1. Introduction
Depression in the postpartum period is a common and vexing problem, affecting up to 20% of postpartum women in the U.S. (Wisner et al., 2013). It results in difficulty with infant care and other responsibilities, poor functioning within the primary relationship at a time when it is under the stress of a newborn’s arrival, and difficulty bonding with the child and establishing breastfeeding in the critical early days. There is abundant evidence for impaired infant care by depressed mothers, including undesirable practices with respect to feeding, sleep, and safety, and reduced frequency of well-child visits and vaccinations (reviewed in Field, 2010). Indeed, suicide is a leading cause of maternal death in the postpartum period (Oates and Cantwell, 2011). Furthermore, extended maternal depression may have lasting negative effects on the child’s development (see Brand and Brennan, 2009 for review).
Postpartum depression (PPD) strikes at a time when caregiver responsibilities make it difficult for new mothers to attend frequent treatment sessions and attend to regular sleep and self-care responsibilities. Thus it can often go undetected and untreated for extended periods of time (Dennis and Chung-Lee, 2006).
Antenatal prediction might offer women the opportunity to initiate prophylactic treatment and support; however, PPD is difficult to predict. At present, previously proposed psychosocially based predictive algorithms for PPD have been insufficiently potent for clinical utility (Austin and Lumley, 2003; Milgrom et al., 2008); and efforts to develop biologically based predictive tests for PPD (Guintivano et al., 2013; Mehta et al., 2014) and have focused solely on women with existing mood disorder histories, who constitute a minority of all women with PPD. In general, clinicians treating antenatal women have been advised to focus on history of mood disorder for risk assessment (O’Hara and Gorman, 2004). While risk for PPD is elevated in women with histories of mood disorders, in several prospective samples a majority of women with depression onset in the postpartum period had no prior history of mood disorder (Banti et al., 2011; Dietz et al., 2007). This suggests that in order to have an appreciable clinical effect, efforts to predict PPD should encompass women both with and without history of mood disorder.
Premorbid personality characteristics have been hypothesized to contribute to susceptibility to PPD, and could potentially serve as clinical predictors in combination with known risk factors such as psychosocial instability and prior history of mood episodes. Several lines of investigation have examined the relationships of particular maternal personality traits to the development of PPD.
One well-documented personality characteristic that has been associated with PPD is insecure attachment style (Bifulco et al., 2004; McMahon et al., 2005; Meredith and Noller, 2003; Monk et al., 2008; Simpson et al., 2003; Rholes et al., 2011). Insecure attachment is a concept first articulated by John Bowlby in his development of attachment theory (Bowlby, 1988), and insecure attachment style in adults is thought to be based to a significant degree on suboptimal experiences with early caregiving (Carlson, 1998; Sroufe, 2005; Simard et al., 2011). Subcategories of insecure attachment styles vary between measurement instruments, and include divisions such as anxious versus avoidant, ambivalent versus avoidant, and preoccupied versus fearful versus dismissing (Ravitz et al., 2010). While some authors have found greater effects on PPD of avoidant over anxious (Bifulco et al., 2004), ambivalent over avoidant (Simpson et al., 2003), or preoccupied over fearful and dismissing styles (Meredith et al., 2003), other groups have found that all insecure subtypes increase risk for PPD without significant differences between them (Monk et al., 2008; Rholes et al., 2011).
Some investigators have conceptualized the transition to parenthood as a generalized life stressor that activates attachment representations (Bifulco et al., 2004; Meredith and Noller, 2003; Simpson et al., 2003). Others have hypothesized that pregnancy and childbirth specifically focus the mother’s attention on attachment concerns (Monk et al., 2008). When the activation of attachment schemas carries negative valence, as in women with pre-existing insecure attachment styles, this is associated with negative mood. We lean toward the latter interpretation, and further hypothesize that an individual’s own early experiences with caregivers lay down a schema for parenting and interpersonal attachment that is reactivated at the onset of parenthood. Women whose early experiences were suboptimal or deficient may confront lacunae in their parenting schemas that result in a crisis when faced with the responsibility of providing care of a type that they themselves did not experience, or experienced only incompletely.
Dysfunctional cognitions have also been associated with PPD (Church et al., 2005; Phillips et al., 2010; Grazioli and Terry, 2000; Warner et al., 1997). These authors hypothesized that, according to cognitive theories of depression (Beck, 1967), negative cognitive schemata (both general and maternal-specific) act as a perceptual filter for external events, are represented as dysfunctional attitudes and are associated with depressed mood.
A third line of inquiry has pursued the relationship of neuroticism and interpersonal sensitivity to the manifestation of PPD (Boyce et al., 1991; Boyce et al., 2001; Dennis and Boyce, 2004; Verkerk et al., 2005). This model also views these personality traits as representing increased vulnerability to external stressors (Boyce et al., 1991), producing a diathesis for depressed mood in the context of the stressor of new parenthood.
Notably, there is a strong possibility that these purportedly distinct personality domains may show significant degrees of overlap in practice. However, to our knowledge there have been no attempts to assess the degree to which these distinct constructs represent independent risk factors for PPD, or to quantify the relative magnitudes of the risks they confer.
Additionally, many of the studies in this area have been cross-sectional in nature, and those that are prospective in design have typically included only two or three assessment points. Because early infant development is rapid and household dynamics are often radically and repeatedly reorganized in the early months following childbirth, we wished to perform a more nuanced temporal assessment of the trajectory of maternal mood in this period.
The present study was intended to explore the relative potency of antenatal measures of each of the above personality factors as predictors of depressive symptoms postpartum, with assessments at monthly intervals in the six months following delivery.
2. Study hypotheses
The first study aim was to determine the relative magnitude of the contributions of personality traits including attachment style, neuroticism/interpersonal sensitivity, and dysfunctional/negative attitudes to the development of postpartum depressive symptoms. We hypothesized that maternal attachment insecurity would have the contribution of greatest relative magnitude among the traits studied.
The second study aim was to examine any overlap or multicollinearity between measures. Our hypothesis was that while all three personality traits tested would likely have predictive value for postpartum depressive symptoms, multicollinearity between measures would account for a significant portion of this predictive value, suggesting an underlying common dimension that could be largely responsible for the postpartum depressive diathesis.
The third study aim was to examine the trajectory of depressive symptoms over the first six postpartum months, and to determine whether key personality traits identified in Aims 1 and 2 moderated the shape of this trajectory. Based on our conception of the task of new motherhood as presenting a crisis to the insecurely attached individual, we hypothesized that the greatest negative effects on mood of insecure attachment style would be found in the early postpartum period.
3. Methods
3.1. Study sample
The study was approved by the Stanford University Institutional Review Board for Human Subjects Research, and all study participants completed informed consent prior to study participation. Participants consisted of a convenience sample of 108 healthy pregnant women recruited sequentially from local obstetric clinics, community postings, and the Stanford Women’s Wellness psychiatric clinic, between September 2011 and September 2014. Inclusion criteria were age at least 18, uncomplicated singleton pregnancy, and ability to complete the interview and self-report measures in English. Exclusion criteria were multiple or highly medically complicated pregnancy, or insufficient English to participate. Women in psychopharmacological treatment during pregnancy were not excluded. However, only seven of the women in the study were so treated, and psychopharmacological treatment in pregnancy did not have any significant relationship with postpartum EPDS scores. Demographic characteristics of the sample are listed in Table 1.
Table 1.
