Abstract
Despite abundant biological, biomechanical, and clinical research, return to sport after anterior cruciate ligament (ACL) injury remains a significant challenge. Residual rotatory knee laxity has been identified as one of the factors responsible for poor functional outcome. To improve and standardize the assessment of knee instability, a variety of instability scoring systems is available. Recently, devices to objectively quantify static and dynamic clinical exams have been developed to complement traditional subjective grading systems. These devices enable an improved evaluation of knee instability and possible associated injuries. This additional information may promote the development of new treatment algorithms and allow for individualized treatment. In this review, the different subjective laxity scores as well as complementary objective measuring systems are discussed, along with an introduction of injury to an individualized treatment algorithm.
Keywords: Anterior cruciate ligament, ACL, Quantitative pivot shift test, Laxity scores, Treatment algorithm
Introduction
Anterior cruciate ligament (ACL) reconstruction surgery has evolved significantly over the last few decades. The continued development of novel research experiments across this period has better characterized the biological, biomechanical, and clinical aspects of ACL injury. In turn, this had led to improved understanding of anatomy, introduction of sophisticated imaging modalities, advancements in surgical techniques, and the use of evidence-based return to sport criteria. Despite these efforts, return to play at pre-injury level is reported to be around 50 % [1]. One of the factors, which is held responsible for the poor functional outcome after reconstructive surgery, is residual rotatory knee instability.
A thorough assessment of knee laxity has a paramount role during ACL injury management. During early evaluation of suspected injury, the objective quantification of specific motion (i.e., lateral compartment translation) is critical in order to determine the level of instability and the treatment algorithm. Intraoperatively, it is important to objectively evaluate for restoration of stability achieved during the surgery and to identify the need to perform a secondary restraint procedure. Lastly, it is important to evaluate stability throughout the post-operative period in order to verify the healing process and rehabilitation course.
Assessment of knee laxity in the injured and uninjured states has been a topic of interest lately, as there is significant inter-observer variation in laxity assessment [2]. This interest has led to development of tools, which can provide repeatable and objective quantification. Improvement in the objective assessment of knee laxity provides clinicians with better insight into the injury profile and can help to specifically shape treatment protocols. This review will focus on the role of scoring laxity in management of the patients with ACL injury, and the use of an individualized treatment algorithm based on objective knee data.
Clinical assessment of knee laxity
In the 1960s, ACL injury was diagnosed by the anterior drawer of the tibia at 90° of knee flexion. Introduction of the Lachman test by Torg et al. [3] and pivot shift test by Galway et al. [4] during the 1970s significantly improved the accuracy of the physical exam in diagnosis of the ACL injury. The Lachman test was determined to be the most sensitive physical exam in diagnosis of ACL injury, while the pivot shift test is the most specific examination, especially when performed under general anesthesia [5].
One of the earliest grading systems of the pivot shift test was based on eliciting the abnormal reduction movement on varying positions of rotation of the tibia (e.g., internal rotation, neutral, and external rotation) with higher grades with abnormal motion during external rotation [6]. However, the weakness of the pivot shift test is its variability and subjective grading. In order to reduce the variability of pivot shift test maneuver between examiners, a standardized technique and mechanized devices have been developed [7, 8].
Subjective scoring of physical exam is traditionally the main component of clinical evaluation for knee ligamentous injuries. According to the International Knee Documentation Committee (IKDC) evaluation form, the anterior drawer test, Lachman test, and pivot shift test are subjectively graded as normal, nearly normal, abnormal, and severely abnormal [9]. Although IKDC is generally accepted as standard for reporting the status of the knee, the subjective nature of the grading system and the potential lack of repeatability are significant limitations. Historically due to inability of traditional methods to completely restore joint stability, the “nearly normal” (IKDC “B”) was considered acceptable outcome for patients after reconstruction surgery. With recent improvement in the field of ACL reconstruction technique, however, the value of subjective grading system is further called into question in favor of clinically applicable objective measurement devices [10].
Since the 1970s, several devices have been developed to quantify the anterior translation of the tibia during these examinations. The KT1000 (MEDmetric Corp, San Diego, CA, USA) can quantify the amount of load applied and the resultant anterior translation and is the most accepted device for measurement of anterior translation [11]. To date, this device has been applied extensively in management of patient with ACL injury.
Instrumented assessment of rotatory knee instability
To eliminate the aforementioned subjective grading, attempts have been made to develop devices to objectively quantify the pivot shift test [12]. Computer-assisted surgical navigation systems and electromagnetic tracking devices are among the technologies that can provide kinematic data during the pivot shift test [13, 14]. These technologies provide accurate kinematic data, but limitations exist such as invasiveness, bulkiness, and cost. In recent years, non-invasive technologies have been developed that can help clinicians to objectively quantify the pivot shift test. These technologies measure different aspects of bony motion during the pivot shift. Lateral compartment translation can be calculated by image analysis technology [15•, 16].
