Abstract
Context
Population-level coverage for immunization against many vaccine-preventable diseases remains below optimal rates in the U.S. The Community Preventive Services Task Force recently recommended several interventions to increase vaccination coverage based on systematic reviews of the evaluation literature. The present study provides the economic results from those reviews.
Evidence acquisition
A systematic review was conducted (search period, January 1980 through February 2012) to identify economic evaluations of 12 interventions recommended by the Task Force. Evidence was drawn from included studies; estimates were constructed for the population reach of each strategy, cost of implementation, and cost per additional vaccinated person because of the intervention. Analyses were conducted in 2014.
Evidence synthesis
Reminder systems, whether for clients or providers, were among the lowest-cost strategies to implement and the most cost effective in terms of additional people vaccinated. Strategies involving home visits and combination strategies in community settings were both costly and less cost effective. Strategies based in settings such as schools and managed care organizations that reached the target population achieved additional vaccinations in the middle range of cost effectiveness.
Conclusions
The interventions recommended by the Task Force differed in reach, cost, and cost effectiveness. This systematic review presents the economic information for 12 effective strategies to increase vaccination coverage that can guide implementers in their choice of interventions to fit their local needs, available resources, and budget.
Context
Vaccines are effective against a range of diseases and have a proven record of averting serious illness and death.1,2 Based on proven effectiveness, the Advisory Committee on Immunization Practices has made recommendations for routine and targeted vaccinations since 1964, with current recommendations covering 17 vaccine-preventable diseases.3 The importance of vaccinations is further emphasized in recent economic research that indicates substantial societal savings from childhood4 and adult5 immunization programs. Despite evidence of effectiveness and economic benefits, vaccination coverage (percentage of target population vaccinated) remains below optimum, and Healthy People 20206 makes several recommendations for clinical and community-level interventions to increase coverage.
The present systematic economic review estimated the reach, cost to implement, and the cost effectiveness of 12 interventions found to be effective in increasing population-level coverage of appropriate vaccinations. The review was performed under the guidance of the Community Preventive Services Task Force (Task Force), an independent, nonfederal, unpaid panel of public health and prevention experts that provides evidence-based findings and recommendations about community preventive services, programs, and policies to improve health.
The first set of Task Force recommendations on vaccination intervention strategies was based on a Community Guide review published in 2000 (the 2000 review), covering evidence from papers appearing from 1980 through 1997.7 The present review updates the economic evidence from that review with studies published from January 1998 through May 2012. An economic review of immunization information systems, published separately,8 is not included in the present review.
Evidence Acquisition
Methods developed for conducting Community Guide systematic economic reviews can be found at www.thecommunityguide.org/about/economics.html. A coordination team (team), comprising vaccination program subject matter experts from various organizations and systematic review experts and health economists from the Community Guide Branch at CDC, conducted the review with oversight from the Task Force. The team developed analytic frameworks, systematically searched for and identified relevant studies, and abstracted information from included studies. Analyses were performed in 2014.
Conceptual Approach
The 12 interventions recommended by the Task Force to increase vaccination coverage were conceptualized in three broad categories for both the effectiveness and economics reviews.
Interventions that enhance access to vaccination services are designed to reduce financial barriers (e.g., by reducing out-of-pocket costs) or reduce the inconvenience of obtaining vaccinations by bringing the services to clients in their homes and other non-medical settings. The four interventions in this category were:
Home Visits to Increase Vaccination Rates
Reducing Client Out-of-Pocket Costs for Vaccinations
Vaccination Programs in Schools and Organized Child Care Centers
Vaccination Programs in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) Settings
Interventions that increase demand for vaccinations are designed to increase the number of people who actively seek vaccination by educating them and making them aware of their vaccination and risk status, by providing financial or material incentives, or by enacting laws. The four interventions in this category were:
Client Reminder and Recall Systems
Client or Family Incentive Rewards
Vaccination Requirements for Child Care, School, and College Attendance
Community-Based Interventions Implemented in Combination
Provider- or health system–based interventions target providers with reminders, feedback assessments, education, and other mechanisms designed to reduce missed opportunities to vaccinate receptive patients during periodic visits. The interventions in this category were:
Provider Reminders
Provider Assessment and Feedback
Standing Orders
Healthcare System-based Interventions Implemented in Combination
Detailed intervention definitions are provided in Appendix Table 1 (available online).
Inclusion Criteria
Studies were included if they:
met the definition of one or more of the 12 interventions;
were published in English;
were conducted in a high-income country9; and
estimated or modeled intervention cost or cost per additional person vaccinated (APV).
The economic concepts related to intervention outcomes in this review are described below, along with how the concepts are measured and constructed from variables usually reported in studies. The three primary outcomes of interest are reach, cost, and cost effectiveness.
Reach of intervention
The intervention’s reach is defined as the number of people in the target population, or, in the case of trials, in the group that received the intervention:
where
.
Cost of intervention
The implementation and operation of vaccination programs use staff time, equipment, supplies, materials, facilities, utilities, and other resources. The cost of intervention is the cost of resources used to implement and operate it:
.
Effectiveness of intervention
The primary effectiveness of the intervention is the number of additional people vaccinated because of the intervention. It is the incremental percentage increase in coverage owing to the intervention multiplied by the target population:
where
.
Cost effectiveness
The primary effect of the intervention is the number of APV. Cost effectiveness is defined as the economic cost incurred by the intervention to achieve a unit increase in a health outcome. The cost effectiveness of each intervention is the intervention cost per APV:
.
This review focuses on the economics of strategies to increase coverage of Advisory Committee on Immunization Practices–recommended vaccines. The cost of vaccines is excluded except for the specific intervention to improve coverage through reduced patient out-of-pocket costs. This approach is taken to ensure that intervention costs are not unduly affected by differences in vaccine prices. For example, when comparing the resource use of identical strategies to increase coverage of the human papillomavirus and the measles, mumps, and rubella vaccines, inclusion of the relevant vaccine prices will incorrectly indicate different resource use for implementing the same intervention strategies. However, it is to be noted that the uptake for different vaccines may still vary due to vaccine-specific attributes that are non-economic.10
Considerable variability is expected in estimates from reviews of public health interventions. Hence, an important objective of Community Guide economic review methods is to try to explain, or at least identify, sources of variability. Estimates are converted to per person per year (PPPY) terms to account for intervention scale and duration. Monetary values are converted to a common base year in U.S. dollars to account for inflation and denomination in foreign currencies. All monetary values in the present review are in 2013 U.S. dollars. The medians and interquartile intervals are presented, where there are more than three estimates, so that the focus is on typical results rather than outliers when unexplained variation remains.
All analysis was performed in Microsoft Excel 2013.
Review Approach
The Task Force considered the evidence for each intervention and issued individual statements of finding for them, with no formal assessment of comparative effectiveness or cost effectiveness across strategies. The approach of the present review is to describe the results from the intervention by intervention analysis of economic data and from analysis of the data pooled together from all interventions to determine how reach, cost, and cost effectiveness varied across type of intervention and type of vaccine, as well as setting and baseline rate of coverage.
Types of interventions
The three primary outcomes of reach, cost, and cost effectiveness are postulated to vary by type of intervention. In creating the categorical variable for type of intervention, strategies are combined where they: were implemented in similar settings, targeted change in the same care behavior for providers, and targeted change in client behavior through financial or material incentives. Hence, strategies based in schools and child care settings are combined, as were provider reminders and provider assessments and feedback, as well as client and family incentives and reduced out-of-pocket costs.
Settings
Reach, cost, and cost effectiveness are expected to vary based on the setting in which the intervention takes place, with setting defined as the organization or social unit where the resources were expended. Studies that evaluated interventions related to vaccination requirements for school and college attendance and reduced out-of-pocket cost had ill-defined settings, and were excluded from the setting-based analysis.
Vaccine
Cost effectiveness drawn from different studies is postulated to vary by the types of vaccine(s) promoted in the interventions. These may be multiple vaccines in a series, multiple doses of a single vaccine, or a single dose of one or more vaccines, and the resource used is expected to be greater for multiple vaccines such as the childhood series than for single dose vaccines such as that for influenza. Further, patients may be more receptive to interventions promoting certain vaccines than others, and this difference would be reflected in cost per APV.
Baseline coverage
Baseline rates of vaccination coverage are postulated to explain observed cost effectiveness, the expectation being that it would require fewer resources to achieve a percentage increment in coverage starting from rates that are low rather than from rates close to 100%. Categories of baseline rates from low to high were constructed from quartiles of estimates reported in the studies, with rates in the first quartile classified as low, those in the second and third quartiles classified as medium, and those in the fourth quartile classified as high.
Search Strategy and Yield
Twenty-four economic studies from the 2000 review (search period, January 1980 to December 1997) were included. Newer evaluation studies of the 12 intervention strategies were identified through a search of the literature published from January 1997 through February 2012. Detailed search strategy and criteria are shown in Appendix Table 2. More than 49,000 candidate studies were identified from the update search, of which 61 economic papers met the inclusion criteria (Figure 1). Hence, this review includes 84 studies: 60 studies11–71 (two61,62 papers were counted as one study) from the recent search and 24 studies72–95 from the 2000 review.7
Figure 1.
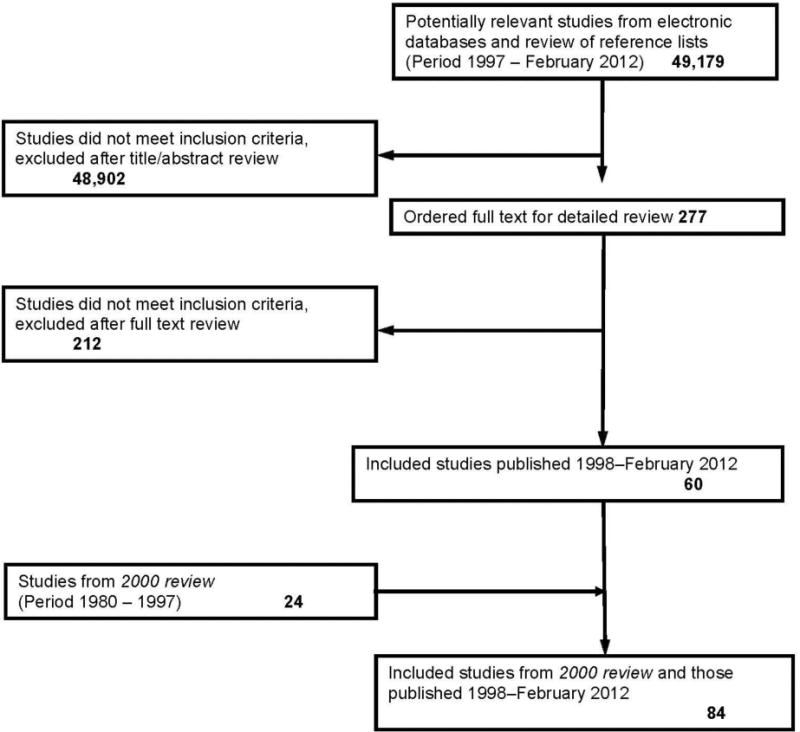
Search process.
Evidence Synthesis
Results for 12 Intervention Strategies Considered by the Task Force
The results from the economic reviews of the 12 recommended intervention strategies are summarized in Appendix Table 3, Appendix Chart 1, and Table 1. Appendix Table 3 shows the number of studies contributing to the economic evidence for each strategy, the period of study publication, the vaccines involved, and the geographic distribution across countries. Table 1 shows the reach of each intervention strategy, the cost to implement the strategy, and the cost to vaccinate an additional person using the strategy. Most studies were U.S.-based. The number of studies that reported both economic outcomes and effectiveness outcomes were almost threefold greater in the 1998–2012 period compared with 1980–1997, signaling the growing importance of the economic perspective in public health. Interventions to increase coverage of early childhood vaccines were researched most often, followed by influenza, hepatitis B, and pneumococcal vaccines. Many of the hepatitis B studies were catch-up vaccinations for adolescents and adults, especially among at-risk and new immigrant populations. Vaccines administered during adolescent years, such as human papillomavirus and meningococcal conjugate vaccine, were the least studied from the economic perspective. Client reminders and standing orders were among the least resource-intensive strategies to implement and home visits and client and family incentives were among the most resource intensive. Strategies involving population-wide vaccination policies and laws and those brought to non-medical settings frequented by a target population had among the greatest reach. Client reminders, standing orders, and those based in school settings were among the most cost-effective strategies.
Table 1.