Characteristics of the study sample.
| Age | Mean: 32.2 ± 4.8 years | |
|---|---|---|
| Marital status | Married | 99 (92.5%) |
| Unmarried | 8 (7.5%) | |
| Parity | Primiparous | 63 (58.9%) |
| Multiparous | 44 (41.1%) | |
| Employment | Employed | 69 (64.5%) |
| Not employed | 38 (35.5%) | |
| Education | No college degree | 9 (8.4%) |
| Associate’s degree | 13 (12.1%) | |
| Four-year degree | 23 (21.5%) | |
| Graduate schooling |
62 (57.9%) | |
| History of major mood disorder | No | 73 (68.2%) |
| Yes | 34 (31.8%) | |
| Psychotropic medication taken in pregnancy | No | 100 (93.5%) |
| Yes | 7 (6.5%) | |
| Postnatal EPDS ≥ 12 within 2 months* of birth | No | 81 (77.1%) |
| Yes | 24 (22.9%) | |
| Postnatal EPDS ≥ 10 within 2 months of birth | No | 70 (66.7%) |
| Yes | 35 (33.3%) | |
| EPDS at 1 month postpartum | Mean: 7.03 ± 4.52 Median: 6 |
|
Sum = 105 because one participant returned only surveys beyond two months.
3.2. Study procedures
Participants completed an initial interview in the third trimester of pregnancy (mean 32.8 weeks). At monthly intervals for six months after delivery, participants completed follow-up surveys via the online tool SurveyMonkey. Participants who did not complete surveys received e-mail reminders and, if necessary, telephone prompts. At intake, participants completed an initial interview comprised of the following measures.
3.3. Assessment tools
Assessment of Psychiatric History: Participants completed the Optional Module of the Structured Clinical Interview for DSM Disorders (SCID, First et al., 2012), a screen for psychiatric history, as well as Part A of the full SCID to clarify their mood disorder histories. The SCID sections were administered by trained clinicians (TKR and JG) who had undergone SCID training and performed three observed SCIDs.
Edinburgh Postnatal Depression scale (EPDS, Cox et al., 1987): This ten-item measure is a widely used and validated screening tool for ante- and postnatal depression, with good internal consistency (Cronbach alpha of 0.87) and moderate to good reliability. The EPDS was included because it is the most widely studied and broadly accepted tool for the assessment of depressive symptoms in postnatal women. It has been suggested that as a screening tool for PPD, the EPDS has rather greater sensitivity but lesser specificity than other measures (Boyd et al., 2005).
Center for Epidemiologic Studies Depression scale (CESD, Radloff, 1977). This twenty-item measure of depressive symptoms intended for the general population has been widely used and validated in large samples (Ross and Mirowsky, 1984), and also has good internal consistency (Cronbach alpha of 0.85) and moderate reliability. The CESD was included in addition to the EPDS because it contains items that address feelings of worthlessness and the quality of relationships with others, aspects of depression which are not measured by the EPDS, and because it has been reported as having greater specificity but lesser sensitivity with respect to the EPDS in the detection of PPD (Boyd et al., 2005).
Attachment Style Questionnaire (ASQ, Feeney et al., 1994). This forty-item measure of attachment insecurity explores the individual’s attitudes towards relationships with others in general; it is not limited to a specific relationship type such as a romantic partnership. It has been validated by demonstrating patterns of association with other measures of adult attachment (Stein et al., 2002). It has been used previously in pregnant women (Alexander et al., 2001) and in the study of postpartum depression (McMahon et al., 2005). The scale is scored as results on five subscales: Confidence, Need for Approval, Relationships as Secondary, Discomfort with Closeness, and Preoccupation with Relationships. For the purposes of this paper we computed an adjusted total score in which the Confidence score was subtracted from the sum of the scores of the four other subscales.
Dysfunctional Attitude Scale (DAS, Power et al., 1994). This scale measures absolutist values that are associated with depression. It has good internal consistency and test–test reliability (Power et al., 1995), and has been used in previous investigations of cognitive style in women with PPD (Church et al. 2005, Jones et al. 2010, Phillips et al. 2010).
Vulnerable Personality Style Questionnaire (VPSQ, Boyce et al., 2001; Dennis and Boyce, 2004). This nine-item measure was developed specifically for the purpose of predicting postnatal depression. Cronbach’s alpha is 0.62 (Boyce et al., 2001). Construct validity has been confirmed against self-esteem and perceived stress (Dennis and Boyce, 2004). Retest reliability has not been assessed, as validation studies were performed in a cross-sectional manner on postnatal samples. To our knowledge a confirmatory prospectively designed study has not been carried out.
Follow-up assessments administered at monthly intervals for six months postpartum consisted of repeat administrations of the EPDS and CESD. Other measures administered to this sample for concurrent studies on stress, coping, and other aspects of reduced functioning in the postpartum period were not included in this analysis (our unpublished data). Women who scored 12 or above on the EPDS were contacted by telephone and offered referral to psychiatric care and to community support resources. (Referral to treatment was found to have no significant effect on EPDS scores at six months postpartum by one-way ANOVA when controlling for EPDS score at 1 month postpartum.)
3.4. Data quality
One woman was lost to follow-up and was not included in the present analysis, resulting in a total N of 107. Rate of survey return was 83.7% overall among women who returned at least one survey (i.e., not including the subject who returned no follow-up surveys). Individual missing items within a measure (< 1% of total) were imputed as an average of the remainder of the items in that measure.
3.5. Statistical analysis
Statistical analysis was carried out using SPSS Statistics version 22 for Windows. In order to facilitate comparisons among independent variables of interest, it was necessary to express dependent variables as single values. Additionally we wished to take into account both the severity and duration of depressive symptoms in the outcome measures, and to reduce random error associated with fluctuations in mood. Thus, depressive scores were averaged over multiple time points. Pearson correlations were initially applied to assess potential relationships among variables of interest. Individual linear regressions were then conducted using age, marital status, parity, whether the pregnancy was planned, education, employment status, ethnicity, history of mood disorder, antenatal depressive symptoms, and mother’s evaluation of her relationship with her partner (single item scaled 0–4) as the independent variables and the EPDS or CESD, averaged over either three or six postpartum time points, as the dependent variables. ASQ score was then added into this analysis in order to gauge the magnitude of its contribution to the model. In order to assess the relative contribution of antenatal ASQ score to postnatal depressive symptoms at each time point, Pearson correlations between antenatal ASQ and postnatal EPDS or CESD at each postpartum month were calculated and plotted on a graph.
4. Results
4.1. All three personality measures have predictive value for postnatal depressive symptoms
In order to obtain initial estimates of the magnitude of the predictive value of included personality inventories for postnatal depressive symptoms, Pearson correlations were computed between antenatal scores on neuroticism/interpersonal sensitivity (VPSQ), negative cognitive attitudes (DAS-24), and attachment style (ASQ) and mean depression symptom scores (EPDS and CESD), averaged over either three or six postnatal surveys.
In unadjusted comparisons, all three personality inventories examined had significant correlations with postnatal depressive symptoms (p < 0.01 for all, see Table 2). Bonferroni correction for three outcomes yielded an equivalent pairwise significance criterion of 0.0167, by which these results were still significant. Pearson correlations with postnatal depressive symptoms were strongest for the ASQ and weakest for the DAS-24.
Table 2.
