Abstract
Although the most common form of the persistent left superior vena cava anomaly is usually clinically silent and often discovered incidentally, the risk of developing cyanosis, heart failure, and embolic cerebrovascular events is high among cases where the anomaly causes a right to left shunt. A rare case of persistent left superior vena cava draining into the left atrium through the superior left pulmonary vein is presented with a discussion of the embryology, morphologic forms, and clinical significance of the persistent left superior vena cava.
Abbreviations: CT, computed tomography
Introduction
The presence of a persistent left superior vena cava is the most common congenital anomaly of the systemic veins of the thorax with an estimated prevalence ranging from 0.3% to 2% in the general population [1, 2] and a higher prevalence of 4.4% among those with congenital heart disease [3]. When the persistent left superior vena cava drains into the coronary sinus and right atrium, which is manifested in 80 to 90% of cases [4], patients are typically asymptomatic, and the anomaly is incidentally encountered on cross sectional imaging for another indication or during intravenous catheterization or placement of pacemaker or defibrillator leads [4, 5]. This form of the anomaly is not associated with increased risks inherent with a right to left shunt such as embolic cerebrovascular events. Rarely, the persistent left superior vena cava will drain into the left atrium through an unroofed coronary sinus, a direct connection to the left atrium, or through the left superior pulmonary vein. In contradistinction to the most common form of the anomaly, these anomalies are associated with an increased risk of cyanosis [6], heart failure [7], intracerebral abscess [8, 9], and embolic cerebrovascular stroke [10].
Case Report
A 71-year-old man developed acute renal failure following repair of a 9.5 cm thoracoabdominal aortic aneurysm complicated by left renal artery occlusion. A left internal jugular hemodialysis catheter was placed with subsequent chest radiograph demonstrating an unusual course of the catheter (Fig. 1). Interventional radiology was consulted to investigate the location and patency of the left internal jugular catheter. Digital subtraction angiography was performed which demonstrated the tip of the left venous catheter to be in the left superior pulmonary vein. Contrast injected into the left internal jugular venous catheter demonstrated opacification of the left superior pulmonary vein, left atrium, left ventricle, and aorta (Fig. 2). The patient’s previous radiographic images were reviewed, and a contrast-enhance computed tomography scan performed prior to this hospitalization demonstrated a persistent left superior vena cava draining into the left superior pulmonary vein. The left brachiocephalic vein bridged the persistent left superior vena cava with the normal right superior vena cava. The coronary sinus was normal (Fig. 3).
Figure 1.
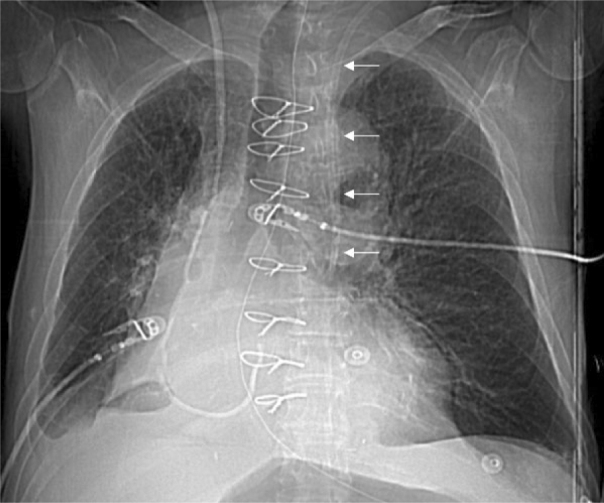
71-year-old man with a persistent left superior vena cava draining into the left superior pulmonary vein. Radiograph of the chest following left internal jugular catheter placement demonstrates the abnormal course of the catheter depicted by the arrows. The tip of the left internal jugular catheter is in the left paramedian location and not in the expected region of the superior vena cava / right atrial junction.
Figure 2.
