Abstract
Overhead athletes subject their elbows to significant valgus stresses throughout the throwing cycle. A steady rise in the number of medial-sided elbow injuries over the years has lead to increased awareness regarding the pathophysiology of the “pitcher’s elbow.” As our understanding of the functional anatomy and throwing biomechanics has become more sophisticated, we have seen a concurrent improvement in the outcomes associated with managing these injuries. Despite this improvement, continued anatomical and biomechanical research is still needed to further optimize outcomes and return to sport.
Keywords: Pitcher’s elbow, Ulnar collateral ligament, Valgus instability, Medial elbow pain, Posteromedial impingement, Valgus extension overload syndrome
Introduction
With the steady increase in the number of participants in overhead-throwing sports over the last few decades, there has been a proportional increase in the incidence of upper extremity injuries among this population [1•]. Historically, discussion of overhead-throwing injuries sustained to the elbow has focused on athletes participating in baseball. This has lead to a commonly accepted general term, “pitcher’s elbow,” to describe injuries sustained to the elbow in the throwing athlete. Despite the connotation associated with this non-specific term, “pitcher’s elbow” can affect any athlete participating in overhead-throwing sports (i.e., softball, football, tennis, javelin, etc.).
Due to the complexity of the functional anatomy of the elbow and the significant biomechanical forces generated during a typical throwing cycle, treating clinicians must have a working knowledge of both these topics in order to effectively treat this growing population. The purpose of this review is to ensure clinicians not only understand relevant anatomy and biomechanics but also understand how they relate to typical complaints and pathology found in the overhead-throwing athlete. The presentation, diagnosis, management (both non-operative and operative), and outcomes of each elbow malady will also be reviewed.
Relevant anatomy
Stability of the elbow is provided by both bony articulations and soft tissue restraints. The ulno-humeral joint, namely the articulation between the olecranon and the olecranon fossa, is the primary stabilizer at the extremes of elbow motion—flexion less than 20° and greater than 120° [2]. Soft tissue restraints have been shown to provide the primary static and dynamic stability needed in the mid arc of elbow motion [3].
The ulnar collateral ligament (UCL) is the main, soft tissue constraint to valgus instability of the elbow. It is composed of three bundles: anterior bundle, posterior bundle, and transverse bundle. The anterior bundle has been shown to be the primary valgus stabilizer of the UCL between 30° and 120° of flexion, which is when the medial elbow experiences the highest level of valgus force during overhead throwing [3, 4].
The anterior bundle of the UCL is attached proximally at the medial epicondyle of the humerus and attached distally on the sublime tubercle of the proximal ulna. It is subdivided into an anterior band and a posterior band. The anterior band is the primary restraint to valgus stress up to 90° of flexion, while the posterior band becomes increasingly more important as a stabilizer with flexion beyond 90° [5].
The common flexor musculature is comprised of the pronator teres, flexor carpi radialis, palmaris longus, flexor carpi ulnaris, and flexor digitorum superficialis. These muscles originate from the medial epicondyle and act as dynamic stabilizers to valgus forces at the elbow.
The ulnar nerve is another medial structure of the elbow that is susceptible to injury in this patient population. The nerve passes the elbow joint within the cubital tunnel, just posterior to the medial epicondyle of the humerus and immediately superficial to the UCL. Ulnar nerve inflammation, compression, or subluxation can lead to severe ulnar nerve symptoms in these athletes that present with pain, numbness, and weakness distally.
Lateral stability of the elbow is provided by the radiocapitellar joint, radial collateral ligament, and common extensor muscles. Although lateral-sided injuries in the overhead-throwing athlete are much less common, an understanding of the static and dynamic lateral stabilizers is needed when evaluating these patients.
Throwing biomechanics
The baseball pitch has been widely studied and can be divided into five main stages. Phase I (windup) involves initial preparation as the elbow flexes and the forearm is slightly pronated. Phase II (early cocking) begins when the ball leaves the glove hand and is complete when the forward foot contacts the ground. Shoulder abduction and external rotation are initiated in this stage. Phase III (late cocking) is characterized by further shoulder abduction and maximal external rotation. Additionally, the elbow flexes between 90° and 120° and the forearm pronates to 90°.
Phase IV (rapid acceleration) generates a large forward-directed force on the extremity that is accompanied by rapid elbow extension. This stage terminates with ball release. Tremendous valgus stress is generated over the medial aspect of the elbow during this stage, a majority of which is transmitted to the anterior bundle of the UCL. The remainder of the stress is dissipated by the secondary supporting structures of the medial elbow, mainly the flexor-pronator musculature. Phase V (follow-through) involves dissipation of all excess kinetic energy as the elbow reaches full extension and finalizes at completion of motion [6, 7].
Multiple biomechanical studies have shown that the elbow extends over 2300°/s during the throwing cycle. This generates a medial shear force of approximately 300 N and a lateral compressive force of nearly 900 N [8, 9•, 10]. Furthermore, in the acceleration phase of the throwing cycle, an additional 64 N of valgus stress is applied to the elbow [9•, 10].
