Abstract
Successful management of complex elbow fracture-dislocations requires, in part, recognition of the overall injury pattern, which can aid in the identification of concomitant bony and soft tissue injuries. Trans-olecranon fracture-dislocations are best treated surgically with stable anatomic restoration of the trochlear notch. Terrible triad elbow injuries are believed to be caused by a valgus posterolateral force. Although select terrible triad injuries can be managed non-operatively, the majority of injuries are treated with stable surgical repair to allow early elbow motion. Unlike terrible triads, varus posteromedial forces are theorized to cause anteromedial coronoid fractures. These are usually associated with LCL disruptions, but do not have concomitant MCL or radial head injuries. A subset of anteromedial coronoid fractures can also be managed non-operatively. Internal fixation is recommended for injuries associated with large fracture fragments or elbow instability preventing early motion.
Keywords: Trans-olecranon, Terrible triad, Anteromedial coronoid, Elbow instability, Fracture-dislocation
Introduction
The elbow is the second most commonly dislocated joint of the upper extremity, and more than one quarter of dislocations are associated with elbow fractures [1]. The majority of elbow dislocations without fractures occur in patients under the age of 30 [2] and are managed non-surgically with good clinical outcomes. Complex elbow fracture-dislocations are a much more difficult problem to manage with the potential for significant long-term morbidity. Inappropriate treatment can lead to persistent instability, post-traumatic arthritis, stiffness, and pain. There are several well-recognized fracture-dislocation injury patterns, and an understanding of these is helpful to predict associated injuries and to guide treatment strategies. This article will review the three common patterns of complex elbow fracture-dislocations and their management: the trans-olecranon fracture-dislocation, the terrible triad injury, and anteromedial coronoid fractures associated with varus posteromedial instability.
Initial evaluation
A complete history and physical examination is required for all patients presenting with complex elbow fracture-dislocations. The mechanism of injury should be clarified to gain insight into the injury forces and energy. This may help predict the pattern of elbow trauma and guide treatment decisions. Physical examination should include a careful and systematic palpation for areas of tenderness, including the collateral ligaments, radial head, and the medial and lateral epicondyles. It should also focus on ruling out open fractures, neurovascular compromise, and associated injuries, including ipsilateral shoulder or wrist fractures.
Plain radiographs are usually diagnostic of complex elbow fracture-dislocations. A closed reduction should be performed if the joint is dislocated or the limb is grossly deformed. A CT scan including three-dimensional reconstructions is recommended for the assessment of the fractures and to guide preoperative planning and treatment.
Defining elbow instability can be difficult in the acute setting, particularly under fluoroscopic stress testing. Pain, apprehension, and inconsistent loading by the treating physician may contribute to variable results. Furthermore, even normal elbows without trauma can display slight medial ulnohumeral joint gapping under valgus stress [3]. In complex elbow fracture-dislocations, criteria for identifying appropriate patients for early surgical fixation are not universally accepted. The literature contains limited data to help guide treatment decisions. In one study, Rhyou et al. [4] showed that good outcomes were obtained in 18 patients with anteromedial coronoid fractures when using the results of a varus fluoroscopic stress test to determine whether lateral collateral ligament (LCL) repair was necessary. In our opinion, given adequate muscle relaxation and pain relief, it is likely that most patients will have instability under stress fluoroscopy after elbow fracture-dislocations, but carefully selected patients will not experience subjective instability that interferes with function after appropriate rehabilitation. Further studies are needed to better define the clinical role and value of fluoroscopic stress tests.
Trans-olecranon fracture-dislocations
Trans-olecranon fracture-dislocations result from an axial loading injury. They are characterized by the disruption of the ulnohumeral joint and anterior displacement of the radial head relative to the capitellum. A complex, comminuted fracture of the proximal ulna is usually present although simple and oblique fractures can occur [5]. Basal coronoid fractures are also common and typically involve more than 50 % of the coronoid height [6]. Radial head fractures can occur concomitantly as well [5, 7, 8]. The collateral ligaments are usually spared [1, 5].
These injuries should not be confused with posterior olecranon fracture-dislocations, which are more similar in treatment to a proximally based Monteggia Bado type 2 lesion [6]. Additionally, trans-olecranon fracture-dislocations need to be differentiated from Monteggia Bado type 1 injuries. In a trans-olecranon fracture dislocation, the proximal radioulnar joint remains intact, whereas Monteggia lesions are characterized by the disruption of the proximal radioulnar joint. In addition, the trans-olecranon fracture-dislocations have a complex disruption of the ulnohumeral joint [5]. This distinction has important treatment implications. In Monteggia injuries, the focus of surgical reduction is anatomic alignment of the ulnar diaphyseal fracture; whereas in trans-olecranon fracture-dislocations, the goal is stable restoration of the greater sigmoid notch [9].
