubMed] [Google Scholar]
- 13.Garner DM, Olmsted MP, Bohr Y, Garfinkel PE. The eating attitudes test: psychometric features and clinical correlates. Psychological Medicine. 1982;12(4):871–878. doi: 10.1017/s0033291700049163. [DOI] [PubMed] [Google Scholar]
- 14.National Heart, Lung and Blood Institute . Guidelines on Overweight and Obesity: Electronic Textbook. National Institute of Health; [Google Scholar]
- 15.Godin G, Shephard RJ. Godin Leisure-Time Exercise Questionnaire. Medicine and Science in Sports and Exercise. 1997 Jun 29;(Supplement):S36–S38. [Google Scholar]
- 16.Jacobs DR, Ainsworth BE, Hartman TJ, Leon AS. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc. 1993;25(1):81–91. doi: 10.1249/00005768-199301000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Kirkpatrick SI, Subar AF, Douglass D, Zimmerman TP, Thompson FE, Kahle LL, George SM, Dodd KW, Potischman N. Performance of the Automated Self-Administered 24-hour Recall relative to a measure of true intakes and to an interviewer-administered 24-h recall. Am J Clin Nutr. 2014 Apr 30;100(1):233–240. doi: 10.3945/ajcn.114.083238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schouwstra SJ. The nutrition efficacy scale: Development and construct validation using the deductive design. UvA-Dare. 2014 [Google Scholar]
- 19.Wilson M, Allen DD, Li JC. Improving measurement in health education and health behavior research by using item response modeling: Comparison with the classical test theory approach. Health Education Research. 2006;21(1):19–32. doi: 10.1093/her/cyl053. [DOI] [PubMed] [Google Scholar]
- 20.U.S. Department of Health and Human Services Physical Activity Guidelines for Americans. 2008 Retrieved from http://health.gov/paguidelines.
- 21.Glanz K, Rimer BK, Viswanath K. Health Behavior and Health Education. 4th Edition Jossey-Bass; San Francisco, CA: 2008. [Google Scholar]
- 22.Allen JK, Stephens JD, Dennison-Himmelfarb C, Stewart KJ, Hauck S. Randomized controlled pilot study testing the use of smartphone technology for obesity treatment. Journal of Obesity. 2013 doi: 10.1155/2013/151597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zuercher JL. Developing Strategies for Helping Women Improve Weight-Related Health Behaviors. University of North Carolina at Chapel Hill; Chapel Hill, NC: 2009. [Google Scholar]
- 24.Hebden L, Cook A, van der Ploeg HP, King L, Bauman A, Allman-Farinelli M. A mobile health intervention for weight management among young adults: A pilot randomized controlled trial. J Hum Nutr Diet. 2014 Aug;27(4):322–32. doi: 10.1111/jhn.12155. [DOI] [PubMed] [Google Scholar]
- 25.Bruce MA, Beech BM, Thorpe RJ, Jr, Griffith DM. Racial disparities in sugar-sweetened beverage consumption change efficacy among male first-year college students. Am J Mens Health. 2015 doi: 10.1177/1557988315599825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi JY, Chang AK, Choi EJ. Sex differences in social cognitive factors and physical activity in Korean college students. J Phys Ther Sci. 2015;27(6):1659–64. doi: 10.1589/jpts.27.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]