Abstract
This study investigated the effects of workplace clean indoor air law (CIAL) coverage on worksite compliance with CIALs, smoking participation among indoor workers, and secondhand smoke (SHS) exposure among non-smoker indoor workers. This study improved on previous research by using the probability of a resident in a county covered by workplace CIALs taking into account the state, county, and city legislation. The county-level probability of being covered by a CIAL is merged into two large nationally representative US surveys on smoking behaviors: Tobacco Use Supplement of the Current Population Survey (2001–2010) and Behavioral Risk Factor Surveillance System (2000–2006) based on the year of the survey and respondent’s geographic location to identify respondents’ CIAL coverage. This study estimated several model specifications of including and not including state or county fixed effects, and the effects of workplace CIALs are consistent across models.
Increased coverage by workplace CIALs significantly increased likelihood of reporting a complete smoking restriction by 8% and 10% for the two different datasets, decreased smoking participation among indoor workers by 12%, and decreased SHS exposure among non-smokers by 28%.
Keywords: clean indoor air law coverage, local ordinances, smoking
1. Introduction
Secondhand smoke (SHS) causes cardiovascular, pulmonary, and cancer-related morbidity and mortality in non-smokers (US Department of Health and Human Services, 2006, 2010). Since the release of the 1986 U.S. Surgeon General’s report, which linked the SHS to higher rates of lung cancer in nonsmokers, U.S. public awareness of the potential harm from the SHS has increased. To reduce public SHS exposure, U.S. local and state governments have increasingly implemented clean indoor air laws (CIALs) that restrict smoking in workplaces, restaurants, bars, schools, public places, and casinos.1
While the CIALs are implemented to reduce SHS exposure, the theory of tobacco social denormalization predicts that CIALs, combined with other strategies including tobacco taxation and the promotion of anti-tobacco industry sentiment will shift social norms towards anti-smoking thereby encouraging either cessation or decreased tobacco consumption among current smokers, and preventing tobacco uptake by new users (Hammond et al. 2006; Biener et al. 2000; Bauer et al. 2000). In particular, CIALs are hypothesized to shift norms and practices around smoking by moving the behavior outdoors and inconveniencing smokers, marking the behavior as socially unacceptable (US Department of Health and Human Services, 2000). A report from the U.S. Bureau of Labor Statistics indicated that employed people spent a substantial proportion of time at work,2 and therefore, their smoking behaviors would be expected to be affected by their workplace smoking restrictions. A growing number of papers in economics and public health have examined whether the smoking restrictions in public places reduce smoking prevalence or cigarette consumption by smokers.
Early studies focused on the smoking restrictions adopted in individual worksites, as opposed to examining the broader trend of workplace CIAL implementation; these studies investigated the relationship between workplace smoking ban and changes in smoking behaviors. Some studies focused on a particular occupational location over a period of time, and compared individual respondents’ smoking behaviors before and after the adoption of workplace smoking bans (Kinne, Kristal, White, & Hunt, 1993; Sorsensen, Rigotti, Rosen, Pinney, & Prible, 1991; Stillman et al., 1990; Woodruff, Rosbrook, Pierce, & Glantz, 1993) and others compared smoking behaviors between group of respondents in workplaces with and without smoking bans (Longo et al., 1996). Fichtenberg & Glantz (2002) conducted a systematic review of 26 studies using the data between 1984 and1993 on the effects of smokefree workplaces and concluded that the smokefree workplaces are associated with reductions in smoking prevalence by 3.8 percentage points and reduced number of cigarettes per day by 3.1. Hopkins et al. (2010) reviewed 21 studies published between 1976 and 2005 on the effects of smokefree workplaces on smoking prevalence, and concluded that the median association between smokefree workplaces and reduced smoking prevalence is 3.4 percentage points.
Recently, several studies took the advantages of the time-location variations of the implementation of comprehensive CIALs to study the impacts of state-level CIALs on smoking prevalence and smoking intensity; such broader studies avoid the potential methodological weakness of self-selection bias due to possible nonrandom match of smokers to firms that could bias the estimated impact of smoking bans (Yurekli & Zhang, 2000; Tauras, 2006; Chaloupka 1992; Wasserman et al. 1991; Powell et al. 2005; Bitler, Carpenter, & Zavodny (2010); Liu (2010); Adda & Cornaglia (2010)).
Although most of the previous studies concluded that state CIALs significantly reduced smoking behaviors, the more recent studies claimed that there is no significant effect of state CIALs on the implementation of workplace smoking bans and worker smoking behaviors. For example, Bitler, Carpenter, & Zavodny (2010) compared smoking behaviors of workers who worked at the locations covered by the venue-specific state CIALs and those who did not. The authors found that report having a worksite smoking ban did not vary between the workers with and without state-level workplace CIALs, and consequently venue-specific state CIALs did not affect smoking behaviors in any targeted venue, except bars. As a result, Bitler, Carpenter, & Zavodny (2010) suggested that the smoking reductions associated with state CIALs found in previous research may be attributable to some other cause, and not to workplace CIALs. Similarly, Liu (2010) separated smoking behaviors into smoking initiation and cessation, and found no evidence that state CIALs affected either of these two behaviors.
A weakness in the current literature is that most studies either look at individual workplaces or examine the effects of state-level CIALs. However, CIAL passage may occur at the local level as well. Only, two studies took into account the influences of local smokefree ordinances on workplace smoking. Carpenter (2009) studied the effects of local workplace smoking ordinances in Ontario, Canada, on the worksite CIAL compliance and exposure at work. This study found that local ordinances significantly increased reported workplace compliance with CIALs, and decreased SHS exposure for blue collar workers, but not for other workers (whose workplaces had often implemented voluntary smoking bans prior to the passage of CIALs). Adda & Cornaglia (2010) investigated the effects of smoking bans on smoking behaviors and SHS exposure, but did not examine local vs state coverage. They constructed a state level estimate of total CIAL coverage, by computing the total population within the state covered by local and state CIALs in workplaces, or restaurants and bars. The CIAL information at state and local levels was obtained from the American Nonsmokers Right Foundation database. They found restaurant and bar CIAL coverage, but not workplace CIAL coverage, significantly reduced smoking prevalence: a state went from 0 to 100% coverage in restaurant and bar significantly reduced the general prevalence by 2 percentage points.
Indeed, it is important to include the effects of existing local CIALs when assessing the marginal effects of enacting a subsequent state CIAL. For example, although West Virginia had no statewide workplace CIAL, in 2009 many counties within West Virginia, including Kanawha County with the largest county population, has already adopted workplace CIALs, resulting in 74% of the population being covered by CIALs. Solely relying on the state level CIALs would completely miss the actual CIAL coverage in local level.
This study investigated the impacts of workplace CIAL coverage on three outcomes: smoking participation among indoor workers, worksite compliance with the workplace CIALs, and SHS exposure among non-smoker workers, accounting for the effects of the coverage of county CIALs as well as municipal CIALs and existing local legislation when state CIALs took effect.
This study contributes to the existing literature in three ways. First, this study contributed in using the probability that an individual in any given county is covered by workplace smoking bans in a county by taking into account all workplace CIALs at city, county, and state levels. It extended Adda & Cornaglia (2010) by investigating the impacts of workplace CIAL coverage in county level instead of state level. The reason for doing so is because the smokefree legislation coverage in local level captures much precisely on individual’s actual law protections compared to the coverage in state level. Indeed, many previous studies investigating the effects of CIALs using large national-level sample of the US population focused on state level laws, and did not take into account of the situations where some local jurisdictions such as counties (or cities) may have already implemented such CIALs prior to the enactment of either the state (or county) CIAL. Such misclassification of CIALs may result in estimated law effect to be biased toward zero and yield non-significant effects.