A posterior midline skin incision is utilized for exposure [6]. The insertion of the triceps should be preserved [1]. Different techniques are available to obtain stable surgical fixation of the greater sigmoid notch, including tension-band wiring or plate osteosynthesis. Available literature suggests a higher failure rate with tension-band wiring [7, 8], but if chosen, this technique should be reserved for simple, non-comminuted transverse or short oblique fractures of the olecranon [1, 5]. In most cases, stable fixation can be achieved with a posterior plate. Fracture extension into the metaphyseal region may require an additional medial and/or lateral plate. Studies have shown that both reconstruction and limited-contact dynamic compression plates yield satisfactory results [7, 8]. Pre-contoured proximal ulna plates are now available which can simplify the procedure. Associated fractures of the coronoid or radial head can usually be addressed through the exposure afforded by the olecranon fracture [6]. In some cases, additional medial and/or lateral approaches are needed and are easily accessed by raising skin flaps from the posterior incision [6].
Terrible triad
A terrible triad injury of the elbow consists of an ulnohumeral dislocation with associated fractures of the coronoid and radial head. This injury has been postulated to occur during a fall on an outstretched arm, causing a valgus posterolateral force to the elbow [10] that results in a sequential lateral to medial disruption of the surrounding capsuloligamentous structures [10]. Associated coronoid fractures are usually type 1 or tip fractures according to the O’Driscoll classification [11]. On average, they involve 35 % of the coronoid height or 7 mm [12]. Radial head fractures typically involve the anterolateral quadrant [13]. The loss of cortical contact of at least one radial head fracture fragment is highly predictive of a complex elbow injury pattern [14].
Ring et al. [15] have previously reported that terrible triad injuries are usually unstable and are prone to complications, including instability, arthritis, and stiffness. While many of these injuries are treated surgically, certain selected patients can be considered for non-operative treatment. In a retrospective study, 12 patients with terrible triads were managed with a non-operative treatment protocol [16•]. After a mean follow-up of 36 months, patients had good functional outcomes with an average range of motion of 134° flexion, 6° extension, 87° pronation, and 82° supination [16•]. Complications included one patient who required surgery for early recurrent instability and another who underwent arthroscopic debridement for heterotopic bone [16•]. Non-operative treatment can be considered if several specific criteria are met including the following: (1) a concentric joint reduction, (2) a radial head fracture that does not cause a mechanical block to rotation, (3) a smaller coronoid fracture (Regan-Morrey type 1 or 2), and (4) a stable arc of motion to a minimum of 30° of extension to allow active motion within the first 10 days [16•].
Failure to meet all criteria for non-operative management necessitates surgical fixation. McKee et al. [17] evaluated a standard surgical algorithm for terrible triad injuries and found that, at an average follow-up of 34 months, the 36 patients had a mean flexion-extension arc of 112° and forearm rotation of 136°. The mean MEPI score was 88, which translated into 15 excellent, 13 good, 7 fair, and 1 poor result [17]. Principles of surgical fixation include restoring stability from deep to superficial and lateral to medial [10, 17]. The operative technique that they recommended includes the following: (1) address the coronoid through internal fixation or anterior capsular repair for smaller avulsion-type fractures; (2) replace or fix the radial head fracture; (3) restore lateral elbow stability with a LCL repair; and (4) repair the MCL and/or apply a hinged external fixator for residual elbow instability [10, 17].
The decision to replace or repair associated radial head fractures is dependent on the extent of comminution, number of fragments, and surgeon experience. Attempts at internal fixation for radial head fractures with more than three articular fragments have been associated with unsatisfactory results [18]. Using this as one indication for radial head arthroplasty, Watters et al. [19] found no difference in functional outcomes or elbow motion compared to internal fixation after a mean follow-up of 24 months. Interestingly, the authors reported three elbows with persistent instability in the internal fixation group compared to no cases in the arthroplasty group [19]. They suggested that the improved visualization of the coronoid during radial head excision and replacement led to more accurate internal fixation. It may also result in less soft tissue stripping and subsequently less instability after radial head arthroplasty [19]. In another study, Leigh and Ball [20] demonstrated no difference in outcomes between radial head arthroplasty and internal fixation in a retrospective, non-randomized study. They concluded that the radial head could be either fixed or replaced, although they preferred radial head fracture fixation in younger patients [20].
