Abstract
Distal biceps tendon ruptures are relatively rare. Patients are usually middle-aged men involved in heavy labor. Patients usually present with the history of a pop and a proximal migration of the biceps muscle belly. Clinical exam should be sufficient to diagnose a complete rupture. Several specific tests have been described. Ultrasound scanning or MRI can help confirm the diagnosis. Radiographs are not needed to diagnose distal biceps tendon rupture but may show typical findings. Imaging, more specifically the flexion-abduction-supination (FABS) view MRI, is particularly helpful in the case of a partial rupture or chronic rupture of the distal biceps tendon. Results of surgical reinsertion of the distal biceps have been shown to be superior to conservative treatment. Different techniques and approaches have been described with specific advantages and disadvantages. Primary repair of the tendon is preferred. If this is no longer possible in chronic tears, an augmentation can be done using tendon graft. Results of surgical treatment are good in the vast majority of patients. Reruptures are rare but minor complications are common. Major complications may include posterior interosseous nerve palsy or radioulnar synostosis, but the risk of these complications may be decreased by meticulous attention to detail during surgery.
Keywords: Biceps tendon, Avulsion, Rupture, Single incision, Double incision, Biceps endoscopy
Introduction
With an incidence rate of about 1.2–2.5 per 100,000, distal biceps brachii tendon avulsions and/or ruptures are relatively uncommon [1, 2•]. Both a decreased arterial blood supply and mechanical impingement have been suggested as possible mechanisms predisposing to a rupture [3]. Both mechanisms seem to be clinically important, as smoking has been shown to be a significant risk factor [1, 2•]. Injuries primarily affect the active middle-aged, male population involved in heavy physical work or sports, suggesting a degenerative basis for these injuries [1, 3].
The biceps brachii is composed of two heads; it originates with the long head on the supraglenoid tubercle and the short head on the coracoid process. This will insert distally on the bicipital tuberosity of the radius [4]. A branch of the musculocutaneous nerve innervates the distal biceps brachii muscle [5].
The most common mechanism by which distal biceps tendon ruptures occur is due to an eccentric load [6] such as a fall on the outstretched hand, elbow extension during heavy lifting, or an abrupt extension of the elbow with the arm in supination [7•, 8, 9]. Degeneration, inflammation of the deep radial bursa, hypovascularization, or friction of the tendon (for example, on boney irregularities at the tuberosity of the radius) is known to contribute to the possibility of rupturing the tendon. Smokers present with a seven times greater predisposition toward tendon tears [1], along with athletes who abuse or used anabolic steroids [10–13].
If treated conservatively, the patient might continuously experience weakness during supination and elbow flexion [14], and better results may be expected with surgical repair rather than nonoperative treatment [14, 15]. Complications are more common in delayed repair due to worsening scar tissue formation and retraction of the tendon over time. In some cases of severe retraction in which direct repair of the tendon to the tuberosity is no longer possible, augmentation by a tendon graft may be necessary.
Several surgical techniques have been described, most with comparable results in clinical outcomes and biomechanics. Currently, there is no clear consensus on which surgical technique should be used.
Presentation and imaging
Patients may present with pain, edema, ecchymosis, and decreased elbow supination and/or flexion strength. They may report having felt a “pop.” Some even sense that a palpable retraction of the biceps tendon and the biceps muscle may be retracted proximally (Fig. 1). Clinical exam is often sufficient to diagnose a complete distal biceps tendon avulsion [7•]. When in doubt, or when a partial rupture is suspected, ultrasonography or magnetic resonance imaging is the preferred imaging modality [8, 9].
Fig. 1.

Proximal retraction of the biceps muscle belly can occur with a complete distal biceps tendon rupture. Reprinted with Permission from MoRe Foundation
Patients may present acutely to the accidents and emergency department or with a chronic rupture to the outpatient clinic. In chronic ruptures, a delay in diagnosis is often due to a late presentation in patients with subtle symptoms.
Resisted flexion and supination may be weaker and painful, although in chronic cases, flexion strength can appear nearly normal due to brachialis contraction. Endurance will be diminished as well. Supination usually is adversely affected in chronic as well as in acute cases. Clinically, several specific tests may help diagnose biceps ruptures: (1) biceps squeeze test, (2) pronation–supination test, (3) biceps crease interval test, and (4) the hook test [16]. The biceps squeeze test is performed with the elbow flexed at around 80° and the forearm slightly pronated while the examiner squeezes the relaxed biceps. Similar to the Thompson test for Achilles ruptures, the test is positive when there is no movement of the forearm. A negative test will create a supination movement of the forearm [17]. In the pronation–supination test, the biceps muscle contour changes shape when the forearm is pronated and supinated in patients with an intact tendon. If the tendon is ruptured, this will not occur [18]. The biceps crease interval is the distance between the antecubital fossa crease and the distal biceps muscle which is increased in full-thickness distal biceps tendon ruptures, due to proximal migration of the muscle belly [19]. With the hook test, an intact biceps tendon can be hooked by the examiner from the lateral side of the antecubital fossa with one finger. This is not possible in the presence of a rupture [16]. In order to avoid false positive results from the intact lacertus fibrosus, the hook test should not be performed from the medial side. For full-thickness, complete biceps tendon ruptures, the above clinical investigations should be sufficient to make the diagnosis, and imaging is usually not needed for diagnosis [7•].