Reach, Cost, and Cost-Effectiveness by Interventions Found to be Effective by the Task Force
| Intervention strategy |
Intervention group size Median (IQI, # Estimates) |
Cost per person per year Median (IQI, # Estimates) |
Cost per vaccinated person Median (IQI, # Estimates) |
|---|---|---|---|
| Enhancing access to vaccination services | |||
| Home visits | 575 (215 to 1,500, n=10)46,47,54,63,64,67,73,83,84 | $56 ($45 to $138, n=10)46,47,54,63,64,67,73,83,84 | $787 ($163 to $2,281, n=10)46,47,54,63,64,67,73,83,84 |
| Reducing client out-of-pocket costs | 129,16751 | $104 $35 to $222a,34,89,51 |
$1,640 $114 to $3,165a,89,51 |
| Vaccination programs in schools and organized child care centers | 5,840 (1,024 to 30,483, n=20)17,18,20,22,27,30,36,40,41,48,49,52,56,65,66,68,69 | $22 ($7 to $35, n=16)17,20,22,27,36,40,41,49,56,65,66,68,69 | $29 ($15 to $54, n=17)17,18,20,22,27,36,40,41,49,56,65,66,68,69 |
| Vaccination programs in WIC settings | 4,967 (3,645 to 11,657, n=4)31,82 | $16 ($10 to $27, n=4)31,82 | $66 ($35 to $103, n=4)31,82 |
| Increasing community demand for vaccinations | |||
| Client reminder and recall systems | 654 (273 to 5,669, n=34)13,14,21,25,35,38,42,46,47,54,59,70,75,76,78–80,85,86,88,89,91,95 | $2.13 ($0.96 to $8.00, n=34)13,14,21,25,35,38,42,46,47,54,59,70,75,76,78–80,85,86,88,89,91,95 | $15 ($8 to $184, n=32)13,14,21,25,35,42,46,47,54,59,70,75,76,79,80,85–89,91,95 |
| Client or family incentive rewardsb | 774 (39 to 18,942, n=6)15,26,37,57,60–62 | $372 ($112 to $559, n=4)26,57,60–62 | $1,032 $248 to $2,447a,26,57,60 |
| Vaccination requirements for child care, school, and college attendance | 4.1 million11 | — | — |
| Community-based intervention strategies implemented in combination | 429 (185 to 6,013, n=25)19,23,26,32,44,54,55,57,63,64,67,71,73,74,81,88,90,92–95 | $54 ($14 to $214, n=22)19,26,32,54,55,57,63,64,67,71,73,74,81,88,90,92–95 | $461 ($51 to $798, n=22)19,26,32,40,54,55,57,63,64,67,71,73,74,81,88,90,92,94,95 |
| Provider- or system-based interventions | |||
| Provider reminders | 2,910 (1,660 to 19,770, n=4)33,58,72,91 | $7 ($2 to $47, n=4)33,72,91 | $309 ($29 to $559, n=4)33,72,91 |
| Standing orders | 11,813 (1,068 to 24,266, n=4)29,33,50 | $5.55 ($5 to $13, n=4)29,33,50 | $29 ($18 to $63, n=4)29,33,50 |
| Provider assessment and feedback | 7,392 1,643 to 18,034a,16,24,45 |
$2.50 $0.22 to $4a,16,24,45 |
$8045 |
| Health care system–based intervention strategies implemented in combination | 20,000 (567 to 212,500, n=5)12,28,29,53,78 | $4 ($0.84 to $13.00, n=4)12,29,53,78 | $12 $6.00 to $21.00a,12,29,78 |
Reach, Cost, and Cost Effectiveness by Intervention Strategies
Table 2 and Appendix Chart 2 present summary statistics for reach, cost per person, and cost per APV in nine types of intervention strategies. Requiring vaccinations for school attendance did not have adequate cost and cost-effectiveness data to be included in the analysis.
Table 2.
Reach, Cost, and Cost-Effectiveness by Type of Intervention
| Intervention strategy |
Intervention group size Median (IQI, # Estimates) |
Cost per person per year Median (IQI, # Estimates) |
Cost per vaccinated person Median (IQI, # Estimates) |
|---|---|---|---|
| Home visits | 575 (215 to 1500, n=10)46,47,54,63,64,67,73,83,84 | $56 ($45 to $138, n=10)46,47,54,63,64,67,73,83,84 | $786 ($163 to $2,281, n=10)46,47,54,63,64,67,73,83,84 |
| Client or family incentive rewards and Reducing client out-of-pocket costs |
774 (85 to 53,226, n=8)15,26,37,51,57,60–62,89 | $209 ($77 to $552, n=6)26,51,57,60–62,89 | $399 ($181 to $2,806, n=5)26,51,57,60,89 |
| Vaccination programs in schools and organized child care centers | 5,840 (1,024 to 30,483, n=21)17,18,20,22,27,30,36,40,41,48,49,52,56,65,66,68,69 | $22 ($7 to $35, n=16)17,20,22,27,36,40,41,49,56,65,66,68,69 | $29 ($15 to $54, n=17)17,18,20,22,27,36,40,41,49,56,65,66,68,69 |
| Vaccination programs in WIC settings | 4,967 (3,645 to 11,657, n=4)31,82 | $16 ($10 to $27, n=4)31,82 | $66 ($35 to $103, n=4)31,82 |
| Client reminder and recall systems | 654 (273 to 5,669, n=34)13,14,21,25,35,38,42,46,47,54,59,70,75,76,78–80,85,86,88,89,91,95 | $2.13 ($0.96 to $8, n=34)13,14,21,25,35,38,42,46,47,54,59,70,75,76,78–80,85,86,88,89,91,95 | $15 ($8 to $184, n=31)13,14,21,25,35,42,46,47,54,59,70,75,76,79,80,85–89,91,95 |
| Community-based intervention strategies implemented in combination | 429 (185 to 6013, n=25)19,23,26,32,44,54,55,57,63,64,67,71,73,74,81,88,90,92–95 | $54 ($14 to $214, n=22)19,26,32,54,55,57,63,64,67,71,73,74,81,88,90,92–95 | $461 ($51 to $798, n=22)19,26,32,40,54,55,57,63,64,67,71,73,74,81,88,90,92,94,95 |
| Provider reminders and Provider assessment and feedback | 2,705 (1,734 to 15,200, n=8)16,24,33,45,58,72,91 | $4 ($0.32 to $7, n=7)16,24,33,45,72,91 | $111 ($41 to $542, n=5)33,45,72,91 |
| Standing orders | 11,813 (1,068 to 24,266, n=4)29,33,50 | $6 ($5 to $13, n=4)29,33,50 | $29 ($18 to $63, n=4)29,33,50 |
| Healthcare system-based intervention strategies implemented in combination | 20,000 (567 to 212,500, n=5)12,28,29,53,78 | $4 ($0.84 to $13, n=4)12,29,53,78 | $12 $6 to $21a,12,29,78 |
Mean and range
IQI, interquartile interval; NA, Not applicable; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children
Interventions with the greatest reach, measured as the size of the intervention group, were those implemented in health systems such as health plans, hospitals, and health centers and within non-medical organizations such as schools. Cost PPPY was highest for client incentives and reducing client out-of-pocket costs, followed by home visits and combined community-based interventions. Reminder systems, whether for providers or patients, were least expensive to implement. Interventions that target populations in particular settings (e.g., schools, WIC) fell in the middle of the cost PPPY distribution. Combined interventions in community settings require more economic resources to implement than those in health systems; in the former, activities occur in dispersed community populations, whereas the target populations for the latter are well identified in patient panels or at the point of care.
The cost per APV followed roughly the same distribution as cost PPPY. They were among the highest for combinations that included home visits and manual tracking and outreach, for home visits alone, and for client incentives and interventions that reduce out-of-pocket cost, and lowest for those implementing client reminder systems and for combined interventions in health systems. Provider reminder and provider assessment and feedback systems are an exception, ranking second in terms of fewest resources to implement but fourth in highest cost per vaccinated person. A partial explanation may be the multiple events necessary to reach a successful vaccination, from provider reminder, to provider advice to client, to client assent.
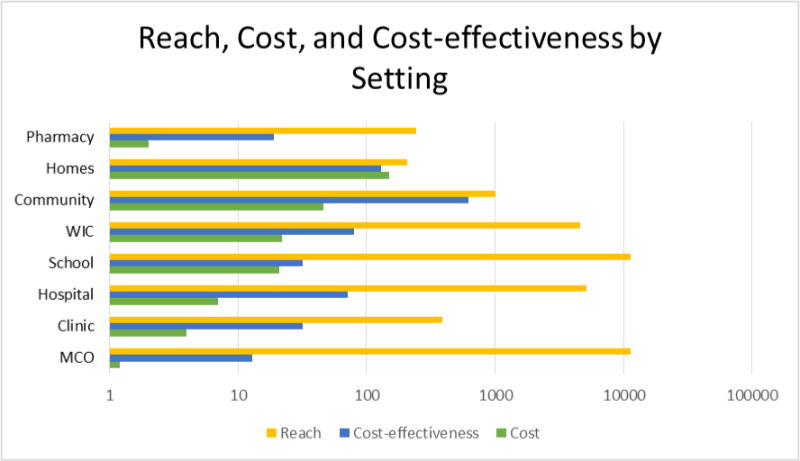
Reach, Cost, and Cost Effectiveness by Type of Setting
Table 3 and Appendix Chart 3 provide a summary, by type of setting, of the reach, cost per person, and cost per vaccinated person. Some results here are repeated from the analyses based on type of intervention strategy because those strategies were designed and defined in terms of specific settings, such as in schools and in WIC offices. Combined interventions implemented in multiple settings appear here in the category of community. The settings of interventions in the included studies were clinic, community, home, hospital, MCO, pharmacy, school, and WIC.
Table 3.
Reach, Cost, and Cost-effectiveness by Type of Setting
| Intervention strategy |
Intervention group size: Median (IQI, # Estimates) |
Cost per person per year: Median (IQI, # Estimates) |
Cost per vaccinated person: Median (IQI, # Estimates) |
|---|---|---|---|
| MCO | 11,288 (9,153 to 40,107, n=10)12–14,28,61,62,85,86 | $1.20 ($0.58 to $1.90, n=9)12–14,61,62,85,86 | $13 ($10 to $15, n=8)12–14,85,86 |
| Clinic | 390 (216 to 1,369, n=40)6,16,21,24,25,35,38,42,44–47,54,57,63,64,67,70,75,76,78,79,87–89,91,93,95 | $4 ($1.28 to $23, n=39)6,16,21,24,25,35,38,42,45–47,54,57,63,64,67,70,75,76,78,79,88,89,91,93,95 | $32 ($7 to $350, n=33)6,21,25,35,42,45–47,54,57,63,64,67,70,75,76,79,88,89,91,95 |
| Hospital | 5,161 (2,232 to 24,266, n=8)29,33,50,58,72 | $7 ($5 to $15, n=7)29,33,50,72 | $71 ($21 to $508, n=7)29,33,50,72 |
| School | 11,335 (2,010 to 49,202, n=18)11,17,20,22,27,36,40,41,49,56,65,66,68,69 | $21 ($6 to $35, n=17)11,17,18,20,22,27,36,40,41,49,56,65,66,68,69 | $32 ($16 to $64, n=18)11,17,18,20,22,27,36,40,41,49,56,65,66,68,69 |
| WIC | 4,585 (1,828 to 9,554, n=5)31,32,82 | $22 ($10 to $145, n=5)31,32,82 | $80 ($41 to $3116, n=5)31,32,82 |
| Community | 1,009 (288 to 6416, n=26)15,19,23,26,37,44,46,47,51,53–55,57,59,60,71,74,81,90,92,94 | $46 ($14 to $220, n=22)19,23,26,46,47,51,53–55,57,59,60,71,74,81,90,92,94 | $617 ($202 to $2450, n=22)19,23,26,40,46,47,51,54,55,57,59,60,71,74,81,90,92,94 |
| Homes | 208 81 to 305a73,83,84 | $149 $78 to $278a73,83,84 | $129 $100 to $183a73,83,84 |
| Pharmacy | 24280 | $280 | $1980 |
Mean and range
IQI, interquartile interval; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children
The greatest reach was achieved primarily in healthcare systems such as MCOs, where implementers were able to access clients through membership databases, and in hospital settings, where implementers targeted admitted patients. Large segments of target populations were also reached by bringing vaccines and their administration to clients in non-healthcare settings such as schools and WIC offices. Cost to implement was highest among interventions in homes, communities, and WIC settings and lowest in MCOs and general practice clinics. The rank order of cost to vaccinate an additional person mirrored the order observed for cost to implement.
Appendix Table 4 provides median or mean cost per vaccinated person cross-tabulated by type of vaccine and setting. The most prevalent types of vaccines evaluated in immunization programs that were also implemented in multiple settings were various childhood series, influenza, and hepatitis B. These are in the first three rows of the table. For the childhood series, the most cost effective were interventions implemented by MCOs, the least were those based in community settings, with those based in homes in the middle range. The cost per person vaccinated in influenza vaccination programs was lowest for MCOs, followed by clinics and schools. Vaccination programs for hepatitis B that targeted children in their school setting achieved additional vaccinations at much lower cost than those based in the community setting, where many were tailored to high-risk injection drug users.
As seen in the cost per vaccinated person based on settings, intervention strategies in the community setting had the highest cost per vaccinated person and those in MCOs had the lowest, regardless of the vaccine. Two factors that contributed to the small magnitude for MCOs were the large numbers of patients targeted and the interventions in operation, namely, client reminders by mail or phone that are less costly to implement. On the other hand, the studies included in the community settings category were combined interventions that include strategies such as home visits, client or provider education, mass media, and client or provider incentives that are more resource intensive to implement.
The remaining values presented in Appendix Table 4 for other vaccines are either based on small numbers of estimates or are isolated to a few specific settings.
Cost Effectiveness by Baseline Rate of Coverage
The median baseline rate was 44% (interquartile interval=15%, 64%) for those studies also reporting cost per APV. The median cost per APV was $22 for interventions occurring in populations with low baseline rates of coverage (≤15%), $59 for those with medium coverage rates (15%–64%), and $204 for those with high baseline coverage (>65%). The data indicate the cost to vaccinate an additional person increases with baseline coverage rates.