Second, this study includes all indoor workers and investigates the relationship between workplace CIALs on smoking behavior using two large nationally representative US surveys: the Tobacco Use Supplement of the Current Population Survey (TUS-CPS) and Behavioral Risk Factor Surveillance System (BRFSS). Finally, this study focused on the period when a large number of local and state US jurisdictions implemented workplace CIALs (2000–2010). As indicated in Figure 1, the percentage of US population protected by a 100% workplace CIAL at the city, county, or state level increased significantly from 3% for private workplaces and 15% for public workplaces in 2000 to 54% and 81% in 2009. Worksites may voluntarily adopted smoking bans prior to the workplace CIALs; according to BRFSS in 2000, the first study wave, 72% of indoor workers reported that smoking is not allowed in any common or their work areas. This study period provided enough variations of CIAL implementation in estimation of the effects of CIALs on smoking related outcomes.
Figure 1. Trend of proportion of population covered by workplace CIALs in state, county, and city levels and smoking prevalence, 2000–2009.
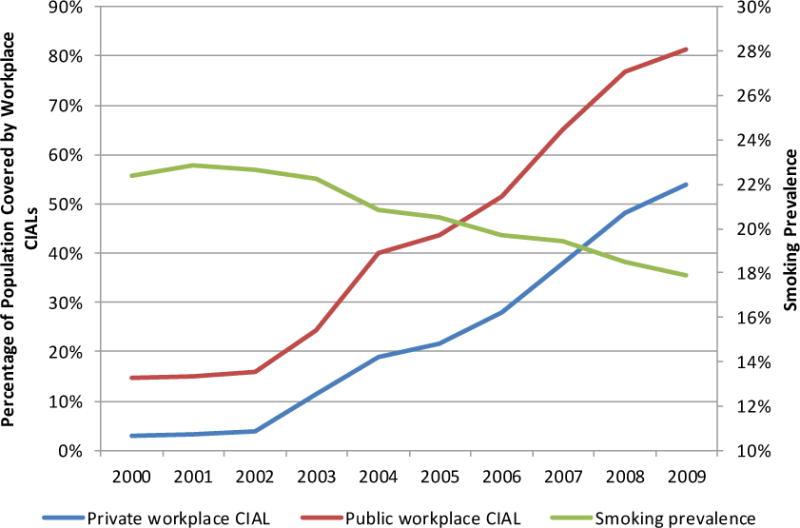
Source: Authors’ computation using data from American Nonsmokers’ Rights Foundation, the Census-Estimated Population (CEP) Cities and Towns, Behavioral Risk Factor Surveillance System, and Tobacco Use Supplements to Current Population Survey.
2. Data
Individual-level data came from two sources: the Tobacco Use Supplements to Current Population Survey (TUS-CPS) 2001/2002, 2003, 2006/2007, and 2010, and the Behavioral Risk Factor Surveillance System (BRFSS) 2000–2006.
The TUS-CPS is a nationally representative cross-sectional survey of households conducted by the US Census Bureau sponsored by National Cancer Institute and, since 2001, co-sponsored by the Centers for Disease Control and Prevention. Each survey provides detailed information on smoking status, smoking history, workplace and home smoking policy, attitudes about smoking, as well as economic and demographic characteristics for a sample of over 100,000 individuals aged 15 years and older.
The Behavioral Risk Factor Surveillance System (BRFSS) is a state-based system of health surveys that collects information on health risk behaviors, preventive health practices, and health care access primarily related to chronic disease and injury from a random sample of households with telephone within each US state. BRFSS was established in 1984 by the Centers for Disease Control and Prevention (CDC), and more than 350,000 adults are interviewed each year. This study used the 2000–2006 BRFSS data. This study focused on indoor workers (i.e., excluded outdoor workers) because the worksite CIALs restrict smoking indoors. This study does not include the BRFSS waves after 2006 because after 2006 the BRFSS stopped asking employed respondents whether they work indoors or outdoors.
Because CIAL coverage was calculated at the county level, this analysis includes only those respondents in the TUS-CPS and BRFSS with publicly available county codes. For confidentiality reason, only the large counties are identified with county codes; so 38% of respondents in TUS-CPS and 85% of BRFSS respondents have county codes.
The probability of being covered by a CIAL in a county was computed as the percentage of county population covered by a workplace CIAL using two data sets: the Census-Estimated Population (CEP) Cities and Towns: Vintage 2009 All States, All Geographies data file and the American Nonsmokers’ Rights Foundation (ANRF) US Tobacco Control Database (Gonzalez et al 2013).
The ANRF database includes tobacco control ordinances, bylaws, and board of health regulations for US jurisdictions (city, county, and state). The database provides the detailed information on CIALs coded from the text of the law including date of passage, date of implementation, venues covered by the law (public workplaces, private workplaces, restaurants, and bars), strength of the laws (100% smokefree with no exemption and no designated areas, partial restrictions with some exemption or designated smoking areas, no restrictions at all), and jurisdiction of the law (state, town, whole county, unincorporated area of the county). The ANRF database includes law repeals and modifications. The current law status as of July 1 for the year in question was used when calculating coverage. The CEP data file contains the population of incorporated and unincorporated jurisdictions within US state. As described in detail in Gonzalez et al (2013), the fraction of the population within each US county covered by a comprehensive CIAL was calculated by combining the ANRF and CEP databases to identify the fraction of each counties’ population covered by a 100% smokefree law. A comprehensive workplace CIAL was defined as a law which bans smoking indoors with no exceptions. Gonzalez et al (2013) calculated population CIAL coverage by comprehensive private workplace CIALs and public workplace CIALs separately. In order to be designated comprehensive, the law cannot include exceptions to the smokefree rule. For example, if the law allowed for separately ventilated smoking rooms within a venue, venue size restrictions, or sole proprietor restrictions it was not designated as a comprehensive law. When calculating population coverage for each county in the United States, our measure took into account CIALs existing at the state, county, or city level. For example, counties in states that had passed CIALs were counted as being fully covered. Counties in states without CIALs were examined to see if county or city level laws existed. If such laws existed, the population of the jurisdiction in question (county or city) was counted as covered. State preemption of local legislation is also taken into account when calculating coverage. The probability of coverage ranges from 0 (no one in the county is covered by a law) to 1 (the entire population of the county is covered by a CIAL).
The data on workplace CIAL coverage at the county level were merged into the TUS-CPS 2001–2010 and BRFSS 2000–2006 based on respondent’s county of residence and survey year to identify the degree of law coverage to a county where the respondent lived. The TUS-CPS provides the information on whether the respondent worker worked in public or private sector, the BRFSS does not. When analyzing the TUS-CPS, we classified respondents by their status as a public (working for a federal, state, or local governmental entity) or private employee and assigned their CIAL coverage (using either the public or private workplace coverage) based on this designation. When analyzing the BRFSS, we used CIAL coverage in private workplaces for all BRFSS respondents’ law coverage measures because the BRFSS does not provide information on the occupation to respondents.
Although BRFSS has its own weakness, such as it covers shorter time series and it does not include information on private or public sector for employee respondents, this study still employed the BRFSS data in addition to the CPS-TUS data aiming to compare the results. BRFSS has several strengths over CPS-TUS – collection is more evenly spaced across calendar months and years, and more geographic areas are identified in this dataset (there are 921 counties identified in BRFSS, and 321 counties identified in CPS-TUS).
The final analysis is based on 70,274 and 257,691 observations from TUS-CPS and BRFSS, respectively. Three outcomes were estimated: (1) current smoking status, (2) the presence of a workplace smoking ban, and (3) SHS exposure among nonsmoker indoor workers.
In accordance with CDC standards, we used two questions to construct current smoking status. The first question respondents were asked was “Have you every smoked 100 cigarettes in your lifetime?” Individuals who reported never smoking 100 cigarettes in their lifetime are classified as a non-smoker and coded as 0 for the current smoking status variable. If respondents identified themselves as having smoked 100 cigarettes, they were asked “Do you now smoke cigarettes every day, some days, or not at all?” Those who answered either “every day” or “some days” were coded as 1, current smokers, otherwise respondents were classified as 0, non-smokers.