In partial tears of the distal biceps tendon, the hook test, squeeze test, and pronation–supination test will be negative and the biceps crease index will be normal. Imaging is usually necessary in cases suspicious for a partial tear.
Radiographs are typically normal although it may show associated elbow injuries and potential predisposing factors, such as flattening of the radial tuberosity which may be a sign of degenerative changes at the insertion (Fig. 2).
Fig. 2.

Lateral radiograph of a patient with a complete distal biceps tendon rupture showing flattening and degenerative changes of the bicipital tuberosity. Reprinted with Permission from MoRe Foundation
Ultrasound may be used to confirm the diagnosis [8, 9, 20, 21]. It is a cheaper imaging study than an MRI and is becoming more readily available; however, it is operator dependent (Fig. 3).
Fig. 3.

The diagnosis of a complete rupture of the distal biceps tendon can easily be confirmed with ultrasound scanning. Reprinted with Permission from MoRe Foundation
Magnetic resonance imaging [22, 23] (Fig. 4), in particular, the flexion-abduction-supination (FABS) view [24•], can be used for optimal visualization. For the FABS view, the patient is placed prone in the MRI scanner with the affected arm in full abduction above the patient’s head, with the elbow flexed to 90° and the forearm supinated [24•] (Fig. 5). Although an MRI may not be needed to confirm the diagnosis of a complete rupture, the FABS MRI view is especially helpful for the diagnosis and evaluation of partial ruptures and chronic ruptures. It allows for visualization of the entire course of the distal biceps tendon, evaluation for possible partial tear, the formation of scar tissue, and the amount of proximal retraction. This information will help the surgeon prepare for surgery.
Fig. 4.
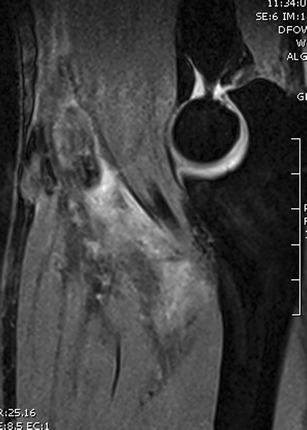
Magnetic resonance image showing a complete distal biceps tendon avulsion. Reprinted with Permission from MoRe Foundation
Fig. 5.

A FABS view MRI is particularly helpful in partial or chronic tendon ruptures. It allows for a clear view of both the insertion and the course of the tendon. Reprinted with Permission from MoRe Foundation
Treatment
Partial tears
With partial tears, patients may complain of loss of flexion and supination strength or just pain in the antecubital fossa.
Nonoperative treatment
Partial tears are usually treated nonoperatively for a minimum of 6 months. There is no consensus on which treatment modality should be used or for how long conservative treatment should be tried before surgery is indicated. A partial tear involving less than 50 % of the tendon is initially treated conservatively. Surgical debridement or primary repair can be an option if conservative therapy fails. If the partial tear is larger than 50 % of the tendon, then surgical repair is typically recommended [25].
In complete acute ruptures, surgical reattachment to bone is preferred over nonoperative treatment. Nonoperative treatment is reserved for older, low-demand patients, and those with significant comorbidities or an unacceptable high risk for surgery. Due to the increased risk of complications, chronic ruptures may be treated nonoperatively unless the injury is too disabling for a satisfactory function of the upper extremity.
Surgical repair
Different surgical techniques exist to treat distal biceps tendon tears [26].
Endoscopic technique
Endoscopic techniques are particularly helpful in diagnosing the extent of partial tears. The patient is placed supine, with the arm on an armtable. A tourniquet is used, as proximal retraction is not an issue in partial ruptures. A 2-cm incision is made centrally on the forearm, 3 cm distal to the elbow crease. Blunt dissection is carried out to the tendon. Care is taken not to injure the lateral antebrachial cutaneous nerve by dissection or retraction (Fig. 6). Retractors are used throughout the procedure, to protect neurovascular structures. The scope is entered in the bicipital bursa (Fig. 7). The scope is advanced to the bicipital tuberosity and the forearm is supinated. This opens the space between the tendon and the bone and a good view of the insertion can be obtained. We use the following algorithm. If the tear is less than 25 % of the surface of the insertion, the tear is debrided. If the tear is between 25 and 50 %, the tear is debrided and the tendon is reinserted using a bone anchor (Fig. 8). If the tear consists of more than 50 % of the tendon, the tendon is detached fully. The stump is debrided and we prefer to repair the tendon to bone, using a cortical bone technique.
Fig. 6.

The lateral antebrachial cutaneous nerve (asterisk) is located just radial to the incision superficial to the brachioradialis muscle. It is vulnerable during the approach but can also be injured by excessive retraction. Reprinted with Permission from MoRe Foundation
Fig. 7.