These extraordinary forces generated on the elbow joint by the overhead athlete leaves the elbow especially vulnerable to injury. The typical pattern of injury sustained is either due to repetitive microtrauma or chronic stress overload.
Valgus instability
Valgus instability caused by ulnar collateral ligament deficiency is rapidly increasing in incidence. This is easily demonstrated by observing the significant increase in the number of Major League Baseball pitchers who have undergone UCL reconstruction between the years 1986 and 2012 [11•]. Further proof of this upsurge is noted when considering the alarming increase in high school athletes undergoing this same surgery [12].
Repetitive microtrauma and chronic stress on the medial elbow during the acceleration phase of throwing can lead to laxity and injury to the UCL over time. The anterior bundle of the UCL, as the primary valgus stabilizer of the elbow from 30° to 120°, is most susceptible to injury in these athletes. More specifically, the posterior band of the anterior bundle is taut when the elbow is flexed from 90° to 120°. Since the largest force is generated through the elbow during the acceleration phase (phase IV) when the elbow is flexed from 90° to 100°, the posterior band of the anterior bundle is most commonly effected [13•]. Disruption of the UCL can lead to pain, loss of throwing velocity, lack of throwing endurance, and less commonly a subjective sense of instability.
Evaluation
A thorough history and physical examination are the most important components of the evaluation and diagnosis of an ulnar collateral ligament injury. Radiographic studies are required to confirm this suspected injury. The athlete with an acute UCL injury typically describes the sudden onset of pain with throwing. In approximately 50 % of cases, the patient will report hearing or feeling a “pop” and are typically unable to continue throwing. More chronic injuries may not present as obvious. They will likely be described as a gradual onset of pain localized to the medial elbow that worsens in the late cocking or early acceleration phase of throwing [14]. A decrease in maximum velocity is also typically reported in chronic cases. Local inflammation of the unstable ligamentous complex can lead to other common elbow complaints such as ulnar nerve symptoms secondary to irritation of the nerve within the cubital tunnel, flexor-pronator mass strain, or medial epicondylitis [15].
Physical examination should begin with a thorough evaluation of the upper extremity. Proximally, the shoulder should be examined for any deficits in range of motion or rotator cuff symptoms. Additionally, scapular motion and position should be assessed to rule out possible dyskinesia. Examination of the elbow with suspected valgus instability may be performed with the patient seated and the elbow flexed 20–30°. This unlocks the olecranon from its fossa and allows isolated testing of the anterior bundle of the UCL. Palpation is first performed along the UCL as it courses from the medial epicondyle toward the proximal ulna. A slight valgus load is then applied to the elbow and any medial joint space opening may signify potential valgus laxity. If suspected, comparison with the contralateral elbow should be performed. Loss of a firm endpoint that is associated with increased medial joint space opening is consisted with an injured UCL. However, it should be noted that most throwing athletes will have a certain degree of increased laxity of the dominant throwing elbow with applied valgus stress when compared to the non-dominant elbow. Therefore, asymmetry of a static valgus stress test alone is typically not sufficient to diagnose an ulnar collateral ligament injury in a throwing athlete.
The milking maneuver has been described as a useful test to assess the functionally more important posterior band of the anterior bundle. This is performed by pulling on the patient’s thumb in order to apply valgus stress while the patient’s shoulder is forward elevated to 90° and elbow flexed beyond 90° [15]. Pain over the UCL with or without apprehension or instability is considered a positive test and suggestive of UCL injury.
Elbow radiographs should be routinely obtained. In rare cases, an avulsion fracture of the sublime tubercle may be seen in acute-on-chronic cases. Radiographs may show calcification or ossification of the medial ligamentous complex. These findings may be evident in chronic UCL injuries; however, they are rarely seen following an acute injury. Stress radiographs using a standardized elbow valgus stress gadget can be used to assess for possible instability and are considered positive when the medial joint opening is found to be greater than 2.9 mm when compared to the contralateral side [15, 16].
Magnetic resonance (MR) imaging has become the gold standard at confirming a diagnosis of UCL injury. MRA has been found to have a sensitivity of 92 % and a specificity of 100 %. It has also been shown to have the best inter-observer reliability [17]. Recent studies have indicated that MRIs may also be prognostic, as retrospective analysis has shown that a UCL injury with higher T2 signal intensity is less likely to respond to conservative treatment [18].
Recently, ultrasound evaluation has also been reported to have usefulness in the diagnosis of UCL injury. Specifically, the dynamic ultrasound test has been found to be a highly reliable tool in diagnosing laxity of the UCL over time as shown by Nazrian et al. and Ciccotti et al. [19•, 20].