The presence of a workplace smoking ban was measured by two questions in the TUS-CPS and BRFSS, “Which of these best describes your place of work’s smoking policy for indoor public or common areas such as lobbies, rest rooms, and lunch rooms?” and “Which of these best describes your place of work’s smoking policy for work areas?” For both questions possible answers include “Not allowed in any areas,” “Allowed in some areas,” “Allowed in all areas,” or “No official policy.” The self-reported workplace smoking ban measure was constructed by setting this variable equal to 1 for workers who reported smoking was “Not allowed in any areas” for both questions (i.e. the measure was set to 1 if smoking was “not allowed in any areas” for common areas and work areas), and equal to 0 otherwise. A self-reported absence of workplace smoking ban measure was constructed as an alternative measure. No workplace restriction was set to 1 for workers who reported “Allowed in all areas” or “No official policy” for both questions (the measure was set to 1 if smoking was “allowed in all areas” or “no official policy” for common areas and work areas), and equal to 0 otherwise.
Non-smoker SHS exposure was measured via the TUS-CPS question “During the past two weeks has anyone smoked in the area in which you work?” SHS exposure was coded as 1 for workers who reported “Yes” for that question, and 0 otherwise.
3. Empirical model
This study investigated the effect of workplace CIAL coverage in the county level on current smoking status, self-reported workplace smoking ban, and non-smoker SHS exposure. First, this study focused on indoor workers whose smoking behaviors are most likely influenced by workplace smoking restrictions to investigate whether or not workplace smoking restrictions reduce indoor workers’ likelihood of being a smoker. Second, it examined worksite compliance with workplace CIALs to understand whether laws engender compliance through actual workplace smokefree policies. Finally, this study used information on self-reported SHS exposure in the workplace to investigate the effect of workplace smoking restriction on worksite SHS exposure among indoor nonsmoking workers.
The following linear probability model was used to estimate the impact of workplace smoking ban on the three outcomes:
| (1) |
where Yict are various outcomes of interest for individual i in county c at time t (smoking status (0/1), self-reported workplace smoking ban (0/1), and SHS exposure (0/1)). CIALct is the probability of a respondent in a given county, year, and month being subject to a comprehensive workplace CIAL. Xict is a vector of individual characteristics including sex, race, age, education, family income, and marital status. Cc is a set of county fixed effects to capture all time-invariant county characteristics that may affect smoking behaviors. Trendc is the county-specific time trends in study period to capture the monotonic changing county characteristics which may affect smoking behaviors. State fixed effects were used in some specifications as the comparison to the previous studies. Tt is a set of year and month fixed effects that controls for any time-specific factors related to smoking behaviors. Standard errors were computed allowing for clustering at the county level.
A concern of the identification of the effect of workplace CIAL coverage on smoking related outcomes is that there might be common determinants omitted and associated with both the implementation of CIALs and smoking prevalence. For example, places with strong attitudes against cigarette smoking or anti-smoking programs and interventions may be more likely to implement workplace CIALs, and these attitudes and interventions may also influence smoking prevalence. Because it is possible that workplace CIALs are a reflection of general anti-smoking attitudes, which could lead the estimated impacts being biased upward, this study adopts the state fixed effects or county fixed effects to capture the time-invariant smoking attitudes within state or county. The county fixed effect model accounts for the unobserved and potentially confounded heterogeneity between counties. This basic identification strategy, like the difference-in-difference model, relies on the within county variation in smoking outcome and CIALs over time and uses respondents who did not face changed CIALs as a control group for unrelated time-series variation. This model includes county-specific time trends to capture the county-specific smoking attitudes which changes monotonically by year.
The data provided substantial variations in county smokefree law coverage that allowed us to detect the impact of workplace CIALs on smoking status. During the study period in TUS-CPS, 254 counties out of 329 counties had changes in public workplace CIALs, and 205 out of 329 counties had changes in private workplace CIALs with 103 counties changed 2001–2006 and 120 counties changed 2007–2010. In BRFSS, there were 135 out of 921 counties had changes in private workplace CIALs 2000 to 2006. In addition, we ran a regression of CIALs on county fixed effects, year/month fixed effects, and county-specific time trends; the R2 is 0.71 and 0.67 for TUS-CPS and BRFSS, respectively, indicating the substantial within-county variations in CIALs.
4. Results
4.1 Descriptive statistics
Table 1 presents the within-state-variation of the workplace CIAL coverage taking into account the CIALs in state, county, and city levels using TUS-CPS data in January 2000 and December 2009, respectively. In January 2000 TUS-CPS, among 50 states and the District of Columbia, 42 states had within-state variation in public workplace CIAL coverage. In December 2009, 13 states had within-state variation. The decreasing number of states having within state variation from 2000 to 2009 reflected the fact that after January 2000 many states passed state-level public workplace CIALs. For private workplace CIAL coverage, in January 2000, 11 states had within-state variation while many states had no private workplace CIAL coverage at either the local or state level. By December 2009, private workplace CIAL passage had increased at both the local and state level, yielding 19 states with within-state variation. The increasing number of states having within-state variation from 2000 to 2009 is due to the fact that many states had moved from no workplace CIAL coverage at all within a state, to increased coverage at the local level.
Table 1.
Within state variation of smoking ban
| January of 2000 | December of 2009 | |||||||
|---|---|---|---|---|---|---|---|---|
| State | Private workplace smoking ban | Public workplace smoking ban | Private workplace smoking ban | Public workplace smoking ban | ||||
| mean | cv | Mean | cv | mean | cv | mean | cv | |
| AL | 0 | . | 0.240 | 0.931 | 0.057 | 2.135 | 0.322 | 0.732 |
| AK | 0 | . | 0 | . | 0.477 | 0.975 | 0.546 | 0.822 |