Discussion
A limitation of the present review is the search period that ended in February 2012, which missed more-recent research in the field. An informal search indicates there is a growing body of research focused on uptake of adolescent and early adult vaccines such as human papillomavirus and meningococcal conjugate vaccine as well as research on strategies that leverage the technologies of social media and electronic health records.
Because few studies evaluated the economics of strategies among rural populations, more research is needed to identify cost-effective strategies for rural areas. Most economic studies were among children, with few focusing on adolescents. The 2000 review had none, and in the present review only six studies focused on adolescents, primarily “catch-up” hepatitis B vaccinations for middle school children.
Although reporting of costs and cost components has improved since the 2000 review,7 many studies still ascribe no economic value to volunteer work or in-kind contributions, preventing accurate estimates of societal costs. Among studies in this review, volunteers were common in community mobilization and community initiatives, and staff from schools or public health departments were used in school-based vaccination programs, sometimes to the detriment of their usual duties.17
Given the relatively high cost observed for strategies using client incentives and rewards, further research may determine the optimal type, magnitude, and timing of incentives. Evidence indicates generosity is neither necessary nor sufficient for a successful program. Small cash gifts can motivate homeless people to return for multiple doses of hepatitis B vaccinations.26,57 A program that generously distributes infant care products can fail to produce more vaccinations.44 Research on finer details is needed to optimally match the incentive to the target population and to design the process such that incentive receipt is more closely contingent on vaccination receipt.
Finally, no intervention strategy considered in this review can be effective without adequate vaccine supply and adequate reimbursement for the providers’ time to vaccinate. Although this review of evaluation studies proceeded under the assumption that all vaccines were readily available, the broader vaccine literature raises concerns about adequate financing to purchase and administer recommended vaccines,96,97 particularly the vaccine administration cost of Medicaid-eligible patients in private clinics.98,99 Issues related to financing vaccine purchases and administration will need to be addressed for success of interventions recommended by the Task Force to increase population-level coverage in real-world implementations.
Conclusions
This review provided estimates of reach, cost, and cost effectiveness for each of 12 interventions recommended by the Community Preventive Services Task Force to increase vaccination coverage. Strategies such as reminder systems targeted to clients and providers showed lower cost to implement and also lower cost per APV. On the other hand, strategies based on home visits and combination strategies in community settings cost more to implement and also to vaccinate an additional person. Strategies designed to reach large segments of a target population, such as those based in schools and WIC settings, cost relatively more to implement but were able to vaccinate large numbers at a cost in the middle range of cost effectiveness. Schools and WIC settings may also be convenient to reach children who might otherwise be unvaccinated, under-immunized, or underserved.
This review does not emphasize the ranking of strategies based on cost or cost effectiveness, as is commonly done in league tables, because a particular strategy may be preferred based on other considerations for a specific population and vaccine. The results from this review are presented as an economic assessment of a portfolio of strategies shown to be effective in increasing vaccination coverage, with local decision makers expected to choose interventions that fit their local needs, available resources, and budget. The estimates provided by this review for cost per capita to implement the different interventions and estimates of the likely cost to vaccinate an additional person using those interventions are useful information in that decision-making process.
Acknowledgments
VJ and SC contributed to the study design, literature search, data extraction, data analysis, drafts, and revisions of the manuscript. DH contributed to the study design, critically supervised the methodologies of the project, and reviewed drafts of the manuscript. JM and AP participated in the study design, initial screening process, drafts, and review of drafts of the manuscript. JC and the Community Preventive Services Task Force directed conceptualization of the review and selection of interventions included in the review, exercised overall oversight of the work, and drew conclusions from the reviewed body of evidence.
The authors are thankful for the contribution and expertise of the review coordination team. The authors would like to thank the following Community Guide staff for their assistance: Anil Thota and Randy Elder for CDC internal review, Kate W. Harris and Kristen Folsom for editorial assistance, and Onnalee Gomez for library services. We acknowledge review or comments from experts at CDC’s National Center for Immunization and Respiratory Diseases—Mark Messonnier, Fang Jun Zhou, and Megan Lindley—and from Alan Hinman at The Task Force for Global Health in Atlanta, Georgia.
Appendix
Chart 1.
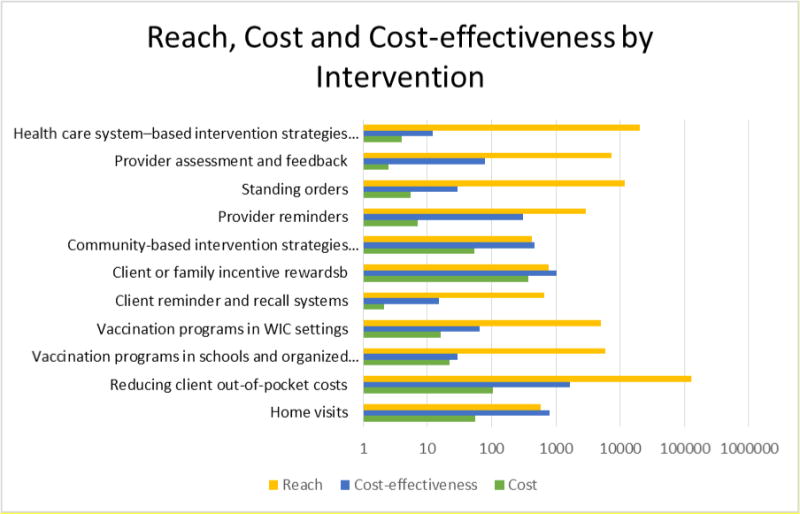
Chart 2.
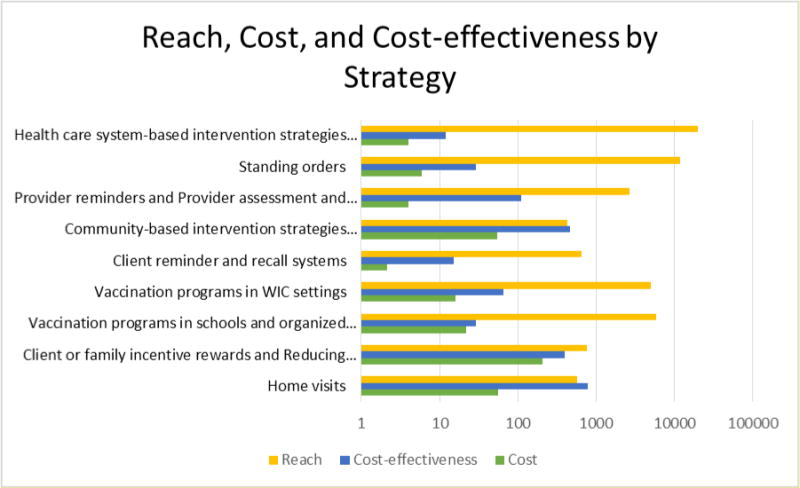
Chart 3.
Appendix Table 1.
Definitions of Interventions to Increase Population Coverage of Appropriate Vaccinations Recommended by the Community Preventive Services Task Force
| Intervention | Definition–Description |
|---|---|
| Enhancing access to vaccination services | |
| Home visits to increase vaccination rates | Home visits intended to increase vaccination rates provide vaccinations to clients in their homes or promote recommended vaccinations with referral to available immunization services. Home visits may be conducted either by vaccination providers, such as nurses, or by other providers, such as social workers. Visits generally include an assessment of client vaccination status and a brief discussion of the importance of the indicated immunizations. The intervention may be directed to all clients in a designated population, such as low-income single mothers, or only to those clients who have been unresponsive to previous intervention efforts, such as client reminder and recall systems. Home visits may be the primary or sole intervention or one component of a larger healthcare system or community-based program to increase vaccination rates. |
| Reducing client out-of-pocket costs for vaccinations | Reducing out-of-pocket costs to families for vaccinations or administration of vaccinations can be implemented by paying for vaccinations or administration, providing insurance coverage, or reducing copayments for vaccinations at the point-of-service. |
| Vaccination programs in schools and organized child care centers | Vaccination programs in schools or organized child care centers are multicomponent interventions delivered on-site to improve immunization rates in children and adolescents. These programs include two or more of the following components: (1) immunization education and promotion, (2) assessment and tracking of vaccination status, (3) referral of under-immunized school or child care center attendees to vaccination providers, and (4) provision of vaccinations. Additional components such as reduced client out-of-pocket costs, client incentives, and enhanced access to vaccination services may be provided. Organized child care centers include non-home day care, nursery or pre-school, and federal Head Start settings for children aged 5 years and younger. In most states, laws establishing vaccination requirements for school and child care center attendance require assessment, documentation, and tracking specific to each vaccine. Vaccination programs considered in this review either expanded the assessment and tracking process to other immunizations or conducted additional interventions. Vaccination programs are often collaborations between the school or child care center and local health departments, private healthcare providers, or community healthcare services. |
| Vaccination programs in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) settings | Coordinated vaccination interventions in Special Supplemental Nutrition Program for Women, Infants and Children (WIC) aim to assess the immunization status of participating infants and children and help them get recommended vaccinations. At a minimum, these interventions assess each child’s immunization status and refer them to vaccination providers as appropriate. Additional intervention components may include client reminder and recall systems, manual tracking and outreach efforts, or client incentives to obtain recommended vaccinations (e.g., monthly voucher pickup schedules that require more frequent WIC visits when vaccinations are not up-to-date). In addition, access may be enhanced by providing vaccinations in WIC settings, or coordinating WIC programs with or near healthcare services. |
| Increasing community demand for vaccinations | |
| Client reminder and recall systems | Client reminder and recall interventions are used to remind members of a target population that vaccinations are due (reminders) or late (recall). Reminders and recalls differ in content and are delivered by various methods—telephone, letter, postcard, text messages, or other. Most reminder and recall systems involve a specific client, and may be accompanied by educational messages regarding the importance of immunization for the targeted vaccine. |
| Client or family incentive rewards | Client or family incentive rewards are used to motivate people to obtain recommended vaccinations. Rewards may be monetary or non-monetary, and they may be given to clients or families in exchange for keeping an appointment, receiving a vaccination, returning for a vaccination series, or producing documentation of vaccination status. Rewards are typically small (e.g., food vouchers, gift cards, lottery prizes, baby products). Incentive reward programs are distinct from interventions that increase access to vaccination services (e.g., the provision of transportation or child care, the administration of vaccinations at no or reduced cost to clients). |
| Vaccination requirements for child care, school, and college attendance | Vaccination requirements are laws or policies requiring vaccinations or other documentation of immunity as a condition of child care, school, and college attendance. Their purpose is to reduce the incidence of vaccine-preventable disease and associated morbidity and mortality by increasing vaccination rates. Laws are created by states, with the specific vaccines required established by the legislature and embodied in statutes or adopted as administrative rules by health or education departments. Institutions, such as colleges and private schools, may establish additional vaccination policies for attendance or residence. Vaccination requirements vary across jurisdictions by comprehensiveness, acceptable documentation of immunity, access to exemptions (especially nonmedical exemptions), and the type and consistency of enforcement. |
| Community-based interventions implemented in combination | Community-based interventions implemented in combination are a set of activities coordinated in a community to increase vaccination rates within a targeted population. Activities focus on increasing community demand for vaccinations and enhancing access to vaccination services. Efforts may also include interventions directed at vaccination providers. Programs are typically coordinated by a set of partnerships between community organizations, local government, and vaccination providers. Coordinated interventions may include client reminder and recall systems, the use of staff to conduct manual outreach and tracking of clients, mass and small media, educational activities, and expanded access to vaccination services. |
| Provider- or system-based interventions | |
| Provider reminders | Provider reminder interventions inform those who administer vaccinations that individual clients are due for specific vaccinations. Techniques by which reminders are delivered vary, but can include notes prepared in advance and posted in client charts, alerts in electronic medical records, and letters sent by mail or email. |
| Standing orders | Standing orders authorize nurses, pharmacists, and other healthcare personnel where allowed by state law, to assess a client’s immunization status and administer vaccinations according to a protocol approved by an institution, physician, or other authorized practitioner. The protocol enables assessment and vaccination without the need for examination or direct order from the attending provider at the time of the interaction. Standing orders can be established for the administration of one or more specific vaccines to clients in health care settings such as clinics, hospitals, pharmacies, and long-term care facilities. In settings that require attending provider signatures for all orders, standing order protocols permit assessment and vaccination in advance of the provider signature. |
| Provider assessment and feedback | Provider assessment and feedback involves retrospectively evaluating the performance of providers in delivering one or more vaccinations to a client population and giving this information as feedback to the providers. Assessment and feedback can also involve other activities (e.g., incentives or benchmarking). |
| Healthcare system-based interventions implemented in combination | Health care system-based interventions implemented in combination involve the use of two or more coordinated interventions to increase vaccination rates within a targeted client population. Interventions are implemented primarily in health care settings, although efforts may include additional activities within the community. Specific interventions may include client reminder and recall systems; clinic-based client education; expanded access in health care settings; provider assessment and feedback; provider reminders; and standing orders. The selection and implementation of coordinated interventions may result from an overall quality improvement effort in a health care setting. |
Source: Definitions developed by the Community Guide systematic review team.
Appendix Table 2.