Image analysis technology
While performing the pivot shift, anterior tibial translation in lateral compartment of the knee is more than that of the medial compartment. This translation correlates with the subjective grading of the pivot shift [13]. Based on this finding, a software has been developed that uses a computer tablet’s camera to record the motion of markers attached to the lateral aspect of the knee during the pivot shift maneuver (Fig. 1). The skin markers are attached to three bony landmarks on lateral side of the knee, i.e., lateral epicondyle, Gerdy’s tubercle, and the fibular head. The software is able to calculate the relative motion of tibia in relation to femur by recording and analyzing the video of the knee motion during pivot shift test [17]. The lateral compartment translation measured by this technique has shown to be strongly correlated with bony motion measured invasively by electromagnetic tracking system [18]. In distances less than or equal to 175 cm between iPad and marker position, this calculation has less than 6 % error, which provides sufficient accuracy for the clinical set-up. Considering the analysis time of 10–15 s, image analysis constitutes an easily applicable tool for the daily clinical work [15•].
Fig. 1.
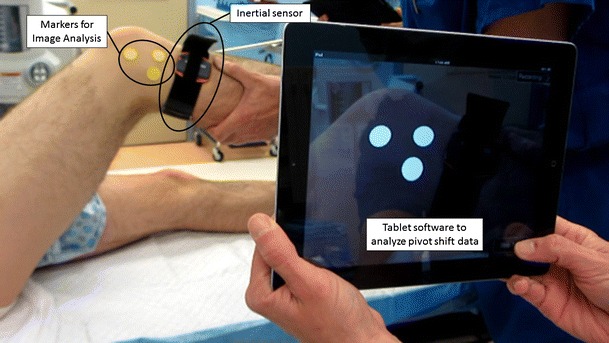
Testing set-up for the quantitative pivot shift measurement. For image analysis, technology markers are attached to the bony landmarks fibular head, Gerdy’s tubercle, and femoral epicondyle to quantify lateral compartment translation. Inertial sensors are attached to the shin using a Velcro strap. Both systems use tablet-software to wirelessly acquire and analysis the data
Inertial sensor technology
The acceleration during the tibial reduction of the pivot shift is significantly higher in ACL-deficient knees and correlates with the clinical grading of the pivot shift [14]. Different types of inertial sensors (accelerometers, gyroscopes, micro-electromechanical system sensors) have been used to quantify this acceleration, rotation, and velocity of the bony motion [19–21]. Similar to the principle of image analysis, the sensors are attached to the lateral aspect of the proximal tibia, close to Gerdy’s tubercle. Transmitting the gathered acceleration via Bluetooth to a tablet software, named Kira (Orthokey LLC, Lewes, DE, USA), the data is subsequently analyzed, plotted, and saved in a patient data base [22, 23•]. The applicability and reliability of this technology were demonstrated in laboratory setting as well as in the clinical use [24, 25]. Together, these devices provide comprehensive insight to joint rotatory laxity (Fig. 1).
Individualized ACL treatment
The concept of “envelope of motion” was described through a series of studies assessing six degrees of freedom of motion by electromagnetic tracking systems. It has been demonstrated that following ACL injury, distinctly different coupled motions occur in response to loads applied during the pivot shift test [26]. Therefore, there is variability in ACL injuries and a single standard treatment approach is unlikely to properly address each individual’s injury. Consequently, it is proposed that each patient should be assessed with a series of subjective and quantitative knee laxity assessment tests. This information together with arthroscopic examination helps in providing individualized treatment to the ACL injured patients. Management can range from single-bundle augmentation to isolated anatomic ACL reconstruction along with secondary procedures such as meniscal repair/reconstruction, extra-articular tenodesis, or high tibial osteotomy in revision surgery.
Some ACL injured patients can be treated non-operatively with rehabilitation. These patients are referred to as “copers” and have been demonstrated to have comparable long-term functional outcome scores and radiographic evidence of osteoarthritis to patients undergoing ACL reconstruction surgery [27]. Recent evidence has demonstrated that the pivot shift test might have potential to further complement the criteria currently used to preemptively identify “copers.” A recent meta-analysis of studies that reported long-term results demonstrated no statistically difference in positive pivot shift results among patients who underwent reconstruction surgery with those that were managed non-operatively [27]. In a recent randomized clinical trial of young active adults with acute ACL injury, patients undergoing early reconstruction surgery did not demonstrate superior outcomes compared to patients undergoing rehabilitation plus delayed optional reconstruction surgery [28]. However, cost-effective analysis studies failed to show reduced costs for non-operative treatments compared to ACL reconstruction surgery, which highlights the need for careful screening of the potential copers [29].
Anatomic ACL reconstruction surgery
The posterolateral (PL) bundle of the ACL has been shown to have a more prominent role in controlling rotational laxity, especially in lower flexion angles [30–32]. The concept of anatomic ACL reconstruction aims at restoring the native anatomy of the ACL by either single- or double-bundle ACL reconstruction, depending on individual variation of anatomy and injury pattern [33, 34]. Using an electromagnetic tracking device, it was demonstrated that patients with partial ACL injury show lower rotational laxity in both antero-posterior motion and during the pivot shift test [35]. If there are undamaged functional ACL fibers, the knee will show less laxity due to stability provided by remaining fibers during the quantitative evaluation of laxity [36]. Therefore, technologies providing pre-operative laxity information can help clinicians to decide whether the ACL remnants observed during surgery have any contribution to joint stability and can potentially be preserved. Further evidence regarding the long-term benefits of augmentation reconstruction surgeries needs to be generated in future studies [37].