| AZ | 0.033 | 0.750 | 0.194 | 1.234 | 1 | 0 | 1 | 0 |
| AR | 0 | . | 0.024 | 3.671 | 0.001 | 9.488 | 1 | 0 |
| CA | 0.201 | 1.460 | 0.398 | 0.648 | 0.256 | 1.146 | 1 | 0 |
| CO | 0.021 | 3.900 | 0.271 | 1.347 | 0.113 | 1.765 | 0.350 | 1.040 |
| CT | 0 | . | 0.015 | 1.701 | 0 | . | 1 | 0 |
| DE | 0 | . | 0 | . | 1 | 0 | 1 | 0 |
| DC | 0 | . | 0 | . | 1 | 0 | 1 | 0 |
| FL | 0 | . | 0.032 | 4.155 | 1 | 0 | 1 | 0 |
| GA | 0 | . | 0.011 | 4.551 | 0.102 | 2.714 | 0.184 | 1.793 |
| HI | 0.302 | 0.637 | 0.411 | 0.636 | 1 | 0 | 1 | 0 |
| ID | 0 | . | 0 | . | 0 | . | 1 | 0 |
| IL | 0 | . | 0.011 | 3.407 | 1 | 0 | 1 | 0 |
| IN | 0 | . | 0.059 | 2.644 | 0.173 | 1.439 | 0.284 | 1.058 |
| IA | 0 | . | 0.050 | 3.246 | 1 | 0 | 1 | 0 |
| KS | 0 | . | 1 | 0 | 0.245 | 1.540 | 1 | 0 |
| KY | 0 | . | 0 | . | 0.323 | 1.384 | 1 | 0 |
| LA | 0 | . | 0.048 | 3.137 | 1 | 0 | 1 | 0 |
| ME | 0 | . | 0.045 | 2.120 | 1 | 0 | 1 | 0 |
| MD | 0 | . | 0.264 | 1.438 | 1 | 0 | 1 | 0 |
| MA | 0.052 | 1.224 | 0.211 | 0.652 | 1 | 0 | 1 | 0 |
| MI | 0 | . | 0.028 | 4.550 | 0.254 | 1.321 | 0.326 | 1.105 |
| MN | 0 | . | 0.011 | 4.760 | 1 | 0 | 1 | 0 |
| MS | 0 | 11.746 | 0.139 | 1.555 | 0.159 | 1.553 | 1 | 0 |
| MO | 0 | . | 0.272 | 1.531 | 0.079 | 2.217 | 0.378 | 1.097 |
| MT | 0 | . | 0.103 | 2.421 | 1 | 0 | 1 | 0 |
| NE | 0 | . | 0.010 | 2.360 | 1 | 0 | 1 | 0 |
| NV | 0 | . | 0 | . | 1 | 0 | 1 | 0 |
| NH | 0 | . | 0.011 | 1.854 | 0 | . | 0.011 | 1.854 |
| NJ | 0.002 | 3.180 | 0.206 | 1.121 | 1 | 0 | 1 | 0 |
| NM | 0 | . | 0.106 | 1.524 | 0.362 | 0.998 | 1 | 0 |
| NY | 0.015 | 8.105 | 0.073 | 2.924 | 1 | 0 | 1 | 0 |
| NC | 0 | 6.223 | 0.150 | 1.594 | 0 | 6.223 | 1 | 0 |
| ND | 0 | . | 0.071 | 2.741 | 1 | 0 | 1 | 0 |
| OH | 0 | . | 0.088 | 1.918 | 1 | 0 | 1 | 0 |
| OK | 0 | . | 0.004 | 2.043 | 0 | . | 0.008 | 2.043 |
| OR | 0.019 | 6.651 | 0.179 | 1.893 | 1 | 0 | 1 | 0 |
| PA | 0 | . | 0.023 | 5.046 | 1 | 0 | 1 | 0 |
| RI | 0 | . | 0.028 | 2.293 | 1 | 0 | 1 | 0 |
| SC | 0 | . | 0.094 | 2.367 | 0.257 | 1.402 | 0.323 | 1.188 |
| SD | 0 | . | 0.263 | 1.340 | 1 | 0 | 1 | 0 |
| TN | 0 | . | 0.025 | 4.109 | 0 | . | 1 | 0 |
| TX | 0 | . | 0.101 | 1.303 | 0.190 | 1.444 | 0.328 | 0.896 |
| UT | 0 | . | 1 | 0 | 1 | 0 | 1 | 0 |
| VT | 0 | . | 0 | . | 1 | 0 | 1 | 0 |
| VA | 0 | . | 0.043 | 4.624 | 0 | . | 1 | 0 |
| WA | 0 | . | 0.066 | 1.727 | 1 | 0 | 1 | 0 |
| WV | 0.028 | 5.853 | 0.055 | 3.844 | 0.819 | 0.470 | 0.849 | 0.423 |
| WI | 0 | . | 0.281 | 1.017 | 0.058 | 2.048 | 1 | 0 |
| WY | 0 | . | 0.011 | 6.302 | 0.039 | 4.960 | 0.091 | 2.578 |
cv: coefficient of variation (the ratio of the standard deviation to the mean)
mean: the proportion of state population covered by a comprehensive workplace CIAL in any levels of city, county, or state.
Source: Authors’ computation using data from American Nonsmokers’ Rights Foundation and the Census-Estimated Population (CEP) Cities and Towns.
Table 2 reports descriptive statistics of smoking outcomes and demographic variables for all indoor workers in TUS-CPS and BRFSS with county identifiers. The statistics for all variables between TUS-CPS and BRFSS are consistent in general. Among indoor workers in the TUS-CPS sample, 14.3% are current smokers, compared to 21.9% for the BRFSS sample. The percentage of respondents self-reported that their workplaces are restricted from smoking is 78.9% and 72.9% in TUS-CPS and BRFSS, respectively.
Table 2.
Summary Statistics
| Variable | TUS-CPS | BRFSS |
|---|---|---|
| Current smoking status | 0.143 | 0.219 |
| Self-reported workplace smoking restriction | ||
| not allowed | 0.789 | 0.729 |
| no restriction | 0.079 | 0.046 |
| Secondhand smoke exposure | 0.039 | N/A |
| Workplace smoking ban coverage | 0.329 | 0.046 |
| Gender | ||
| male | 0.444 | 0.482 |
| Female | 0.556 | 0.518 |
| Race | ||
| non-Hispanic white | 0.668 | 0.739 |
| non-Hispanic black | 0.118 | 0.108 |
| Hispanic | 0.124 | 0.102 |
| other races | 0.090 | 0.051 |
| Age at the survey year | ||
| 18–29 | 0.228 | 0.229 |
| 30–39 | 0.251 | 0.251 |
| 40–49 | 0.261 | 0.262 |
| 50–59 | 0.191 | 0.188 |
| 60 or older | 0.068 | 0.070 |
| Education | ||
| less than high school | 0.043 | 0.063 |
| high school | 0.195 | 0.249 |
| some college | 0.299 | 0.271 |
| College | 0.464 | 0.417 |
| Family income in nominal dollars | ||
| less than 20k | 0.066 | 0.086 |
| 20–35k | 0.121 | 0.180 |
| 35–50k | 0.131 | 0.164 |
| 50–75k | 0.207 | 0.192 |
| 75k+ | 0.399 | 0.293 |
| income missing | 0.077 | 0.085 |
| Marital status | ||
| Married | 0.547 | 0.616 |
| widowed, divorced or separated | 0.167 | 0.148 |
| never married | 0.287 | 0.236 |
| Year | ||
| 2000 | 0.157 | |
| 2001 | 0.199 | 0.157 |
| 2002 | 0.098 | 0.178 |
| 2003 | 0.242 | 0.115 |
| 2004 | 0.159 | |
| 2005 | 0.119 | |
| 2006 | 0.184 | 0.144 |
| 2007 | 0.091 | |
| 2010 | 0.186 | |
| Sample size | 70,274 | 257,691 |
There are differences in coverage by CIALs between TUS-CPS and BRFSS. The average probability of being covered by workplace CIALs is 32.9% for TUS-CPS and only 4.6% for BRFSS. The possible reasons for this difference that the datasets cover different time periods (BRFSS 2000–2006 and TUS-CPS 2001–2010), and the law coverage may not take place until the late 2000s. Second, we used private workplace smoking ban for all respondents in the BRFSS sample because BRFSS does not provide occupation identifiers, while the TUS-CPS provides detailed occupation categories that allowed us to distinguish the public and private workplace workers. The proportion of private workplaces covered by CIALs is consistently lower than the proportion of covered public workplaces every year. Third, workplace CIAL prevalence may be higher in the TUS-CPS than the BRFSS because public versions of TUS-CPS only include county codes for counties with significantly large populations. And some large-population states (California, Massachusetts, and New York) are excluded from the BRFSS sample because these state did not ask employed respondents whether they worked indoors or outdoors.3
4.2 Effects on smoking prevalence
Table 3 reports the effects of workplace CIAL coverage on smoking participation (measured by current smoking status) for indoor workers. In Columns (1) and (6), the model specification does not control for fixed effects in either state or county level. In Columns (2) and (7), state fixed effects were controlled. In Columns (3) and (8), county fixed effects were controlled instead. In Columns (4) and (9), in addition to county fixed effects, the county characteristics, such as average age, percentage of minority population, percentage of college graduates, average family income, and unemployment rate were controlled.4 We include the county level characteristics because the county characteristics might be correlated with both CIALs and smoking outcomes.5 In Columns (5) and (10), model specification controls for county fixed effects, the county characteristics, and county time trends.
Table 3.