Antenatally measured psychiatric and personality factors correlate with postnatal depressive symptoms. Personality factors are stronger predictors of postnatal depression symptom score than history of mood disorder, and are comparable in predictive value to the antenatal depression score. ASQ is the strongest predictor of the three personality dimensions tested. For purposes of comparison, correlations between current best clinical predictors (history of mood disorder and antenatal depression) and depression symptom scores are also shown. The predictive value of the ASQ for mean postpartum depression scores is similar to that of mean ante-partum depression scores (both EPDS and CESD). Pearson Correlations.
| Probed personality traits |
Comparison with existing predictors |
|||||
|---|---|---|---|---|---|---|
| VPSQ | DAS24 | ASQ | Mood dis- order hx |
Intake EPDS |
Intake CESD |
|
| EPDS mean 3m |
0.474*** | 0.474*** | 0.516*** | 0.321*** | 0.553*** | |
| CESD mean 3m |
0.378*** | 0.479*** | 0.558*** | 0.346*** | 0.561*** | |
| EPDS mean 6m |
0.425*** | 0.409*** | 0.435*** | 0.350*** | 0.498*** | |
| CESD mean 6m |
0.341*** | 0.440*** | 0.507*** | 0.372*** | 0.501*** | |
p ≤ 0.01;
p ≤ 0.05
p ≤ 0.001;
In order to compare the contribution of personality traits to that of established risk factors for PPD, Pearson correlations with postnatal depression scores were also computed for history of mood disorder and antenatal depression scores. Notably, each of the three personality inventories was more strongly predictive of postnatal depressive symptoms than was mood disorder history. Correlations between antenatal VPSQ and DAS-24 scores were generally weaker than correlations between antenatal depression scores and postnatal depression scores. In contrast, the predictive capacity of antenatal ASQ scores for postnatal depression scores was quite similar to the predictive capacity of antenatal measures of depression (Table 2). Differences between correlations that reached significance by Steiger’s z-test included: ASQ versus history of mood disorder for the outcome of mean EPDS in the first three months (z=1.97); ASQ versus history of mood disorder for the outcome of mean CESD in the first three months (z= 2.17); and ASQ versus VPSQ for the outcome of mean CESD in the first three months (z= 2.08).
These results indicate that, in this study sample, personality factors (in particular the ASQ) were stronger predictors of postnatal depression scores than history of mood disorder, and were approximately comparable in predictive value to antenatal depression scores.
4.2. Antenatal ASQ retains significance when intercorrelations between personality traits are controlled
In order to account for intercorrelations between scores on each of the three personality measures, multiple linear regressions containing all three personality measures as independent variables, with 3-month and 6-month mean depressive scores as dependent variables, were performed.
Using EPDS as the dependent variable, both the VPSQ and the ASQ were significant predictors of postnatal depressive symptoms over both 3-month and 6-month time periods. (For 3-month EPDS: VPSQ (Beta=0.244, p=0.01); ASQ (Beta=0.290, p < 0.01). For 6-month EPDS: VPSQ (Beta=0.234, p < 0.05); ASQ (Beta=0.226, p < 0.05).) Significance for the three-month averages, but not the six-month averages, survived Bonferroni correction. DAS-24 did not correlate significantly with any measure of postnatal depressive symptoms in this analysis. Using CESD as the dependent variable, only the ASQ was a significant predictor of depressive symptoms over both 3-month (Beta=0.391, p < 0.001) and 6-month (Beta=0.352, p=0.001) time periods, and survived Bonferroni correction in both cases. Multicollinearity was not evident, with VIFs under 2 for all cases.
Because the independent predictive value of the ASQ was robust across both depression scales used, the remainder of the analysis centered on this predictor.
4.3. Antenatal ASQ is a potent predictor of postnatal depressive symptoms when covariates are accounted for
In order to determine whether the predictive value of the ASQ remained relevant when potential psychiatric and socio-demographic confounders were accounted for, a set of multiple regressions that included age, marital status, parity, whether the pregnancy was planned, education, employment status, ethnicity, and mother’s evaluation of her relationship with her partner was performed, with dependent variables corresponding to the 3-month and 6-month means of the EPDS and CESD measures of depression. None of these factors were significant determinants of postpartum depressive symptoms in this model (data not shown).
The additional factors of mood disorder history, antenatal depression score, and ASQ score were then added to the model in a stepwise fashion. Mood disorder history and antenatal depression were highly significant predictors of postpartum depressive symptoms, consistent with existing literature (O’Hara and Swain, 1996). However the addition of ASQ score to the model reduced the betas for these factors by 25–50%, indicating that a significant proportion of the variance ascribed to psychiatric history factors could in fact be accounted for by attachment insecurity (Table 3). (Outcomes using CESD as the dependent variable were similar, but for simplicity are not shown.) These results indicate that antenatal ASQ outperforms history of mood disorder as well as antenatal depression as a predictor of depression within three months postpartum in our study sample.
Table 3.
Attachment insecurity is a more powerful predictor of depressive symptoms in the early postnatal period than either mood disorder history or antenatal depression. When ASQ is entered into a two-step multiple regression after history of mood disorder and depression at intake, beta values for these variables are reduced by 25–50%. This proportion is greater over three months than over six months postpartum. The beta value for ASQ in the three-month regression exceeds the beta values for mood disorder history and intake EPDS, and R2 values for both models are improved with the addition of ASQ. Nonsignificant covariates included in these models but not shown in the table include age, marital status, parity, planned pregnancy, education, employment, ethnicity, and rating of partner relationship, none of which made significant contributions to the model. Results for CESD outcome are similar (not shown).
| Unstandardized coefficients | Standardized coefficients | t | P | F | R2 | Adj R2 | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | Beta | ||||||||
| Dependent: EPDS mean over 3 months pp | ||||||||||
| Step 1 | (Constant) | 2.236 | 3.301 | 0.677 | NS | 3.286 | 0.274 | 0.191 | ||
| Mood disorder history | 0.992 | 0.649 | 0.145 | 1.529 | NS | |||||
| Intake EPDS | 0.397 | 0.098 | 0.432 | 4.071 | < 0.001 | |||||
| Step 2 | (Constant) | −0.784 | 3.345 | −0.234 | NS | 3.975 | 0.337 | 0.252 | ||
| Mood Disorder History | 0.524 | 0.645 | 0.077 | 0.813 | NS | |||||
| Intake EPDS | 0.256 | 0.106 | 0.279 | 2.420 | 0.018 | |||||
| ASQ | 0.056 | 0.020 | 0.326 | 2.856 | 0.005 | |||||
| Dependent: EPDS mean over 6 months pp | ||||||||||
| Step 1 | (Constant) | 2.848 | 3.212 | 0.887 | NS | 2.694 | 0.236 | 0.149 | ||
| Mood disorder history | 1.323 | 0.631 | 0.204 | 2.095 | 0.039 | |||||
| Intake EPDS | 0.318 | 0.095 | 0.365 | 3.351 | 0.001 | |||||
| Step 2 | (Constant) | 0.763 | 3.330 | 0.229 | NS | 2.888 | 0.270 | 0.176 | ||
| Mood Disorder History | 1.000 | 0.642 | 0.154 | 1.557 | NS | |||||
| Intake EPDS | 0.221 | 0.105 | 0.253 | 2.094 | 0.039 | |||||
| ASQ | 0.039 | 0.019 | 0.237 | 1.981 | 0.051 | |||||
In order to offer an initial estimate of the potential clinical utility of attachment insecurity for the prediction of PPD, an estimated risk for postnatal depression, measured as an EPDS score over 12 recorded in either the first or the second postpartum survey (aligning with DSM-V diagnostic criteria for postnatal depression that stipulate onset in the first month postpartum), was calculated. This calculation used a cutoff for the adjusted ASQ score of 72.5, which represented the 25th percentile in this study population. The calculation yielded a positive predictive value of 0.54 and a negative predictive value of 0.84, with an associated relative risk of 3.6, for women in the top 25% as compared to the bottom 75% of the ASQ distribution.