The scope is entered into the bicipital bursa, between the tendon and the tuberosity. Reprinted with Permission from MoRe Foundation
Fig. 8.

Endoscopic view of a bone anchor repair of a partially torn distal biceps tendon. Reprinted with Permission from MoRe Foundation
Complete tears can also be treated with the endoscopic technique described. Mostly, the endoscopy is used as an aide in retrieving the retracted tendon and finding the footprint for insertion.
Other endoscopic techniques have also been described. Duffiet et al. described a technique using a cannula, to protect the adjacent neural structures [27]. Gregory et al. used a slightly larger incision in the anterior crease of the forearm. Unfortunately, one patient had a severe neurological complication in their series [28].
The postoperative regimen depends on the procedure. Both the debridement and anchor repair are protected with a removable splint for 2 weeks. The patient is encouraged to remove the splint four times a day for a period of 15 min, to gently mobilize the elbow. A patient with a surgical repair is allowed to mobilize and load immediately.
Single-incision technique
The patient is placed in supine position with the arm on an armtable. A tourniquet can be used in acute cases, but the surgeon should be aware that this may impair the possibility of pulling the torn tendon distally. The patient’s arm is supinated on the armtable and a longitudinal 2-cm incision is made centrally on the forearm, 3 cm distal to the elbow crease in the antecubital fossa. Blunt dissection develops the plane between the brachioradialis and flexor carpi radialis muscle bellies. The lateral antebrachial cutaneous nerve can be identified superficially to the brachioradialis muscle. We tend not to dissect the nerve, and this has significantly decreased the incidence of temporary numbness of the forearm. The biceps tendon stump is typically found proximal to the elbow crease. Flexing the elbow is usually sufficient to digitally localize and mobilize the stump. It is very rarely necessary to extend the incision or the make a second incision proximal to the elbow crease. The stump is debrided to healthy tendon and the tendon is prepared for repair. Preparation of the tendon depends on the type of fixation used. Bone tunnels, bone anchors, or different types of cortical bone buttons, with or without interference screw fixation, have been successfully used to repair the distal biceps tendon back to bone. We prefer to use a cortical button as we feel that this allows for the strongest initial repair. The tendon is sutured to a cortical button using nonresorbable suture (Fig. 9). Dissection is then taken to the level of the bicipital tuberosity. In acute ruptures, this can easily be identified as the path of the tendon can be followed to the tuberosity. This is more difficult in delayed cases, as scar tissue rapidly forms in this tunnel [29]. The bicipital tuberosity is visualized with the use of retractors. Extreme care should be taken to stay on the bone of the radius if Hohman-type retractors are used around the radius, as the posterior interosseous nerve is located posterior to the bone. The bone is then prepared, depending on the preferred fixation method. For the cortical bone technique, a guide wire is drilled from the center of the tuberosity through both cortices. In order to decrease the risk of injuring the posterior interosseous nerve, the forearm needs to be supinated maximally. The guide wire is directed straight posterior or in an ulnar direction and should not be drilled distally or radially [30]. The guide wire is then overdrilled with an 8- or 9-mm canulated drill, through the first cortex. A 4.5-mm canulated drill is then used to drill the second cortex (Fig. 10). The guide wire is then removed, as well as as much bone debris as possible. The wound is then irrigated to remove the last remaining debris.
Fig. 9.

The tendon is sutured to a cortical button. The stump will be debrided, leaving a 2-mm gap between the tendon and the button. Reprinted with Permission from MoRe Foundation
Fig. 10.

Both the 8-mm drill hole in the near cortex and the 4.5-mm drill hole in the far cortex are seen. The cortical button will be pulled past the second cortex and flipped, thereby securing the tendon in the intramedullary canal of the proximal radius. Reprinted with Permission from MoRe Foundation
The arm is then supinated fully and the guide wire is advanced through the tunnel created in the radius. The guide wire is used to bring trailing sutures through the skin on the posterior forearm. With the elbow flexed, the tendon is pulled into the tunnel and the button is flipped, once it clears the second cortex. The elbow is then extended and this secures the button against the far cortex. The forearm is taken through a full range of pronation and supination to clear any soft tissue between the radius and the button. Fluoroscopy can be used to check the position of the button [31] (Fig. 11). As the endobutton technique has the highest initial fixation strength [32], aggressive rehabilitation can be started early. Postoperatively, the patient is allowed to mobilize the elbow immediately. Loading is permitted as pain allows, but patients are instructed not to load more than 20 kg for the first 3 months and to avoid peak loading.
Fig. 11.

Postoperative radiograph showing correct position of the cortical button and ingrowth of the tendon in the canal. Reprinted with Permission from MoRe Foundation
Two-incision technique
The two-incision technique is started with a transverse or longitudinal proximal incision over the distal biceps sheath. Dissection to the tuberosity is identical to the single-incision technique, as is identification and preparation of the tendon stump. With the arm supinated, passing a large curved Kelly clamp through the extensor muscles on the medial side of the radius then creates a path. A second incision is made where the Kelly clamp can be felt under the skin and progressive dissection through the extensor muscle is performed until the radial tuberosity is visualized. At this stage, be careful not to expose the ulna as this is found to increase the likelihood of radioulnar synostosis [33]. Fixation of the tendon can again be performed with various devices described above. Bone tunnels, bone anchors, or different types of cortical bone buttons, with or without interference screw fixation, have been successfully used to repair the distal biceps tendon back to bone.
