Abstract
Ascites is found in a variety of conditions, both acute and chronic, and computed tomography (CT) is usually successful in detecting its presence. We reviewed the CT images from a three-month window of patients in order to evaluate the prevalence and utility of a new radiographic sign for diagnosing ascites.
Abbreviations: CT, computed tomography
Introduction
Ascites is a pathologic collection of fluid within the abdominal cavity that is most often associated with chronic liver disease [1]. Ascites can be an important finding in several clinical scenarios, especially trauma and the workup of fever of unknown origin. A proper history and physical examination plays an important part in the diagnosis of ascites. Nevertheless, the accuracy of physical exam findings may vary depending on the technique and expertise of the examiner, the quantity of fluid present and such clinical factors as obesity that hinder fluid detection, thereby influencing the exam's sensitivity and specificity [2]. Consequently, an imaging test can be an important adjunct in diagnosing this pathologic condition and associated findings. While ultrasound remains a non-ionizing and inexpensive modality for detecting fluid collections within the abdominal cavity, computed tomography (CT) scans are also effective in detecting ascites and may have some advantages for areas blind to ultrasound due to overlying bowel gas. This study proposes the utility of a new radiographic sign, we have named the “Concave margin sign” for descriptive purposes, as it has been found useful to radiologists in Body CT at our institution.
Materials and Methods
Abdominal CT scans (with and without contrast) of 60 patients with “ascites” found in the Radiology Report Impression from January 2006 through March 2006 were reviewed retrospectively to determine if a concave margin sign was present. 18 patients had >1 CT scan showing ascites, and consequently, the overall number of CT scans reviewed totaled 83.
Free fluid forms concave margins, conforming to loops of bowel and other round structures with peaks at the apices of the margins (Fig. 1). Using this definition of the sign, the presence or absence of the concave margin sign in these patients with CT-confirmed ascites was recorded.
Figure 1.
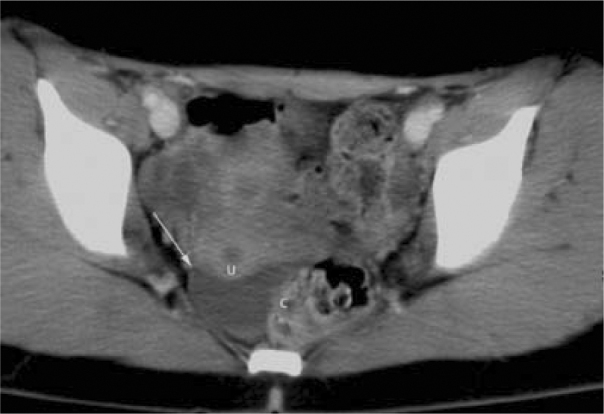
CT image shows free fluid forming a concave margin with the uterus (U) and sigmoid colon (C) and the peaked apex (arrow).
The amount of ascites observed on the images was categorized as trace (4 studies, 4.8%), mild/small volume (27, 32.5%), moderate (30, 36.1%), or marked/large volume (17, 20.5%). There were 5 studies (6.0%) in which the fluid was not so quantified but described in other terms such as scattered pockets, loculated, or perihepatic or perisplenic.
Results
Of the 83 total scans showing peritoneal fluid, 80 (96.4%) exhibited the concave margin sign (Table 1). From the 3 studies not demonstrating the concave margin sign, two were from studies showing only trace amount of ascites while the other study only revealed perihepatic fluid, which does form a concave margin with the liver, but not with bowel. Smaller volumes of fluid were found easily when looking for its concave margin against bowel loops. The sign was even more useful in scans without oral or intravenous contrast where peritoneal free fluid and fluid within the unenhanced bowel can appear similar on imaging. When there was a large amount of fluid, the sign added little to the “obvious” finding of fluid.
Table 1.
