Abstract
Focal mediastinal F-18 FDG uptake may be from potential adenopathy requiring biopsy confirmation or benign active brown adipose tissue to be left untouched. Knowledge of this potential pitfall and precise localization with fusion PET/CT are important in preventing misinterpretation as malignancy. Our case report is important in the aspect that CT was not able to confirm the uptake as benign finding, which led to invasive biopsy and biopsy confirmed it to be a benign brown adipose tissue.
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; PET, positron emission tomography; SUV, standardized uptake value
Case Report
A 57-year-old woman was recently diagnosed with lung cancer. As part of the evaluation, PET/CT scan of the whole body was performed. It revealed high-grade uptake at the site of primary malignancy in the right lower lobe with a mean SUV of 7.8 (Fig. 1) and a 10 by 7 mm ipsilateral precarinal lymph node with mean SUV of 2.4 (not shown). In addition, it revealed a hyperactive metabolic nodular density with mean SUV of 2.4, localized anterior and to the left of the main pulmonary artery (Fig. 1-arrow). The CT portion of the PET/CT described it as soft tissue nodular density of about 11*7 cm in size and 40 house field units. The possibility of additional focus of metastatic lymphadenopathy was raised. The prior dedicated chest CT 2 weeks before PET/CT staging described it as soft tissue density, of unknown significance. The 3D PET, CT and PET/CT fusion imaging was not more helpful to further characterize the lesion in terms of its benign or malignant nature (Figure 2). The biopsy was performed shortly after the PET/CT scan and 3 months after the biopsy of primary lesion. The gross description of the lesion was described as yellow fatty tissue of 1.5 by 1.4 by 1.0 cm in size and final diagnosis was “pericardial adipose tissue with no evidence of malignancy” (Fig. 3). The biopsy of the primary lesion of the lung 3 months before showed a large cell (non-small cell) type cancer (Fig. 4). The CD56 (Fig. 5) and synaptophysin antibody markers (Fig. 6) showed the primary lung cancer to be of neuroendocrine differentiation. Patient underwent radiation and chemotherapy treatment. Subsequent follow-up with PET/CT 6 months later (Fig. 7) showed marked improvement in the primary lesion showing photopenia with minimal rim of hypermetabolic activity and no new lesions. The contralateral pericardial soft tissue nodular density was unchanged in appearance and showed a mild decrease in SUV from 2.4 to 2.0.
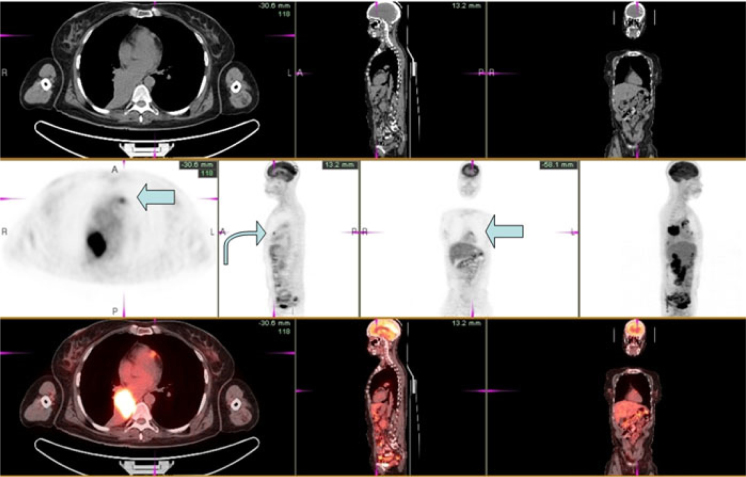
Figure 1.
57-year-old woman with lung cancer. The PET/CT image showing hypermetabolic activity in the primary malignancy of the right lung (Arrows) and hypermetabolic activity in the pericardial region (Arrowhead), suspicion of metastatic lymphadenopathy was raised.