There has been some data to suggest that certain coronoid fractures can be left without internal fixation in terrible triad injuries. In a cadaveric study, Jeon et al. [21] demonstrated that Regan-Morrey type 2 coronoid fractures were unstable to valgus and external rotation moments only when the radial head was removed. In contrast, type 3 coronoid fractures were unstable, even with intact collateral ligaments and radial head [21]. Papatheodorou et al. [22] evaluated the clinical outcomes in patients with terrible triad injuries and Regan-Morrey types 1 and 2 coronoid fractures. In their series, all patients underwent either radial head fixation or arthroplasty and a LCL repair. An intraoperative fluoroscopic check for elbow stability was done to ensure a concentric ulnohumeral reduction within 20° to 130° of flexion. None of the patients received fixation of the coronoid fracture, required MCL repair, or had an external fixator applied for residual stability. At an average follow-up of 41 months, Papatheodorou et al. [22] reported good outcomes with no cases of late instability.
Anteromedial coronoid fractures
The anteromedial coronoid may be prone to injury because approximately 58 % is unsupported by the proximal ulna [23]. Fractures of the anteromedial coronoid are theorized to occur from a varus posteromedial rotatory injury force [24]. These are distinct elbow injuries associated with the disruption of the LCL and typically the preservation of the radial head and MCL [25]. Recognition of anteromedial coronoid fractures led to the O’Driscoll classification of coronoid fractures [6], which takes into account both the size and location of the injury (Fig. 1). In this system, anteromedial coronoid fractures are categorized as type 2 and further subdivided into subtype 1 (rim), subtype 2 (rim and tip), and subtype 3 (rim and sublime tubercle) [6].
Fig. 1.
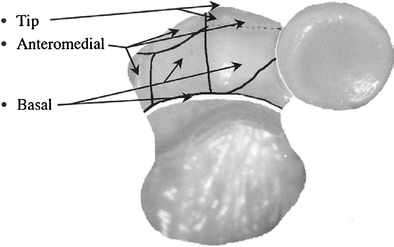
O’Driscoll classification of coronoid fractures, including type 1 (tip), type 2 (anteromedial), and type 3 (basal) (reprinted with permission from reference [6]
Identification of the fracture requires a high index of suspicion because the injury pattern can be subtle and the elbow joint is usually not grossly unstable [1]. Plain radiographic features may include an asymmetric ulnohumeral joint space on an anteroposterior view, with narrowing of the medial ulnotrochlear facet [24]. Depending on the degree of fracture displacement, a lateral view may demonstrate a “double crescent sign,” representing a depressed anteromedial coronoid fragment and loss of congruency with the medial aspect of the distal humeral articular surface [24]. In our opinion, all patients should undergo CT scans with three-dimensional reconstruction images for further fracture characterization and treatment planning.
When properly selected, a subset of anteromedial coronoid fractures can be managed non-operatively. In an unpublished study, we evaluated 10 patients (9 anteromedial coronoid subtype 2 and 1 subtype 3) who were successfully treated non-surgically after a mean follow-up of 50 months (range 12–83 months). We found that the following criteria could be used to consider patients for non-operative treatment: (1) minimally displaced or undisplaced smaller subtype 2 fractures, especially those ≤5 mm, (2) a concentric elbow joint, and (3) a stable range of motion to a minimum of 30° of extension. There were no subtype 1 fractures in our study, but Pollock et al. [26] have shown that these fractures may be treated non-operatively if the fragment size remains small (<5 mm) and the MCL is intact. Caution is advised when managing subtype 3 fractures, even though we successfully treated one patient with a minimally displaced subtype 3 fracture, similar to a small series by Moon et al. [27]. Surgical fixation is recommended for the majority of patients with this injury since the elbow joint lacks stability from the lateral collateral ligament and the loss of the medial buttressing effect of an intact coronoid. When patients elect for non-operative treatment, weekly radiographic and clinical follow-up is critical to ensure that the fracture remains undisplaced. In all instances, when considering patients for non-operative treatment, it is important to ensure that they are compliant with rehabilitation and able to return for close follow-up in order to monitor for complications, such as instability.
The relationship between anteromedial coronoid fracture fragment size and the elbow stability is unresolved. In the same unpublished study, our series of non-operatively treated patients with anteromedial coronoid subtype 2 fractures had a mean fragment size of 5 ± 1 mm (range 2–7 mm). In contrast, a biomechanical study by Pollock et al. [26] concluded that internal fixation should be considered for subtype 2 fractures >2.5 mm. Differences in these results may be explained by sufficient stability conferred by remaining soft tissue restraints in vivo, including muscles acting across the joint and the intact MCL, to allow rehabilitation while the fracture and lateral ligaments heal. Further studies are needed to clarify the threshold fragment size.