Chronic ruptures
In delayed cases, the tendon will retract proximally, unless there is an intact bicipital aponeurosis. With a retracted tendon, direct repair may be difficult.
Nonoperative treatment is an option, as well as nonanatomic repair if the tendon cannot be brought back to the tuberosity. The indication for surgery is functional impairment due to decreased strength or severe pain. Overall, anatomic repair will be preferred by most orthopedic surgeons as a nonanatomic repair has only been shown to be successful in 60 % of patients [34].
Either a single- or double-incision technique may be used, as described above. Some pitfalls may complicate surgery. First, tendon retraction proximal to the elbow crease may require lengthening of the incision past the crease. This is best done by a lazy-S over the crease or by a separate incision proximal, over the tendon stump. The retracted tendon will be encased in scar tissue and may be of very poor quality. Releasing the tendon from the scar tissue can be challenging. The tendon may be shortened as well as the muscle belly. Prolonged traction on the tendon can mobilize the muscle and tendon sufficiently to repair the tendon back to the tuberosity. Another challenge is tissue obliterating the bicipital tunnel. This increases the risk of injury to the neurovascular bundle in the antecubital fossa and proximal forearm [29]. Care should be taken when dissecting to the tuberosity. The forearm is fully supinated throughout the dissection, but rotation of the forearm may help identify the tuberosity.
Once the tendon and tuberosity have been identified and prepared, an attempt is made to bring the stump back to the bone. We prefer to use the cortical button approach, as was described above. The elbow is hyperflexed and the tendon is pulled into the bone tunnel. Primary repair is often still possible [35]. The tendon can be fixed with the elbow in hyperflexion, and most patients will regain full extension as the tendon and muscle stretch over time [36•].
If it is not possible to bring the tendon back to bone or if the quality of the tendon is insufficient, a graft can be used to reconstruct the tendon. A wide variety of autografts and allografts have been used. Autograft lacertus fibrosis [37], semitendinosus [38, 39], quadriceps tendon [40], and fascia lata [41] have all been described. Allograft Achilles [42, 43], semitendinosus, tibialis anterior [44], and fascia lata [41, 45] have all been used to reconstruct the tendon [44, 46].
Results
Nonoperative treatment clearly yields inferior results to surgical repair [15, 47], with residual pain [47], a loss of about 40 % supination strength, and an average of 30 % decrease in flexion strength [48]. However, some patients may be able to adapt to the decreased strength and can still be satisfied with nonoperative treatment [49, 50].
Anatomic repair is preferred over nonanatomic fixation to the brachialis, with good results in 90 % of patients in the anatomic repair group, compared to only 60 % in the latter [34]. Controversy still exists on which fixation method to choose and whether to use a single- or two-incision technique [51]. Up to now, no device has been proven to have clinical superiority over another, but the cortical button and bone tunnel techniques have shown a decrease in complication rate compared to other techniques [50]. No clear differences have been shown between the button or bone tunnel techniques [52]. In a randomized clinical trial, Grewal et al. found no significant differences in outcome between a single- and double-incision technique. A 10 % increase in supination strength was found in the double-incision technique, and a slight increase in minor complications was found in the single incision technique [53].
In general, patients can expect less than a 5° decrease in extension and flexion and up to 10° loss for forearm rotation [54–56]. Flexion and supination strength will recover to an average of 90 % of the uninjured side [31, 57].
Delayed repair or reconstruction has also been shown to be able to restore flexion strength to up to 90 % and supination strength to almost 80 % of the uninjured side, with better results if the tendon was repaired back to bone, compared to patients where a graft was needed [58].
Complications
The overall complication rate of distal biceps tendon repair is approximately 25 % [50] for all surgical techniques combined. Most complications are minor, with transient lateral antebrachial cutaneous nerve neuropraxia or radial sensory nerve paraesthesia as the most common complications [59•]. Asymptomatic heterotopic ossification is found in over one third of patients following distal biceps repair [60], but this does not significantly affect the functional outcome [54]. There are no significant differences in overall complication rate between the one- and two-incision techniques, but cortical button or bone tunnel fixation has shown a decrease in complication rate compared to other techniques [50].
Unfortunately, possible complications also include posterior interosseous nerve palsy [61], symptomatic heterotopic ossification [59•, 60] (Fig. 12), or radioulnar synostosis [62–64].
Fig. 12.

Postoperative CT scan, showing a significant amount of heterotopic ossification following a cortical button repair of the distal biceps. Although rotation was limited, this did not bother the patient and he declined revision surgery. Reprinted with Permission from MoRe Foundation
Reruptures are rare, with a rerupture rate of about 1–2 % [59•, 62, 64, 65]. A higher rerupture rate of 5 % has been published in patients treated with suture anchor fixation [51].