4.4. Anxious and avoidant subtypes of attachment insecurity are both related to postnatal depressive symptoms
The ASQ consists of five subscales, which have been mapped by a large factor-analytic study onto the more widely recognized anxious and avoidant subtypes of attachment impairment (Brennan et al., 1998). In order to determine whether score on any particular subscale was most strongly associated with postnatal depression, Pearson correlations between measures of postnatal depressive symptoms and individual ASQ subscale scores were computed (Table 4).
Table 4.
Relative Contributions of the Five ASQ Subscales to Antenatal Prediction of Postpartum Depressive Symptoms. Predictive value for postpartum depressive symptoms is somewhat higher for ASQ subscales loading to the anxious subtype of attachment insecurity than to the avoidant subtype, though both make significant contributions. Pearson Correlations.
| Confidence (avoidant, re- verse scored) |
Discomfort (avoidant) |
Relationships as Secondary (avoidant) |
Need for Approval (anxious) |
Preoccupation with Relation- ships (anxious) |
ASQ, total | |
|---|---|---|---|---|---|---|
| EPDS mean 3 months |
−0.316*** | 0.361*** | 0.277** | 0.525*** | 0.543*** | 0.516*** |
| CESD mean 3 months |
−0.376*** | 0.465*** | 0.319*** | 0.503*** | 0.490*** | 0.558*** |
| EPDS mean 6 months |
−0.249** | 0.285** | 0.195* | 0.457*** | 0.517*** | 0.435*** |
| CESD mean 6 months |
−0.316*** | 0.430*** | 0.269** | 0.461*** | 0.467*** | 0.507*** |
p ≤ 0.05,
p ≤ 0.01,
p ≤ 0.001.
All ASQ subscales showed significant correlations with postnatal depressive symptoms, however the magnitude of the correlation was greater for the subscales loading to anxious attachment (i.e., Preoccupation with Relationships and Need for Approval) than for the subscales loading to avoidant attachment (i.e. Discomfort with Closeness, Relationships as Secondary, and Confidence).
4.5. Antenatal ASQ most strongly predicts mood in the early postnatal period, while history of mood disorder more strongly predicts mood over the long term
A hypothesis consistent with the above findings is that inadequate early parenting experiences as reflected in high attachment insecurity (particularly of the anxious subtype) could predispose women to crisis when faced with responsibility for a neonate. If this were so, high ASQ scores should predict depressive symptoms most strongly in the early postnatal period, and history of mood disorder should be less relevant in this timeframe but perhaps more indicative of depressive symptoms over the long term.
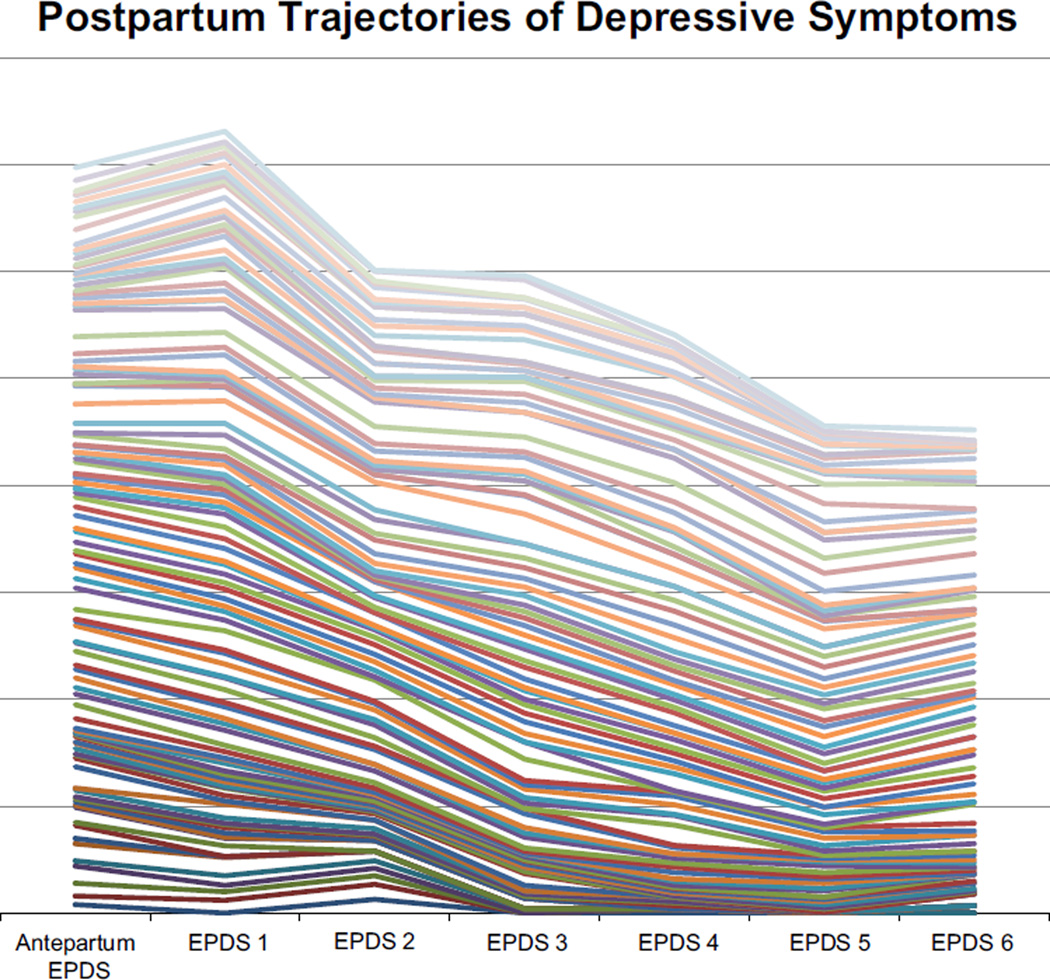
For an initial exploration of this hypothesis, EPDS trajectories for all participants were plotted out to determine whether a gross trend was evident (Fig. 1). This graph indicated that most study participants had the highest levels of depressive symptoms in the first two months postpartum, and that this early peak in depressive symptoms was increasingly more prominent in women with greater attachment insecurity.
Fig. 1.
Individual Trajectories of Depressive Symptoms Over Six Months Post-partum. Participants with lower ASQ scores are pictured in darker colors, those with higher ASQ scores in lighter colors. Participants with lower ASQ scores have flatter trajectories. Participants with higher ASQ scores show a depressive peak in the first postpartum month, which is progressively more pronounced with higher ASQ scores. (N=107).
One-way repeated measures ANOVA revealed significant effects of time alone (F(5.22, 287)=4.96, p < 0.001), of ASQ (F(1,55)= 13.52 , p=0.001), and also of time*ASQ (F(5.22, 287)=6.03, p < 0.001) on the trajectory of EPDS scores over the seven available timepoints.
One-way repeated measures ANOVA on the trajectory of CESD scores over the seven available timepoints also showed significant effects of time (F(4.64, 250)=5.39, p < 0.001), of ASQ (F(1.56)= 20.32, p=0.001), and of time*ASQ (F(4.64, 250)=7.10, p < 0.001). For both measures of depression, Mauchly’s test indicated that the assumption of sphericity had been violated, χ2(20)=66.9, p=0 .001, therefore degrees of freedom were corrected using Huynh–Feldt estimates of sphericity (ε =0.87 and 0.77 for EPDS and CESD respectively).