Treatment
The cornerstone of non-operative treatment for UCL injuries is eliminating the aggravating event (i.e., throwing) for an extended period of time and slowly initiating a course of physical therapy that focuses on maintaining elbow range of motion and strengthening the flexor-pronator musculature. Additionally, strengthening exercises focused on the core and shoulder musculature have been shown to minimize forces across the elbow and optimize neuromuscular control of the extremity [21•]. These modalities are often done in concordance with daily icing, anti-inflammatory medication, and bracing. Once the elbow is pain free, a well-supervised, progressive return to throwing may be initiated over a 2–3-month period. When non-operative measures are exhausted and an athlete continues to have significant dysfunction with persistent medial elbow pain that prevents the athlete from returning to a prior activity level, surgical intervention may be indicated.
Surgical reconstruction of the ulnar collateral ligament was first described by Jobe et al. in 1986 [22]. This technique involved elevation of the flexor muscles off the medial epicondyle as well as a submuscular transposition of the ulnar nerve. Attachment points of the native UCL were identified and re-approximated with two drill holes in the ulna and three drill holes in the medial epicondyle. Palmaris longus autograft was then passed through the tunnels using a figure-of-eight configuration and sutured back to itself.
Since Jobe’s initial description, there have been numerous modifications described in the literature [23–29]. These modifications typically involve differing techniques on dealing with graft fixation, ulnar nerve management, and graft configuration. The most commonly used graft in UCL reconstruction is the palmaris longus autograft; however, other autograft options include gracilis, plantaris, or toe extensor tendon [2].
The senior author’s (LSO) preferred surgical management of UCL injuries in the overhead athlete depends on the preoperative evaluation of the behavior of the ulnar nerve. If the athlete does not have a subluxating ulnar nerve, then a muscle splitting surgical approach using a modified docking technique is used [28]. If the athlete has a subluxating ulnar nerve, then the preferred method is to transpose the ulnar nerve and elevate and separate the flexor-pronator muscle group off the UCL without disrupting either structure. In either technique, an ipsilateral palmaris longus tendon is harvested and then used to reconstruct the UCL. Once the appropriate drill holes are placed in the medial epicondyle and proximal ulna, the graft is passed through the ulna and “docked” into the medial epicondyle of the humerus.
The drill holes in the ulna are made with a 3.2-mm drill bit for a palmaris longus autograft or a 3.5-mm drill bit for a gracilis autograft. After the graft has been passed through the ulnar bone tunnel, the docking site in the medial epicondyle is made with the aid of a 4.5-mm drill hole and connected by two additional 1.5-mm drill holes (one anteriorly and one posteriorly). One end of the graft is passed through the docking hole, and tension is maintained while the other end of the graft positioned over the medical epicondyle in order to determine the location of suture placement so as not to bottom out on the docking hole. Once a braided non-absorbable suture has been placed on the appropriate location on the end of the graft, both ends of the graft are docked into the main bone tunnel in the medial epicondyle. Once the elbow is taken through a range of motion and appropriate graft tension is confirmed, the sutures are tied securely over the humeral bone bridge, and the graft is fixed in place while the elbow held in 30° of flexion and the forearm in neutral rotation. Additional sutures may then be used to sew the reconstructed graft back to the native UCL stump, further strengthening the reconstruction.
Outcomes
The first successful UCL reconstruction surgery was performed in 1974 by Dr. Frank Jobe, on Los Angeles Dodgers pitcher, Tommy John. Prior to this surgery, a UCL tear was considered to be a career-ending injury. Tommy John’s return to baseball in 1976 changed the way this injury was viewed and marked the initiation of an evolution of surgical techniques that would take place over the next 40 years.
Dr. Jobe’s initial results on baseball pitchers and javelin throwers reported a 63 % success rate, as defined by return to pre-injury or better level of participation in athletic activity. This original surgery, however, was associated with a 32 % complication rate, primarily related to postoperative ulnar neuropathy [22].
The numerous modifications to this procedure that have been described through the years have all focused on minimizing complications and optimizing return to play. A recent systematic review looking at numerous series of UCL reconstruction surgeries with a minimum of 75 % follow-up showed an 83 % success rate. This success rate was defined as a rating of “excellent” on the Conway-Jobe rating scale [30]. The same review identified several advancements in the original technique that appear to be associated with improved rate of return to prior level of play and decreased complication rate. One of the most significant modifications is the development of the muscle splitting technique as described by Smith et al. [31] The original description of this technique was accompanied by a 0 % ulnar neuropathy rate in their series of 22 patients at 1-year follow-up.
With the introduction of the docking technique as described by Rohbrough and Altcheck [28], Dodson et al. reported a 90 % rate of return to previous level of play for at least 1 year and only a 2 % rate of ulnar neuropathy postoperatively [32]. These results were reconfirmed by Koh et al. who used a modified docking technique and reported a 95 % rate of return to sports at the athlete’s previous level of competition for at least 1 year and a 5 % rate of ulnar neuropathy [33].