Search for Economic Evidence - Search Strategy and Inclusion Criteria
| The present review included studies that reported economic outcomes from the 2000 review1 (search period 1980–1997) combined with studies identified from updated searches (search period 1997–February 2012) within the standard medical and health-related research databases, Google Scholar, and databases specialized to economics and social sciences. The details of the two sets of searches are provided below. |
| Search Strategy |
| Details of the original search (1980–1997) |
The following five electronic databases were searched during the original review period of 1980 up to1997: MEDLINE, Embase, Psychlit, CAB Health, and Sociological Abstracts. The team also reviewed reference lists in articles and consulted with immunization experts. To be included, a study had to:
|
| Details of the update search (1997–February 2012) |
| The team conducted a broad literature search to identify studies assessing interventions to improve vaccination rates. The following nine databases were searched during the period of 1997 up to February 2012: CABI, CINAHL, The Cochrane Library, EMBASE, ERIC, MEDLINE, PSYCHINFO, Soci Abs and WOS. In addition, Google Scholar and specialized databases (CRD-University of York: NHS EED, EconLit, and JSTOR), were also searched. Reference lists of articles reviewed as well as lists in review articles were also considered, and subject matter experts consulted for additional references. |
Search Terms
|
To be included in the updated review, a study had to:
|
Appendix Table 3.
Community Preventive Services Task Force Recommended Interventions and Number of Included Economic Studies: Present Review and 2000 Review
| Intervention | Number of studies Jan 1980 – Feb 2012 2000 Review: Jan 1980 – Dec 1997 | By vaccine | By country |
|---|---|---|---|
| Enhancing access to vaccination services | |||
| Home visits | 91–9 42,3,10,11a |
HPV/MCV 17 MMR 15 Other childhood series 71–4,6,8,9 |
U.S. 54,6–9, U.K. 22,3; Canada 15; Australia 11 |
| Reducing client out-of-pocket costs | 312–14 113 |
Influenza12,13 Childhood series 114 |
U.S 114 Japan 112; Denmark 113 |
| Vaccination programs in schools and organized child care centers | School-based 1415–28; Child care 329–31 No economic review conductedb |
Varicella 127 Influenza 915,18–20,22,23,29–31 Hepatitis B 716,17,21,24–26,28 |
U.S. 1215–24,30,31 Canada 325–27; U.K. 128; Multiple non-U.S. locations 129 |
| Vaccination programs in WIC settings | 332–34 232,34 |
Childhood Series 332–34 | U.S. 332–34 |
| Increasing community demand for vaccinations | |||
| Client reminder & recall systems | 244–6,13,35–54 1113,36–38,40,45–48,52,53 |
Influenza 813,35–41 Pneumococcal 142 Influenza and pneumococcal 143 DTP/DTaP 144 MMR 25,45 Tetanus 246,47 Other childhood series 94,6,48–54 |
U.S. 184,6,35,36,38,40–46,48–52,54 Denmark 113 New Zealand 153 U.K. 139 Canada 35,37,47 |
| Client or family incentive rewards | 7c,55–62 No economic review conductedb |
Hepatitis B 459–62 Influenza 157,58 Childhood series 255,56 |
U.S. 459–62 Australia 255,56 Germany 157,58 |
| Vaccination requirements for child care, school & college attendance | 263,64 No studies found |
Hepatitis B 163 Varicella 164 |
U.S.63,64 |
| Community-based intervention strategies implemented in combination | 221,6–11,20,40,54,59,61,65–74 268,73 |
Hepatitis B 459,61,66,74 Influenza 320,40,72 MMR 171 DTP 173 Other childhood series 131,6–11,54,65,67–70 |
U.S. 196–11,20,40,54,59,61,65–70,73,74 Australia 11; Canada 172; Finland 171 |
| Provider- or system-based interventions | |||
| Provider reminders | 447,75–77 346,47,77d |
Pneumococcal 175 Influenza and pneumococcal 176 Tetanus 147 Childhood series 177 |
U.S. 447,75–77 |
| Standing orders | 376,78,79 No studies found |
Tdap 178, Pneumococcal 179 Influenza and pneumococcal 176 | U.S. 376,78,79 |
| Provider assessment & feedback | 380–82 No studies found |
Childhood series 380–82 | U.S. 281,82 Canada 180 |
| Health care system-based intervention strategies implemented in combination | 546,78,83–85 173,e |
Pneumococcal 283,85 Tetanus 146 TdaP 178 Childhood series 184 |
U.S. 446,78,83,84 Canada 185 |
Two studies2,10 classified as home visits in the 2000 review are now reclassified as a combination strategy in the community.
There was insufficient evidence for the Task Force to determine effectiveness.
One study46 classified as a provider reminder in the 2000 review is now reclassified as a client reminder and also as a combination strategy in the community.
One study73 classified as a combination strategy within health systems in the 2000 review is now reclassified as a combination strategy in the community.
Appendix Table 4.
Median or Mean Cost per Vaccinated Person (Number of Estimates) by Setting and Vaccine
| Clinic | Community | Hospital | MCO | Pharmacy | School | WIC | Homes | |
|---|---|---|---|---|---|---|---|---|
| Childhood Series | $225 (15)4,6,8,9,48,49,51,53,54,82 | $1,332 (8)4,6,10,14,65,68 | $577a (1)77 | $13a (3)52 | — | — | $66 (4)33,34 | $129a (3)1–3 |
| Influenza | $11 (8)13,36,37,39,40 | $69a (3)20,41,72 | — | $13a (2)35 | $19a (1)38 | $15 (6)15,18–20,22,23 | — | — |
| HBV | $399a (1)61 | $492 (8)59,61,62,66,74 | — | — | — | $38 (10)16,17,21,24–26,28 | — | — |
| DTP/DTaP | $12a (2)44 | — | — | — | — | — | — | — |
| DTP/OPV | — | $17,187a (1)11 | — | — | — | — | — | — |
| Influenza-Pneumococcal Polysaccharide and Pneumococcal Polysaccharide | $184a (1)42 | — | $71 (5)76,79 | $64a (2)43,83 | — | — | — | — |
| MMR | $232a (1)5 | $1,590a (2)5,71 | — | $6a (1)45 | — | — | — | — |
| Tdap | — | — | $21a (1)78 | — | — | — | — | — |
| Tdap/MCV/HPV | $522a (1)7 | — | — | — | — | — | — | — |
| Tetanus | $9 (4)46,47 | — | — | — | — | — | — | — |
| Varicella | — | — | — | — | — | $102a (2)27,64 | — | — |
Mean
DTP, diphtheria, tetanus, pertussis; HPV, human papillomavirus; MCV, meningococcal vaccine; MMR, measles, mumps, rubella; Tdap, tetanus, diphtheria, pertussis; OPV, oral polio vaccine; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children
Appendix References
- 1.Bond LM, Nolan TM, Lester RA. Home vaccination for children behind in their immunisation schedule: a randomised controlled trial. Med J Aust. 1998;168(10):487–490. doi: 10.5694/j.1326-5377.1998.tb141411.x. [DOI] [PubMed] [Google Scholar]
- 2.Jefferson N, Sleight G, Macfarlane A. Immunisation of children by a nurse without a doctor present. BMJ Clin Res. 1987;294(6569):423. doi: 10.1136/bmj.294.6569.423. http://dx.doi.org/10.1136/bmj.294.6569.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones AE. Domiciliary immunisation for preschool child defaulters. BMJ Clin Res. 1984;289(6456):1429. doi: 10.1136/bmj.289.6456.1429. http://dx.doi.org/10.1136/bmj.289.6456.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.LeBaron CW, Starnes DM, Rask KJ. The impact of reminder-recall interventions on low vaccination coverage in an inner-city population. Arch Pediatr Adolesc Med. 2004;158(3):255–261. doi: 10.1001/archpedi.158.3.255. http://dx.doi.org/10.1001/archpedi.158.3.255. [DOI] [PubMed] [Google Scholar]
- 5.Lemstra M, Rajakumar D, Thompson A, Moraros J. The effectiveness of telephone reminders and home visits to improve measles, mumps and rubella immunization coverage rates in children. Pediatr Child Health. 2011;16(1):e1. doi: 10.1093/pch/16.1.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rask KJ, LeBaron CW, Starnes DM. The costs of registry-based immunization interventions. Am J Prev Med. 2001;21(4):267–271. doi: 10.1016/s0749-3797(01)00370-1. http://dx.doi.org/10.1016/S0749-3797(01)00370-1. [DOI] [PubMed] [Google Scholar]
- 7.Szilagyi PG, Humiston SG, Gallivan S, Albertin C, Sandler M, Blumkin A. Effectiveness of a citywide patient immunization navigator program on improving adolescent immunizations and preventive care visit rates. Arch Pediatr Adolesc Med. 2011;165(6):547. doi: 10.1001/archpediatrics.2011.73. http://dx.doi.org/10.1001/archpediatrics.2011.73. [DOI] [PubMed] [Google Scholar]
- 8.Szilagyi PG, Schaffer S, Shone L, et al. Reducing geographic, racial, and ethnic disparities in childhood immunization rates by using reminder/recall interventions in urban primary care practices. Pediatrics. 2002;110(5):e58. doi: 10.1542/peds.110.5.e58. http://dx.doi.org/10.1542/peds.110.5.e58. [DOI] [PubMed] [Google Scholar]
- 9.Vora S, Verber L, Potts S, Dozier T, Daum RS. Effect of a novel birth intervention and reminder-recall on on-time immunization compliance in high-risk children. Hum Vaccin. 2009;5(6):395. doi: 10.4161/hv.5.6.7282. http://dx.doi.org/10.4161/hv.5.6.7282. [DOI] [PubMed] [Google Scholar]
- 10.Rodewald LE, Szilagyi PG, Humiston SG, Barth R, Kraus R, Raubertas RF. A randomized study of tracking with outreach and provider prompting to improve immunization coverage and primary care. Pediatrics. 1999;103(1):31–38. doi: 10.1542/peds.103.1.31. http://dx.doi.org/10.1542/peds.103.1.31. [DOI] [PubMed] [Google Scholar]
- 11.Wood D, Halfon N, Donald-Sherbourne C, et al. Increasing immunization rates among inner-city, African American children. JAMA. 1998;279(1):29. doi: 10.1001/jama.279.1.29. http://dx.doi.org/10.1001/jama.279.1.29. [DOI] [PubMed] [Google Scholar]
- 12.Hoshi SL, Kondo M, Honda Y, Okubo I. Cost-effectiveness analysis of influenza vaccination for people aged 65 and over in Japan. Vaccine. 2007;25(35):6511–6521. doi: 10.1016/j.vaccine.2007.05.067. http://dx.doi.org/10.1016/j.vaccine.2007.05.067. [DOI] [PubMed] [Google Scholar]
- 13.Nexoe JR, Kragstrup J, Ronne T. Impact of postal invitations and user fee on influenza vaccination rates among the elderly: a randomized controlled trial in general practice. Scand J Prim Health Care. 1997;15(2):109–112. doi: 10.3109/02813439709018497. http://dx.doi.org/10.3109/02813439709018497. [DOI] [PubMed] [Google Scholar]
- 14.Molinari NAM, Kolasa M, Messonnier ML, Schieber RA. Out-of-pocket costs of childhood immunizations: a comparison by type of insurance plan. Pediatrics. 2007;120(5):e1148. doi: 10.1542/peds.2006-3654. http://dx.doi.org/10.1542/peds.2006-3654. [DOI] [PubMed] [Google Scholar]
- 15.Carpenter LR, Lott J, Lawson BM, et al. Mass distribution of free, intranasally administered influenza vaccine in a public school system. Pediatrics. 2007;120(1):e172–e178. doi: 10.1542/peds.2006-2603. http://dx.doi.org/10.1542/peds.2006-2603. [DOI] [PubMed] [Google Scholar]