Parameter estimates indicated significant effects of ASQ on CESD slope at the intake and first four postpartum months (p < 0.005 for all timepoints between the third trimester and four months postpartum) but not for the fifth or sixth postpartum month. Effects of ASQ on EPDS slope were significant at the same timepoints, with p < 0.001 for intake through the third month postpartum, p =0.014 for the fourth month, and nonsignificant results for the fifth and sixth months.
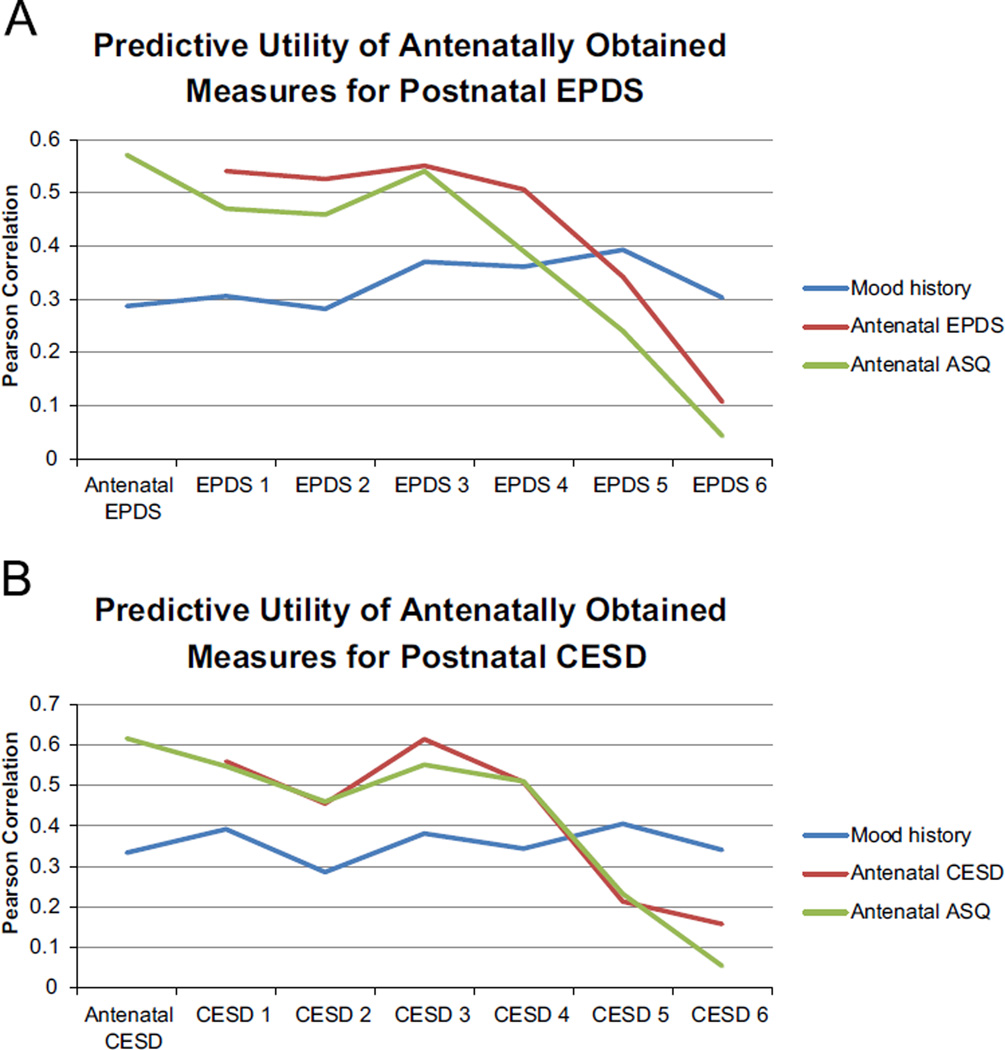
In order to probe this observation further, correlations between antenatal ASQ, antenatal depressive symptoms, and history of mood disorder against mean depression scores were examined at each postnatal time point (Fig. 2). The initial results (Fig. 2A and B) are consistent with the hypothesis, showing that both antenatal ASQ and antenatal depressive symptoms correlate most strongly with postnatal depressive symptoms in the first three to four months postpartum, and are less predictive of depressive symptoms after this point. In contrast, history of mood disorder maintains a more stable correlation with depressive symptoms. During the first three to four months postpartum, the correlation between history of mood disorder and postnatal depressive symptoms is lower than the correlations between antenatal depressive symptoms/ASQ and postnatal depressive symptoms; however, at five to six months postpartum, the correlations between antenatal depressive symptoms/ASQ and postnatal depressive symptoms drop off, while the correlation between mood disorder history and postnatal depressive symptoms remains steady.
Fig. 2.
Correlation coefficients between selected antenatal measures and depressive symptoms at each monthly time point. Both antenatal depressive symptoms and antenatal ASQ scores predict postpartum depressive symptoms most strongly in the first three months, and decrease in importance thereafter. (N=107).
In order to account for collinearity between the antenatal depression scores and the ASQ score, the analysis was repeated using adjusted antenatal depression and ASQ scores that had been corrected for the relationship between the two (data not shown). As expected, this decreased the individual predictive utility of each of these measures, however the temporal pattern remained the same.
5. Conclusions
This work demonstrates that maternal personality factors are of importance in determining vulnerability to PPD, over and above their relationship to history of mood disorder or antenatal depressive symptoms. Among the three personality traits studied in this research, attachment insecurity was the most potent and robust predictor of postnatal depressive symptoms in this sample. An existing scale based on neuroticism and interpersonal sensitivity, the VPSQ, was equally predictive for postnatal depressive symptoms as measured by the EPDS (which was the outcome measure used to develop the scale) but was not independently predictive of postnatal depressive symptoms as measured by the CESD, which differs from the EPDS in that it contains items that address feelings of worthlessness and the quality of relationships with others, aspects of depression which are not measured by the EPDS. It is notable that the ASQ, which was not developed with any specific regard to pregnant populations or to the prediction of depressive symptoms, nonetheless outperformed the VPSQ in this study sample.
The predictive value of attachment insecurity for postnatal depressive symptoms could account for a significant proportion of the variance otherwise ascribed to mood disorder history and to antenatal depressive symptoms, which until now have been considered the most powerful and relevant clinical predictors (O’Hara and Swain, 1996). It is important to note that the effect size we found for mood disorder history is quite consonant with effect sizes found by previous investigators in this area. A landmark meta-analysis of predictors of PPD (O’Hara and Swain, 1996) found an r=0.27 for history of psychopathology; this is actually somewhat lower than our own correlation coefficients for history of mood disorder, which ranged from 0.32 to 0.37 depending on the measure and period of time assessed. O’Hara and Swain also found r=0.35 for antenatal depression; this is also lower than our values of 0.55 and 0.50 for the relationship between antenatal and postnatal EPDS over three and six months respectively. Thus it is not likely that our results represent a chance underestimation of the importance of mood disorder history or of antenatal depression. The fact that attachment insecurity remained highly significant even when antenatal depressive symptoms were controlled indicates that attachment insecurity represents a risk factor in its own right, and is not simply a proxy for existing depression. Indeed, it is possible that antenatal depression itself is also in part a result of attachment insecurity, although the present work was not designed to test that hypothesis.