Overall, the past 30 years has been marked by an evolution in surgical technique to address UCL injuries. Outcomes have steadily improved and have been estimated to achieve an overall 82 % success rate of excellent results [30]. A more recent study looking specifically at MLB pitchers has shown an 83 % return to sport following ulnar collateral ligament reconstruction [11•]. Although these results are promising and UCL injury is no longer considered a career-ending injury, high-performance athletes should understand that success rate is not 100 %.
Posteromedial impingement
Posteromedial impingement was first described in 1983 by Wilson et al. [34]. This condition has also become known as valgus extension overload syndrome and is almost exclusively found in overhead-throwing athletes.
An overload of medial tension secondary to extreme repetitive valgus stress may lead to injury and inflammation to the surrounding soft tissue structures of the elbow. Microtrauma to the UCL may occur, leading to subtle valgus instability. This instability will lead to excessive force being transmitted to the lateral and posterior elbow compartments that is most significant in the late cocking and follow-through phases, as the elbow comes into extension. With the continuance of throwing in the setting of subtle instability, shear forces due to a combination of compressive and rotatory forces gradually increase, leading to synovitis and osteophyte formation [34, 35].
Osteophyte formation is hastened as abutment of the olecranon with the olecranon fossa that occurs as the elbow extends. This impingement can lead to worsening pain and posterior synovitis. Increased forces across the articular surface of the elbow then lead to chondromalacia and loose body formation [34, 35] (Fig. 1).
Fig. 1.
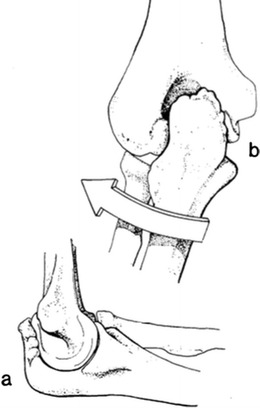
The mechanism of valgus extension overload syndrome. a Lateral view demonstrating the posterior olecranon osteophytes typically seen. b PA view demonstrating the valgus force (demonstrated by the arrow) that will ultimately lead to the formation of olecranon osteophytes. Borrowed with permission from Wilson et al. [34]
Evaluation
A thorough history of athletes suffering from valgus extension overload syndrome typically involves a complaint of posterior or posteromedial pain during the follow-through phase of throwing. It is during this final phase of throwing that the elbow extends and the posterior osteophytes impinge. Pain that occurs earlier in the throwing cycle (i.e., late cocking/early acceleration phase) should raise suspicion for other pathology such as UCL injury. If loose bodies are present, the athlete may also report mechanical symptoms such as locking or catching.
Physical examination should focus on the evaluation of range of motion. Posterior osteophytes often lead to loss of terminal extension. In these patients, forced terminal extension may lead to pain. Additionally, Andrews described the “valgus extension overload test” or the “valgus extension snap maneuver” [9•]. In this test, a moderate valgus stress is applied to the elbow with simultaneous palpation of the posteromedial tip of the olecranon. The elbow is then moved from 30° of flexion to full extension. Pain elicited from this maneuver is considered a positive test. As this condition is caused by repetitive valgus strain, the examiner must also assess for UCL laxity.
Imaging of overhead athletes with suspected valgus extension overload syndrome should first include plain radiographs of the elbow. Anteroposterior, lateral, and axial views are typically the views of choice. The axial view has been shown to be helpful in detecting osteophytes on the olecranon or on the borders of the posterior fossa [9•]. However, our preference is to obtain a computed tomography (CT) scan. A CT scan may be used to further assess or rule out other bony pathology that could cause similar pain symptoms such as stress fractures or avulsion fractures. Magnetic resonance imaging with or without intra-articular contrast may also be a useful imaging modality in many cases. The sensitivity of the MRI for identifying posterior loose bodies or osteophytes has been found to be 90 % [9•].
Treatment
Non-operative treatment of valgus extension overload syndrome consists of an initial period of rest along with a course of ice and anti-inflammatories. Once the initial pain resolves, functional strengthening of the elbow and forearm is initiated with the aid of stretching and isotonic and isometric strengthening. As range of motion and strength improve, strengthening of the flexor-pronator musculature and a supervised throwing program can be progressively initiated. Surgical intervention is indicated if these modalities fail or if the athlete is having significant mechanical symptoms secondary to loose bodies within the elbow joint.
The surgical procedure of choice in the overhead athlete that fails conservative treatment of posteromedial impingement is osteophyte excision and exploration for loose bodies. Although this procedure was originally described by Bennet et al. as an open procedure [36], the current trend is for arthroscopic intervention.
Elbow arthroscopy allows visualization of all compartments as well as arthroscopic evaluation of the UCL with an arthroscopic valgus stress test. With arthroscopy, chondromalacia of the ulnohumeral or lateral-sided radiocapitellar joint may be treated with debridement or drilling. Loose body excision and debridement of hypertrophic scar tissue and synovium can also be adequately addressed through the arthroscope. Posterior and posteromedial osteophytes can be easily visualized and debrided to address impingement within the olecranon fossa. Care is taken to debride only enough osteophyte that is needed to allow impingement-free motion. Over-resection has been associated with delayed rupture of the UCL. (Andrews et al.)