- 16.Deuson RR, Hoekstra EJ, Sedjo R, et al. The Denver school-based adolescent hepatitis B vaccination program: a cost analysis with risk simulation. Am J Public Health. 1999;89(11):1722. doi: 10.2105/ajph.89.11.1722. http://dx.doi.org/10.2105/AJPH.89.11.1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dilraj A, Strait-Jones J, Nagao M, Cui K, Terrell-Perica S, Effler PV. A statewide hepatitis B vaccination program for school children in Hawaii: vaccination series completion and participation rates over consecutive school years. Public Health Rep. 2003;118(2):127. doi: 10.1016/S0033-3549(04)50227-3. http://dx.doi.org/10.1016/S0033-3549(04)50227-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Effler PV, Chu C, He H, et al. Statewide school-located influenza vaccination program for children 5–13 years of age, Hawaii, USA. Emerg Infect Dis. 2010;16(2):244. doi: 10.3201/eid1602.091375. http://dx.doi.org/10.3201/eid1602.091375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hull HF, Frauendienst RS, Gundersen ML, Monsen SM, Fishbein DB. School-based influenza immunization. Vaccine. 2008;26(34):4312–4313. doi: 10.1016/j.vaccine.2008.06.015. http://dx.doi.org/10.1016/j.vaccine.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 20.Kansagra SM, McGinty MD, Morgenthau BM, et al. Cost comparison of 2 mass vaccination campaigns against influenza A H1N1 in New York City. Am J Public Health. 2011;102(7):1378–1383. doi: 10.2105/AJPH.2011.300363. http://dx.doi.org/10.2105/AJPH.2011.300363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mark H, Conklin VG, Wolfe MC. Nurse volunteers in school-based hepatitis B immunization programs. J Sch Nurs. 2001;17(4):185. doi: 10.1177/10598405010170040301. http://dx.doi.org/10.1177/10598405010170040301. [DOI] [PubMed] [Google Scholar]
- 22.Schmier J, Li S, King JC, Nichol K, Mahadevia PJ. Benefits and costs of immunizing children against influenza at school: an economic analysis based on a large-cluster controlled clinical trial. Health Aff. 2008;27(2):w96. doi: 10.1377/hlthaff.27.2.w96. http://dx.doi.org/10.1377/hlthaff.27.2.w96. [DOI] [PubMed] [Google Scholar]
- 23.Tran CH, McElrath J, Hughes P, et al. Implementing a community-supported school-based influenza immunization program. Biosecur Bioterror. 2010;8(4):331–341. doi: 10.1089/bsp.2010.0029. http://dx.doi.org/10.1089/bsp.2010.0029. [DOI] [PubMed] [Google Scholar]
- 24.Wilson T. Economic evaluation of a metropolitan wide, school based hepatitis B vaccination program. Public Health Nurs. 2000;17(3):222–227. doi: 10.1046/j.1525-1446.2000.00222.x. http://dx.doi.org/10.1046/j.1525-1446.2000.00222.x. [DOI] [PubMed] [Google Scholar]
- 25.Guay M, Clouâtre AM, Blackburn M, et al. Effectiveness and cost comparison of two strategies for hepatitis B vaccination of schoolchildren. Can J Public Health. 2003;94(1):64–67. doi: 10.1007/BF03405055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krahn M, Guasparini R, Sherman M, Detsky AS. Costs and cost-effectiveness of a universal, school-based hepatitis B vaccination program. Am J Public Health. 1998;88(11):1638. doi: 10.2105/ajph.88.11.1638. http://dx.doi.org/10.2105/AJPH.88.11.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sweet L, Gallant P, Morris M, Halperin SA. Canada’s first universal varicella immunization program: Lessons from Prince Edward Island. Can J Infect Dis. 2003;14(1):41. doi: 10.1155/2003/904351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wallace LA, Young D, Brown A, et al. Costs of running a universal adolescent hepatitis B vaccination programme. Vaccine. 2005;23(48–49):5624–5631. doi: 10.1016/j.vaccine.2005.06.034. http://dx.doi.org/10.1016/j.vaccine.2005.06.034. [DOI] [PubMed] [Google Scholar]
- 29.Hibbert CL, Piedra PA, McLaurin KK, Vesikari T, Mauskopf J, Mahadevia PJ. Cost-effectiveness of live-attenuated influenza vaccine, trivalent in preventing influenza in young children attending day-care centres. Vaccine. 2007;25(47):8010–8020. doi: 10.1016/j.vaccine.2007.09.018. http://dx.doi.org/10.1016/j.vaccine.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 30.Luce BR, Zangwill KM, Palmer CS, et al. Cost-effectiveness analysis of an intranasal influenza vaccine for the prevention of influenza in healthy children. Pediatrics. 2001;108(2):e24. doi: 10.1542/peds.108.2.e24. http://dx.doi.org/10.1542/peds.108.2.e24. [DOI] [PubMed] [Google Scholar]
- 31.Pisu M, Meltzer MI, Hurwitz ES, Haber M. Household-based costs and benefits of vaccinating healthy children in daycare against influenza virus: results from a pilot study. Pharmacoeconomics. 2005;23(1):55–67. doi: 10.2165/00019053-200523010-00005. http://dx.doi.org/10.2165/00019053-200523010-00005. [DOI] [PubMed] [Google Scholar]
- 32.Flatt K, Watson JC, Anderson KN, Logan L, Nguyen V. A cost comparison of methods used to increase immunization levels in a WIC setting; Paper presented at: The 124th annual meeting and exposition of the American Public Health Association; November 17–21. 1996; New York. [Google Scholar]
- 33.Hoekstra EJ, LeBaron CW, Megaloeconomou Y, et al. Impact of a large-scale immunization initiative in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) JAMA. 1998;280(13):1143. doi: 10.1001/jama.280.13.1143. http://dx.doi.org/10.1001/jama.280.13.1143. [DOI] [PubMed] [Google Scholar]
- 34.Hutchins SS, Rosenthal J, Eason P, Swint E, Guerrero H, Hadler S. Effectiveness and cost-effectiveness of linking the special supplemental program for women, infants, and children (WIC) and immunization activities. J Public Health Policy. 1999:408–426. http://dx.doi.org/10.2307/3343128. [PubMed]
- 35.Baker AM, McCarthy B, Gurley VF, Yood MU. Influenza immunization in a managed care organization. J Gen Intern Med. 1998;13(7):469–475. doi: 10.1046/j.1525-1497.1998.00136.x. http://dx.doi.org/10.1046/j.1525-1497.1998.00136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buchner DM, Larson EB, White RF. Influenza vaccination in community elderly. A controlled trial of postcard reminders. J Am Geriatr Soc. 1987;35(8):755. doi: 10.1111/j.1532-5415.1987.tb06354.x. http://dx.doi.org/10.1111/j.1532-5415.1987.tb06354.x. [DOI] [PubMed] [Google Scholar]
- 37.Frank JW, McMurray L, Henderson M. Influenza vaccination in the elderly: 2. The economics of sending reminder letters. CMAJ. 1985;132(5):516. [PMC free article] [PubMed] [Google Scholar]
- 38.Grabenstein JD, Hartzema AG, Guess HA, Johnston WP, Rittenhouse BE. Community pharmacists as immunization advocates: cost-effectiveness of a cue to influenza vaccination. Med Care. 1992:503–513. doi: 10.1097/00005650-199206000-00004. http://dx.doi.org/10.1097/00005650-199206000-00004. [DOI] [PubMed]
- 39.Hull S, Hagdrup N, Hart B, Griffiths C, Hennessy E. Boosting uptake of influenza immunisation: a randomised controlled trial of telephone appointing in general practice. Br J Gen Pract. 2002;52(482):712. [PMC free article] [PubMed] [Google Scholar]
- 40.Moran WP, Nelson K, Wofford JL, Velez R, Case LD. Increasing influenza immunization among high-risk patients: education or financial incentive? Am J Med. 1996;101(6):612–620. doi: 10.1016/S0002-9343(96)00327-0. http://dx.doi.org/10.1016/S0002-9343(96)00327-0. [DOI] [PubMed] [Google Scholar]
- 41.Smith DM, Zhou XH, Weinberger M, Smith F, McDonald RC. Mailed reminders for area-wide influenza immunization: a randomized controlled trial. J Am Geriatr Soc. 1999;47(1):1. doi: 10.1111/j.1532-5415.1999.tb01893.x. http://dx.doi.org/10.1111/j.1532-5415.1999.tb01893.x. [DOI] [PubMed] [Google Scholar]
- 42.Winston CA, Mims AD, Leatherwood KA. Increasing pneumococcal vaccination in managed care through telephone outreach. Am J Manag Care. 2007;13(10):581. [PubMed] [Google Scholar]
- 43.Berg GD, Thomas E, Silverstein S, Neel CL, Mireles M. Reducing medical service utilization by encouraging vaccines Randomized controlled trial. Am J Prev Med. 2004;27(4):284–288. doi: 10.1016/j.amepre.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 44.Franzini L, Rosenthal J, Spears W, et al. Cost-effectiveness of childhood immunization reminder/recall systems in urban private practices. Pediatrics. 2000;106(Suppl 1):177–183. [PubMed] [Google Scholar]
- 45.Lieu TA, Black SB, Ray P, et al. Computer-generated recall letters for underimmunized children: how cost-effective? Pediatr Infect Dis J. 1997;16(1):28–33. doi: 10.1097/00006454-199701000-00007. http://dx.doi.org/10.1097/00006454-199701000-00007. [DOI] [PubMed] [Google Scholar]
- 46.Frame PS, Zimmer JG, Werth PL, Hall WJ, Eberly SW. Computer-based vs manual health maintenance tracking: a controlled trial. Arch Fam Med. 1994;3(7):581. doi: 10.1001/archfami.3.7.581. http://dx.doi.org/10.1001/archfami.3.7.581. [DOI] [PubMed] [Google Scholar]
- 47.Rosser WW, Hutchison BG, McDowell I, Newell C. Use of reminders to increase compliance with tetanus booster vaccination. CMAJ. 1992;146(6):911. [PMC free article] [PubMed] [Google Scholar]
- 48.Chiu TT. Community mobilization for preschool immunizations: the Shots by Two Project. Am J Public Health. 1997;87(3):462–463. [PubMed] [Google Scholar]
- 49.Dini EF, Linkins RW, Sigafoos J. The impact of computer-generated messages on childhood immunization coverage. Am J Prev Med. 2000;18(2):132–139. doi: 10.1016/s0749-3797(99)00086-0. http://dx.doi.org/10.1016/S0749-3797(99)00086-0. [DOI] [PubMed] [Google Scholar]
- 50.Irigoyen MM, Findley S, Earle B, Stambaugh K, Vaughan R. Impact of appointment reminders on vaccination coverage at an urban clinic. Pediatrics. 2000;106(4):919. [PubMed] [Google Scholar]
- 51.Kreuter MW, Caburnay CA, Chen JJ, Donlin MJ. Effectiveness of individually tailored calendars in promoting childhood immunization in urban public health centers. Am J Public Health. 2004;94(1):122. doi: 10.2105/ajph.94.1.122. http://dx.doi.org/10.2105/AJPH.94.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lieu TA, Capra AM, Makol J, Black SB, Shinefield HR. Effectiveness and cost-effectiveness of letters, automated telephone messages, or both for underimmunized children in a health maintenance organization. Pediatrics. 1998;101(4):e3. doi: 10.1542/peds.101.4.e3. http://dx.doi.org/10.1542/peds.101.4.e3. [DOI] [PubMed] [Google Scholar]
- 53.McLeod D, Bowie RD, Kljakovic M. The cost of childhood immunisation in general practice. N Z Med J. 1998;111(1061):73. [PubMed] [Google Scholar]
- 54.Yokley JM, Glenwick DS. Increasing the immunization of preschool children; an evaluation of applied community interventions. J Appl Behav Anal. 1984;17(3):313. doi: 10.1901/jaba.1984.17-313. http://dx.doi.org/10.1901/jaba.1984.17-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bond L, Davie G, Carlin JB, Lester R, Nolan T. Infectious disease: increases in vaccination coverage for children in child care, 1997 to 2000: an evaluation of the impact of government incentives and initiatives. Aust N Z J Public Health. 2002;26(1):58–64. doi: 10.1111/j.1467-842x.2002.tb00272.x. http://dx.doi.org/10.1111/j.1467-842X.2002.tb00272.x. [DOI] [PubMed] [Google Scholar]
- 56.Lawrence GL, MacIntyre CR, Hull BP, McIntyre PB. Effectiveness of the linkage of child care and maternity payments to childhood immunisation. Vaccine. 2004;22(17):2345–2350. doi: 10.1016/j.vaccine.2003.10.038. http://dx.doi.org/10.1016/j.vaccine.2003.10.038. [DOI] [PubMed] [Google Scholar]