Effects of workplace CIAL coverage on smoking participation
| TUS-CPS | BRFSS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) |
| Dependent variable: being a current smoker (1), otherwise (0) | ||||||||||
| CIAL coverage | −0.013** (0.005) | −0.016*** (0.005) | −0.017*** (0.006) | −0.017*** (0.006) | −0.018*** (0.007) | −0.018*** (0.010) | −0.018** (0.007) | −0.021*** (0.007) | −0.021*** (0.007) | −0.024*** (0.009) |
| State fixed effects | No | Yes | No | No | No | No | Yes | No | No | No |
| County fixed effects | No | No | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| County characteristics | Yes | No | No | Yes | Yes | Yes | No | No | Yes | Yes |
| County time trends | No | No | No | No | Yes | No | No | No | No | Yes |
| 70,274 | 257,691 | |||||||||
Models (1)–(5) use data from TUS-CPS, and Models (6)–(10) use data from BRFSS. These models include same set of variables (state cigarette tax, sex, race, age, education, family income, marital status, year and month fixed effects), and differ by including county characteristics only, state fixed effects only, county fixed effects only, or county fixed effects and county time trends. The county characteristics include the average age, % minority population, % college graduate, average family income, and unemployment rate in a county. Sampling weights are applied and robust standard errors clustered at county level are shown in parentheses.
Significant at 1% level based on a two-tailed test
Significant at 5% level based on a two-tailed test
Significant at 10% level based on a two-tailed test
Workplace CIAL coverage significantly reduced smoking prevalence among indoor workers across different model specifications. In the model which control for county fixed effects, county characteristics, and county time trends (column 5 and 10), going from 0% to 100% workplace CIAL county coverage reduced smoking participation by 1.8 percentage points for TUS-CPS sample and 2.4 percentage points for BRFSS sample. Given that the sample mean of smoking participation is 14.3% for TUS-CPS data and 21.9% for BRFSS data, the relative change is about 13% and 11% for TUS-CPS and BRFSS, respectively.6 These results are comparable to Carpenter (2009) which found that the bylaw adoption decreased the smoking prevalence by 12.7% in Ontario, Canada, although our results are smaller than the effect magnitudes summarized in Fichtenberg and Glantz (2002) and Hopkins et al. (2010) which found that smokefree policies lead to a 17% and 14% reductions in smoking prevalence.7 The smaller effects observed in this study may reflect that there were more voluntary policies already in place when the CIALs went into effect than in the earlier studies.
In our models the estimated coefficient on cigarette taxes is −0.012 indicating that when tax rises by $1, smoking prevalence falls by 1.2 percentage points; this tax coefficient is comparable to that observed by Callison and Kaestner (2014) who also used the TUS-CPS data and concluded that the tax coefficient is −0.01 for the age group 18–74.
Our results indicate that CIALs have a stronger effect on smoking behavior than taxes. To obtain the 1.7 percentage points decrease in smoking prevalence resulting from workplace CIAL one would require cigarette taxes per pack to increase from the average level $0.89 per pack in 2000–2010 to $2.31 per pack,8 indicating that CIALs have a major effect as a tobacco control intervention.
4.3 Compliance with legislation
It is intuitive to think that the implementation of workplace CIALs should increase indoor workers’ self-reported smoking restriction in their worksites; however, this is not always the case. For example, some worksites may voluntarily adopt smoking restrictions even without any state or local CIALs, or some employers may actively defy workplace CIALs. If the passage of workplace CIALs do not increase the actual smoking restrictions in worksites because they are not needed (voluntary rules have been previously adopted) or they are not complied with (active defiance of CIALs), then we should not expect workplace CIALs to have any influence on the smoking behaviors of indoor workers and there should not be a significant relationship between CIALs and the reported existence of a worksite smoking restriction.
The effects of workplace CIAL coverage on self-reported smoking restrictions at worksites are presented in Table 4. We estimated two outcome variables for measuring law compliance: (1) whether smoking is not allowed in work areas and common areas (yes: 1 and no: 0), (2) whether no smoking restriction in either work areas or common areas (yes: 1 and no: 0). In Columns (1) and (6), the model specification does not control for county or state fixed effects. In Columns (2) and (7), the model specification controls for state fixed effects and in Columns (3), (4), (8), and (9) the county fixed effects. In Columns (4) and (9), the model specification also controls for county characteristics. In Columns (5) and (10), the model specification controls for county fixed effects and county time trends.
Table 4.
Effects of workplace CIAL coverage on self-reported smoking restriction at workplace
| TUS-CPS | BRFSS | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Model | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) |
| Dependent variable: smoking is not allowed in work areas or common areas (1); otherwise (0) | ||||||||||
| CIAL coverage | 0.051*** (0.009) | 0.066*** (0.008) | 0.063*** (0.009) | 0.061*** (0.009) | 0.067*** (0.009) | 0.098*** (0.010) | 0.079*** (0.011) | 0.070*** (0.010) | 0.070*** (0.010) | 0.071*** (0.011) |
| State fixed effects | No | Yes | No | No | No | No | Yes | No | No | No |
| County fixed effects | No | No | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| County characteristics | Yes | No | No | Yes | Yes | Yes | No | No | Yes | Yes |
| County time trends | No | No | No | No | Yes | No | No | No | No | Yes |
| Dependent variable: there is no smoking restriction in worksite (1); otherwise (0) | ||||||||||
| CIAL coverage | −0.019*** (0.005) | −0.026*** (0.005) | −0.025*** (0.006) | −0.026*** (0.006) | −0.033*** (0.006) | −0.013*** (0.004) | −0.012*** (0.004) | −0.014*** (0.004) | −0.014*** (0.004) | −0.021*** (0.007) |
| State fixed effects | No | Yes | No | No | No | No | Yes | No | No | No |
| County fixed effects | No | No | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| County characteristics | Yes | No | No | Yes | Yes | Yes | No | No | Yes | Yes |
| County time trends | No | No | No | No | Yes | No | No | No | No | Yes |
| 70,274 | 257,691 | |||||||||
Models (1)–(5) use data from TUS-CPS, and Models (6)–(10) use data from BRFSS. These models include same set of variables (state cigarette tax, sex, race, age, education, family income, marital status, year and month fixed effects), and differ by including county characteristics only, state fixed effects only, county fixed effects only, or county fixed effects and county time trends. The county characteristics include the average age, % minority population, % college graduate, average family income, and unemployment rate in a county. Sampling weights are applied and robust standard errors clustered at county level are shown in parentheses.
Significant at 1% level based on a two-tailed test
Significant at 5% level based on a two-tailed test
Significant at 10% level based on a two-tailed test
The results from the upper panel of Table 4 indicate that workplace CIAL coverage significantly increased the likelihood of reporting smoking was not allowed at work; the lower panel indicates that workplace CIAL significantly reduced the likelihood of reporting no restrictions on smoking at work. All estimates of the effect of workplace CIAL coverage are statistically significant, implying worksite compliance with CIALs.
The association between CIAL coverage and respondent’s actual workplace smoking restrictions provides strong evidence of law compliance, and indicates that the measure of workplace CIAL coverage this study used could be used as a proxy for respondents’ actual workplace smoking restrictions. Results suggested that when the CIAL coverage of a county increased from 0% to 100%, self-reported smoking restriction rose by 6.7 percentage points from the sample mean for TUS-CPS data, and by 7.1 percentage points for BRFSS data. Given that the sample mean of self-reported workplace smoking restrictions is 79% for TUS-CPS data and 73% for BRFSS data, the effect is between 8% (.067/.79) and 10% (.071/.73).
4.4 Robustness check
Previous studies (Bitler, Carpenter, & Zavodny (2010); Liu (2010); Adda & Cornaglia (2010)) found that the state CIALs or the CIALs aggregated up at the state level do not statistically significantly influence smoking status. This study used the state CIALs from ANRF and ImpacTeen9, and estimated the impact of state CIALs on smoking status as the robustness check. The specifications including state CIALs yields results similar to previous studies. Our results failed to find a statistically significant effect of state CIALs on smoking status (columns (1), (2), (5), and (6)), likely due to misclassification of workers as not covered by a state CIAL when they are, in fact, covered by a county law.