Variable surgical treatment algorithms have been presented in the literature. Rhyou et al. [4] used the fracture fragment size and the results of a varus fluoroscopic stress examination to determine the appropriate treatment. If the fracture was ≥6 mm, a medial elbow approach was used and internal fixation was achieved with cannulated screws, tension band, or buttress plate. Additionally, LUCL repair was undertaken if there was either a lack of a firm end point or asymmetry of the medial ulnohumeral joint space during varus fluoroscopic stress testing. After an average follow-up of 37 months, Rhyou et al. [4] reported a mean Mayo Elbow Performance Index (MEPI) score of 98. In another study, Park et al. [28•] treated anteromedial coronoid subtype 1 fractures with LCL repair alone, and subtypes 2 and 3 fractures with a buttress plate. At a mean follow-up of 31 months, the average MEPI score was 89, mean flexion of 134°, and mean extension of 6° [28•].
Conclusions
Complex traumatic elbow instability can be a difficult problem to treat for orthopedic surgeons. Understanding the injury pattern helps to predict associated injuries, which ultimately guide definitive management. Although studies will continue to challenge and complement current beliefs, the basic treatment goal remains the same: to obtain a stable pain-free elbow within a functional arc of motion.
Compliance with ethical standards
Conflict of interest
Kevin Chan and Kenneth J. Faber declare that they have no conflict of interest.
Graham J.W. King reports personal fees from Wright Medical Technology and Tornier Incorporated, out the submitted work. In addition, Dr. King has a patent Wright Medical Technology with royalties paid, and a patent Tornier Incorporated with royalties paid.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Elbow Soft Tissue Surgery
Contributor Information
Kevin Chan, Email: chank85@gmail.com.
Graham J. W. King, Phone: +519-646-6011, Email: gking@uwo.ca
Kenneth J. Faber, Phone: +519-646-6312, Email: kjfaber@uwo.ca
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Wyrick JD, Dailey SK, Gunzenhaeuser JM, Casstevens EC. Management of complex elbow dislocations: a mechanistic approach. J Am Acad Orthop Surg. 2015;23(5):297–306. doi: 10.5435/JAAOS-D-14-00023. [DOI] [PubMed] [Google Scholar]
- 2.Stoneback JW, Owens BD, Sykes J, Athwal GS, Pointer L, Wolf JM. Incidence of elbow dislocations in the United States population. J Bone Joint Surg Am. 2012;94(3):240–5. doi: 10.2106/JBJS.J.01663. [DOI] [PubMed] [Google Scholar]
- 3.Lee GA, Katz SD, Lazarus MD. Elbow valgus stress radiography in an uninjured population. Am J Sports Med. 1998;26(3):425–7. doi: 10.1177/03635465980260031401. [DOI] [PubMed] [Google Scholar]
- 4.Rhyou IH, Kim KC, Lee JH, Kim SY, et al. Strategic approach to O’Driscoll type 2 anteromedial coronoid facet fracture. J Shoulder Elb Surg. 2014;23(7):924–32. doi: 10.1016/j.jse.2014.02.016. [DOI] [PubMed] [Google Scholar]
- 5.Ring D, Jupiter JB, Sanders RW, Mast J, Simpson NS. Transolecranon fracture-dislocation of the elbow. J Orthop Trauma. 1997;11(8):545–50. doi: 10.1097/00005131-199711000-00001. [DOI] [PubMed] [Google Scholar]
- 6.O’Driscoll SW, Jupiter JB, Cohen MS, Ring D, McKee MD. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–34. [PubMed] [Google Scholar]
- 7.Mortazavi SM, Asadollahi S, Tahririan MA. Functional outcome following treatment of transolecranon fracture-dislocation of the elbow. Injury. 2006;37(3):284–8. doi: 10.1016/j.injury.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 8.Mouhsine E, Akiki A, Castagna A, Cikes A, Wettstein M, Borens O, et al. Transolecranon anterior fracture dislocation. J Shoulder Elb Surg. 2007;16(3):352–7. doi: 10.1016/j.jse.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Doornberg J, Ring D, Jupiter JB. Effective treatment of fracture-dislocations of the olecranon requires a stable trochlear notch. Clin Orthop Relat Res. 2004;429:292–300. doi: 10.1097/01.blo.0000142627.28396.cb. [DOI] [PubMed] [Google Scholar]