Prevalence of the concave margin sign in 83 cases
| Descriptive amount of ascites | Number of cases (% of total) | Prevalence of sign in each category |
|---|---|---|
| Trace | 4 (4.8%) | 50% |
| Mild/small volume | 27 (32.5%) | 100% |
| Moderate | 30 (36.1%) | 100% |
| Marked/large volume | 17 (20.5%) | 100% |
| Other | 5 (6.0%) | 80% |
| TOTALS | 83 (100%) | 96.4% |
Discussion
Ascites can become symptomatic in itself for the patient but is also a marker for many other conditions. While it can be seen in patients with pancreatitis, renal failure, or such systemic illnesses as heart failure and severe hypoalbuminemia, it is most commonly associated with cirrhosis, especially from alcoholism, and has even been proposed as an indication for liver transplantation [1, 3]. Accordingly, detecting ascitic fluid on imaging serves a significant role in the management of patients with such diseases [4]. In trauma cases, it can be the critical finding of hemoperitoneum, sometimes leading to the diagnosis of mesenteric or bowel laceration. Also, many patients are examined for the signs of fever of unknown origin and the finding of ascites could lead to the diagnosis of spontaneous bacterial peritonitis
Ultrasonography provides a quick, nonionizing, portable, and economic tool in detecting peritoneal fluid [5]. But with the increasing use of body CT scans for many clinical conditions, ascites is also seen on these images. The use of the concave margin sign in distinguishing such fluid within the abdomen appears to be effective, especially when smaller volumes are present.
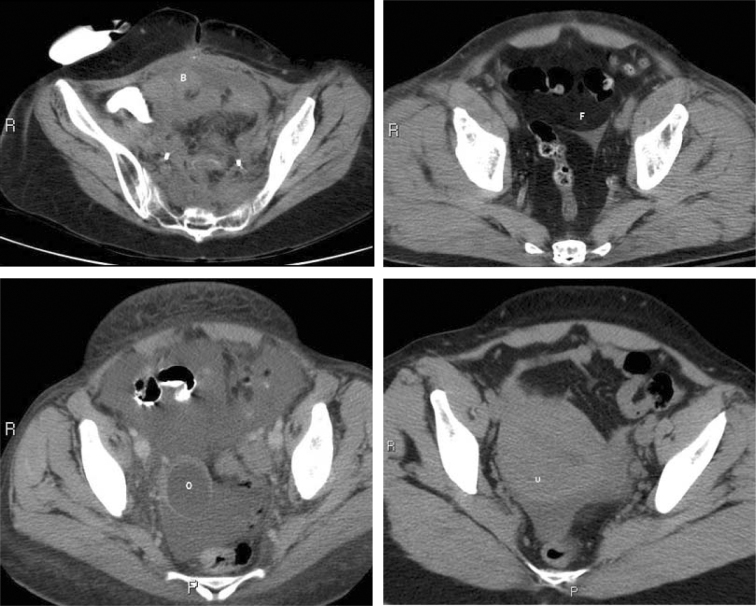
Free fluid in the peritoneum and in unopacified bowel often has a similar density at CT. Free fluid will forms concave margins, conforming to loops of bowel with peaks at the apices of the margins. Fluid-filled loops of bowel or ovaries have convex margins without peaks, and these can be differentiated from free fluid if the concave margin sign is used (Fig. 2).
Figure 2.
Concave margin sign demonstrated in CT scans of four different patients with unopacified bowel (B), mesenteric fat (F), ovary (O) and the uterus (U).
Of note, in this retrospective study it was observed that ascites also forms a concave margin against convex, rounded structures such as the ovaries or uterus (Fig. 2). In very trace amounts of fluid, however, the utility of the concave margin sign may be limited by the small amount of interface with bowel or other intraabdominal structures.
In summary, the concave margin sign was found in an overwhelming number of cases of ascites in this case series and could lead to a more confident diagnosis of peritoneal fluid.
Footnotes
Published: July 8, 2008
References
- 1.Runyon BA. Care of patients with ascites. New England Journal of Medicine. 1994 Feb 3;330(5):337–342. doi: 10.1056/NEJM199402033300508. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Cattau EL, Jr, Benjamin SB, Knuff TE, Castell DO. The accuracy of the physical examination in the diagnosis of suspected ascites. JAMA. 1982 Feb 26;247(8):1164–1166. [PubMed] [PubMed] [Google Scholar]
- 3.Runyon BA. Management of adult patients with ascites caused by cirrhosis. Hepatology. 1998 Jan;27(1):264–272. doi: 10.1002/hep.510270139. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Moore KP, Wong F, Gines P, Bernardi M, Ochs A, Salerno F, Angeli P, Porayko M, Moreau R, Garcia-Tsao G, Jimenez W, Planas R, Arroyo V. The management of ascites in cirrhosis: report on the consensus conference of the International Ascites Club. Hepatology. 2003 Jul;38(1):258–266. doi: 10.1053/jhep.2003.50315. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.Goldberg BB, Goodman GA, Clearfield HR. Evaluation of ascites by ultrasound. Radiology. 1970 Jul;96(1):15–22. doi: 10.1148/96.1.15. [PubMed] [DOI] [PubMed] [Google Scholar]