Because of the limitation of the linear probability model that predict probabilities of smoking can be outside of [0,1], Columns (3) and (7) reported results from probit models of smoking participation that includes the full set of variables as in columns (5) and (10) of Table 3. To compare the results across model specifications, Table 5 reported the implied marginal effect of smoking ban on the probability of smoking, evaluated at the sample averages of the relevant variables.
Table 5.
Effects of workplace CIAL coverage on smoking participation, robustness check
| TUS-CPS | BRFSS | ||||||
|---|---|---|---|---|---|---|---|
| Dependent variable: being a current smoker (1); otherwise (0) | |||||||
| Model | (1) | (2) | (3) | (4) | (5) | (6) | (7) |
| State-level CIAL from ANRF | State-level CIAL from ImpacTeen | Probit | 2001–2006 | State-level CIAL from ANRF | State-level CIAL from ImpacTeen | Probit | |
| CIAL coverage | −0.002 (0.002) | −0.008 (0.007) | −0.017*** (0.006) | −0.025*** (0.009) | −0.004 (0.003) | 0.003 (0.011) | −0.023*** (0.008) |
| Sample size | 70,274 | 70,274 | 70,256 | 51,797 | 257,691 | 257,691 | 257,652 |
Models (1)–(4) use data from TUS-CPS, and Models (5)–(7) use data from BRFSS. These models include a set of variables (state cigarette tax, sex, race, age, education, family income, marital status, year and month fixed effects, county fixed effects, county characteristics, and county time trends). In addition, models (1) and (5) use state-level CIAL coverage from ANRF; models (2) and (6) use state-level CIAL coverage from ImpacTeen; models (3) and (7) are estimated using a probit model instead of linear probability for models; model (4) use data from 2001 to 2006. Sampling weights are applied and robust standard errors clustered at county level are shown in parentheses.
Significant at 1% level based on a two-tailed test
Significant at 5% level based on a two-tailed test
Significant at 10% level based on a two-tailed test
To ensure results using TUS-CPS sample are comparable to BRFSS, we restricted TUS-CPS sample to 2001–2006 period and included the same set of variables as in column (4) of Table 4. Results are consistent.
4.5 Placebo checks
Indoor workers are the subgroup of people who are most directly influenced by smoke-free workplace laws and policies. We conducted a placebo check to estimate models of smoking participation for other groups of people which are not protected by workplace smoking ban such as those who work outdoors, unemployed, and not in labor force (Table 6). For the TUS-CPS, those who were unemployed or not in labor force are not influenced by the workplace CIALs. For the BRFSS, workplace CIALs do not impact smoking prevalence for those who worked outdoors, were unemployed, or not in labor force. In TUS-CPS, however, people who worked outdoors had reduced smoking prevalence if they lived where there were workplace CIALs, perhaps reflecting indirect social and normative changes.
Table 6.
Placebo checks: effects of workplace CIAL coverage on smoking participation, other groups
| TUS-CPS | BRFSS | |||||
|---|---|---|---|---|---|---|
| Dependent variable: being a current smoker (1); otherwise (0) | ||||||
| Model | (1) | (2) | (3) | (4) | (5) | (6) |
| Working outdoors | Unemployed | Not in labor force | Working outdoors | Unemployed | Not in labor force | |
| CIAL coverage | −0.013* (0.007) | −0.016 (0.034) | −0.010 (0.007) | −0.006 (0.036) | −0.002 (0.024) | 0.008 (0.006) |
| Sample size | 73,718 | 10,025 | 80,539 | 62,909 | 62,902 | 554,400 |
Models (1)–(3) use data from TUS-CPS, and Models (4)–(6) use data from BRFSS. Models (1) and (4) are estimated among people working outdoors; models (2) and (5) are estimated among people unemployed; models (3) and (6) are estimated among people not in labor force. These models include same set of variables (state cigarette tax, sex, race, age, education, family income, marital status, year and month fixed effects, county fixed effects, county characteristics, and county time trends). Sampling weights are applied and robust standard errors clustered at county level are shown in parentheses.
Significant at 1% level based on a two-tailed test
Significant at 5% level based on a two-tailed test
Significant at 10% level based on a two-tailed test
4.6 Effects of leads and lags workplace CIAL coverage on smoking prevalence
The identification of Equation (1) relies on the within county variation in smoking outcome and CIAL coverage over time. The estimated correlation of workplace CIAL coverage and smoking prevalence could not make any inference on causal relationship from workplace CIAL coverage to smoking prevalence. Indeed, it is possible that the correlation is driven by a reverse causality from smoking prevalence to workplace CIAL coverage. In this section, we attempted to confirm that our estimated association between workplace CIAL coverage and smoking status was not due to the reverse causality from smoking prevalence to implementation of smokefree legislation (For example, an area with a high prevalence of non-smoker voters may promote passage of smokefree legislations). To test whether the reverse causality exists, we estimated whether the leads (t+1, t+2) and lags (t-1, t-2) workplace CIALs influenced smoking status at the current time (t). If the reverse causality exists, we would expect to see a negative correlation between the current smoking status (t) and workplace CIALs in later periods (t+1, t+2).
The results of the influences of the leads (t+1, t+2) and lags (t-1, t-2) workplace CIALs on smoking status at the current time (t) are presented in Table 7. The results indicated that the lags CIALs were associated with significantly decreased current smoking participation, and the leads CIALs were not significantly associated with current smoking participation, except for CIAL (t+1). The significant lag effect of CIALs indicates that the acceptance of the smokefree ordinance can be delayed possibly due to the initial resistance by its opponents and legal wrangling over its enforcement. Besides, it might take time for smoker workers to change their smoking behaviors due to the smoking restriction in their workplace. Indeed, the insignificant association between leads CIALs and current smoking participation, as well as the positive association between CIALs (t+1) and smoking participation (t) indicate the reverse causality is not a concern in this study. (Table 7).
Table 7.
Effects of lagged and leaded workplace CIAL coverage on current smoking participation
| TUS-CPS | BRFSS | |||||||
|---|---|---|---|---|---|---|---|---|
| Dependent variable: being a current smoker (1); otherwise (0) | ||||||||
| Model | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) |
| CIAL(t-1) | CIAL(t-2) | CIAL(t+1) | CIAL(t+2) | CIAL(t-1) | CIAL(t-2) | CIAL(t+1) | CIAL(t+2) | |
| Smoke (t) | −0.019** (0.008) | −0.022*** (0.008) | −0.012 (0.008) | −0.006 (0.009) | −0.034*(0.018) | −0.010 (0.030) | 0.018* (0.009) | 0.004 (0.008) |
| Sample size | 68,991 | 52,813 | 57,548 | 57,548 | 236,476 | 198,243 | 257,431 | 257,431 |
Models (1)–(4) use data from TUS-CPS, and Models (5)–(8) use data from BRFSS. The dependent variable for models (1)–(8) is current smoking status at t. Models (1)–(8) include same set of variables (state cigarette tax, sex, race, age, education, family income, marital status, year and month fixed effects, county fixed effects, county characteristics, and county time trends) except that the CIAL variable was measured at different time points: (t-1), (t-2), (t+1), and (t+2) for models (1) and (5), models (2) and (6), models (3) and (7), and models (4) and (8), respectively. Sampling weights are applied and robust standard errors clustered at county level are shown in parentheses.
Significant at 1% level based on a two-tailed test
Significant at 5% level based on a two-tailed test
Significant at 10% level based on a two-tailed test
4.7 Effects on exposure to SHS
Table 8 presents the results of the effects of workplace CIAL coverage on self-reported SHS exposure in worksite for indoor nonsmoker workers. Increasing workplace CIAL county coverage from 0 to 100% reduced worksite SHS exposure by 1.1 percentage points. Given that the sample mean of exposure to SHS is 3.9%, the effect is 28%.
Table 8.