- 57.Stock S, Schmidt H, Büscher G, et al. Financial incentives in the German Statutory Health Insurance: New findings, new questions. Health Policy. 2010;96(1):51–56. doi: 10.1016/j.healthpol.2009.12.015. http://dx.doi.org/10.1016/j.healthpol.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 58.Stock S, Stollenwerk B, Klever-Deichert G, et al. Preliminary analysis of short term financial implications of a prevention bonus program: First results from the German statutory health insurance. Int J Public Health. 2008;53(2):78–86. doi: 10.1007/s00038-008-7026-0. http://dx.doi.org/10.1007/s00038-008-7026-0. [DOI] [PubMed] [Google Scholar]
- 59.Greengold B, Nyamathi A, Kominski G, et al. Cost-effectiveness analysis of behavioral interventions to improve vaccination compliance in homeless adults. Vaccine. 2009;27(5):718–725. doi: 10.1016/j.vaccine.2008.11.031. http://dx.doi.org/10.1016/j.vaccine.2008.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hwang LY, Grimes CZ, Tran TQ, et al. Accelerated hepatitis B vaccination schedule among drug users: a randomized controlled trial. J Infect Dis. 2010;202(10):1500–1509. doi: 10.1086/656776. http://dx.doi.org/10.1086/656776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Seal KH, Kral AH, Lorvick J, McNees A, Gee L, Edlin BR. A randomized controlled trial of monetary incentives vs. outreach to enhance adherence to the hepatitis B vaccine series among injection drug users. Drug Alcohol Depend. 2003;71(2):127–131. doi: 10.1016/s0376-8716(03)00074-7. http://dx.doi.org/10.1016/S0376-8716(03)00074-7. [DOI] [PubMed] [Google Scholar]
- 62.Stitzer ML, Polk T, Bowles S, Kosten T. Drug users’ adherence to a 6-month vaccination protocol: effects of motivational incentives. Drug Alcohol Depend. 2010;107(1):76–79. doi: 10.1016/j.drugalcdep.2009.09.006. http://dx.doi.org/10.1016/j.drugalcdep.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Jacobs RJ, Meyerhoff AS. Effect of middle school entry requirements on hepatitis B vaccination coverage. J Adolesc Health. 2004;34(5):420–423. doi: 10.1016/j.jadohealth.2003.08.014. http://dx.doi.org/10.1016/S1054-139X(03)00343-4. [DOI] [PubMed] [Google Scholar]
- 64.Abrevaya J, Mulligan K. Effectiveness of state-level vaccination mandates: evidence from the varicella vaccine. J Health Econ. 2011;30(5):966–976. doi: 10.1016/j.jhealeco.2011.06.003. http://dx.doi.org/10.1016/j.jhealeco.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 65.Browngoehl K, Kennedy K, Krotki K, Mainzer H. Increasing immunization: a Medicaid managed care model. Pediatrics. 1997;99(1):e4. doi: 10.1542/peds.99.1.e4. http://dx.doi.org/10.1542/peds.99.1.e4. [DOI] [PubMed] [Google Scholar]
- 66.Deuson RR, Brodovicz KG, Barker L, Zhou F, Euler GL. Economic analysis of a child vaccination project among Asian Americans in Philadelphia, PA. Arch Pediatr Adolesc Med. 2001;155(8):909–914. doi: 10.1001/archpedi.155.8.909. http://dx.doi.org/10.1001/archpedi.155.8.909. [DOI] [PubMed] [Google Scholar]
- 67.El-Mohandes AAE, Katz KS, El-Khorazaty MN, et al. The effect of a parenting education program on the use of preventive pediatric health care services among low-income, minority mothers: a randomized, controlled study. Pediatrics. 2003;111(6):1324. doi: 10.1542/peds.111.6.1324. http://dx.doi.org/10.1542/peds.111.6.1324. [DOI] [PubMed] [Google Scholar]
- 68.Hand JS, Anderson D, Feffer D, Day C. A successful school immunization program–or not? J Sch Health. 1980;50(1):50. doi: 10.1111/j.1746-1561.1980.tb03888.x. http://dx.doi.org/10.1111/j.1746-1561.1980.tb03888.x. [DOI] [PubMed] [Google Scholar]
- 69.Hoekstra EJ, LeBaron CW, Johnson-Partlow TLD. Does reminder-recall augment the impact of voucher incentives on immunization rates among inner-city infants enrolled in WIC? J Pediatr. 1999;135(2 Part 1):261. doi: 10.1016/s0022-3476(99)70033-8. http://dx.doi.org/10.1016/S0022-3476(99)70033-8. [DOI] [PubMed] [Google Scholar]
- 70.LeBaron CW, Starnes D, Dini EF, Chambliss JW, Chaney M. The impact of interventions by a community-based organization on inner-city vaccination coverage: Fulton County, Georgia, 1992-1993. Arch Pediatr Adolesc Med. 1998;152(4):327. doi: 10.1001/archpedi.152.4.327. http://dx.doi.org/10.1001/archpedi.152.4.327. [DOI] [PubMed] [Google Scholar]
- 71.Paunio M, Virtanen M, Peltola H, et al. Increase of vaccination coverage by mass media and individual approach: intensified measles, mumps, and rubella prevention program in Finland. Am J Epidemiol. 1991;133(11):1152. doi: 10.1093/oxfordjournals.aje.a115827. [DOI] [PubMed] [Google Scholar]
- 72.Sander B, Kwong JC, Bauch CT, et al. Economic appraisal of Ontario’s Universal Influenza Immunization Program: a cost-utility analysis. PLoS Med. 2010;7(4):e1000256. doi: 10.1371/journal.pmed.1000256. http://dx.doi.org/10.1371/journal.pmed.1000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Westman S, Halbert RJ, Walton LG, Henneman CE. A clinic without walls: the Los Angeles Immunization Demonstration Project. Am J Public Health. 1997;87(2):293–294. [PubMed] [Google Scholar]
- 74.Zhou F, Euler GL, McPhee SJ, et al. Economic analysis of promotion of hepatitis B vaccinations among Vietnamese-American children and adolescents in Houston and Dallas. Pediatrics. 2003;111(6):1289–1296. doi: 10.1542/peds.111.6.1289. http://dx.doi.org/10.1542/peds.111.6.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shevlin JD, Summers-Bean C, Thomas D, Whitney CG, Todd D, Ray SM. A systematic approach for increasing pneumococcal vaccination rates at an inner-city public hospital. Am J Prev Med. 2002;22(2):92–97. doi: 10.1016/s0749-3797(01)00408-1. http://dx.doi.org/10.1016/S0749-3797(01)00408-1. [DOI] [PubMed] [Google Scholar]
- 76.Honeycutt AA, Coleman MS, Anderson WL, Wirth KE. Cost-effectiveness of hospital vaccination programs in North Carolina. Vaccine. 2007;25(8):1484–1496. doi: 10.1016/j.vaccine.2006.10.029. http://dx.doi.org/10.1016/j.vaccine.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 77.Bell LM, Pritchard M, Anderko R, Levenson R. A program to immunize hospitalized preschool-aged children: evaluation and impact. Pediatrics. 1997;100(2):192. doi: 10.1542/peds.100.2.192. http://dx.doi.org/10.1542/peds.100.2.192. [DOI] [PubMed] [Google Scholar]
- 78.Healy CM, Rench MA, Baker CJ. Implementation of cocooning against pertussis in a high-risk population. Clin Infect Dis. 2011;52(2):157. doi: 10.1093/cid/ciq001. http://dx.doi.org/10.1093/cid/ciq001. [DOI] [PubMed] [Google Scholar]
- 79.Middleton DB, Lin CJ, Smith KJ, et al. Economic evaluation of standing order programs for pneumococcal vaccination of hospitalized elderly patients. Infect Control Hosp Epidemiol. 2008;29(5):385–394. doi: 10.1086/587155. http://dx.doi.org/10.1086/587155. [DOI] [PubMed] [Google Scholar]
- 80.Brousseau N, Sauvageau C, Ouakki M, et al. Feasibility and impact of providing feedback to vaccinating medical clinics: evaluating a public health intervention. BMC Public Health. 2010;10(1):750. doi: 10.1186/1471-2458-10-750. http://dx.doi.org/10.1186/1471-2458-10-750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fontanesi J, De Guire M, Kopald D, Holcomb K. The price of prevention Cost of recommended activities to improve immunizations. Am J Prev Med. 2004;26(1):41–45. doi: 10.1016/j.amepre.2003.09.009. http://dx.doi.org/10.1016/j.amepre.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 82.LeBaron CW, Mercer JT, Massoudi MS, et al. Changes in clinic vaccination coverage after institution of measurement and feedback in 4 states and 2 cities. Arch Pediatr Adolesc Med. 1999;153(8):879–886. doi: 10.1001/archpedi.153.8.879. http://dx.doi.org/10.1001/archpedi.153.8.879. [DOI] [PubMed] [Google Scholar]
- 83.Ahmed F, Elbasha EE, Thompson BL, Harris JR, Sneller VP. Cost-benefit analysis of a new HEDIS performance measure for pneumococcal vaccination. Med Decis Making. 2002;22(Suppl 1):s58–s66. doi: 10.1177/027298902237711. http://dx.doi.org/10.1177/027298902237711. [DOI] [PubMed] [Google Scholar]
- 84.Hambidge SJ, Phibbs SL, Chandramouli V, Fairclough D, Steiner JF. A stepped intervention increases well-child care and immunization rates in a disadvantaged population. Pediatrics. 2009;124(2):455. doi: 10.1542/peds.2008-0446. http://dx.doi.org/10.1542/peds.2008-0446. [DOI] [PubMed] [Google Scholar]
- 85.Poirier B, De Wals P, Petit G, Erickson LJ, Pépin J. Cost-effectiveness of a 3-dose pneumococcal conjugate vaccine program in the province of Quebec, Canada. Vaccine. 2009;27(50):7105–7109. doi: 10.1016/j.vaccine.2009.09.057. http://dx.doi.org/10.1016/j.vaccine.2009.09.057. [DOI] [PubMed] [Google Scholar]
Footnotes
Points of view are those of the authors and do not necessarily reflect those of CDC.
No financial disclosures were reported by the authors of this paper.
References
- 1.Roush SW, Murphy TV, Vaccine-Preventable Disease Table Working Group Historical comparisons of morbidity and mortality for vaccine-preventable diseases in the United States. JAMA. 2007;298(18):2155–2163. doi: 10.1001/jama.298.18.2155. http://dx.doi.org/10.1001/jama.298.18.2155. [DOI] [PubMed] [Google Scholar]
- 2.CDC. Ten great public health achievements–United States, 1900–1999. MMWR Morb Mortal Wkly Rep. 1999;48(12):241. [PubMed] [Google Scholar]
- 3.Advisory Committee on Immunization Practices (ACIP) Recommendations and Immunization Schedules. www.cdc.gov/vaccines/acip/recs/index.html. Accessed july 25, 2015.
- 4.Zhou F, Shefer A, Wenger J, et al. Economic evaluation of the routine childhood immunization program in the United States, 2009. Pediatrics. 2014;133(4):577–585. doi: 10.1542/peds.2013-0698. http://dx.doi.org/10.1542/peds.2013-0698. [DOI] [PubMed] [Google Scholar]
- 5.McLaughlin JM, McGinnis JJ, Tan L, Mercatante A, Fortuna J. Estimated human and economic burden of four major adult vaccine-preventable diseases in the United States, 2013. J Prim Prev. 2015;36(4):259–273. doi: 10.1007/s10935-015-0394-3. http://dx.doi.org/10.1007/s10935-015-0394-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DHHS. Office of Disease Prevention and Health Promotion. Healthy People 2020. 2012 www.healthypeople.gov. Accessed October 10, 2012.
- 7.Briss PA, Rodewald LE, Hinman AR, et al. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. The Task Force on Community Preventive Services. Am J Prev Med. 2000;18(1Suppl):97–140. doi: 10.1016/s0749-3797(99)00118-x. http://dx.doi.org/10.1016/S0749-3797(99)00118-X. [DOI] [PubMed] [Google Scholar]
- 8.Patel M, Pabst L, Chattopadhyay S, et al. Economic review of immunization information systems to increase vaccination rates: a Community Guide systematic review. J Public Health Manag Pract. 2015;21(3):253–262. doi: 10.1097/PHH.0000000000000100. http://dx.doi.org/10.1097/PHH.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 9.World Bank Country and lending groups. 2015 data.worldbank.org/about/country-and-lending-groups. Accessed November 2, 2015.