A crucial portion of the elbow arthroscopy is the intra-articular evaluation of the UCL [37]. An arthroscopic valgus stress test is performed with the elbow in 70° of flexion. If, under direct visualization, medial opening of greater than 1–2 mm occurs, ulnar collateral ligament insufficiency is suggested. If insufficiency is noted, surgical reconstruction of the UCL must be considered to minimize recurrence and optimize outcome.
Outcomes
The results of arthroscopic treatment for symptomatic and recalcitrant valgus extension overload syndrome are variable in the literature. Andrews and Timmerman reported on 56 major league baseball pitchers who underwent arthroscopic posterior olecranon osteophyte excision. There series found a 68 % return to play for at least one season; however, it was associated with a 41 % reoperation rate. They concluded that the incidence of UCL insufficiency in these overhead athletes was likely underestimated and that procedures solely addressing secondary effects of UCL insufficiency (posteromedial osteophytes) without addressing the underlying primary pathology are associated with unsatisfactory results [38].
More recently, Reddy et al. reviewed 187 elbow arthroscopies. In their series, 51 % of patients had posterior olecranon impingement, 31 % were noted to have loose bodies, and 22 % were reported to have findings consistent with degenerative joint disease. Of this cohort, they reported an 85 % return to previous level of competition [39]. Their reoperation rate was not reported.
It has been hypothesized that these mixed results are likely secondary to an initial void in our understanding of the underlying pathology. Currently, it is unclear whether the removal of posteromedial osteophytes uncovers underlying UCL insufficiency or their excision places the overhead athlete at increased risk of UCL rupture with return to throwing secondary to increased strain on the medial elbow. Long-term follow-up studies that utilize the arthroscopic valgus stress test for intra-articular UCL evaluation will likely be needed to definitively answer this question.
Ulnar neuropathy in the overhead athlete
Ulnar nerve symptoms are common in the throwing athlete and have been estimated to occur in over 40 % of athletes with valgus instability [14]. These symptoms may occur secondary to traction from excessive valgus stress, compression by nearby osteophytes, flexor muscle hypertrophy, or irritation due to subluxation [2].
Evaluation
Throwing athletes with ulnar neuropathy typically complain of paresthesia in the small and ring fingers that occurs during or after throwing. A full motor sensory exam of the upper extremity should be performed with specific attention to hand intrinsic strength and muscle mass. Any weakness or atrophy compared to the contralateral extremity should be noted and alert the clinician to potential ulnar nerve compression or irritation.
Although ulnar nerve compression can typically occur anywhere along the upper extremity, in throwing athletes, it almost exclusively occurs about the elbow. A positive Tinel’s sign over the cubital tunnel or just proximal or distal to the tunnel often confirms ulnar neuropathy at the level of the elbow. In these patients, the elbow should be taken through a range of motion and UCL competency should be carefully tested. Palpation of the ulnar nerve during flexion/extension of the elbow should also be performed to rule out ulnar nerve subluxation—a common cause of ulnar neuritis in the overhead athlete.
Treatment
Non-operative treatment of ulnar neuritis includes rest, avoidance of inciting activity, and the use of anti-inflammatory medication. Once pain resolves, an interval, supervised, throwing program may be initiated. In patients with ulnar nerve subluxation, the elbow may be splinted for a period of 6 weeks to immobilize the nerve and minimize irritation.
When non-operative measures fail to alleviate the symptoms of ulnar neuropathy in the overhead athlete, surgical treatment is indicated. Treatment options typically include in situ ulnar nerve decompression versus ulnar nerve decompression with transposition. The decision to transpose the nerve or perform an in situ decompression should be based on whether or not the ulnar nerve is found to be unstable on preoperative exam or at the time of surgery.
Ulnar nerve decompression takes place with a medial-based incision centered over the medial epicondyle. Once the medial antebrachial cutaneous nerve is identified and protected, dissection is taken down to the cubital tunnel and the ulnar nerve is identified. The nerve is then decompressed beginning proximally at the arcade of Struthers and extending distally down to the flexor carpi ulnaris muscle belly origin. Care is taken to ensure adequate decompression at all the potential sites of compression as described by Amadio et al., including the arcade of Struthers, intermuscular septum, Osborne’s fascia, fascia of the flexor carpi ulnaris, and the two heads of the flexor carpi ulnaris as well as the deep aponeurosis of the flexor carpi ulnaris [40]. In athletes who did not demonstrate an unstable ulnar nerve preoperatively, the stability of the ulnar nerve needs to be assessed after the neurolysis to determine its stability. A transposition should be performed if the nerve is felt to be unstable.