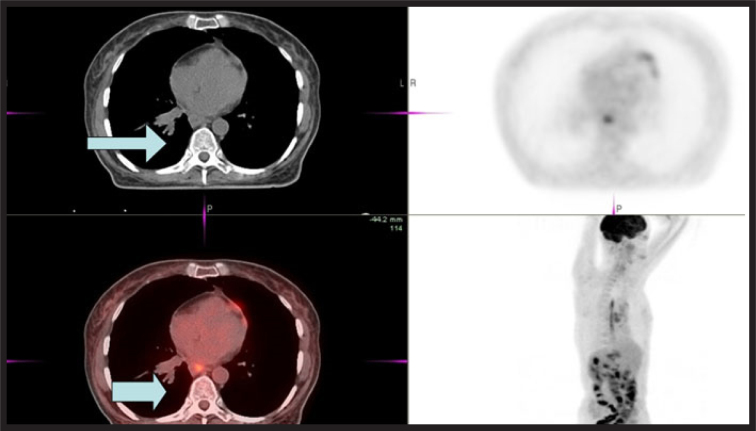
Figure 2.
57-year-old woman with lung cancer. The 3D views of the coronal, sagittal and transaxial views of the CT, PET and fused PET/CT showing the pericardial uptake.
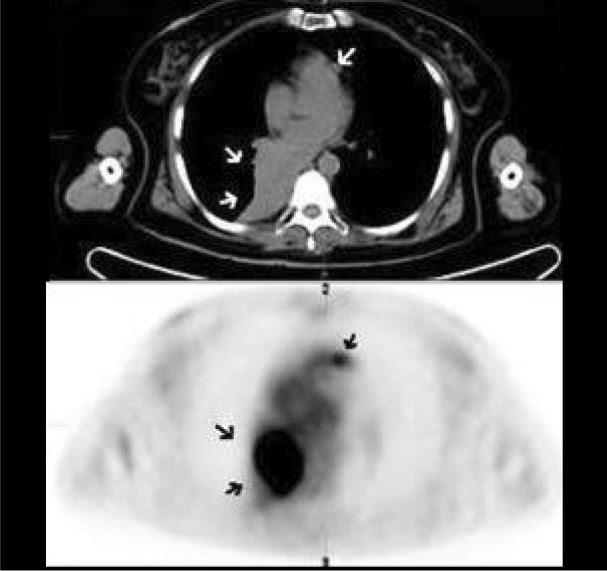
Figure 3.
57-year-old woman with lung cancer. Histopathology of pericardial tissue shows it to be adipose tissue.
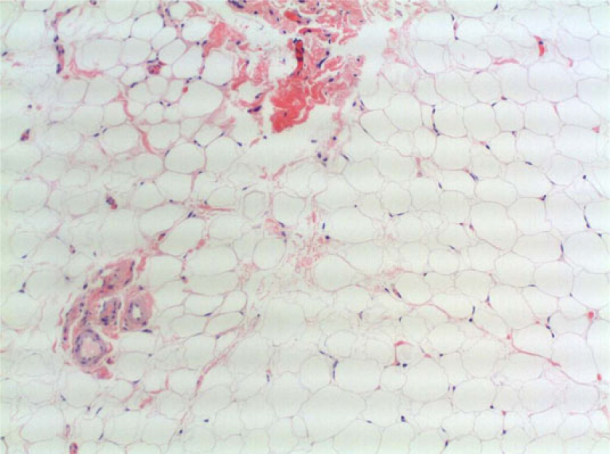
Figure 4.
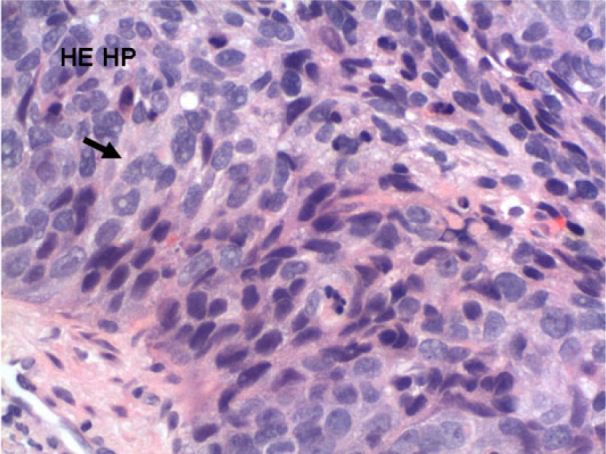
57-year-old woman with lung cancer. Histopathologic examination of primary malignancy reveals large cell type lung cancer.