- 10.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168(1):76–82. doi: 10.1001/jamapediatrics.2013.2752. http://dx.doi.org/10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abrevaya J, Mulligan K. Effectiveness of state-level vaccination mandates: evidence from the varicella vaccine. J Health Econ. 2011;30(5):966–976. doi: 10.1016/j.jhealeco.2011.06.003. http://dx.doi.org/10.1016/j.jhealeco.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed F, Elbasha EE, Thompson BL, Harris JR, Sneller VP. Cost-benefit analysis of a new HEDIS performance measure for pneumococcal vaccination. Med Decis Making. 2002;22(Suppl 1):s58–s66. doi: 10.1177/027298902237711. http://dx.doi.org/10.1177/027298902237711. [DOI] [PubMed] [Google Scholar]
- 13.Baker AM, McCarthy B, Gurley VF, Yood MU. Influenza immunization in a managed care organization. J Gen Intern Med. 1998;13(7):469–475. doi: 10.1046/j.1525-1497.1998.00136.x. http://dx.doi.org/10.1046/j.1525-1497.1998.00136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berg GD, Thomas E, Silverstein S, Neel CL, Mireles M. Reducing medical service utilization by encouraging vaccines: randomized controlled trial. Am J Prev Med. 2004;27(4):284–288. doi: 10.1016/j.amepre.2004.07.001. http://dx.doi.org/10.1016/j.amepre.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 15.Bond L, Davie G, Carlin JB, Lester R, Nolan T. Infectious disease: increases in vaccination coverage for children in child care, 1997 to 2000: an evaluation of the impact of government incentives and initiatives. Aust N Z J Public Health. 2002;26(1):58–64. doi: 10.1111/j.1467-842x.2002.tb00272.x. http://dx.doi.org/10.1111/j.1467-842X.2002.tb00272.x. [DOI] [PubMed] [Google Scholar]
- 16.Brousseau N, Sauvageau C, Ouakki M, et al. Feasibility and impact of providing feedback to vaccinating medical clinics: evaluating a public health intervention. BMC Public Health. 2010;10(1):750. doi: 10.1186/1471-2458-10-750. http://dx.doi.org/10.1186/1471-2458-10-750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carpenter LR, Lott J, Lawson BM, et al. Mass distribution of free, intranasally administered influenza vaccine in a public school system. Pediatrics. 2007;120(1):e172–e178. doi: 10.1542/peds.2006-2603. http://dx.doi.org/10.1542/peds.2006-2603. [DOI] [PubMed] [Google Scholar]
- 18.Deuson RR, Hoekstra EJ, Sedjo R, et al. The Denver school-based adolescent hepatitis B vaccination program: a cost analysis with risk simulation. Am J Public Health. 1999;89(11):1722. doi: 10.2105/ajph.89.11.1722. http://dx.doi.org/10.2105/AJPH.89.11.1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deuson RR, Brodovicz KG, Barker L, Zhou F, Euler GL. Economic analysis of a child vaccination project among Asian Americans in Philadelphia, PA. Arch Pediatr Adolesc Med. 2001;155(8):909–914. doi: 10.1001/archpedi.155.8.909. http://dx.doi.org/10.1001/archpedi.155.8.909. [DOI] [PubMed] [Google Scholar]
- 20.Dilraj A, Strait-Jones J, Nagao M, Cui K, Terrell-Perica S, Effler PV. A statewide hepatitis B vaccination program for school children in Hawaii: vaccination series completion and participation rates over consecutive school years. Public Health Rep. 2003;118(2):127. doi: 10.1016/S0033-3549(04)50227-3. http://dx.doi.org/10.1016/S0033-3549(04)50227-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dini EF, Linkins RW, Sigafoos J. The impact of computer-generated messages on childhood immunization coverage. Am J Prev Med. 2000;18(2):132–139. doi: 10.1016/s0749-3797(99)00086-0. http://dx.doi.org/10.1016/S0749-3797(99)00086-0. [DOI] [PubMed] [Google Scholar]
- 22.Effler PV, Chu C, He H, et al. Statewide school-located influenza vaccination program for children 5-13 years of age, Hawaii, USA. Emerg Infect Dis. 2010;16(2):244. doi: 10.3201/eid1602.091375. http://dx.doi.org/10.3201/eid1602.091375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.El-Mohandes AAE, Katz KS, El-Khorazaty MN, et al. The effect of a parenting education program on the use of preventive pediatric health care services among low-income, minority mothers: a randomized, controlled study. Pediatrics. 2003;111(6):1324. doi: 10.1542/peds.111.6.1324. http://dx.doi.org/10.1542/peds.111.6.1324. [DOI] [PubMed] [Google Scholar]
- 24.Fontanesi J, De Guire M, Kopald D, Holcomb K. The price of prevention Cost of recommended activities to improve immunizations. Am J Prev Med. 2004;26(1):41–45. doi: 10.1016/j.amepre.2003.09.009. http://dx.doi.org/10.1016/j.amepre.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 25.Franzini L, Rosenthal J, Spears W, et al. Cost-effectiveness of childhood immunization reminder/recall systems in urban private practices. Pediatrics. 2000;106(Suppl 1):177–183. [PubMed] [Google Scholar]
- 26.Greengold B, Nyamathi A, Kominski G, et al. Cost-effectiveness analysis of behavioral interventions to improve vaccination compliance in homeless adults. Vaccine. 2009;27(5):718–725. doi: 10.1016/j.vaccine.2008.11.031. http://dx.doi.org/10.1016/j.vaccine.2008.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guay M, Clouâtre AM, Blackburn M, et al. Effectiveness and cost comparison of two strategies for hepatitis B vaccination of schoolchildren. Can J Public Health. 2003;94(1):64–67. doi: 10.1007/BF03405055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hambidge SJ, Phibbs SL, Chandramouli V, Fairclough D, Steiner JF. A stepped intervention increases well-child care and immunization rates in a disadvantaged population. Pediatrics. 2009;124(2):455. doi: 10.1542/peds.2008-0446. http://dx.doi.org/10.1542/peds.2008-0446. [DOI] [PubMed] [Google Scholar]
- 29.Healy CM, Rench MA, Baker CJ. Implementation of cocooning against pertussis in a high-risk population. Clin Infect Dis. 2011;52(2):157. doi: 10.1093/cid/ciq001. http://dx.doi.org/10.1093/cid/ciq001. [DOI] [PubMed] [Google Scholar]
- 30.Hibbert CL, Piedra PA, McLaurin KK, Vesikari T, Mauskopf J, Mahadevia PJ. Cost-effectiveness of live-attenuated influenza vaccine, trivalent in preventing influenza in young children attending day-care centres. Vaccine. 2007;25(47):8010–8020. doi: 10.1016/j.vaccine.2007.09.018. http://dx.doi.org/10.1016/j.vaccine.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 31.Hoekstra EJ, LeBaron CW, Megaloeconomou Y, et al. Impact of a large-scale immunization initiative in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) JAMA. 1998;280(13):1143. doi: 10.1001/jama.280.13.1143. http://dx.doi.org/10.1001/jama.280.13.1143. [DOI] [PubMed] [Google Scholar]
- 32.Hoekstra EJ, LeBaron CW, Johnson-Partlow TLD. Does reminder-recall augment the impact of voucher incentives on immunization rates among inner-city infants enrolled in WIC? J Pediatr. 1999;135(2 Part 1):261. doi: 10.1016/s0022-3476(99)70033-8. http://dx.doi.org/10.1016/S0022-3476(99)70033-8. [DOI] [PubMed] [Google Scholar]
- 33.Honeycutt AA, Coleman MS, Anderson WL, Wirth KE. Cost-effectiveness of hospital vaccination programs in North Carolina. Vaccine. 2007;25(8):1484–1496. doi: 10.1016/j.vaccine.2006.10.029. http://dx.doi.org/10.1016/j.vaccine.2006.10.029. [DOI] [PubMed] [Google Scholar]
- 34.Hoshi SL, Kondo M, Honda Y, Okubo I. Cost-effectiveness analysis of influenza vaccination for people aged 65 and over in Japan. Vaccine. 2007;25(35):6511–6521. doi: 10.1016/j.vaccine.2007.05.067. http://dx.doi.org/10.1016/j.vaccine.2007.05.067. [DOI] [PubMed] [Google Scholar]
- 35.Hull S, Hagdrup N, Hart B, Griffiths C, Hennessy E. Boosting uptake of influenza immunisation: a randomised controlled trial of telephone appointing in general practice. Br J Gen Pract. 2002;52(482):712. [PMC free article] [PubMed] [Google Scholar]
- 36.Hull HF, Frauendienst RS, Gundersen ML, Monsen SM, Fishbein DB. School-based influenza immunization. Vaccine. 2008;26(34):4312–4313. doi: 10.1016/j.vaccine.2008.06.015. http://dx.doi.org/10.1016/j.vaccine.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 37.Hwang LY, Grimes CZ, Tran TQ, et al. Accelerated hepatitis B vaccination schedule among drug users: a randomized controlled trial. J Infect Dis. 2010;202(10):1500–1509. doi: 10.1086/656776. http://dx.doi.org/10.1086/656776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Irigoyen MM, Findley S, Earle B, Stambaugh K, Vaughan R. Impact of appointment reminders on vaccination coverage at an urban clinic. Pediatrics. 2000;106(4):919. [PubMed] [Google Scholar]
- 39.Jacobs RJ, Meyerhoff AS. Effect of middle school entry requirements on hepatitis B vaccination coverage. J Adolesc Health. 2004;34(5):420–423. doi: 10.1016/j.jadohealth.2003.08.014. http://dx.doi.org/10.1016/S1054-139X(03)00343-4. [DOI] [PubMed] [Google Scholar]
- 40.Kansagra SM, McGinty MD, Morgenthau BM, et al. Cost comparison of 2 mass vaccination campaigns against influenza A H1N1 in New York City. Am J Public Health. 2011;102(7):1378–1383. doi: 10.2105/AJPH.2011.300363. http://dx.doi.org/10.2105/AJPH.2011.300363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Krahn M, Guasparini R, Sherman M, Detsky AS. Costs and cost-effectiveness of a universal, school-based hepatitis B vaccination program. Am J Public Health. 1998;88(11):1638. doi: 10.2105/ajph.88.11.1638. http://dx.doi.org/10.2105/AJPH.88.11.1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kreuter MW, Caburnay CA, Chen JJ, Donlin MJ. Effectiveness of individually tailored calendars in promoting childhood immunization in urban public health centers. Am J Public Health. 2004;94(1):122. doi: 10.2105/ajph.94.1.122. http://dx.doi.org/10.2105/AJPH.94.1.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lawrence GL, MacIntyre CR, Hull BP, McIntyre PB. Effectiveness of the linkage of child care and maternity payments to childhood immunisation. Vaccine. 2004;22(17):2345–2350. doi: 10.1016/j.vaccine.2003.10.038. http://dx.doi.org/10.1016/j.vaccine.2003.10.038. [DOI] [PubMed] [Google Scholar]
- 44.LeBaron CW, Starnes D, Dini EF, Chambliss JW, Chaney M. The impact of interventions by a community-based organization on inner-city vaccination coverage: Fulton County, Georgia, 1992–1993. Arch Pediatr Adolesc Med. 1998;152(4):327. doi: 10.1001/archpedi.152.4.327. http://dx.doi.org/10.1001/archpedi.152.4.327. [DOI] [PubMed] [Google Scholar]
- 45.LeBaron CW, Mercer JT, Massoudi MS, et al. Changes in clinic vaccination coverage after institution of measurement and feedback in 4 states and 2 cities. Arch Pediatr Adolesc Med. 1999;153(8):879–886. doi: 10.1001/archpedi.153.8.879. http://dx.doi.org/10.1001/archpedi.153.8.879. [DOI] [PubMed] [Google Scholar]
- 46.LeBaron CW, Starnes DM, Rask KJ. The impact of reminder-recall interventions on low vaccination coverage in an inner-city population. Arch Pediatr Adolesc Med. 2004;158(3):255–261. doi: 10.1001/archpedi.158.3.255. http://dx.doi.org/10.1001/archpedi.158.3.255. [DOI] [PubMed] [Google Scholar]
- 47.Lemstra M, Rajakumar D, Thompson A, Moraros J. The effectiveness of telephone reminders and home visits to improve measles, mumps and rubella immunization coverage rates in children. Pediatr Child Health. 2011;16(1):e1. doi: 10.1093/pch/16.1.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Luce BR, Zangwill KM, Palmer CS, et al. Cost-effectiveness analysis of an intranasal influenza vaccine for the prevention of influenza in healthy children. Pediatrics. 2001;108(2):e24. doi: 10.1542/peds.108.2.e24. http://dx.doi.org/10.1542/peds.108.2.e24. [DOI] [PubMed] [Google Scholar]
- 49.Mark H, Conklin VG, Wolfe MC. Nurse volunteers in school-based hepatitis B immunization programs. J Sch Nurs. 2001;17(4):185. doi: 10.1177/10598405010170040301. http://dx.doi.org/10.1177/10598405010170040301. [DOI] [PubMed] [Google Scholar]
- 50.Middleton DB, Lin CJ, Smith KJ, et al. Economic evaluation of standing order programs for pneumococcal vaccination of hospitalized elderly patients. Infect Control Hosp Epidemiol. 2008;29(5):385–394. doi: 10.1086/587155. http://dx.doi.org/10.1086/587155. [DOI] [PubMed] [Google Scholar]
- 51.Molinari NAM, Kolasa M, Messonnier ML, Schieber RA. Out-of-pocket costs of childhood immunizations: a comparison by type of insurance plan. Pediatrics. 2007;120(5):e1148. doi: 10.1542/peds.2006-3654. http://dx.doi.org/10.1542/peds.2006-3654. [DOI] [PubMed] [Google Scholar]
- 52.Pisu M, Meltzer MI, Hurwitz ES, Haber M. Household-based costs and benefits of vaccinating healthy children in daycare against influenza virus: results from a pilot study. Pharmacoeconomics. 2005;23(1):55–67. doi: 10.2165/00019053-200523010-00005. http://dx.doi.org/10.2165/00019053-200523010-00005. [DOI] [PubMed] [Google Scholar]
- 53.Poirier B, De Wals P, Petit G, Erickson LJ, Pepin J. Cost-effectiveness of a 3-dose pneumococcal conjugate vaccine program in the province of Quebec, Canada. Vaccine. 2009;27(50):7105–7109. doi: 10.1016/j.vaccine.2009.09.057. http://dx.doi.org/10.1016/j.vaccine.2009.09.057. [DOI] [PubMed] [Google Scholar]