The timing of surgery has been shown to play a role in the occurrence of complications [50, 59•]. Cain et al. reported a 30 % complication rate in acutely operated injuries compared to 41 % in patients operated 4 weeks or later after the injury. Bisson et al. found a complication rate of 20 % in patients operated between 0 and 2 weeks following the rupture, compared to 40 % if surgery was delayed for more than 2 weeks [62]. Kelly et al. had similar findings with 24 % complications if operated within 10 days and 41 % complications if operated after 21 days [29].
Irrespective of which approach or technique is used, a meticulous technique is imperative to avoid these disastrous complications; removal of bone debris, lavage, and hemostasis may decrease the rate of heterotopic ossification. Careful use of retractors, avoiding blind placement of retractors posterior to the radius, may decrease the rate of posterior interosseous nerve palsy, especially in the single-incision technique.
Conclusion
Distal biceps tendon rupture is an uncommon injury. It occurs mainly in middle-aged men involved in heavy labor or sports. Early surgical repair yields the best results with a decreased risk of complications.
Compliance with ethical standards
Conflict of interest
Melanie Vandenberghe and Roger van Riet declare that they have no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Elbow Soft Tissue Surgery
References
Papers of particular interest, published recently, have been highlighted as: • of importance
- 1.Safran MR, Graham SM. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;404:275–83. [PubMed] [Google Scholar]
- 2.•.Kelly MP, Perkinson SG, Ablove RH, Tueting JL. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med. 2015;43(8):2012–7. doi: 10.1177/0363546515587738. [DOI] [PubMed] [Google Scholar]
- 3.Seiler JG, 3rd, Parker LM, Chamberland PD, Sherbourne GM, Carpenter WA. The distal biceps tendon. Two potential mechanisms involved in its rupture: arterial supply and mechanical impingement. Journal of shoulder and elbow surgery / American Shoulder and Elbow Surgeons [et al]. 1995;4(3):149-56. [DOI] [PubMed]
- 4.Eames MH, Bain GI, Fogg QA, van Riet RP. Distal biceps tendon anatomy: a cadaveric study. J Bone Joint Surg Am. 2007;89(5):1044–9. doi: 10.2106/JBJS.D.02992. [DOI] [PubMed] [Google Scholar]
- 5.Pacha Vicente D, Forcada Calvet P, Carrera Burgaya A, Llusa PM. Innervation of biceps brachii and brachialis: anatomical and surgical approach. Clin Anat. 2005;18(3):186–94. doi: 10.1002/ca.20057. [DOI] [PubMed] [Google Scholar]
- 6.Bernstein AD, Breslow MJ, Jazrawi LM. Distal biceps tendon ruptures: a historical perspective and current concepts. Am J Orthop. 2001;30(3):193–200. [PubMed] [Google Scholar]
- 7.•.Devereaux MW, ElMaraghy AW. Improving the rapid and reliable diagnosis of complete distal biceps tendon rupture: a nuanced approach to the clinical examination. Am J Sports Med. 2013;41(9):1998–2004. doi: 10.1177/0363546513493383. [DOI] [PubMed] [Google Scholar]
- 8.Belli P, Costantini M, Mirk P, Leone A, Pastore G, Marano P. Sonographic diagnosis of distal biceps tendon rupture: a prospective study of 25 cases. J Ultrasound Med. 2001;20(6):587–95. doi: 10.7863/jum.2001.20.6.587. [DOI] [PubMed] [Google Scholar]
- 9.Weiss C, Mittelmeier M, Gruber G. Do we need MR images for diagnosing tendon ruptures of the distal biceps brachii? The value of ultrasonographic imaging. Ultraschall Med. 2000;21(6):284–6. doi: 10.1055/s-2000-9119. [DOI] [PubMed] [Google Scholar]
- 10.Green JB, Skaife TL, Leslie BM. Bilateral distal biceps tendon ruptures. J Hand Surg Am. 2012;37(1):120–3. doi: 10.1016/j.jhsa.2011.09.043. [DOI] [PubMed] [Google Scholar]
- 11.Pagonis T, Givissis P, Ditsios K, Pagonis A, Petsatodis G, Christodoulou A. The effect of steroid-abuse on anatomic reinsertion of ruptured distal biceps brachii tendon. Injury. 2011;42(11):1307–12. doi: 10.1016/j.injury.2011.03.018. [DOI] [PubMed] [Google Scholar]
- 12.Schneider A, Bennett JM, O'Connor DP, Mehlhoff T, Bennett JB. Bilateral ruptures of the distal biceps brachii tendon. J Shoulder Elbow Surg. 2009;18(5):804–7. doi: 10.1016/j.jse.2009.01.029. [DOI] [PubMed] [Google Scholar]