Figure 5.
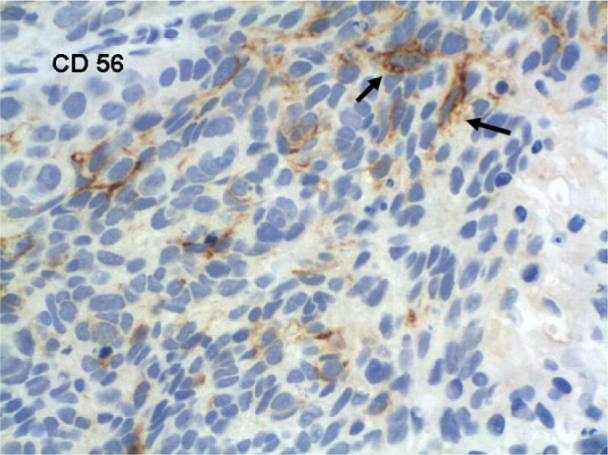
57-year-old woman with lung cancer. The CD56 antibody showed the primary malignancy to be of neuroendocrine origin.
Figure 6.
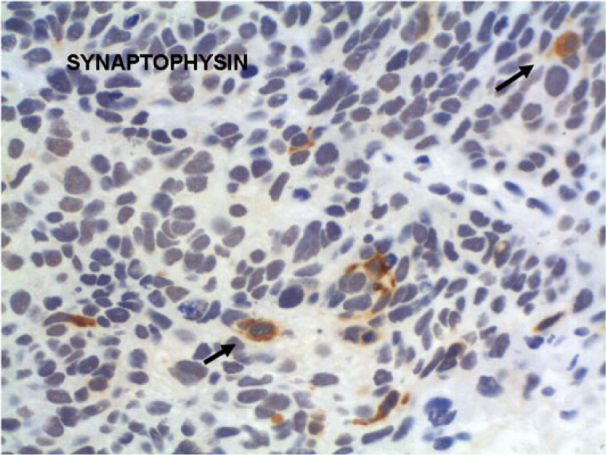
57-year-old woman with lung cancer. Synaptophysin stain showed the primary malignancy to be of neuroendocrine origin.
Figure 7.
57-year-old woman with lung cancer. Six month follow-up PET/CT showing marked improvement in the primary lesion (arrow) and non-significant decrease in soft tissue pericardial density, when compared to the prior PET scan.
Discussion
The focal mediastinal uptake in the FDG/PET imaging has been described, which on CT confirm the activity to be either in the brown adipose tissue or in the lymph node (1, 2, 3, 4). PET with CT can usually identify suspicious lymph nodes that require biopsy (5). Hypermetabolic brown fat can be localized to the mediastinum and manifests as focal increased FDG uptake. Knowledge of this potential pitfall and precise localization with fusion PET/CT are important in preventing misinterpretation as malignancy (2). In most of the cases, the location, symmetry and shape of the FDG uptake can differentiate benign tissue from malignancy. Typical supraclavicular adipose tissue is bilateral, curvilinear, symmetric and elongated; the appearance is rarely confused with malignancy. The mediastinal adipose tissue uptake can be seen in the following areas: azygous vein, brachiocephalic artery, interatrial septum, hemiazygous vein, azygoesophageal recess, pericardial, prevascular and paratracheal adipose tissue. The benign FDG uptake in mediastinal adipose tissue is usually focal and spherical (2). Positive mediastinal FDG uptake is considered abnormal, when it is substantially larger than mediastinal blood pool activity. However, the mediastinal F-18 FDG uptake is less specific and could be seen in many different disease entities, which includes infection, inflammation, breathing motion artifact and atrial appendage radiotracer. These entities may also simulate mediastinal primary or secondary malignancy. Due to the imperfect specificity of positron emission tomography, biopsies recommended for all PET positive mediastinal lymph nodes in order to confirm or rule out metastasis (6). Though, there are no SUV cut offs for malignancy and furthermore there is a lot of SUV variability based on different acquisitions and timing of scan relative to dose, the SUV ratio can distinguish benign vs. malignant focus. The ratio of the maximum SUV of the mediastinal (N2) lymph node to the maximum SUV of the primary tumor in patients with non small-cell lung cancer predicts mediastinal nodal pathology. When the ratio is 0.56 or greater, there is a 94% chance that the node is malignant. In our case, the ratio was 0.30(again, the ratio may take into account the different techniques used at different centers (7)). In non-small cell lung cancer, PET may reduce the necessity for mediastinoscopy when the primary lesion standardized uptake value is less than 2.5 and the mediastinum is PET negative (8).