If complete ACL reconstruction surgery is indicated, restoration of the native ACL footprint size is essential for anatomical reconstruction surgery. It has been demonstrated that there is large variation in size of ACL insertion site among patients; therefore, the same graft size or reconstruction technique cannot restore the native insertion side in all patients [38]. Recent studies highlighted the increased risk of reconstruction failure with smaller grafts [39] and demonstrate that single-bundle reconstruction surgery restores only 70–79 % of the native ACL insertion side [40]. Several biomechanical studies [41–43] as well as randomized clinical trials [44] reported higher antero-posterior and rotational stability in double-bundle reconstructions surgery compared to anatomical single-bundle reconstruction surgery. However, when reconstruction surgery was individualized for patients based on intraoperative measurements, no difference was observed between single-bundle and double-bundle reconstruction surgery emphasizing importance of patient selection for either treatment group [45]. Overall, based on evidence from recent meta-analysis, it appears that double-bundle reconstruction provides superior stability and mid-term outcome scores; however, more research is needed to determine long-term outcomes [46, 47].
Treatment of associated injuries
Though the ACL serves as the primary restraint to both anteroposterior and rotational stability, especially at low flexion angles, other surrounding knee structures contribute to joint stability [48]. Concomitant injury to medial or lateral meniscus is reported to be present in 16 to 82 % in acute ACL injuries and up to 96 % in chronic ACL injuries [49–51]. In addition to load distribution function, menisci also play a role in joint stability. It has been well demonstrated that injuries to either the medial meniscus or lateral meniscus significantly increase the grade of the pivot shift test [52–54]. Not surprisingly, anterolateral capsule injuries also have been shown to increase the rotatory laxity during pivot shift test [53, 54]. In vitro biomechanical studies have supported a mainly secondary role of the anterolateral capsule to rotatory knee laxity [55–57]. However, a recent study reported that the iliotibial band (ITB) might have a more significant role in controlling knee rotatory laxity compared to the so-called anterolateral ligament or ALL [58]. Injury to the medial collateral ligament increases internal and external rotation of the knee; conversely, the pivot shift grade is reduced in this injury pattern due to elimination of the tension on the medial compartment [59].
Understanding the relative contributions of intra- and extra-articular knee stabilizers, it can be theorized that increased rotatory laxity due to untreated or undiagnosed injury to these secondary structures will cause abnormal loads on the menisci and cartilage that may ultimately increase the risk of osteoarthritis. Moreover, due to load sharing of the structures in the knee, neglected injury to secondary restraints can result in increased force on ACL graft tissue and subsequent graft failure [60]. Therefore, injuries to any or all of the secondary restraints should be timely diagnosed and addressed properly to achieve an optimal patient outcome (Table 1). The objective assessment of rotatory laxity before and during reconstruction surgery can provide physicians with subtle, previously unavailable information to more carefully identify injuries to secondary structures that may warrant operative intervention.
Table 1.
Treatment algorithm: ACL and associated injuries management
| Primary ACL reconstruction | |
| Partial ACL | Single-bundle augmentation |
| ACL small footprint | Single-bundle anatomical ACLR |
| ACL large footprint | Single- or double-bundle ACLR |
| ACL + medial and/or lateral meniscal tear | Anatomic ACLR + medial/lateral meniscal repair |
| ACL + RAMP lesion | Anatomic ACLR + RAMP lesion repair |
| ACL + MCL injury | Anatomic ACLR + healing response/consider repair |
| ACL + PLC injury | Anatomic ACLR + PLC repair/reconstruction |
| ACL + medial or lateral capsule injury | Anatomic ACLR + healing response capsule/consider repair |
| Revision ACL reconstruction | |
| ACL + medial meniscus deficiency | Revision ACLR + MM transplant |
| ACL + lateral meniscus deficiency | Revision ACLR + LM transplant |
| ACL + chronic MCL laxity | Revision ACLR + MCL reconstruction |
| ACL + posterolateral corner injury | Revision ACLR + posterolateral corner reconstruction |
| ACL+ marked increased posterior tibial slope | Revision ACLR + de-flexion proximal tibial osteotomy |
| ACL + coronal plane malalignment | Revision ACLR + proximal tibial osteotomy—for varus malalignment |
| Distal femur osteotomy—for valgus malalignment | |
ACLR anterior cruciate ligament reconstruction, MM medial meniscus, LM lateral meniscus, MCL medial collateral injury, PLC posterolateral corner
Extra-articular tenodesis
Recent reports regarding the lateral capsule complex have stimulated increased interest in combining an extra-articular tenodesis (EAT) to ACL reconstruction surgery. Different surgical techniques and graft types have been described in the literature [61–63]. However, biomechanical studies comparing different reconstruction techniques have failed to show improved stability when the so-called anatomic anterolateral ligament reconstruction was performed. Despite these findings, these studies have reinforced a significant role for a previously known tenodesis technique using a strip of iliotibial band [64].