- 13.Visuri T, Lindholm H. Bilateral distal biceps tendon avulsions with use of anabolic steroids. Med Sci Sports Exerc. 1994;26(8):941–4. [PubMed] [Google Scholar]
- 14.Baker BE, Bierwagen D. Rupture of the distal tendon of the biceps brachii. Operative versus non-operative treatment. J Bone Joint Surg Am. 1985;67(3):414–7. [PubMed] [Google Scholar]
- 15.Chillemi C, Marinelli M, De Cupis V. Rupture of the distal biceps brachii tendon: conservative treatment versus anatomic reinsertion--clinical and radiological evaluation after 2 years. Arch Orthop Trauma Surg. 2007;127(8):705–8. doi: 10.1007/s00402-007-0326-7. [DOI] [PubMed] [Google Scholar]
- 16.O'Driscoll SW, Goncalves LB, Dietz P. The hook test for distal biceps tendon avulsion. Am J Sports Med. 2007;35(11):1865–9. doi: 10.1177/0363546507305016. [DOI] [PubMed] [Google Scholar]
- 17.Ruland RT, Dunbar RP, Bowen JD. The biceps squeeze test for diagnosis of distal biceps tendon ruptures. Clin Orthop Relat Res. 2005;437:128–31. doi: 10.1097/01.blo.0000167668.18444.f5. [DOI] [PubMed] [Google Scholar]
- 18.Metzman LS, Tivener KA. The supination-pronation test for distal biceps tendon rupture. Am J Orthop. 2015;44(10):E361–4. [PubMed] [Google Scholar]
- 19.ElMaraghy A, Devereaux M, Tsoi K. The biceps crease interval for diagnosing complete distal biceps tendon ruptures. Clin Orthop Relat Res. 2008;466(9):2255–62. doi: 10.1007/s11999-008-0334-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kayser R, Mahlfeld K, Scheller W, Muller J, Schmidt W, Heyde CE. Sonographic imaging of the distal biceps tendon—an experimental and clinical study. Ultraschall Med. 2005;26(1):17–23. doi: 10.1055/s-2004-813718. [DOI] [PubMed] [Google Scholar]
- 21.Lozano V, Alonso P. Sonographic detection of the distal biceps tendon rupture. J Ultrasound Med. 1995;14(5):389–91. doi: 10.7863/jum.1995.14.5.389. [DOI] [PubMed] [Google Scholar]
- 22.Le Huec JC, Moinard M, Liquois F, Zipoli B, Chauveaux D, Le Rebeller A. Distal rupture of the tendon of biceps brachii. Evaluation by MRI and the results of repair. J Bone Joint Surg Br. 1996;78(5):767–70. [PubMed] [Google Scholar]
- 23.Mayer DP, Schmidt RG, Ruiz S. MRI diagnosis of biceps tendon rupture. Comput Med Imaging Graph. 1992;16(5):345–7. doi: 10.1016/0895-6111(92)90147-2. [DOI] [PubMed] [Google Scholar]
- 24.•.Giuffre BM, Moss MJ. Optimal positioning for MRI of the distal biceps brachii tendon: flexed abducted supinated view. AJR Am J Roentgenol. 2004;182(4):944–6. doi: 10.2214/ajr.182.4.1820944. [DOI] [PubMed] [Google Scholar]
- 25.Frazier MS, Boardman MJ, Westland M, Imbriglia JE. Surgical treatment of partial distal biceps tendon ruptures. J Hand Surg Am. 2010;35(7):1111–4. doi: 10.1016/j.jhsa.2010.04.024. [DOI] [PubMed] [Google Scholar]
- 26.Ozyurekoglu T, Tsai TM. Ruptures of the distal biceps brachii tendon: results of three surgical techniques. Hand Surg. 2003;8(1):65–73. doi: 10.1142/s0218810403001431. [DOI] [PubMed] [Google Scholar]
- 27.Duffiet P, Fontes D. Endoscopic repair of distal biceps brachii tendon avulsion: a new technique. Report of 25 cases. Chirurgie de la main. 2009;28(3):146–52. doi: 10.1016/j.main.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 28.Gregory T, Roure P, Fontes D. Repair of distal biceps tendon rupture using a suture anchor: description of a new endoscopic procedure. Am J Sports Med. 2009;37(3):506–11. doi: 10.1177/0363546508326985. [DOI] [PubMed] [Google Scholar]
- 29.Kelly EW, Morrey BF, O'Driscoll SW. Complications of repair of the distal biceps tendon with the modified two-incision technique. J Bone Joint Surg Am. 2000;82-A(11):1575–81. doi: 10.2106/00004623-200011000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Bain GI, Prem H, Heptinstall RJ, Verhellen R, Paix D. Repair of distal biceps tendon rupture: a new technique using the Endobutton. J Shoulder Elbow Surg. 2000;9(2):120–6. [PubMed] [Google Scholar]
- 31.Peeters T, Ching-Soon NG, Jansen N, Sneyers C, Declercq G, Verstreken F. Functional outcome after repair of distal biceps tendon ruptures using the endobutton technique. J Shoulder Elbow Surg. 2009;18(2):283–7. doi: 10.1016/j.jse.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 32.Mazzocca AD, Burton KJ, Romeo AA, Santangelo S, Adams DA, Arciero RA. Biomechanical evaluation of 4 techniques of distal biceps brachii tendon repair. Am J Sports Med. 2007;35(2):252–8. doi: 10.1177/0363546506294854. [DOI] [PubMed] [Google Scholar]