Effects of workplace CIAL coverage on exposure to secondhand smoke
| Dependent variable: being exposed to secondhand smoke (1); otherwise (0) | |||||
|---|---|---|---|---|---|
| Model | (1) | (2) | (3) | (4) | (5) |
| Workplace CIAL coverage | −0.010* (0.004) | −0.012** (0.004) | −0.013** (0.004) | −0.011** (0.004) | −0.011** (0.005) |
| State fixed effects | No | Yes | No | No | No |
| County fixed effects | No | No | Yes | Yes | Yes |
| County characteristics | Yes | No | No | Yes | Yes |
| County time trend | No | No | No | No | Yes |
| Sample size | 49,620 | ||||
Data comes from TUS-CPS. Models (1)–(5) control for state cigarette tax, sex, race, age, education, family income, marital status, county fixed effects, year and month fixed effects. In addition, model (1) controls for county characteristics (the average age, % minority population, % college graduate, average family income, and unemployment rate in a county); model (2) controls for state fixed effects; model (3) controls for county fixed effects; model (4) controls for county fixed effects and county characteristics; and model (5) controls for county fixed effects, county characteristics, and county time trends. Sampling weights are applied and robust standard errors clustered at county level are shown in parentheses.
Mean of exposure to second hand smoke is 3.89%.
Significant at 1% level based on a two-tailed test
Significant at 5% level based on a two-tailed test
Significant at 10% level based on a two-tailed test
5. Limitations
Our main model specifications include county fixed effects, county characteristics, and county specific time trends to control for the unobserved factors associated with CIALs and smoking behaviors. This model specification allows the unobserved factors vary by counties, and for each county the confounders could monotonically change by year. However, if the unobserved trends are not changing monotonically, this would pose a threat to the internal validity. In addition, because only counties with large populations are identified and linked with workplace CIALs, the results of this study make inference for counties with large populations. There is little analysis investigating on the probability of a county adopting a law based on county size, and the CDC has done an analysis of the 50 largest cities in the US showing that the majority of these cities had adopted a law by 2012 (CDC 2012). However, there are significant variations between states in the passage of smokefree laws as an analysis of Massachusetts local-law diffusion found that areas with large minority populations were less likely to be covered with smokefree laws (Deverell et al. 2006), while an analysis of smokefree law coverage in Texas found that cities with large populations of minorities were more likely to have coverage (Gingiss et al. 2009). Another limitation this study has is the potential existence of cross-county jobs. If the respondent who worked in different county from where they lived, we may misclassify their workplace CIALs. However, McKenzie (2013) uses the American Community Survey 2006–2010 and Census 2000 and indicates that a majority of U.S. workers worked in the same county of their residence. In 2006–2010, during a typical week 72.6% of U.S. workers worked within of their residence county, which is similar to the, 2000 finding of 73.3%. The influence of cross-county jobs on our results should be limited. While we are unable to directly assess if smokers are more likely to work in counties without CIALs in response to CIALs in their county of residence. However, if this potential situation exists, our results would be biased toward zero. Our results would underestimate the association between CIALs and smoking status.
6. Conclusion
This study expanded on previous research by using the probability of residents in a county being covered by workplace CIALs taking into account the state, county, and city legislation as a measure of workplace smoking ban, and examined their impact on smoking related outcomes. Previous research used the state CIALs and did not examine the impact of county or city policies. It is possible that some local jurisdictions such as counties (cities) may have implemented local-level CIALs prior to state laws, which leads to the measurement errors on the CIALs and the effects of CIALs biased toward zero. In particular, this study expanded Carpenter (2009), Adda and Cornaglia (2010), and Bitler et al. (2010) and focused on the current employees who worked indoors, divided them into workers who worked in public sector and those who worked in private sector, and linked them to the sector specific CIAL coverage in a county level.
We found that workplace CIALs significantly decreased worker smoking participation (being a current smoker) by around 10%. These results are robust to different model specifications. Furthermore, CIALs were associated with significant increases in actual smoking policies in worksites, 8% and 10% in TUS-CPS and BRFSS, indicating compliance with the law. Finally, nonsmoking indoor workers who lived in a county with workplace CIAL coverage are about 28% less likely to report SHS exposure at work independent of model specifications. This study provided evidence that workplace CIALs reduced nonsmokers’ SHS exposure as well as reduced workers’ smoking prevalence.
Acknowledgments
Taiwan National Science Council grant NSC 101-2410-H-002-207; National Cancer Institute Grant CA-061021.
Footnotes
Sources from http://www.no-smoke.org/pdf/EffectivePopulationList.pdf; http://www.no-smoke.org/pdf/USOrdMap.pdf
Table 4. Employed persons working (1) and time spent working on days worked by full- and part-time status and sex, jobholding status, educational attainment, and day of week, 2012 annual averages. (2012, March 2). U.S. Bureau of Labor Statistics. Retrieved June 11, 2014, from http://www.bls.gov/news.release/atus.t04.htm
We conducted some further analysis and found that the three factors (different time periods, different geographic coverage, use the private workplace laws) all contribute to the difference. We used the ANRF database which includes all the county-level CIAL coverage in the US to analyze the difference. First, we compared the CIAL coverage of private workplace and the CIAL coverage of public workplace, and restrict both datasets covering the same period (2000–2010) and the same geographic areas (same counties). We found that the CIAL coverage in private workplace is lower than the coverage in public workplace (16.1% for CIAL coverage in private workplace and 34.6% for CIAL coverage in public workplace). Secondly, we compared the CIAL coverage 2001–2010 (CPS-TUS period) and 2000–2006 (BRFSS period), and found that the CIAL coverage in the private workplace is 6.2% from 2000 to 2006 lower than 17.6% from 2001 to 2010. Third, since BRFSS did not include respondents from the three states, California, Massachusetts, and New York, so we excluded those states from the dataset, and we found that after the California, Massachusetts, and New York are excluded, the CIAL coverage in the private workplace is 4.7% from 2000 to 2006 similar to what we got from BRFSS.
The variance inflation factor (VIF) for multicollinearity for workplace CIALs is 3.65 for CPS data and 2.76 for BRFSS data suggesting that the multicollinearity is not a serious issue.
Regional studies of the implementation of smokefree laws in the US (for example:(Bartosch & Pope, 1999; Deverell, Randolph, Albers, Hamilton, & Siegel, 2006; Ferketich et al., 2010; Gingiss, Boerm, Huang, & Hermer, 2009; Skeer, George, Hamilton, Cheng, & Siegel, 2004) have found that communities with high education and income are more likely to adopt 100% smokefree laws than communities with lower education and income levels, and there are also overall disparities in smokefree coverage by race/ethnicity (see(Gonzalez et al., 2013)).
The interaction of survey year and CIAL coverage were included in the regression of smoking behaviors which serves as an alternative model specification. The non-significant interaction coefficients indicated that the influence of CIAL coverage does not significantly change over time. Therefore, this study lumped all survey years together and estimated the average effect of CIAL on smoking prevalence in these years.
Fichtenberg and Glantz (2002) reported that the implementation of a comprehensive smokefree workplace policy was associated with a decrease in consumption of 3.1 cigarettes per day per continuing smoker. The total effect is 1.3 fewer cigarettes were smoked per day per employee (including both smokers and nonsmokers), which corresponds to a 29% relative reduction. This implies the relative reduction in prevalence is 17%: ((3.1–1.3)/3.1)*29% = 17%.
To obtain a 1.7 percentage points decrease in smoking prevalence, tax needs to rise by $1.42 (1.7/1.2=1.42). Given that the average tax is $0.89 in our sample, a $1.42 tax rise leads the final tax $2.31.
Contributor Information
Kai-Wen Cheng, Research Specialist, Institute of Health Research and Policy, University of Illinois at Chicago, Chicago, United States of America.
Feng Liu, Associate Professor, School of Management and Economics, CUHK Business School, The Chinese University of Hong Kong, Shenzhen, China.
MariaElena Gonzalez, Assistant Professor, School of Social Sciences, Humanities, and Arts, University of California, Merced, United States of America.