Randomized clinical trials that compared combined EAT and ACL reconstruction with isolated ACL reconstruction have reported conflicting results regarding restraining laxity or improving functional outcome [65•]. Two recent meta-analysis of these studies revealed that patients with ACLR and EAT had superior pivot shift test and Lachman results, but no difference was found in functional outcomes or return to play [65•, 66]. Another multicenter study of revision ACL reconstruction patients with minimum 2-year follow-up revealed that combined EAT was more successful in controlling pivot shift test compared to isolated ACL reconstruction surgery [67]. Addition of EAT to ACL reconstruction has also shown to reduce stress on ACL graft by 43 % at time zero in a cadaveric study [68]. Although, adding an EAT has shown to have a positive effect on controlling knee laxity after ACL reconstruction, some authors have raised concerns about over-constraining the knee joint by restricting internal rotation [55, 69, 70•]. Hence, decision to add an EAT should be made carefully.
Combining an EAT to ACL reconstruction surgery could be considered in primary ACL reconstruction in patients with high-grade rotatory knee instability without associated meniscus or collateral ligament injuries. In revision ACL reconstruction, it should be considered if high-grade rotatory laxity is observed after treatment of all associated injuries (e.g., meniscus). Possible indications are summarized in Table 2.
Table 2.
Indications for considering combined extra-articular tenodesis with ACL reconstruction
| 1. Primary ACL injury + high-grade pivot shift without additional soft tissue injury |
| 2. Primary ACL injury + generalized ligament laxity, i.e., hyperextension >10° |
| 3. Chronic ACL injury + high-grade pivot shift |
| 4. Revision ACL + persistent high-grade pivot shift after managing associated injuries |
Future directions
In the era of individualized medicine and restructured bundled reimbursement in health care, the development of clinically applicable devices to objectively score knee instability for each individual patient is of critical importance. The evaluation of knee instability scores along with other screening scores can provide important insight influencing treatment decisions. Using the pivot shift combined with quantitative devices pre-operatively, different injury patterns and instability grades can be characterized based on patient factors.
Objective quantification of the pivot shift test in a routine clinical setting requires methods that can easily, reliably, and inexpensively measure variable knee kinematics. These devices provide objective quantification of rotatory knee instability and avoid second-guessing with subjective grading scales. Furthermore, standardized exam techniques support a universally acceptable scientific exchange [71]. The preliminary results from a cohort of ACL injured patients using two of these technologies show that rotatory knee instability is widely variable between patients. This only further emphasizes the need for individualized treatment of patients with ligamentous knee injuries. Future research is necessary to evaluate clinical outcomes of different reconstruction procedures for patients with outlier scores (Fig. 2) [16, 23•]. Developing registries of ACL injured patients could also help to define optimal thresholds by distinguishing between injury patterns and the associated outcome of different reconstruction procedures. Furthermore, in clinical outcomes research, subjective scoring systems may not be sensitive enough to detect meaningful, significant differences. The future application of widespread quantitative evaluation technologies will help correlate patient-reported outcome with objective findings of knee instability with the goal of improved patient outcomes.
Fig. 2.
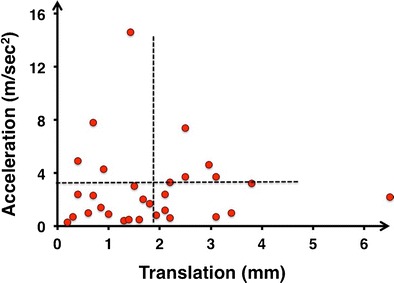
Quantitative pivot shift data for 30 ACL-injured patients. The dotted lines represent the median number for acceleration and translation, respectively. Outliers might require further treatment in addition to anatomic ACL reconstruction
Conclusions
Quantitative evaluation of knee instability allows clinicians to make strong, informed decisions by presenting knee kinematics in a manner that is accurate, reproducible, and patient specific. In the future, different treatment categories, such as non-operative, isolated ACL reconstruction or additional soft tissue repair/reconstruction can be assigned based on side-to-side comparison of quantitative knee instability. Using pre-operative side-to-side quantitative knee instability scores as a baseline, patient specific rehabilitation can be more focused on individual patient performance with the restoration of knee stability continuously monitored until return to full activity. Thus, the implementation of objective scoring systems by means of technologic advancements has a great potential to contribute to the individualized treatment in all aspects and stages of ACL reconstruction surgery.