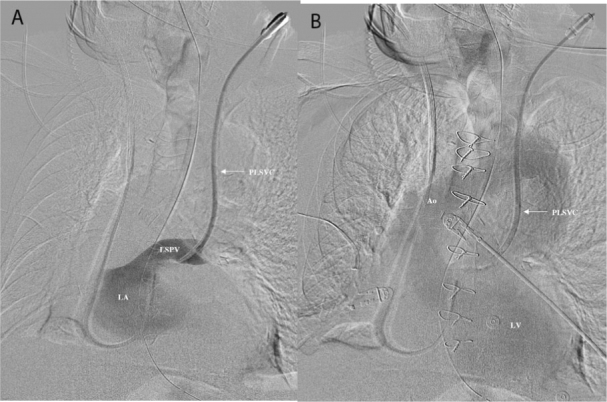
71-year-old man with a persistent left superior vena cava draining into the left superior pulmonary vein. Digital subtraction angiography following injection of left internal jugular venous catheter demonstrates catheterization of a persistent left superior vena cava (PLSVC) and (A) opacification of the left superior pulmonary vein (LSPV) and left atrium (LA). Subsequent image demonstrates (B) opacification of the left ventricle (LV) and aorta (Ao).
Figure 3.
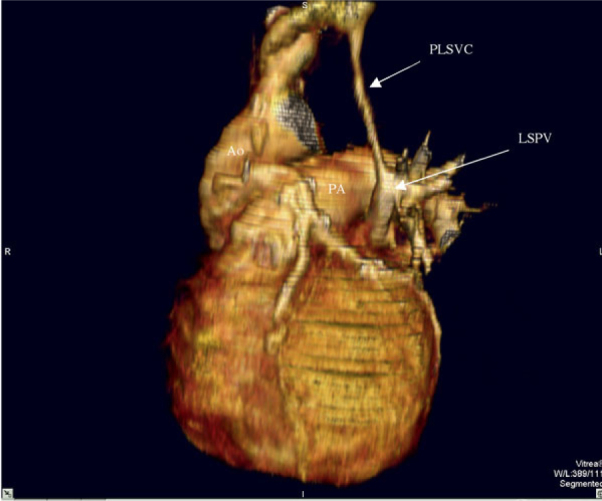
71-year-old man with a persistent left superior vena cava draining into the left superior pulmonary vein. Volume rendering oblique view of the heart from CT scan demonstrates a persistent left superior vena cava (PLSVC) anterior to the suppressed aorta (Ao) draining into the left superior pulmonary vein (LSPV). The pulmonary artery (PA) is labeled.
Discussion
The case presented here is a very rare form of persistent left superior vena cava with only five cases reported in the literature to our knowledge. In 1915, Johnston provided the first description of a persistent left superior vena cava communicating with the left superior pulmonary vein from the autopsy of a 56-year-old man [11]. The entity has been described in conjunction with congenital heart anomalies including coarctiation of the aorta [12] and an atrial septal defect [13]. The first report of this variation as an isolated entity without additional congenital cardiac malformations was in 2002 by Metzler where he described a patient with hypoxemia and erythrocytosis [6]. The treatment of this entity in a patient who had two episodes of transient ischemic attack following air embolism from the infusion of intravenous fluid through a peripheral left arm vein has been reported using an Amplatzer vascular plug to successfully occlude a persistent left superior vena cava communicating with the left superior pulmonary vein [10].
While the case presented here is very rare, 50 to 70% of patients with a persistent left superior vena cava are at risk of paradoxical embolism due to the presence of a right to left shunt [14]. This most frequently occurs through an atrial septal defect in patients with normal drainage of the persistent left superior vena cava into the right atrium through the coronary sinus. In eight to ten percent of patients, the right to left shunt occurs when the persistent left superior vena cava drains into the left atrium through an unroofed coronary sinus [5]. Though very rare, the persistent left superior vena cava has also been shown to drain directly into the left atrium in the presence of a normal coronary sinus [15, 16]. Complications of the right to left shunt have included cerebrovascular embolism [8, 9, 10], cyanosis [6], and heart failure [7].