On the basis of this work, we propose that postnatal depression, at least in many cases, may be conceptually classified as a result of disordered attachment. The postnatal period may represent a period of crisis for the mother whose own attachments are insecure, or who received inadequate early parental care. She may be confronting a developmental lacuna that resulted in inadequacies in her own parenting instinct, or even the unconscious expectation that the baby would fulfill the role of loving, secure presence that had been lacking for the mother herself.
The question of whether particular subtypes of attachment insecurity are more strongly related to postnatal depressive symptoms remains an open one; the issue is clouded by in-homogeneities in the choices of instrument and subtypes of attachment insecurity used in the existing literature. For example, Bifulco et al. (2004) found that avoidant but not anxious attachment predicted PPD. Meredith and Noller (2003) found an association with PPD for preoccupied but not fearful or dismissing attachment. Simpson et al. (2003) found that ambivalent but not avoidant attachment styles were associated with increased depression postnatally. In contrast, Monk et al. (2008) and Rholes et al. (2011) found that all insecure attachment styles (which included fearful, preoccupied, dismissing for Monk et al. and avoidant, anxious for Rholes et al.) increased risk for PPD without significant differences between subtypes of insecure attachment. The findings from the present study are more in line with the results of the latter two investigations, although a somewhat greater association with postnatal depressive symptoms was found for anxious than for avoidant attachment style. In general it will be difficult to resolve this disparity in the literature without greater agreement among investigators on optimal measures and attachment orientation subtypes for use in the perinatal population.
Given that underlying insecure attachment has far-reaching effects on the stability of an individual’s social network and the support resources available, it is possible that other psychosocial contributors to PPD (e.g. poor partner support (Gremigni et al., 2011) or poor general social support (Xie et al., 2009)) may in fact be themselves related to disordered attachment, and act in part as mediators for the ultimate effect of attachment insecurity on postpartum mood. However, confirmation of this hypothesis would require a more targeted study.
The predictive value of attachment insecurity is most potent for postnatal depressive symptoms occurring in the first three months postpartum. This is in contrast with the predictive value of mood disorder history, which is less potent for depressive symptoms in the early postpartum period but becomes more relevant at later time points.
The relatively greater importance of mood disorder history in predicting depressive symptoms beyond the early postpartum suggests that there may be etiological differences between PPD and depression occurring at other phases of the life cycle. Other investigators have also documented specificity in the patterns of risk imposed by psychiatric history, such that previous or familial episodes of PPD predispose more specifically to future episodes of PPD, rather than to non-postpartum depressive episodes (Cooper and Murray, 1995; Forty et al., 2006; Payne et al., 2008). Thus, while many etiological factors in PPD remain to be elucidated, our research adds to the evidence from previous studies of psychiatric history and PPD risk that suggests at least one pathway in the genesis of PPD that is distinct from those in other unipolar or bipolar depressive episodes.
It is notable that there is also a highly significant correlation between antenatal depressive symptoms and attachment insecurity. One obvious explanation for this could be that depressed mood prompts more negative assessments of one’s self and one’s relationships with others. This is important to note because until recently, adult attachment style has been treated as something of an immutable personality characteristic, although to our knowledge this was not based on any reliable data. However, several investigators have documented positive results from interventions intended to alter attachment style (Kilmann et al., 1999; Kirchmann et al., 2012; Maxwell et al., 2013; Travis et al., 2001). It is also possible that attachment insecurity is specifically related to perinatal depression in general, and thus increases the risk for depressive symptoms both antenatally and postnatally; however this would not align with data suggesting significant phenotypic differences between antenatal and postnatal depression (Altemus et al., 2012). It is impossible to distinguish between these two explanations based on the data reported here, and both explanations may be valid to an extent.
Weaknesses in our study design include relatively small sample size and socioeconomic homogeneity in the sample. Nonetheless the size of the effect we have found is easily significant in the available sample, and given that previous investigators have found similar effects we do not believe that our results are likely to represent a statistical anomaly. Socioeconomic homogeneity is another concern - by and large our participants were married, well educated, and economically stable. Thus we cannot generalize to other populations from this work. However, we do note that rates and severity of early life stress (and hence of attachment insecurity) are likely to be lower in our sample than they would be in a more socioeconomically disadvantaged group, and so if anything we would expect this effect to be more difficult to detect in the sample we have used. That the association between attachment insecurity and PPD was highly significant even in this socioeconomically privileged sample speaks to the powerful nature of the effect. Another major weakness in our study design was the lack of a clinical interview to confirm or rule out a diagnosis of depression in women with elevated EPDS or CESD scores. This means that conclusions are restricted to statements about levels of symptoms assessed by these self-report scales rather than about clinical depression. However the advantage of self-report scales is that they minimize the risk of rater bias. Overall these findings remain important, especially given the recognized validity of the scales and the use of repeated administrations to reduce error associated with transient periods of “blues.”
Strengths of our study include prospective longitudinal design, accurate assessment of psychiatric history by interviewer-administered SCID, and excellent retention rate. As mentioned we are far from the first group to report an association between attachment insecurity and PPD; however we believe we are the first to describe the size of the effect in a quantitative manner with a reliable comparison to mood disorder history, antenatal depression, and alternative personality-based predictors as well as other psychosocial risk factors in both clinical and nonclinical subjects. We are also the first to use frequently repeated measures within a longitudinal design to delineate the trajectory of depressive symptoms over six months postpartum. Most previous studies of this topic have used either one or two postpartum time-points, and thus would not have been able to elicit the information about the early postpartum peak in depressive symptoms and its unique relationship to attachment insecurity.
Based on our data we predict that therapeutic interventions targeted towards strengthening the mother’s interpersonal relationships and attachment security should be most effective. This prediction is consistent with available research supporting the effectiveness of interpersonal psychotherapy (IPT), which is grounded in attachment theory, for PPD (Grote et al., 2009; Mulcahy et al., 2010; O’Hara et al., 2000; Zlotnick et al., 2001,), although the body of literature on this topic is scant and appropriate controls are difficult to design. We suggest that, for example, existing basic IPT could be further modified for the depressed new mother by including a more formal measure of attachment style (such as the ASQ) and structuring the therapy to address specific areas of attachment insecurity that are relevant for the particular patient. Incorporating measures of attachment insecurity into antenatal assessments may also prove to be useful for the prediction of postnatal depression, although further research to develop and validate a clinically useful scale would be required.
Supplementary Material
Acknowledgments
We thank Lin Lee, C.N.M., Maria Greulich, C.N.M., and Nicole Wilcox, M.D. for assistance with recruiting.
Role of funding source
This work was supported by a T32 training grant to the Stanford University Department of Psychiatry from the National Institutes of Mental Health. The T32 covered Dr. Robakis’ salary and some expenses related to recruitment for the study. The NIMH did not have any role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the article for publication.
Footnotes
Author contributions
Thalia Robakis conceived of the study, designed it with input from Drs. Williams and Rasgon, managed recruitment, did the majority of study subject interviews, data entry and analysis, compiled figures and tables, and did the majority of the writing of the paper.
Katherine Ellie Williams provided clinical and research-based advice and oversight, and contributed to the writing and editing of the paper. Susan Crowe provided advice and oversight and participated in subject recruitment. Katie Watson-Lin provided statistical expertise and contributed to writing and editing. Jamie Gannon assisted with study subject interviews. Natalie Rasgon provided guidance and oversight throughout the project, and contributed proofreading and editing to the final paper.
Appendix A Supplementary material
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1016/j.jad.2015.09.067.