Compliance with ethical standards
Conflict of interest
Ata A. Rahnemai-Azar, Jan-Hendrik Naendrup, Ashish Soni, Adam Olsen, and Jason Zlotnicki declare that they have no conflict of interest. Volker Musahl has received educational funding as a consultant from Smith and Nephew. He also has a patent for Pivot software Serial (No. 61/566,761) licensed to Impelia.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on ACL Update: Objective Measures on Knee Instability
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Ardern CL, Taylor NF, Feller JA, Webster KE. Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med. 2012;40(1):41–48. doi: 10.1177/0363546511422999. [DOI] [PubMed] [Google Scholar]
- 2.Peeler J, Leiter J, MacDonald P. Accuracy and reliability of anterior cruciate ligament clinical examination in a multidisciplinary sports medicine setting. Clin J Sport Med. 2010;20(2):80–85. doi: 10.1097/JSM.0b013e3181ceca45. [DOI] [PubMed] [Google Scholar]
- 3.Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976;4(2):84–93. doi: 10.1177/036354657600400206. [DOI] [PubMed] [Google Scholar]
- 4.Galway HR, MacIntosh DL. The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res. 1980;147:45–50. [PubMed] [Google Scholar]
- 5.van Eck CF, van den Bekerom MP, Fu FH, Poolman RW, Kerkhoffs GM. Methods to diagnose acute anterior cruciate ligament rupture: a meta-analysis of physical examinations with and without anaesthesia. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1895–1903. doi: 10.1007/s00167-012-2250-9. [DOI] [PubMed] [Google Scholar]
- 6.Jakob RP, Staubli HU, Deland JT. Grading the pivot shift. Objective tests with implications for treatment. J Bone Joint Surg. 1987;69(2):294–299. doi: 10.1302/0301-620X.69B2.3818763. [DOI] [PubMed] [Google Scholar]
- 7.Musahl V, Voos J, O’Loughlin PF, Stueber V, Kendoff D, Pearle AD. Mechanized pivot shift test achieves greater accuracy than manual pivot shift test. Knee Surg Sports Traumatol Arthrosc. 2010;18(9):1208–1213. doi: 10.1007/s00167-009-1004-9. [DOI] [PubMed] [Google Scholar]
- 8.Musahl V, Hoshino Y, Ahlden M, Araujo P, Irrgang JJ, Zaffagnini S, et al. The pivot shift: a global user guide. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):724–731. doi: 10.1007/s00167-011-1859-4. [DOI] [PubMed] [Google Scholar]
- 9.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 10.Irrgang JJ, Bost JE, Fu FH. Re: Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2009;37(2):421–2. doi:10.1177/0363546508327555. author reply 2. [DOI] [PubMed]
- 11.Daniel DM, Stone ML, Sachs R, Malcom L. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med. 1985;13(6):401–407. doi: 10.1177/036354658501300607. [DOI] [PubMed] [Google Scholar]
- 12.Ahlden M, Hoshino Y, Samuelsson K, Araujo P, Musahl V, Karlsson J. Dynamic knee laxity measurement devices. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):621–632. doi: 10.1007/s00167-011-1848-7. [DOI] [PubMed] [Google Scholar]
- 13.Bedi A, Musahl V, Lane C, Citak M, Warren RF, Pearle AD. Lateral compartment translation predicts the grade of pivot shift: a cadaveric and clinical analysis. Knee Surg Sports Traumatol Arthrosc. 2010;18(9):1269–1276. doi: 10.1007/s00167-010-1160-y. [DOI] [PubMed] [Google Scholar]
- 14.Hoshino Y, Kuroda R, Nagamune K, Yagi M, Mizuno K, Yamaguchi M, et al. In vivo measurement of the pivot-shift test in the anterior cruciate ligament-deficient knee using an electromagnetic device. Am J Sports Med. 2007;35(7):1098–1104. doi: 10.1177/0363546507299447. [DOI] [PubMed] [Google Scholar]
- 15.•.Muller B, Hofbauer M, Rahnemai-Azar AA, Wolf M, Araki D, Hoshino Y et al. Development of computer tablet software for clinical quantification of lateral knee compartment translation during the pivot shift test. Computer methods in biomechanics and biomedical engineering. 2015:1-12. doi:10.1080/10255842.2015.1006210. This publication described development of computer tablet software for objective quantification of anterior translation of lateral compartment during pivot shift test. It was demonstrated that this software could provide a reliable method for quantification of pivot shift with acceptable accuracy in clinical practice. [DOI] [PubMed]
- 16.Hoshino Y, Araujo P, Ahlden M, Samuelsson K, Muller B, Hofbauer M, et al. Quantitative evaluation of the pivot shift by image analysis using the iPad. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):975–980. doi: 10.1007/s00167-013-2396-0. [DOI] [PubMed] [Google Scholar]