Occurring in 80 to 90% of cases, the most common manifestation of the persistent left superior vena cava demonstrates drainage into the right atrium through the coronary sinus. The anomaly develops in the eighth week of gestation as the main venous drainage system of the embryo’s body develops. Paired anterior cardinal veins drain the cranial portions of the body while the caudal portions of the body are drained by the paired posterior cardinal veins. The right anterior and posterior cardinal veins and the left anterior and posterior cardinal veins drain into the right and left common cardinal veins, respectively. At eight weeks of gestation the inomminate vein connects the left and right anterior cardinal veins. The internal jugular veins develop from the anterior cardinal veins cephalic to the inomminate vein. Caudal to the inomminate vein, the right anterior cardinal vein joins with a portion of the right common cardinal vein to form the normal right-sided superior vena cava. The left anterior cardinal vein, caudal to the inomminate vein, normally regresses to form the ligament of Marshall. Failure of the left anterior cardinal vein to regress caudal to the inomminate vein results in the development of a persistent left superior vena cava. A normal right superior vena cava is present in 90% of cases where a persistent left superior vena cava is present. A bridging inomminate vein connecting the vena cavae is present in 30% of these cases [17].
Although the common form of persistent left superior vena cava is not associated with the risks inherent with a right to left shunt, there are other important clinical implications to consider in patients with a persistent left superior vena cava. Catheterization of the coronary sinus through a persistent left superior vena cava is 4.8 times more likely to cause supraventricular tachycardia than catheterization through a right superior vena cava [18]. Atrial fibrillation and sudden death can occur in patients with persistent left superior vena cava owing to repetitive rapid discharges and shorter activation cycle length from the multiple anatomical and electrical communications with the atria [4]. In patients with coronary sinus ostial atresia, severe myocardial ischemia can occur if there is interruption of the persistent left superior vena cava during cardiac surgery [19]. Also, technical difficulties in the placement of pacemaker or defibrillator leads in patients with persistent left superior vena cava have been well described [4].
Footnotes
Published: October 1, 2008
Contributor Information
Muhammad Yousaf, Email: yousafmuhammad@uams.edu.
Sharp F. Malak, Email: sfmalak@uams.edu.
References
- 1.Albert M, Geissler W. [Persistent left superior vena cava and mitral stenosis.] Z Gesamte Inn Med. 1956 Oct 1;11(19):865–874. [PubMed] [PubMed] [Google Scholar]
- 2.Edwards J, DuShane J. Thoracic venous anomalies. Arch Pathol. 1950;49:517–537. [Google Scholar]
- 3.Cha EM, Khoury GH. Persistent left superior vena cava. Radiologic and clinical significance. Radiology. 1972 May;103(2):375–381. doi: 10.1148/103.2.375. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Ratliff HL, Yousufuddin M, Lieving WR. Persistent left superior vena cava: case reports and clinical implications. Int J Cardiol. 2006 Nov 10;113(2):242–246. doi: 10.1016/j.ijcard.2005.08.067. [PubMed] Epub 2005 Nov 28. [DOI] [PubMed] [Google Scholar]