References
- Alexander R, Feeney J, Hohaus L, Noller P. Attachment style and coping resources as predictors of coping strategies in the transition to parenthood. Pers. Relationsh. 2001;8(2):137–152. [Google Scholar]
- Altemus M, Neeb CC, Davis A, Occhiogrosso M, Nguyen T, Bleiberg KL. Phenotypic differences between pregnancy-onset and postpartum-onset major depressive disorder. J. Clin. Psychiatry. 2012;73(12):e1485–e1491. doi: 10.4088/JCP.12m07693. [DOI] [PubMed] [Google Scholar]
- Austin M, Lumley J. Antenatal screening for postnatal depression: a systematic review. Acta Psychiatr. Scand. 2003;107(1):10–17. doi: 10.1034/j.1600-0447.2003.02024.x. [DOI] [PubMed] [Google Scholar]
- Banti S, Mauri M, Oppo A, Borri C, Rambelli C, Ramacciotti D, et al. From the third month of pregnancy to 1 year postpartum. prevalence, incidence, recurrence, and new onset of depression. Results from the perinatal Depression - research and screening unit study. Compr. Psychiatry. 2011;52(4):343–351. doi: 10.1016/j.comppsych.2010.08.003. [DOI] [PubMed] [Google Scholar]
- Beck AT. Depression: Clinical Experimental Theoretical aspects. Vol. 32. University of Pennsylvania Press; 1967. [Google Scholar]
- Bifulco A, Figueiredo B, Guedeney N, Gorman LL, Hayes S, Muzik M, et al. Maternal attachment style and depression associated with childbirth: Preliminary results from a European and US cross-cultural study. Br. J. Psychiatry. 2004;46(Suppl):s31–s37. doi: 10.1192/bjp.184.46.s31. [DOI] [PubMed] [Google Scholar]
- Boyce P, Parker G, Barnett B, Cooney M, Smith F. Personality as a vulnerability factor to depression. Br. J. Psychiatry. 1991;159(1):106–114. doi: 10.1192/bjp.159.1.106. [DOI] [PubMed] [Google Scholar]
- Boyce P, Hickey A, Gilchrist J, Talley N. The development of a brief personality scale to measure vulnerability to postnatal depression. Arch. Women’s Ment. Health. 2001;3(4):147–153. [Google Scholar]
- Bowlby J. A Secure Base: Parent-Child Attachment and Healthy Human Development. Routledge, London: 1988. [Google Scholar]
- Boyd RC, Le HN, Somberg R. Review of screening instruments for postpartum depression. Arch. Women’s Ment. Health. 2005;8(3):141–153. doi: 10.1007/s00737-005-0096-6. [DOI] [PubMed] [Google Scholar]
- Brand SR, Brennan PA. Impact of antenatal and postpartum maternal mental illness: how are the children. Clin. Obstet. Gynecol. 2009;52(3):441–455. doi: 10.1097/GRF.0b013e3181b52930. [DOI] [PubMed] [Google Scholar]
- Brennan KA, Clark CL, Shaver PR. Self-report measurement of adult attachment. Attach. Theory Close Relationsh. 1998:46–76. [Google Scholar]
- Carlson EA. A prospective longitudinal study of attachment disorganization/ disorientation. Child Dev. 1998;69(4):1107–1128. [PubMed] [Google Scholar]
- Church NF, Brechman-Toussaint ML, Hine DW. Do dysfunctional cognitions mediate the relationship between risk factors and postnatal depression symptomatology. J. Affect. Disord. 2005;87(1):65–72. doi: 10.1016/j.jad.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Cooper PJ, Murray L. Course and recurrence of postnatal depression. Evidence for the specificity of the diagnostic concept. Br. J. Psychiatry. 1995;166(2):191–195. doi: 10.1192/bjp.166.2.191. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. development of the 10-item edinburgh postnatal depression scale. Br. J. Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Dennis C, Chung-Lee L. Postpartum depression Help-Seeking barriers and maternal treatment preferences: a qualitative systematic review. Birth. 2006;33(4):323–331. doi: 10.1111/j.1523-536X.2006.00130.x. [DOI] [PubMed] [Google Scholar]
- Dennis C, Boyce P. Further psychometric testing of a brief personality scale to measure vulnerability to postpartum depression. J. Psychosom. Obstet. Gynaecol. 2004;25(3–4):305–311. doi: 10.1080/01674820400017962. [DOI] [PubMed] [Google Scholar]
- Dietz PM, Williams SB, Callaghan WM, Bachman DJ, Whitlock EP, Horn-brook MC. Clinically identified maternal depression before, during, and after pregnancies ending in live births. Am. J. Psychiatry. 2007;164(10):1515–1520. doi: 10.1176/appi.ajp.2007.06111893. [DOI] [PubMed] [Google Scholar]
- Feeney JA, Noller P, Hanrahan M. Assessing adult attachment. In: Sperling Michael B, Berman William H, editors. Attachment in Adults: Clinical and Developmental Perspectives. New York, NY, US: Guilford Press; 1994. [Google Scholar]
- Field T. Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav. Dev. 2010;33(1):1–6. doi: 10.1016/j.infbeh.2009.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV® Axis I Disorders (SCID-I), Clinician Version, Administration Booklet. American Psychiatric Publ. 2012 [Google Scholar]
- Forty L, Jones L, Macgregor S, Caesar S, Cooper C, Hough A, Psych MRC. Familiality of postpartum depression in unipolar disorder: results of a family study. Am. J. Psychiatry. 2006;163:9. doi: 10.1176/ajp.2006.163.9.1549. [DOI] [PubMed] [Google Scholar]
- Grazioli R, Terry DJ. The role of cognitive vulnerability and stress in the prediction of postpartum depressive symptomatology. Br. J. Clin. Psychol. 2000;39(4):329–347. doi: 10.1348/014466500163347. [DOI] [PubMed] [Google Scholar]
- Gremigni P, Mariani L, Marracino V, Tranquilli AL, Turi A. Partner support and postpartum depressive symptoms. J. Psychosom. Obstet. Gynaecol. 2011;32(3):135–140. doi: 10.3109/0167482X.2011.589017. [DOI] [PubMed] [Google Scholar]
- Grote N, Swartz H, Geibel S, Zuckoff A, Houck P, Frank E. A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatr. Serv. 2009;60(3):313–321. doi: 10.1176/appi.ps.60.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guintivano J, Arad M, Gould T, Payne J, Kaminsky Z. Antenatal prediction of postpartum depression with blood DNA methylation biomarkers. Mol. Psychiatry. 2013;19(5):560–567. doi: 10.1038/mp.2013.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones L, Scott J, Cooper C, Forty L, Smith KG, Sham P, Jones I. Cognitive style, personality and vulnerability to postnatal depression. Br. J. Psychiatry. 2010;196(3):200–205. doi: 10.1192/bjp.bp.109.064683. [DOI] [PubMed] [Google Scholar]
- Kilmann PR, Laughlin JE, Carranza LV, Downer JT, Major S, Parnell MM. Effects of an attachment-focused group preventive intervention on insecure women. Group Dyn.: Theory Res. Pract. 1999;3(2):138. [Google Scholar]
- Kirchmann H, Steyer R, Mayer A, Joraschky P, Schreiber-Willnow K, Strauss B. Effects of adult inpatient group psychotherapy on attachment characteristics: an observational study comparing routine care to an untreated comparison group. Psychother. Res. 2012;22(1):95–114. doi: 10.1080/10503307.2011.626807. [DOI] [PubMed] [Google Scholar]