- 54.Rask KJ, LeBaron CW, Starnes DM. The costs of registry-based immunization interventions. Am J Prev Med. 2001;21(4):267–271. doi: 10.1016/s0749-3797(01)00370-1. http://dx.doi.org/10.1016/S0749-3797(01)00370-1. [DOI] [PubMed] [Google Scholar]
- 55.Sander B, Kwong JC, Bauch CT, et al. Economic appraisal of Ontario’s Universal Influenza Immunization Program: a cost-utility analysis. PLoS Med. 2010;7(4):e1000256. doi: 10.1371/journal.pmed.1000256. http://dx.doi.org/10.1371/journal.pmed.1000256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schmier J, Li S, King JC, Nichol K, Mahadevia PJ. Benefits and costs of immunizing children against influenza at school: an economic analysis based on a large-cluster controlled clinical trial. Health Aff. 2008;27(2):w96. doi: 10.1377/hlthaff.27.2.w96. http://dx.doi.org/10.1377/hlthaff.27.2.w96. [DOI] [PubMed] [Google Scholar]
- 57.Seal KH, Kral AH, Lorvick J, McNees A, Gee L, Edlin BR. A randomized controlled trial of monetary incentives vs. outreach to enhance adherence to the hepatitis B vaccine series among injection drug users. Drug Alcohol Depend. 2003;71(2):127–131. doi: 10.1016/s0376-8716(03)00074-7. http://dx.doi.org/10.1016/S0376-8716(03)00074-7. [DOI] [PubMed] [Google Scholar]
- 58.Shevlin JD, Summers-Bean C, Thomas D, Whitney CG, Todd D, Ray SM. A systematic approach for increasing pneumococcal vaccination rates at an inner-city public hospital. Am J Prev Med. 2002;22(2):92–97. doi: 10.1016/s0749-3797(01)00408-1. http://dx.doi.org/10.1016/S0749-3797(01)00408-1. [DOI] [PubMed] [Google Scholar]
- 59.Smith DM, Zhou XH, Weinberger M, Smith F, McDonald RC. Mailed reminders for area-wide influenza immunization: a randomized controlled trial. J Am Geriatr Soc. 1999;47(1):1. doi: 10.1111/j.1532-5415.1999.tb01893.x. http://dx.doi.org/10.1111/j.1532-5415.1999.tb01893.x. [DOI] [PubMed] [Google Scholar]
- 60.Stitzer ML, Polk T, Bowles S, Kosten T. Drug users’ adherence to a 6-month vaccination protocol: effects of motivational incentives. Drug Alcohol Depend. 2010;107(1):76–79. doi: 10.1016/j.drugalcdep.2009.09.006. http://dx.doi.org/10.1016/j.drugalcdep.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stock S, Stollenwerk B, Klever-Deichert G, et al. Preliminary analysis of short term financial implications of a prevention bonus program: First results from the German statutory health insurance. Int J Public Health. 2008;53(2):78–86. doi: 10.1007/s00038-008-7026-0. http://dx.doi.org/10.1007/s00038-008-7026-0. [DOI] [PubMed] [Google Scholar]
- 62.Stock S, Schmidt H, Buscher G, et al. Financial incentives in the German Statutory Health Insurance: new findings, new questions. Health Policy. 2010;96(1):51–56. doi: 10.1016/j.healthpol.2009.12.015. http://dx.doi.org/10.1016/j.healthpol.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 63.Szilagyi PG, Humiston SG, Gallivan S, Albertin C, Sandler M, Blumkin A. Effectiveness of a citywide patient immunization navigator program on improving adolescent immunizations and preventive care visit rates. Arch Pediatr Adolesc Med. 2011;165(6):547. doi: 10.1001/archpediatrics.2011.73. http://dx.doi.org/10.1001/archpediatrics.2011.73. [DOI] [PubMed] [Google Scholar]
- 64.Szilagyi PG, Schaffer S, Shone L, et al. Reducing geographic, racial, and ethnic disparities in childhood immunization rates by using reminder/recall interventions in urban primary care practices. Pediatrics. 2002;110(5):e58. doi: 10.1542/peds.110.5.e58. http://dx.doi.org/10.1542/peds.110.5.e58. [DOI] [PubMed] [Google Scholar]
- 65.Sweet L, Gallant P, Morris M, Halperin SA. Canada’s first universal varicella immunization program: Lessons from Prince Edward Island. Can J Infect Dis. 2003;14(1):41. doi: 10.1155/2003/904351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tran CH, McElrath J, Hughes P, et al. Implementing a community-supported school-based influenza immunization program. Biosecur Bioterror. 2010;8(4):331–341. doi: 10.1089/bsp.2010.0029. http://dx.doi.org/10.1089/bsp.2010.0029. [DOI] [PubMed] [Google Scholar]
- 67.Vora S, Verber L, Potts S, Dozier T, Daum RS. Effect of a novel birth intervention and reminder-recall on on-time immunization compliance in high-risk children. Hum Vaccin. 2009;5(6):395. doi: 10.4161/hv.5.6.7282. http://dx.doi.org/10.4161/hv.5.6.7282. [DOI] [PubMed] [Google Scholar]
- 68.Wallace LA, Young D, Brown A, et al. Costs of running a universal adolescent hepatitis B vaccination programme. Vaccine. 2005;23(48–49):5624–5631. doi: 10.1016/j.vaccine.2005.06.034. http://dx.doi.org/10.1016/j.vaccine.2005.06.034. [DOI] [PubMed] [Google Scholar]
- 69.Wilson T. Economic evaluation of a metropolitan wide, school based hepatitis B vaccination program. Public Health Nurs. 2000;17(3):222–227. doi: 10.1046/j.1525-1446.2000.00222.x. http://dx.doi.org/10.1046/j.1525-1446.2000.00222.x. [DOI] [PubMed] [Google Scholar]
- 70.Winston CA, Mims AD, Leatherwood KA. Increasing pneumococcal vaccination in managed care through telephone outreach. Am J Manag Care. 2007;13(10):581. [PubMed] [Google Scholar]
- 71.Zhou F, Euler GL, McPhee SJ, et al. Economic analysis of promotion of hepatitis B vaccinations among Vietnamese-American children and adolescents in Houston and Dallas. Pediatrics. 2003;111(6):1289–1296. doi: 10.1542/peds.111.6.1289. http://dx.doi.org/10.1542/peds.111.6.1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bell LM, Pritchard M, Anderko R, Levenson R. A program to immunize hospitalized preschool-aged children: evaluation and impact. Pediatrics. 1997;100(2):192. doi: 10.1542/peds.100.2.192. http://dx.doi.org/10.1542/peds.100.2.192. [DOI] [PubMed] [Google Scholar]
- 73.Bond LM, Nolan TM, Lester RA. Home vaccination for children behind in their immunisation schedule: a randomised controlled trial. Med J Aust. 1998;168(10):487–490. doi: 10.5694/j.1326-5377.1998.tb141411.x. [DOI] [PubMed] [Google Scholar]
- 74.Browngoehl K, Kennedy K, Krotki K, Mainzer H. Increasing immunization: a Medicaid managed care model. Pediatrics. 1997;99(1):e4. doi: 10.1542/peds.99.1.e4. http://dx.doi.org/10.1542/peds.99.1.e4. [DOI] [PubMed] [Google Scholar]
- 75.Buchner DM, Larson EB, White RF. Influenza vaccination in community elderly. A controlled trial of postcard reminders. J Am Geriatr Soc. 1987;35(8):755. doi: 10.1111/j.1532-5415.1987.tb06354.x. http://dx.doi.org/10.1111/j.1532-5415.1987.tb06354.x. [DOI] [PubMed] [Google Scholar]
- 76.Chiu TT. Community mobilization for preschool immunizations: the Shots by Two Project. Am J Public Health. 1997;87(3):462–463. [PubMed] [Google Scholar]
- 77.Flatt K, Watson JC, Anderson KN, Logan L, Nguyen V. A cost comparison of methods used to increase immunization levels in a WIC setting. Paper presented at: The 124th annual meeting and exposition of the American Public Health Association; November 17-21. 1996; New York. [Google Scholar]
- 78.Frame PS, Zimmer JG, Werth PL, Hall WJ, Eberly SW. Computer-based vs manual health maintenance tracking: a controlled trial. Arch Fam Med. 1994;3(7):581. doi: 10.1001/archfami.3.7.581. http://dx.doi.org/10.1001/archfami.3.7.581. [DOI] [PubMed] [Google Scholar]
- 79.Frank JW, McMurray L, Henderson M. Influenza vaccination in the elderly: 2. The economics of sending reminder letters. CMAJ. 1985;132(5):516. [PMC free article] [PubMed] [Google Scholar]
- 80.Grabenstein JD, Hartzema AG, Guess HA, Johnston WP, Rittenhouse BE. Community pharmacists as immunization advocates: cost-effectiveness of a cue to influenza vaccination. Med Care. 1992:503–513. doi: 10.1097/00005650-199206000-00004. http://dx.doi.org/10.1097/00005650-199206000-00004. [DOI] [PubMed]
- 81.Hand JS, Anderson D, Feffer D, Day C. A successful school immunization program–or not? J Sch Health. 1980;50(1):50. doi: 10.1111/j.1746-1561.1980.tb03888.x. http://dx.doi.org/10.1111/j.1746-1561.1980.tb03888.x. [DOI] [PubMed] [Google Scholar]
- 82.Hutchins SS, Rosenthal J, Eason P, Swint E, Guerrero H, Hadler S. Effectiveness and cost-effectiveness of linking the special supplemental program for women, infants, and children (WIC) and immunization activities. J Public Health Policy. 1999:408–426. http://dx.doi.org/10.2307/3343128. [PubMed]
- 83.Jefferson N, Sleight G, Macfarlane A. Immunisation of children by a nurse without a doctor present. BMJ Clin Res. 1987;294(6569):423. doi: 10.1136/bmj.294.6569.423. http://dx.doi.org/10.1136/bmj.294.6569.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jones AE. Domiciliary immunisation for preschool child defaulters. BMJ Clin Res. 1984;289(6456):1429. doi: 10.1136/bmj.289.6456.1429. http://dx.doi.org/10.1136/bmj.289.6456.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lieu TA, Black SB, Ray P, et al. Computer-generated recall letters for underimmunized children: how cost-effective? Pediatr Infect Dis J. 1997;16(1):28–33. doi: 10.1097/00006454-199701000-00007. http://dx.doi.org/10.1097/00006454-199701000-00007. [DOI] [PubMed] [Google Scholar]
- 86.Lieu TA, Capra AM, Makol J, Black SB, Shinefield HR. Effectiveness and cost-effectiveness of letters, automated telephone messages, or both for underimmunized children in a health maintenance organization. Pediatrics. 1998;101(4):e3. doi: 10.1542/peds.101.4.e3. http://dx.doi.org/10.1542/peds.101.4.e3. [DOI] [PubMed] [Google Scholar]
- 87.McLeod D, Bowie RD, Kljakovic M. The cost of childhood immunisation in general practice. N Z Med J. 1998;111(1061):73. [PubMed] [Google Scholar]
- 88.Moran WP, Nelson K, Wofford JL, Velez R, Case LD. Increasing influenza immunization among high-risk patients: education or financial incentive? Am J Med. 1996;101(6):612–620. doi: 10.1016/S0002-9343(96)00327-0. http://dx.doi.org/10.1016/S0002-9343(96)00327-0. [DOI] [PubMed] [Google Scholar]
- 89.Nexoe JR, Kragstrup J, Ronne T. Impact of postal invitations and user fee on influenza vaccination rates among the elderly: a randomized controlled trial in general practice. Scand J Prim Health Care. 1997;15(2):109–112. doi: 10.3109/02813439709018497. http://dx.doi.org/10.3109/02813439709018497. [DOI] [PubMed] [Google Scholar]
- 90.Paunio M, Virtanen M, Peltola H, et al. Increase of vaccination coverage by mass media and individual approach: intensified measles, mumps, and rubella prevention program in Finland. Am J Epidemiol. 1991;133(11):1152. doi: 10.1093/oxfordjournals.aje.a115827. [DOI] [PubMed] [Google Scholar]
- 91.Rosser WW, Hutchison BG, McDowell I, Newell C. Use of reminders to increase compliance with tetanus booster vaccination. CMAJ. 1992;146(6):911. [PMC free article] [PubMed] [Google Scholar]
- 92.Rodewald LE, Szilagyi PG, Humiston SG, Barth R, Kraus R, Raubertas RF. A randomized study of tracking with outreach and provider prompting to improve immunization coverage and primary care. Pediatrics. 1999;103(1):31–38. doi: 10.1542/peds.103.1.31. http://dx.doi.org/10.1542/peds.103.1.31. [DOI] [PubMed] [Google Scholar]
- 93.Westman S, Halbert RJ, Walton LG, Henneman CE. A clinic without walls: the Los Angeles Immunization Demonstration Project. Am J Public Health. 1997;87(2):293–294. [PubMed] [Google Scholar]
- 94.Wood D, Halfon N, Donald-Sherbourne C, et al. Increasing immunization rates among inner-city, African American children. JAMA. 1998;279(1):29. doi: 10.1001/jama.279.1.29. http://dx.doi.org/10.1001/jama.279.1.29. [DOI] [PubMed] [Google Scholar]
- 95.Yokley JM, Glenwick DS. Increasing the immunization of preschool children; an evaluation of applied community interventions. J Appl Behav Anal. 1984;17(3):313. doi: 10.1901/jaba.1984.17-313. http://dx.doi.org/10.1901/jaba.1984.17-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lindley C, Orenstein W, Shen A, Rodewald L, Birkhead G. Assuring vaccination of children and adolescents without financial barriers: recommendations from the National Vaccine Advisory Committee (NVAC), US DHHS. Washington, DC: National Vaccine Advisory Committee Vaccine Financing Working Group; 2009. [Google Scholar]
- 97.Lindley MC, Shen AK, Orenstein WA, Rodewald LE, Birkhead GS. Financing the delivery of vaccines to children and adolescents: challenges to the current system. Pediatrics. 2009;124(Suppl 5):S548. doi: 10.1542/peds.2009-1542O. http://dx.doi.org/10.1542/peds.2009-1542O. [DOI] [PubMed] [Google Scholar]
- 98.AAP Task Force on Immunization. Immunization financing: where is the breaking point? 2007 Discussion paper. www.aap.org/en-us/Documents/immunization_taskforcewhitepaper.pdf Accessed November 2, 2015.
- 99.Freed GL, Cowan AE, Clark SJ. Primary care physician perspectives on reimbursement for childhood immunizations. Pediatrics. 2008;122(6):1319–1324. doi: 10.1542/peds.2008-2033. http://dx.doi.org/10.1542/peds.2008-2033. [DOI] [PubMed] [Google Scholar]