Subcutaneous transposition is commonly utilized to address the unstable ulnar nerve in the overhead-throwing athlete compared to a submuscular transposition so as not to disrupt the flexor-pronator muscle group that is important for medial elbow stability as a dynamic stabilizer. With submuscular transposition, the flexor origin is elevated off the medial epicondyle and then reattached through drill holes after the nerve is moved anteriorly. In subcutaneous transposition, the nerve is moved anteriorly and rests on top of the flexor origin. It may be held in place by fascial slings that have been created by the flexor fascia distally or the intermuscular septum proximally. Care should be taken that these fascial slings do not create a new area of compression or kinking of the ulnar nerve. A more thorough discussion of surgical technique for ulnar nerve transposition is beyond the scope of this review.
Outcomes
Traditionally, authors have advocated for submuscular transposition of the ulnar nerve in the overhead athlete as they believe this better protects the nerve from future direct or indirect trauma [41–44]. Several of these reports have shown excellent results with high rates of return to play. A potential disadvantage of submuscular transposition is the lengthy rehabilitation period that is required to allow the reattached flexor-pronator origin time to heal.
Andrews and Timmerman advocate for anterior subcutaneous ulnar nerve transfer with their report on eight professional baseball players that underwent this procedure. They reported an 88 % return to play for at least one season at the professional level [38]. These results were further reinforced by Rettig et al. when they reported a 95 % return to play at an average 12.6 weeks postoperatively in 20 high-level athletes [45].
As previously discussed, ulnar neuritis is often seen in the setting of UCL insufficiency. In this setting, concomitant procedures for UCL reconstruction and ulnar nerve decompression, with or without transposition, are indicated. More recently, Cain et al. looked at 1281 UCL reconstructions. All cases were performed along with an anterior subcutaneous ulnar nerve transposition. In this study, 83 % of athletes returned to the same or higher level of play postoperatively. They reported a 16 % incidence of postoperative ulnar nerve symptoms with anterior subcutaneous transposition. All but one of these cases fully resolved without further intervention by 1 year [46].
Flexor-pronator muscle mass injuries
Much of the dynamic stability about the medial elbow during the throwing cycle is provided by the common flexor-pronator muscle origin. Repetitive valgus stress leads to continued muscle contraction of the common flexor-pronator muscle, which can lead to muscle fatigue and may lead to injury. These injuries typically occur during the acceleration and follow-through phases of the throwing cycle with forceful extension of the elbow and pronation of the forearm. Injuries can range from mild muscular overuse to chronic tendinitis or acute muscle tears [2].
Evaluation and treatment
The overhead athlete with flexor-pronator muscle mass injury typically complains of medial-sided elbow pain during the late cocking or acceleration phase. This is a typical presentation of UCL injury, and so careful examination must be performed in order to differentiate between the two pathologies. Flexor muscle or tendon injury typically demonstrates tenderness just distal to the common tendon origin from the medial epicondyle. UCL injury is noted to have tenderness posterior and distal to the common flexor tendon, along the anterior band of the UCL.
The vast majority of flexor-pronator muscle mass injuries respond well to non-operative treatment. This entails rest, anti-inflammatory medication, and physical therapy. Once pain has resolved, a gradual return to throwing may be initiated. For those patients that continue to experience medial pain despite adequate non-operative treatment, the clinician should have suspicion for other, more serious underlying pathology. When imaging and exam confirm an isolated flexor-pronator muscle mass injury, and the patient has exhausted non-operative measures, surgical side-to-side repair of the tears or re-insertion to the medial epicondyle may be performed as described by Norwood et al. [47].
Summary
Elbow pain in the overhead-throwing athlete has become more commonplace in recent years. Appropriate diagnosis and management of these patients not only requires a working knowledge of the osseous, ligamentous, nervous, and musculotendinous structures of the medial elbow but also mandates the clinician understand certain biomechanical aspects of the throwing cycle. This will assist a vigilant and thorough clinician with obtaining an accurate diagnosis early on in a patient’s symptomatology and potentially improve the chances of successful non-operative treatment.
For those athletes who ultimately require surgical intervention, future research aimed at furthering our understanding of the anatomy, biomechanics, and pathophysiology associated with overhead activities will likely lead to continued further improvements in our surgical outcomes.