- 33.Failla JM, Amadio PC, Morrey BF, Beckenbaugh RD. Proximal radioulnar synostosis after repair of distal biceps brachii rupture by the two-incision technique. Report of four cases. Clin Orthop Relat Res. 1990;253:133–6. [PubMed] [Google Scholar]
- 34.Rantanen J, Orava S. Rupture of the distal biceps tendon. A report of 19 patients treated with anatomic reinsertion, and a meta-analysis of 147 cases found in the literature. Am J Sports Med. 1999;27(2):128–32. doi: 10.1177/03635465990270020201. [DOI] [PubMed] [Google Scholar]
- 35.Bosman HA, Fincher M, Saw N, et al. Anatomic direct repair of chronic distal biceps brachii tendon rupture without interposition graft. J Shoulder Elbow Surg. 2012;21(10):1342–7. doi: 10.1016/j.jse.2012.01.012. [DOI] [PubMed] [Google Scholar]
- 36.•.Morrey ME, Abdel MP, Sanchez-Sotelo J, Morrey BF, et al. Primary repair of retracted distal biceps tendon ruptures in extreme flexion. J Shoulder Elbow Surg. 2014;23(5):679–85. doi: 10.1016/j.jse.2013.12.030. [DOI] [PubMed] [Google Scholar]
- 37.Hamer MJ, Caputo AE. Operative treatment of chronic distal biceps tendon ruptures. Sports Med Arthrosc. 2008;16(3):143–7. doi: 10.1097/JSA.0b013e3181824e76. [DOI] [PubMed] [Google Scholar]
- 38.Hallam P, Bain GI. Repair of chronic distal biceps tendon ruptures using autologous hamstring graft and the Endobutton. J Shoulder Elbow Surg. 2004;13(6):648–51. doi: 10.1016/j.jse.2004.01.032. [DOI] [PubMed] [Google Scholar]
- 39.McCarty LP, 3rd, Alpert JM, Bush-Joseph C. Reconstruction of a chronic distal biceps tendon rupture 4 years after initial injury. Am J Orthop. 2008;37(11):579–82. [PubMed] [Google Scholar]
- 40.Blond L, Kaewkongnok B. Reconstruction of delayed diagnoses simultaneous bilateral distal biceps tendon ruptures using semtendinosus and quadriceps tendon autografts. SpringerPlus. 2015;4:117. doi: 10.1186/s40064-015-0897-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morrell NT, Mercer DM, Moneim MS. Late reconstruction of chronic distal biceps tendon ruptures using fascia lata autograft and suture anchor fixation. Tech Hand Up Extrem Surg. 2012;16(3):141–4. doi: 10.1097/BTH.0b013e318258e358. [DOI] [PubMed] [Google Scholar]
- 42.Sanchez-Sotelo J, Morrey BF, Adams RA, O'Driscoll SW. Reconstruction of chronic ruptures of the distal biceps tendon with use of an achilles tendon allograft. J Bone Joint Surg Am. 2002;84-A(6):999–1005. doi: 10.2106/00004623-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 43.Patterson RW, Sharma J, Lawton JN, Evans PJ. Distal biceps tendon reconstruction with tendoachilles allograft: a modification of the endobutton technique utilizing an ACL reconstruction system. J Hand Surg Am. 2009;34(3):545–52. doi: 10.1016/j.jhsa.2008.12.019. [DOI] [PubMed] [Google Scholar]
- 44.Snir N, Hamula M, Wolfson T, Meislin R, Strauss EJ, Jazrawi LM. Clinical outcomes after chronic distal biceps reconstruction with allografts. Am J Sports Med. 2013;41(10):2288–95. doi: 10.1177/0363546513502306. [DOI] [PubMed] [Google Scholar]
- 45.Bayat A, Neumann L, Wallace WA. Late repair of simultaneous bilateral distal biceps brachii tendon avulsion with fascia lata graft. Br J Sports Med. 1999;33(4):281–3. doi: 10.1136/bjsm.33.4.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cross MB, Egidy CC, Wu RH, Osbahr DC, Nam D, Dines JS. Single-incision chronic distal biceps tendon repair with tibialis anterior allograft. Int Orthop. 2014;38(4):791–5. doi: 10.1007/s00264-013-2182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Geaney LE, Brenneman DJ, Cote MP, Arciero RA, Mazzocca AD. Outcomes and practical information for patients choosing nonoperative treatment for distal biceps ruptures. Orthopedics. 2010;33(6):391. doi: 10.3928/01477447-20100429-10. [DOI] [PubMed] [Google Scholar]
- 48.Morrey BF, Askew LJ, An KN, Dobyns JH. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am. 1985;67(3):418–21. [PubMed] [Google Scholar]
- 49.Hetsroni I, Pilz-Burstein R, Nyska M, Back Z, Barchilon V, Mann G. Avulsion of the distal biceps brachii tendon in middle-aged population: is surgical repair advisable? A comparative study of 22 patients treated with either nonoperative management or early anatomical repair. Injury. 2008;39(7):753–60. doi: 10.1016/j.injury.2007.11.287. [DOI] [PubMed] [Google Scholar]