- Maxwell H, Tasca GA, Ritchie K, Balfour L, Bissada H. Change in attachment insecurity is related to improved outcomes 1 year post group therapy in women with binge eating disorder. Psychotherapy. 2013;51(1):57–65. doi: 10.1037/a0031100. [DOI] [PubMed] [Google Scholar]
- McMahon C, Barnett B, Kowalenko N, Tennant C. Psychological factors associated with persistent postnatal depression: past and current relationships, defence styles and the mediating role of insecure attachment style. J. Affect. Disord. 2005;84(1):15–24. doi: 10.1016/j.jad.2004.05.005. [DOI] [PubMed] [Google Scholar]
- Mehta D, Newport D, Frishman G, Kraus L, Rex-Haffner M, Ritchie J, et al. Early predictive biomarkers for postpartum depression point to a role for estrogen receptor signaling. Psychol. Med. 2014:1–14. doi: 10.1017/S0033291713003231. [DOI] [PubMed] [Google Scholar]
- Meredith P, Noller P. Attachment and infant difficultness in postnatal depression. J. Fam. Issues. 2003;24(5):668–686. [Google Scholar]
- Milgrom J, Gemmill AW, Bilszta JL, Hayes B, Barnett B, Brooks J, et al. Antenatal risk factors for postnatal depression: a large prospective study. J. Affect. Disord. 2008;108(1):147–157. doi: 10.1016/j.jad.2007.10.014. [DOI] [PubMed] [Google Scholar]
- Monk C, Leight KL, Fang Y. The relationship between women’s attachment style and perinatal mood disturbance: implications for screening and treatment. Arch. Women’s Ment. Health. 2008;11(2):117–129. doi: 10.1007/s00737-008-0005-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulcahy R, Reay RE, Wilkinson RB, Owen C. A randomised control trial for the effectiveness of group interpersonal psychotherapy for postnatal depression. Arch. Women’s Ment. Health. 2010;13(2):125–139. doi: 10.1007/s00737-009-0101-6. [DOI] [PubMed] [Google Scholar]
- Oates M, Cantwell R. Saving mothers’ lives: reviewing maternal deaths to make motherhood safer. the eighth report of the confidential enquiries into maternal deaths in the United Kingdom. Chapter 11: deaths from psychiatric causes. Centre for Maternal and Child Enquiries (CMACE) BJOG. 2011;118(Suppl. 1):1–203. doi: 10.1111/j.1471-0528.2010.02847.x. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, Stuart S, Gorman LL, Wenzel A. Efficacy of interpersonal psychotherapy for postpartum depression. Arch. Gen. Psychiatry. 2000;57(11):1039–1045. doi: 10.1001/archpsyc.57.11.1039. [DOI] [PubMed] [Google Scholar]
- O’Hara MW, Swain AM. Rates and risk of postpartum depression - a meta-analysis. Int. Rev. Psychiatry. 1996;8:37–54. [Google Scholar]
- O’Hara WM, Gorman LL. Can postpartum depression be predicted. Prim. Psychiatry. 2004;11(3):42–47. [Google Scholar]
- Payne JL, MacKinnon DF, Mondimore FM, McInnis MG, Schweizer B, Za-moiski RB, Potash JB. Familial aggregation of postpartum mood symptoms in bipolar disorder pedigrees. Bipolar Disord. 2008;10(1):38–44. doi: 10.1111/j.1399-5618.2008.00455.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips J, Sharpe L, Matthey S, Charles M. Subtypes of postnatal depression? A comparison of women with recurrent and de novo postnatal depression. J. Affect. Disord. 2010;120(1):67–75. doi: 10.1016/j.jad.2009.04.011. [DOI] [PubMed] [Google Scholar]
- Power M, Duggan C, Lee A, Murray R. Dysfunctional attitudes in depressed and recovered depressed patients and their first-degree relatives. Psychol. Med. 1995;25(1):87–94. doi: 10.1017/s0033291700028117. [DOI] [PubMed] [Google Scholar]
- Power M, Katz R, McGuffin P, Duggan C, Lam D, Beck A. The dysfunctional attitude scale (DAS): a comparison of forms A and B and proposals for a new subscaled version. J. Res. Personal. 1994;28(3):263–276. [Google Scholar]
- Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1(3):385–401. [Google Scholar]
- Ravitz P, Maunder R, Hunter J, Sthankiya B, Lancee W. Adult attachment measures: a 25-year review. J. Psychosom. Res. 2010;69(4):419–432. doi: 10.1016/j.jpsychores.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Rholes WS, Simpson JA, Kohn JL, Wilson CL, Martin AM, III, Tran S, et al. Attachment orientations and depression: A longitudinal study of new parents. J. Pers. Soc. Psychol. 2011;100(4):567. doi: 10.1037/a0022802. [DOI] [PubMed] [Google Scholar]
- Ross CE, Mirowsky J. Components of depressed mood in married men and women: the Center for Epidemiologic Studies’ Depression Scale. Am. J. Epidemiol. 1984;119(6):997–1004. doi: 10.1093/oxfordjournals.aje.a113819. [DOI] [PubMed] [Google Scholar]
- Simard V, Moss E, Pascuzzo K. Early maladaptive schemas and child and adult attachment: a 15-year longitudinal study. Psychol. Psychother. 2011;84(4):349–366. doi: 10.1111/j.2044-8341.2010.02009.x. [DOI] [PubMed] [Google Scholar]
- Simpson JA, Rholes WS, Campbell L, Tran S, Wilson CL. Adult attachment, the transition to parenthood, and depressive symptoms. J. Pers. Soc. Psychol. 2003;84(6):1172. doi: 10.1037/0022-3514.84.6.1172. [DOI] [PubMed] [Google Scholar]
- Sroufe LA. Attachment and development: a prospective, longitudinal study from birth to adulthood. Attach. Hum. Dev. 2005;7(4):349–367. doi: 10.1080/14616730500365928. [DOI] [PubMed] [Google Scholar]
- Stein H, Koontz AD, Fonagy P, Allen JG, Fultz J, Brethour JR, et al. Adult attachment: What are the underlying dimensions. Psychol. Psychother. 2002;75(1):77–91. doi: 10.1348/147608302169562. [DOI] [PubMed] [Google Scholar]
- Travis LA, Bliwise NG, Binder JL, Horne-Moyer HL. Changes in clients’ attachment styles over the course of time-limited dynamic psychotherapy. Psychotherapy. 2001;38(2):149. [Google Scholar]
- Verkerk GJ, Denollet J, Van Heck GL, Van Son MJ, Pop VJ. Personality factors as determinants of depression in postpartum women: a prospective 1-year follow-up study. Psychosom. Med. 2005;67(4):632–637. doi: 10.1097/01.psy.0000170832.14718.98. [DOI] [PubMed] [Google Scholar]
- Wisner KL, Sit DK, McShea MC, Rizzo DM, Zoretich RA, Hughes CL, et al. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression. JAMA Psychiatry. 2013;70(5):490–498. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie R, He G, Koszycki D, Walker M, Wen SW. Prenatal social support, postnatal social support, and postpartum depression. Ann. Epidemiol. 2009;19(9):637–643. doi: 10.1016/j.annepidem.2009.03.008. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Johnson SL, Miller IW, Pearlstein T, Howard M. Postpartum depression in women receiving public assistance: pilot study of an interpersonal-therapy-oriented group intervention. Am. J. Psychiatry. 2001;158(4):638–640. doi: 10.1176/appi.ajp.158.4.638. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.