- 5.Biffi M, Boriani G, Frabetti L, Bronzetti G, Branzi A. Left superior vena cava persistence in patients undergoing pacemaker or cardioverter defibrillator implantation: a 10-year experience. Chest. 2001 Jul;120(1):139–144. doi: 10.1378/chest.120.1.139. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Metzler B, Hillebrand H, Eulenbruch HP, Dierkesmann R, Hust MH. [Persistent left superior vena cava with right-left shunt into the left atrium] Dtsch Med Wochenschr. 2002 Jan 18;127(3):83–86. doi: 10.1055/s-2002-19592. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Kuhn A, Hauser M, Eicken A, Vogt M. Right heart failure due to an unroofed coronary sinus in an adult. Int J Cardiol. 2006 Nov 10;113(2):248–249. doi: 10.1016/j.ijcard.2005.08.059. [PubMed] Epub 2005 Nov 14. [DOI] [PubMed] [Google Scholar]
- 8.Erol I, Cetin II, Alehan F. Brain abscess associated with isolated left superior vena cava draining into the left atrium in the absence of coronary sinus and atrial septal defect. Cardiovasc Intervent Radiol. 2006 May-Jun;29(3):454–456. doi: 10.1007/s00270-005-0082-4. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.De Geest B, Vandommele J, Herregods MC. Isolated left sided superior vena cava draining into the left atrium associated with recurring intracerebral abscesses. A case report. Acta Cardiol. 1994;49(2):175–182. [PubMed] [PubMed] [Google Scholar]
- 10.Recto MR, Sadlo H, Sobczyk WL. Rare case of persistent left superior vena cava to left upper pulmonary vein: pathway for paradoxical embolization and development of transient ischemic attack and subsequent occlusion with an amplatzer vascular plug. J Invasive Cardiol. 2007 Oct;19(10):E313–E316. [PubMed] [PubMed] [Google Scholar]
- 11.Johnston TB. A Rare Vascular Anomaly-Opening of the Upper Left Pulmonary Vein into a Persistent Left Superior Vena Cava. J Anat Physiol. 1915 Jan;49(Pt 2):182–186. [PubMed] [PMC free article] [PubMed] [Google Scholar]
- 12.Odman P. A persistent left superior vena cava communicating with the left atrium and pulmonary vein. Acta radiol. 1953 Dec;40(6):554–560. doi: 10.3109/00016925309177064. [PubMed] [DOI] [PubMed] [Google Scholar]
- 13.Overy HR, Steinbicker PG, Jr, Blount SG., Jr Anomalous systemic venous drainage with hypoplasia of the right ventricular myocardium. Circulation. 1966 Apr;33(4):613–616. doi: 10.1161/01.cir.33.4.613. [PubMed] [DOI] [PubMed] [Google Scholar]
- 14.Tak T, Crouch E, Drake GB. Persistent left superior vena cava: incidence, significance and clinical correlates. Int J Cardiol. 2002 Jan;82(1):91–93. doi: 10.1016/s0167-5273(01)00586-1. [PubMed] [DOI] [PubMed] [Google Scholar]
- 15.Davis WH, Jordaan FR, Snyman HW. Persistent left superior vena cava draining into the left atrium, as an isolated anomaly. Am Heart J. 1959 Apr;57(4):616–622. doi: 10.1016/0002-8703(59)90036-5. [PubMed] [DOI] [PubMed] [Google Scholar]
- 16.Ardilouze P, Bricot V, Maurel C, Christiaens L. A rare case of left superior vena cava draining into left atrium demonstrated by MDCT. Int J Cardiol. 2007 Aug 9 doi: 10.1016/j.ijcard.2007.05.104. [PubMed] [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Yagel S, Kivilevitch Z, Achiron R. The fetal venous system: normal embryology, anatomy and physiology, and the development and appearance of anomalies. In: Yagel G, editor. Fetal Cardiology: Embryology, Genetics, Physiology, Echocardiographic Evaluation, Diagnosis and Perinatal Management of Cardiac Diseases. Taylor & Francis; London, England: 2003. pp. 321–324. [Google Scholar]
- 18.Fraser RS, Dvorkin J, Rossall RE, Eidem R. Left superior vena cava: a review of associated congenital heart lesions, catheterization data and roentgenologic findings. Am J Med. 1961 Nov;31:711–716. doi: 10.1016/0002-9343(61)90155-3. [PubMed] [DOI] [PubMed] [Google Scholar]
- 19.Muster AJ, Naheed ZJ, Backer CL, Mavroudis C. Is surgical ligation of an accessory left superior vena cava always safe? Pediatr Cardiol. 1998 Jul-Aug;19(4):352–354. doi: 10.1007/s002469900321. [PubMed] [DOI] [PubMed] [Google Scholar]