Stanton Glantz, Professor of Medicine, University of California, San Francisco, United States of America.
References
- Adda Jérôme, Cornaglia Francesca. The Effect of Bans and Taxes on Passive Smoking. American Economic Journal: Applied Economics. 2010;2(1):1–32. doi: 10.1257/app.2.1.1. [DOI] [Google Scholar]
- Bartosch WJ, Pope GC. Local restaurant smoking policy enactment in Massachusetts. J Public Health Manag Pract. 1999;5(1):63–73. doi: 10.1097/00124784-199901000-00010. [DOI] [PubMed] [Google Scholar]
- Bauer UE, Johnson TM, Hopkins RS, Brooks RG. Changes in youth cigarette use and intentions following implementation of a tobacco control program: Findings from the Florida Youth Tobacco Survey, 1998–2000. JAMA: The Journal of the American Medical Association. 2000;284(6):723–728. doi: 10.1001/jama.284.6.723. [DOI] [PubMed] [Google Scholar]
- Biener LJ, Harris E, Hamilton W. Impact of the Massachusetts tobacco control programme: Population based trend analysis. BMJ. 2000;321(7257):351–35. doi: 10.1136/bmj.321.7257.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitler MP, Carpenter CS, Zavodny M. Effects of venue-specific state clean indoor air laws on smoking-related outcomes. Health Econ. 2010;19(12):1425–1440. doi: 10.1002/hec.1559. [DOI] [PubMed] [Google Scholar]
- Callison Kevin, Kaestner Robert. Do Higher Tobacco Taxes Reduce Adult Smoking? New Evidence of the Effect of Recent Cigarette Tax Increases on Adult Smoking. Economic Inquiry. 2014;52(1):155–172. [Google Scholar]
- Carpenter Christopher S. The Effects of Local Workplace Smoking Laws on Smoking Restrictions and Exposure to Smoke at Work. Journal of Human Resources. 2009;44(4):1023–1046. [Google Scholar]
- Centers for Disease Control and Prevention. Comprehensive smoke-free laws–50 largest U.S. cities, 2000 and 2012. MMWR Morb Mortal Wkly Rep. 2012;61(45):914–7. [PubMed] [Google Scholar]
- Chaloupka F. Clean indoor air laws, addiction and cigarette smoking. Applied Economics. 1992;24:193–205. [Google Scholar]
- Deverell M, Randolph C, Albers A, Hamilton W, Siegel M. Diffusion of local restaurant smoking regulations in Massachusetts: identifying disparities in health protection for population subgroups. J Public Health Manag Pract. 2006;12(3):262–269. doi: 10.1097/00124784-200605000-00007. [DOI] [PubMed] [Google Scholar]
- Ferketich AK, Liber A, Pennell M, Nealy D, Hammer J, Berman M. Clean indoor air ordinance coverage in the Appalachian region of the United States. Am J Public Health. 2010;100(7):1313–1318. doi: 10.2105/ajph.2009.179242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fichtenberg CM, Glantz SA. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ. 2002;325(7357):188. doi: 10.1136/bmj.325.7357.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gingiss PM, Boerm M, Huang P, Hermer L. Smoke-free ordinances in Texas worksites, restaurants, and bars, 2000–2007. Am J Prev Med. 2009;36(2):91–95. doi: 10.1016/j.amepre.2008.09.032. [DOI] [PubMed] [Google Scholar]
- Gonzalez M, Sanders-Jackson A, Song AV, Cheng KW, Glantz SA. Strong smoke-free law coverage in the United States by race/ethnicity: 2000–2009. Am J Public Health. 2013;103(5):e62–66. doi: 10.2105/ajph.2012.301045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammon David, Fong GT, Zanna MP, Thrasher JF, Borland R. Tobacco Denormalization and Industry Beliefs among Smokers from Four Countries. American Journal of Preventive Medicine. 2006;31(3):225–232. doi: 10.1016/j.amepre.2006.04.004. [DOI] [PubMed] [Google Scholar]
- Hopkins DP, Razi S, Leeks KD, Kalra GP, Chattopadhyay SK, Soler RE. Smokefree policies to reduce tobacco use: A systematic review. American Journal of Preventive Medicine. 2010;38(2S):S275–S289. doi: 10.1016/j.amepre.2009.10.029. [DOI] [PubMed] [Google Scholar]
- Kinne S, Kristal AR, White E, Hunt J. Work-site smoking policies: their population impact in Washington State. Am J Public Health. 1993;83(7):1031–1033. doi: 10.2105/ajph.83.7.1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Feng. Cutting through the smoke: separating the effect of price on smoking initiation, relapse and cessation. Applied Economics. 2010;42(23):2921–2939. doi: 10.1080/00036840801964880. [DOI] [Google Scholar]
- Longo DR, Brownson RC, Johnson JC, Hewett JE, Kruse RL, Novotny TE, Logan RA. Hospital smoking bans and employee smoking behavior: Results of a national survey. JAMA. 1996;275(16):1252–1257. [PubMed] [Google Scholar]
- McKenzie Brian. County-to-County Commuting Flows: 2006–10. Census Bureau Working Papers 2013 [Google Scholar]
- Powell L, Ross H, Tauras JA. The Importance of Peer Effects, Cigarette Prices and Tobacco Control Policies for Youth Smoking Behavior. Journal of Health Economics. 2005;24(5):950–968. doi: 10.1016/j.jhealeco.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Sanders-Jackson A, Gonzalez M, Zerbe B, Song AV, Glantz SA. The pattern of indoor smoking restriction law transitions, 1970–2009: laws are sticky. Am J Public Health. 2013;103(8):e44–51. doi: 10.2105/ajph.2013.301449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeer M, George S, Hamilton WL, Cheng DM, Siegel M. Town-level characteristics and smoking policy adoption in Massachusetts: are local restaurant smoking regulations fostering disparities in health protection? Am J Public Health. 2004;94(2):286–292. doi: 10.2105/ajph.94.2.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorsensen G, Rigotti N, Rosen A, Pinney J, Prible R. Effects of a worksite nonsmoking policy: evidence for increased cessation. Am J Public Health. 1991;81(2):202–204. doi: 10.2105/ajph.81.2.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stillman FA, Becker DM, Swank RT, Hantula D, Moses H, Glantz S, Waranch HR. Ending smoking at the Johns Hopkins Medical Institutions. An evaluation of smoking prevalence and indoor air pollution. JAMA. 1990;264(12):1565–1569. [PubMed] [Google Scholar]
- Tauras JA. Smoke Free Air Laws, Cigarette Prices, and Adult Cigarette Demand (no co-authors) Economic Inquiry. 2006;44(2):333–342. [Google Scholar]
- US Department of Health and Human Services. Healthy People 2010: Understanding and Improving Health. Washington, DC: US Department of Health and Human Services; 2000. [Google Scholar]
- US Department of Health and Human Services. Health Consequences of Involuntary Exposure to Tobacco Smoke. Atlanta, GA: US Department of Health and Human Services; 2006. [Google Scholar]
- US Department of Health and Human Services. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta GA: 2010. [PubMed] [Google Scholar]
- Wasserman J, Manning WG, Newhouse JP, Winkler JD. The effects of excise taxes and regulations on cigarette smoking. Journal of Health Economics. 1991;10:43–64. doi: 10.1016/0167-6296(91)90016-g. [DOI] [PubMed] [Google Scholar]
- Woodruff TJ, Rosbrook B, Pierce J, Glantz SA. Lower levels of cigarette consumption found in smoke-free workplaces in California. Arch Intern Med. 1993;153(12):1485–1493. [PubMed] [Google Scholar]
- Yurekli AA, Zhang P. The impact of clean indoor-air laws and cigarette smuggling on demand for cigarettes: an empirical model. Health Econ. 2000;9(2):159–170. doi: 10.1002/(sici)1099-1050(200003)9:2<159::aid-hec499>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]