Compliance with ethical standards
Conflict of interest
William H. Rossy and Luke S. Oh declare that they have no conflict of interest.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Elbow Soft Tissue Surgery
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.•.Makhni EC, Morrow ZS, Luchetti TJ, Mishra-Kalyani PS, Gualtieri AP, Lee RW, Ahmad CS. Arm pain in youth baseball players: a survey of healthy players. Am J Sports Med. 2015;43(1):41–6. [DOI] [PubMed]
- 2.Cain EL, Dugas JR, Wolf RS, Andrews AR. Elbow injuries in the throwing athletes: a current concepts review. Am J Sports Med. 2003;31(4):621–35. [DOI] [PubMed]
- 3.Morrey BF, Tanaka S, An KN. Valgus stability of the elbow: a definition of primary and secondary constraints. Clin Orthop. 1991;265:187–95. [PubMed]
- 4.Fleisig GS, Andrews JR, Dillman CJ, et al. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233–9. [DOI] [PubMed]
- 5.Callaway GH, Field LD, Deng XH, et al. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997;79:1223–31. [DOI] [PubMed]
- 6.Jobe FW, Moynes DR, Tibone JE, Perry J. An EMG analysis of the shoulder in pitching: a second report. Am J Sports Med. 1984;12:218–20. [DOI] [PubMed]
- 7.Sisto DJ, Jobe FW, Moynes DR, Antonelli DJ. An electromyographic analysis of the elbow in pitching. Am J Sports Med. 1987;15:260–3. [DOI] [PubMed]
- 8.Fleisig GS, Escamilla RF. Biomechanics of the elbow in the throwing athlete. Oper Tech Sports Med. 1996;4:62–8.
- 9.•.van den Bekerom MP, Eygendaal D. Posterior elbow problems in the overhead athlete. Sports Med Arthrosc. 2014;22(3):183–7. [DOI] [PubMed]
- 10.Werner SL, Fleisig GS, Dillman CJ, et al. Biomechanics of the elbow during baseball pitching. J Orthop Sports Phys Ther. 1993;17:274–8. [DOI] [PubMed]
- 11.•.Erickson BJ, Gupta AK, Harris JD, et al. Rate of return to pitching and performance after Tommy John surgery in Major League Baseball pitchers. Am J Sports Med. 2014;42:536–43. [DOI] [PubMed]
- 12.Petty DH, Andrews JR, Fleisig GS, Cain EL. Ulnar collateral ligament reconstruction in high school baseball players: clinical results and injury risk factors. Am J Sports Med. 2004;2004(32). [DOI] [PubMed]
- 13.•.Erickson B, Garris JD, Chalmers PN, Bach BR, Verma NN, Bush-Joseph CA, et al. Ulnar collateral ligament reconstruction: anatomy, indications, techniques, and outcomes. Sports Health. 2015;7(6):511–7. doi: 10.1177/1941738115607208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen FS, Rokito AS, Jobe FW. Medial elbow problems in the overhead-throwing athlete. J Am Acad Orthop Surg. 2001;9(2):99–113. [DOI] [PubMed]
- 15.Jobe FW, Kvitne RS. Elbow instability in the athlete. Instr Course Lect. 1991;40:17–23.
- 16.Schwab GH, Bennett JB, Woods GW, Tullos HS. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin Orthop. 1980;146:42–52. [PubMed]
- 17.Schwartz ML, al-Zahrani S, Morwessel RM, Andrews JR. Ulnar collateral ligament injury in the throwing athlete: evaluation with saline-enhanced MR arthrography. Radiology. 1995;197:297–9. [DOI] [PubMed]
- 18.Kim NR, Moon SG, Ko SM, Moon WJ, Choi JW, Park JY. MR imaging of ulnar collateral ligament injury in baseball players: value for predicting rehabilitation outcome. Eur J Radiol. 2011;80:e422–6. [DOI] [PubMed]
- 19.•.Ciccotti MG, Atanda A Jr, Nazarian LN, Dodson CC, Holmes L, Cohen SB. Stress sonography of the ulnar collateral ligament of the elbow in professional baseball pitchers: a 10-year study. Am J Sports Med. 2014;42(3):544–51. [DOI] [PMC free article] [PubMed]
- 20.Nazarian LN, McShane JM, Ciccotti MG, O’Kane PL, Harwood MI. Dynamic US of the anterior band of the ulnar collateral ligament of the elbow in asymptomatic major league baseball pitchers. Radiology. 2003;227(1):149–54. [DOI] [PubMed]
- 21.•.Hibberd EE, Brown JR, Hoffer JT. Optimal management of ulnar collateral ligament injury in baseball pitchers. Open Access J Sports Med. 2015;11(6):343–52. [DOI] [PMC free article] [PubMed]
- 22.Jobe FW, Stark H, Lombardo SJ. Reconstruction of the ulnar collateral ligament in athletes. J Bone Joint Surg Am. 1986;68:1158–63. [PubMed]
- 23.Dines JS, Elattrache NS, Conway JE, Smith W, Ahmad CS. Clinical outcomes of the DANE TJ technique to treat ulnar collateral ligament insufficiency of the elbow. Am J Sports Med. 2007;5:2039–44. [DOI] [PubMed]