In the case present, we were unable to distinguish normal brown fat from the metastatic lymph node on CT. As it is highly unusual to have contralateral pericardial mediastinal node activity without intervening ipsilateral nodal activity, the involvement of the ipsilateral precarinal lymph node raised the suspicion of malignancy in the contralateral pericardial hypermetabolic tissue. The SUV ratio of the suspected lymph node to the primary malignancy may have potentially suggested benign nature of the lymph node. Further evaluation with biopsy confirmed it as brown fat.
Footnotes
Published: June 13, 2008
References
- 1.Kuester LB, Fischman AJ, Fan CM, Halpern EF, Aquino SL. Lipomatous hypertrophy of the inteatrial septum: Prevalance and features on fusion 18F fluorodeoxyglucose positron emission tomography/CT. Chest. 2005; Dec;128(6):3888–3893. doi: 10.1378/chest.128.6.3888. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Truong MT, Erasmus JJ, Munden RF. Focal FDG uptake in mediastinal brown fat mimicking malignancy: a potential pitfall resolved on PET/CT. AJR. 2004; Oct;183(4):1127–1132. doi: 10.2214/ajr.183.4.1831127. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Yeung HW, Grewal RK, Gonen M, Schoder H, Larson SM. Patterns of 18F-FDG uptake in adipose tissue and muscle: a potential source of false-positives for PET. J Nucl Med. 2003 Nov;44(11):1789–1796. [PubMed] [PubMed] [Google Scholar]
- 4.Kelly RF, Tran T, Holmstrom A, Murar J, Segurola RJ. Accuracy and cost effectiveness of [18F]-2-fluoro-deoxy-D-glucose-positron emission tomography scan in potentially resectable non-small cell lung cancer. Chest. 2004 Apr;125(4):1413–1423. doi: 10.1378/chest.125.4.1413. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Eloubeidi MA, Cerfolio RJ, Chen VK, Desmond R, Syed S, Ojha B. Endoscopic Ultrasound-guided fine needle aspiration of mediastinal lymph node in patients with suspected lung cancer after positron emission tomography and computed tomography scans. Ann Thorac Surg. 2005 Jan;79(1):263–268. doi: 10.1016/j.athoracsur.2004.06.089. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Annema JT, Hoekstra OS, Smit EF, Veseliç M, Versteegh MI, Rabe KF. Towards a minimally invasive staging strategy in NSCLC: analysis of PET positive mediastinal lesions by EUS-FNA. Lung Cancer. 2004 Apr;44(1):53–60. doi: 10.1016/j.lungcan.2003.10.013. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Cerfolio RJ, Bryant AS. Ratio of the maximum standardized uptake value on FDG-PET of the mediastinal (N2) lymph nodes to the primary tumor may be a universal predictor of nodal malignancy in patients with non-small-cell lung cancer. Ann Thorac Surg. 2007 May;83(5):1826–1829. doi: 10.1016/j.athoracsur.2006.12.034. [PubMed] discussion 1829-30. [DOI] [PubMed] [Google Scholar]
- 8.Kernstine KH, Mclaughlin KA, Menda Y, Rossi NP, Kahn DJ, Bushnell DL, Graham MM, Brown CK, Madsen MT. Can FDG-PET reduce the need for mediastinoscopy in potentially resectable non-small cell lung cancer? Ann Thorac Surg. 2002 Feb;73(2):394–401. doi: 10.1016/s0003-4975(01)03432-4. [PubMed] discussion 401-402. [DOI] [PubMed] [Google Scholar]