- 17.Hoshino Y, Araujo P, Irrgang JJ, Fu FH, Musahl V. An image analysis method to quantify the lateral pivot shift test. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):703–707. doi: 10.1007/s00167-011-1845-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Arilla F, Rahnemai-Azar A, Scott B, Yacuzzi C, Guenther D, Fu F, et al. Reliability of a 2D simple image analysis method to predict 3D bony motion of the lateral. Las Vegas: Orthopeadic Research Society; 2015. [Google Scholar]
- 19.Lopomo N, Signorelli C, Bonanzinga T, Marcheggiani Muccioli GM, Visani A, Zaffagnini S. Quantitative assessment of pivot-shift using inertial sensors. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):713–717. doi: 10.1007/s00167-011-1865-6. [DOI] [PubMed] [Google Scholar]
- 20.Labbe DR, Li D, Grimard G, de Guise JA, Hagemeister N. Quantitative pivot shift assessment using combined inertial and magnetic sensing. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2330–2338. doi: 10.1007/s00167-014-3056-8. [DOI] [PubMed] [Google Scholar]
- 21.Borgstrom PH, Markolf KL, Wang Y, Xu X, Yang PR, Joshi NB, et al. Use of inertial sensors to predict pivot-shift grade and diagnose an ACL injury during preoperative testing. Am J Sports Med. 2015;43(4):857–864. doi: 10.1177/0363546514565090. [DOI] [PubMed] [Google Scholar]
- 22.Zaffagnini S, Lopomo N, Signorelli C, Marcheggiani Muccioli GM, Bonanzinga T, Grassi A, et al. Inertial sensors to quantify the pivot shift test in the treatment of anterior cruciate ligament injury. Joints. 2014;2(3):124–129. doi: 10.11138/jts/2014.2.3.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.•.Lopomo N, Zaffagnini S, Signorelli C, Bignozzi S, Giordano G, Marcheggiani Muccioli GM, et al. An original clinical methodology for non-invasive assessment of pivot-shift test. Comput Methods Biomech Biomed Engin. 2012;15(12):1323–1328. doi: 10.1080/10255842.2011.591788. [DOI] [PubMed] [Google Scholar]
- 24.Berruto M, Uboldi F, Gala L, Marelli B, Albisetti W. Is triaxial accelerometer reliable in the evaluation and grading of knee pivot-shift phenomenon? Knee Surg Sports Traumatol Arthrosc. 2013;21(4):981–985. doi: 10.1007/s00167-013-2436-9. [DOI] [PubMed] [Google Scholar]
- 25.Araujo PH, Ahlden M, Hoshino Y, Muller B, Moloney G, Fu FH, et al. Comparison of three non-invasive quantitative measurement systems for the pivot shift test. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):692–697. doi: 10.1007/s00167-011-1862-9. [DOI] [PubMed] [Google Scholar]
- 26.Bull AM, Earnshaw PH, Smith A, Katchburian MV, Hassan AN, Amis AA. Intraoperative measurement of knee kinematics in reconstruction of the anterior cruciate ligament. J Bone Joint Surg. 2002;84(7):1075–1081. doi: 10.1302/0301-620X.84B7.13094. [DOI] [PubMed] [Google Scholar]
- 27.Chalmers PN, Mall NA, Moric M, Sherman SL, Paletta GP, Cole BJ, et al. Does ACL reconstruction alter natural history?: A systematic literature review of long-term outcomes. J Bone Joint Surg Am. 2014;96(4):292–300. doi: 10.2106/JBJS.L.01713. [DOI] [PubMed] [Google Scholar]
- 28.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–342. doi: 10.1056/NEJMoa0907797. [DOI] [PubMed] [Google Scholar]
- 29.Swart E, Redler L, Fabricant PD, Mandelbaum BR, Ahmad CS, Wang YC. Prevention and screening programs for anterior cruciate ligament injuries in young athletes: a cost-effectiveness analysis. J Bone Joint Surg Am. 2014;96(9):705–711. doi: 10.2106/JBJS.M.00560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W. The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med. 2007;35(2):223–227. doi: 10.1177/0363546506294571. [DOI] [PubMed] [Google Scholar]
- 31.Petersen W, Zantop T. Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res. 2007;454:35–47. doi: 10.1097/BLO.0b013e31802b4a59. [DOI] [PubMed] [Google Scholar]
- 32.Gabriel MT, Wong EK, Woo SL, Yagi M, Debski RE. Distribution of in situ forces in the anterior cruciate ligament in response to rotatory loads. J Orthop Res. 2004;22(1):85–89. doi: 10.1016/S0736-0266(03)00133-5. [DOI] [PubMed] [Google Scholar]
- 33.Adachi N, Ochi M, Uchio Y, Sumen Y. Anterior cruciate ligament augmentation under arthroscopy. A minimum 2-year follow-up in 40 patients. Arch Orthop Trauma Surg. 2000;120(3-4):128–133. doi: 10.1007/s004020050028. [DOI] [PubMed] [Google Scholar]
- 34.Ochi M, Adachi N, Uchio Y, Deie M, Kumahashi N, Ishikawa M, et al. A minimum 2-year follow-up after selective anteromedial or posterolateral bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25(2):117–122. doi: 10.1016/j.arthro.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 35.Araki D, Kuroda R, Matsushita T, Matsumoto T, Kubo S, Nagamune K, et al. Biomechanical analysis of the knee with partial anterior cruciate ligament disruption: quantitative evaluation using an electromagnetic measurement system. Arthroscopy. 2013;29(6):1053–1062. doi: 10.1016/j.arthro.2013.02.012. [DOI] [PubMed] [Google Scholar]