- 24.Hechtman KS, Zvijac JE, Wells ME, Botto-van BA. Long-term results of ulnar collateral ligament reconstruction in throwing athletes based on a hybrid technique. Am J Sports Med. 2011;39:342–7. [DOI] [PubMed]
- 25.Jackson A, Maerz T, Koueiter DM, Andrecovich CJ, Baker KC, Anderson K. Strength of ulnar fixation in ulnar collateral ligament reconstruction: a biomechanical comparison of traditional bone tunnels to the tension-slide technique. J Should Elbow Surg. 2012;21:1674–9. [DOI] [PubMed]
- 26.Jackson TJ, Adamson GJ, Peterson A, Patton J, McGarry MG, Lee TQ. Ulnar collateral ligament reconstruction using bisuspensory fixation: a biomechanical comparison with the docking technique. Am J Sports Med. 2013;41:1158–64. [DOI] [PubMed]
- 27.Morgan RJ, Starman JS, Habet NA, et al. A biomechanical evaluation of ulnar collateral ligament reconstruction using a novel technique for ulnar-sided fixation. Am J Sports Med. 2010;38:1448–55. [DOI] [PubMed]
- 28.Rohrbough JT, Altchek DW, Hyman J, Williams 3rd RJ, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30:541–8. [DOI] [PubMed]
- 29.Thompson WH, Jobe FW, Yocum LA, Pink MM. Ulnar collateral ligament reconstruction in athletes: muscle-splitting approach without transposition of the ulnar nerve. J Should Elbow Surg. 2001;10:152–7. [DOI] [PubMed]
- 30.Vitale MA, Ahmad CS. The outcome of elbow ulnar collateral ligament reconstruction in overhead athletes: a systematic review. Am J Sports Med. 2008;36(6):1193–205. [DOI] [PubMed]
- 31.Smith GR, Altchek DW, Pagnani MJ, Keeley JR. A muscle-splitting approach to the ulnar collateral ligament of the elbow: neuroanatomy and operative technique. Am J Sports Med. 1996;24:575–80. [DOI] [PubMed]
- 32.Dodson CC, Thomas A, Dines JS, Nho SJ, Williams 3rd RJ, Altchek DW. Medial ulnar collateral ligament reconstruction of the elbow in throwing athletes. Am J Sports Med. 2006;34:1926–32. [DOI] [PubMed]
- 33.Koh JL, Schafer MF, Keuter G, Hsu JE. Ulnar collateral ligament reconstruction in elite throwing athletes. Arthroscopy. 2006;22:1187–91. [DOI] [PubMed]
- 34.Wilson FD, Andrews JR, Blackburn TA, et al. Valgus extension overload in the pitching elbow. Am J Sports Med. 1983;11:83–8. [DOI] [PubMed]
- 35.Miller CD, Savoie FH 3rd. Valgus extension injuries of the elbow in the throwing athlete. J Am Acad Orthop Surg. 1994;2:261–9. [DOI] [PubMed]
- 36.Bennett GE. Elbow and shoulder lesions of baseball players. Am J Surg. 1959;98:484–92. [DOI] [PubMed]
- 37.Field LD, Altchek DW. Evaluation of the arthroscopic valgus instability test of the elbow. Am J Sports Med. 1996;24:177–81. [DOI] [PubMed]
- 38.Andrews JR, Timmerman LA. Outcome of elbow surgery in professional baseball players. Am J Sports Med. 1995;23:407–13. [DOI] [PubMed]
- 39.Reddy AS, Kvitne RS, Yocum LA, et al. Arthroscopy of the elbow: a long-term clinical review. Arthroscopy. 2000;16:588–94. [DOI] [PubMed]
- 40.Gabel GT, Amadio PC. Reoperation for failed decompression of the ulnar nerve in the region of the elbow. J Bone Joint Surg Am. 1990;72(2):213–9. [PubMed]
- 41.Del Pizzo W, Jobe FW, Norwood L. Ulnar nerve entrapment syndrome in baseball players. Am J Sports Med. 1977;5:182–5. [DOI] [PubMed]
- 42.Childress HM. Recurrent ulnar-nerve dislocation at the elbow. Clin Orthop. 1975;108:168–73. [DOI] [PubMed]
- 43.Jobe FW, Nuber G. Throwing injuries of the elbow. Clin Sports Med. 1986;5:621–36. [PubMed]
- 44.Glousman RE. Ulnar nerve problems in the athlete’s elbow. Clin Sports Med. 1990;9:365–77. [PubMed]
- 45.Rettig AC, Ebben JR. Anterior subcutaneous transfer of the ulnar nerve in the athlete. Am J Sports Med. 1993;21:836–40. [DOI] [PubMed]
- 46.Cain EL, Andrews JR, Dugas JR, Wilk KE, McMichael CS, Walter JC 2nd, Riley RS, et al. Outcome of ulnar collateral ligament reconstruction of the elbow in 1281 athletes: results in 743 athletes with minimum 2-year follow up. Am J Sports Med. 2010;38(12):2426–34. [DOI] [PubMed]
- 47.Norwood LA, Shook JA, Andrews JR. Acute medial elbow ruptures. Am J Sports Med. 1981;9:16–9. [DOI] [PubMed]
- 48.DiGiovine NM, Jobe FW, Pink M, Perry J. An electromyographic analysis of the upper extremity in pitching. J Shoulder Elb Surg. 1992;1(1):15–25. [DOI] [PubMed]