- 50.Watson JN, Moretti VM, Schwindel L, Hutchinson MR. Repair techniques for acute distal biceps tendon ruptures: a systematic review. J Bone Joint Surg Am. 2014;96(24):2086–90. doi: 10.2106/JBJS.M.00481. [DOI] [PubMed] [Google Scholar]
- 51.Citak M, Backhaus M, Seybold D, Suero EM, Schildhauer TA, Roetman B. Surgical repair of the distal biceps brachii tendon: a comparative study of three surgical fixation techniques. Knee Surg Sports Traumatol Arthrosc. 2011;19(11):1936–41. doi: 10.1007/s00167-011-1591-0. [DOI] [PubMed] [Google Scholar]
- 52.Recordon JA, Misur PN, Isaksson F, Poon PC. Endobutton versus transosseous suture repair of distal biceps rupture using the two-incision technique: a comparison series. J Shoulder Elbow Surg. 2015;24(6):928–33. doi: 10.1016/j.jse.2014.12.032. [DOI] [PubMed] [Google Scholar]
- 53.Grewal R, Athwal GS, MacDermid JC, Faber KJ, Drosdowech DS, El-Hawary R, et al. Single versus double-incision technique for the repair of acute distal biceps tendon ruptures: a randomized clinical trial. J Bone Joint Surg Am. 2012;94(13):1166–74. doi: 10.2106/JBJS.K.00436. [DOI] [PubMed] [Google Scholar]
- 54.Siebenlist S, Fischer SC, Sandmann GH, Ahrens P, Wolf P, Stockle U, et al. The functional outcome of forty-nine single-incision suture anchor repairs for distal biceps tendon ruptures at the elbow. Int Orthop. 2014;38(4):873–9. doi: 10.1007/s00264-013-2200-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McKee MD, Hirji R, Schemitsch EH, Wild LM, Waddell JP. Patient-oriented functional outcome after repair of distal biceps tendon ruptures using a single-incision technique. J Shoulder Elbow Surg. 2005;14(3):302–6. doi: 10.1016/j.jse.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 56.Khan AD, Penna S, Yin Q, Sinopidis C, Brownson P, Frostick SP. Repair of distal biceps tendon ruptures using suture anchors through a single anterior incision. Arthroscopy. 2008;24(1):39–45. doi: 10.1016/j.arthro.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 57.Cil A, Merten S, Steinmann SP. Immediate active range of motion after modified 2-incision repair in acute distal biceps tendon rupture. Am J Sports Med. 2009;37(1):130–5. doi: 10.1177/0363546508323749. [DOI] [PubMed] [Google Scholar]
- 58.Ryhanen J, Kaarela O, Siira P, Kujala S, Raatikainen T. Recovery of muscle strength after late repair of distal biceps brachii tendon. Scand J Surg. 2006;95(1):68–72. doi: 10.1177/145749690609500113. [DOI] [PubMed] [Google Scholar]
- 59.•.Cain RA, Nydick JA, Stein MI, Williams BD, Polikandriotis JA, Hess AV. Complications following distal biceps repair. J Hand Surg Am. 2012;37(10):2112–7. doi: 10.1016/j.jhsa.2012.06.022. [DOI] [PubMed] [Google Scholar]
- 60.Gallinet D, Dietsch E, Barbier-Brion B, Lerais JM, Obert L. Suture anchor reinsertion of distal biceps rupture: clinical results and radiological assessment of tendon healing. Orthop Traumatol Surg Res. 2011;97(3):252–9. doi: 10.1016/j.otsr.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 61.Van den Bogaerde J, Shin E. Posterior interosseous nerve incarceration with endobutton repair of distal biceps. Orthopedics. 2015;38(1):e68–71. doi: 10.3928/01477447-20150105-92. [DOI] [PubMed] [Google Scholar]
- 62.Bisson L, Moyer M, Lanighan K, Marzo J. Complications associated with repair of a distal biceps rupture using the modified two-incision technique. J Shoulder Elbow Surg. 2008;17(1 Suppl):67S–71. doi: 10.1016/j.jse.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 63.Karunakar MA, Cha P, Stern PJ. Distal biceps ruptures. A followup of Boyd and Anderson repair. Clin Orthop Relat Res. 1999;363:100–7. [PubMed] [Google Scholar]
- 64.Hinchey JW, Aronowitz JG, Sanchez-Sotelo J, Morrey BF. Re-rupture rate of primarily repaired distal biceps tendon injuries. J Shoulder Elbow Surg. 2014;23(6):850–4. doi: 10.1016/j.jse.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 65.Cusick MC, Cottrell BJ, Cain RA, Mighell MA. Low incidence of tendon rerupture after distal biceps repair by cortical button and interference screw. J Shoulder Elbow Surg. 2014;23(10):1532–6. doi: 10.1016/j.jse.2014.04.013. [DOI] [PubMed] [Google Scholar]