- 36.Yoon KH, Lee SH, Park SY, Kang DG, Chung KY. Can physical examination predict the intraarticular tear pattern of the anterior cruciate ligament? Arch Orthop Trauma Surg. 2014;134(10):1451–1457. doi: 10.1007/s00402-014-2048-y. [DOI] [PubMed] [Google Scholar]
- 37.Hu J, Qu J, Xu D, Zhang T, Zhou J, Lu H. Clinical outcomes of remnant preserving augmentation in anterior cruciate ligament reconstruction: a systematic review. Knee Surg Sports traumatol Arthrosc. 2014;22(9):1976–1985. doi: 10.1007/s00167-013-2749-8. [DOI] [PubMed] [Google Scholar]
- 38.Kopf S, Pombo MW, Szczodry M, Irrgang JJ, Fu FH. Size variability of the human anterior cruciate ligament insertion sites. Am J Sports Med. 2011;39(1):108–113. doi: 10.1177/0363546510377399. [DOI] [PubMed] [Google Scholar]
- 39.Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012;28(4):526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 40.Middleton KK, Muller B, Araujo PH, Fujimaki Y, Rabuck SJ, Irrgang JJ, et al. Is the native ACL insertion site “completely restored” using an individualized approach to single-bundle ACL-R? Knee Surg Sports traumatol Arthrosc. 2015;23(8):2145–2150. doi: 10.1007/s00167-014-3043-0. [DOI] [PubMed] [Google Scholar]
- 41.Zelle BA, Vidal AF, Brucker PU, Fu FH. Double-bundle reconstruction of the anterior cruciate ligament: anatomic and biomechanical rationale. J Am Acad Orthop Surg. 2007;15(2):87–96. doi: 10.5435/00124635-200702000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002;30(5):660–666. doi: 10.1177/03635465020300050501. [DOI] [PubMed] [Google Scholar]
- 43.Morimoto Y, Ferretti M, Ekdahl M, Smolinski P, Fu FH. Tibiofemoral joint contact area and pressure after single- and double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009;25(1):62–69. doi: 10.1016/j.arthro.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 44.Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. 2012. [DOI] [PubMed]
- 45.Individualized anterior cruciate ligament surgery: a prospective study comparing anatomic single- and double-bundle reconstruction. 2012. [DOI] [PubMed]
- 46.Desai N, Bjornsson H, Musahl V, Bhandari M, Petzold M, Fu FH, et al. Anatomic single- versus double-bundle ACL reconstruction: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2014;22(5):1009–1023. doi: 10.1007/s00167-013-2811-6. [DOI] [PubMed] [Google Scholar]
- 47.Chen G, Wang S. Comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction after a minimum of 3-year follow-up: a meta-analysis of randomized controlled trials. Int J Clin Exp Med. 2015;8(9):14604–14614. [PMC free article] [PubMed] [Google Scholar]
- 48.Lipke JM, Janecki CJ, Nelson CL, McLeod P, Thompson C, Thompson J, et al. The role of incompetence of the anterior cruciate and lateral ligaments in anterolateral and anteromedial instability. A biomechanical study of cadaver knees. J Bone Joint Surg Am. 1981;63(6):954–960. [PubMed] [Google Scholar]
- 49.Kilcoyne KG, Dickens JF, Haniuk E, Cameron KL, Owens BD. Epidemiology of meniscal injury associated with ACL tears in young athletes. Orthopedics. 2012;35(3):208–212. doi: 10.3928/01477447-20120222-07. [DOI] [PubMed] [Google Scholar]
- 50.Sharifah MI, Lee CL, Suraya A, Johan A, Syed AF, Tan SP. Accuracy of MRI in the diagnosis of meniscal tears in patients with chronic ACL tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):826–830. doi: 10.1007/s00167-013-2766-7. [DOI] [PubMed] [Google Scholar]
- 51.Krinsky MB, Abdenour TE, Starkey C, Albo RA, Chu DA. Incidence of lateral meniscus injury in professional basketball players. Am J Sports Med. 1992;20(1):17–19. doi: 10.1177/036354659202000105. [DOI] [PubMed] [Google Scholar]
- 52.Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38(8):1591–1597. doi: 10.1177/0363546510364402. [DOI] [PubMed] [Google Scholar]
- 53.Musahl V, Rahnemai-Azar A, Costello J, Arner J, Fu F, Hoshino Y, et al. The influence of anterolateral capsular injury on knee laxity of anterior cruciate ligament injured patients. Orlando: Orthopaedic Research Society; 2016. [DOI] [PubMed] [Google Scholar]
- 54.Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H. Risk factors associated with grade 3 pivot shift after acute anterior cruciate ligament injuries. The American journal of sports medicine. 2015. doi:10.1177/0363546515613069. [DOI] [PubMed]