- 10.Mathew PK, Athwal GS, King GJ. Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg. 2009;17(3):137–51. doi: 10.5435/00124635-200903000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Mellema JJ, Doornberg JN, Dyer GS, Ring D. Distribution of coronoid fracture lines by specific patterns of traumatic elbow instability. J Hand Surg. 2014;39(10):2041–6. doi: 10.1016/j.jhsa.2014.06.123. [DOI] [PubMed] [Google Scholar]
- 12.Doornberg JN, van Duijn J, Ring D. Coronoid fracture height in terrible-triad injuries. J Hand Surg. 2006;31(5):794–7. doi: 10.1016/j.jhsa.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Van Leeuwen DH, Guitton TG, Lambers K, Ring D, et al. Quantitative measurement of radial head fracture location. J Shoulder Elb Surg. 2012;21(8):1013–7. doi: 10.1016/j.jse.2011.08.056. [DOI] [PubMed] [Google Scholar]
- 14.Rineer CA, Guitton TG, Ring D, et al. Radial head fractures: loss of cortical contact is associated with concomitant fracture or dislocation. J Shoulder Elb Surg. 2010;19(1):21–5. doi: 10.1016/j.jse.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 15.Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84(4):547–51. doi: 10.2106/00004623-200204000-00006. [DOI] [PubMed] [Google Scholar]
- 16.•.Chan K, MacDermid JC, Faber KJ, King GJ, Athwal GS. Can we treat select terrible triad injuries nonoperatively? Clin Orthop Relat Res. 2014;472(7):2092–9. doi: 10.1007/s11999-014-3518-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKee MD, Pugh DM, Wild LM, Schemitsch EH, King GJ. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. Surgical technique. J Bone Joint Surg Am. 2005;87(1):22–32. doi: 10.2106/JBJS.D.02933. [DOI] [PubMed] [Google Scholar]
- 18.Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am. 2002;84(10):1811–5. doi: 10.2106/00004623-200210000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Watters TS, Garrigues GE, Ring D, Ruch DS. Fixation versus replacement of radial head in terrible triad: is there a difference in elbow stability and prognosis? Clin Orthop Relat Res. 2014;472(7):2128–35. doi: 10.1007/s11999-013-3331-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Leigh WB, Ball CM, et al. Radial head reconstruction versus replacement in the treatment of terrible triad injuries of the elbow. J Shoulder Elb Surg. 2012;21(10):1336–41. doi: 10.1016/j.jse.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 21.Jeon IH, Sanchez-Sotelo J, Zhao K, An KN, Morrey BM. The contribution of the coronoid and radial head to the stability of the elbow. J Bone Joint Surg. 2012;94(1):86–92. doi: 10.1302/0301-620X.94B1.26530. [DOI] [PubMed] [Google Scholar]
- 22.Papatheodorou LK, Rubright JH, Heim KA, Weiser RW, Sotereanos DG. Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res. 2014;472(7):2084–91. doi: 10.1007/s11999-014-3471-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doornberg JN, De Jong IM, Lindenhovius AL, Ring D, et al. The anteromedial facet of the coronoid process of the ulna. J Shoulder Elb Surg. 2007;16(5):667–70. doi: 10.1016/j.jse.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 24.Sanchez-Sotelo J, O’Driscoll SW, Morrey BF, et al. Medial oblique compression fracture of the coronoid process of the ulna. J Shoulder Elb Surg. 2005;14(1):60–4. doi: 10.1016/j.jse.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 25.Doornberg JN, Ring DC. Fracture of the anteromedial facet of the coronoid process. J Bone Joint Surg Am. 2006;88(10):2216–24. doi: 10.2106/JBJS.E.01127. [DOI] [PubMed] [Google Scholar]
- 26.Pollock JW, Brownhill J, Ferreira L, McDonald CP, Johnson J, King G. The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J Bone Joint Surg Am. 2009;91(6):1448–58. doi: 10.2106/JBJS.H.00222. [DOI] [PubMed] [Google Scholar]
- 27.Moon JG, Bither N, Jeon YJ, Oh SM. Non surgically managed anteromedial coronoid fractures in posteromedial rotatory instability: three cases with 2 years follow-up. Arch Orthop Trauma Surg. 2013;133(12):1665–8. doi: 10.1007/s00402-013-1846-y. [DOI] [PubMed] [Google Scholar]
- 28.•.Park SM, Lee JS, Jung JY, Kim JY, Song KS, et al. How should anteromedial coronoid facet fracture be managed? A surgical strategy based on O’Driscoll classification and ligament injury. J Shoulder Elb Surg. 2015;24(1):74–82. doi: 10.1016/j.jse.2014.07.010. [DOI] [PubMed] [Google Scholar]