- 55.Arilla F, Guenther D, Yacuzzi C, Rahnemai-Azar A, Fu F, Debski R, et al. Effects of anterolateral capsular injury and extra-articular tenodesis on knee kinematics during physical examination. American Orthopaedic Society for Sports Medicine. Orlando: Orthopaedic Journal of Sports Medicine; 2015. p. 2325967115S00032. [Google Scholar]
- 56.Monaco E, Ferretti A, Labianca L, Maestri B, Speranza A, Kelly MJ, et al. Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surg Sports Traumatol Arthrosc. 2012;20(5):870–877. doi: 10.1007/s00167-011-1640-8. [DOI] [PubMed] [Google Scholar]
- 57.Rasmussen MT, Nitri M, Williams BT, Moulton SG, Cruz RS, Dornan GJ et al. An in vitro robotic assessment of the anterolateral ligament, part 1: secondary role of the anterolateral ligament in the setting of an anterior cruciate ligament injury. The American journal of sports medicine. 2015. doi:10.1177/0363546515618387. [DOI] [PubMed]
- 58.Kittl C, El-Daou H, Athwal KK, Gupte CM, Weiler A, Williams A, et al. The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee. Am J Sports Med. 2016;44(2):345–354. doi: 10.1177/0363546515614312. [DOI] [PubMed] [Google Scholar]
- 59.Cavaignac E, Carpentier K, Pailhe R, Luyckx T, Bellemans J. The role of the deep medial collateral ligament in controlling rotational stability of the knee. Knee Surg Sports Traumatol Arthrosc. 2014. doi:10.1007/s00167-014-3095-1. [DOI] [PubMed]
- 60.LaPrade RF, Resig S, Wentorf F, Lewis JL. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med. 1999;27(4):469–475. doi: 10.1177/03635465990270041101. [DOI] [PubMed] [Google Scholar]
- 61.Lemaire M, Combelles F. Plastic repair with fascia lata for old tears of the anterior cruciate ligament (author’s transl) Rev Chir Orthop Reparatrice Appar Mot. 1980;66(8):523–525. [PubMed] [Google Scholar]
- 62.Marcacci M, Zaffagnini S, Iacono F, Neri MP, Loreti I, Petitto A. Arthroscopic intra- and extra-articular anterior cruciate ligament reconstruction with gracilis and semitendinosus tendons. Knee Surg Sports Traumatol Arthrosc. 1998;6(2):68–75. doi: 10.1007/s001670050075. [DOI] [PubMed] [Google Scholar]
- 63.Ireland J, Trickey EL. Macintosh tenodesis for anterolateral instability of the knee. J Bone Joint Surg. 1980;62(3):340–345. doi: 10.1302/0301-620X.62B3.7410466. [DOI] [PubMed] [Google Scholar]
- 64.Spencer L, Burkhart TA, Tran MN, Rezansoff AJ, Deo S, Caterine S, et al. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am J Sports Med. 2015;43(9):2189–2197. doi: 10.1177/0363546515589166. [DOI] [PubMed] [Google Scholar]
- 65.•.Hewison CE, Tran MN, Kaniki N, Remtulla A, Bryant D, Getgood AM. Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: a systematic review of the literature. Arthroscopy. 2015;31(10):2022–2034. doi: 10.1016/j.arthro.2015.04.089. [DOI] [PubMed] [Google Scholar]
- 66.Rezende FC, de Moraes VY, Martimbianco AL, Luzo MV, da Silveira Franciozi CE, Belloti JC. Does combined intra- and extraarticular ACL reconstruction improve function and stability? A meta-analysis. Clin Orthop Relat Res. 2015;473(8):2609–2618. doi: 10.1007/s11999-015-4285-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Trojani C, Beaufils P, Burdin G, Bussiere C, Chassaing V, Djian P, et al. Revision ACL reconstruction: influence of a lateral tenodesis. Knee Surg Sports Traumatol Arthrosc. 2012;20(8):1565–1570. doi: 10.1007/s00167-011-1765-9. [DOI] [PubMed] [Google Scholar]
- 68.Engebretsen L, Lew WD, Lewis JL, Hunter RE. Knee mechanics after repair of the anterior cruciate ligament. A cadaver study of ligament augmentation. Acta Orthop Scand. 1989;60(6):703–709. doi: 10.3109/17453678909149609. [DOI] [PubMed] [Google Scholar]
- 69.Rahnemai-Azar AA, Miller RM, Guenther D, Fu FH, Lesniak BP, Musahl V et al. Structural properties of the anterolateral capsule and iliotibial band of the knee. The American journal of sports medicine. 2016. doi:10.1177/0363546515623500. [DOI] [PubMed]
- 70.•.Branch T, Lavoie F, Guier C, Branch E, Lording T, Stinton S, et al. Single-bundle ACL reconstruction with and without extra-articular reconstruction: evaluation with robotic lower leg rotation testing and patient satisfaction scores. Knee Surg Sports Traumatol Arthrosc. 2015;23(10):2882–2891. doi: 10.1007/s00167-015-3772-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hoshino Y, Araujo P, Ahlden M, Moore CG, Kuroda R, Zaffagnini S, et al. Standardized pivot shift test improves measurement accuracy. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):732–736. doi: 10.1007/s00167-011-1850-0. [DOI] [PubMed] [Google Scholar]


