Abstract
Choledochal cyst is a dilation that encloses the intrahepatic or both extra- and intrahepatic portions of the biliary ducts. Postnatally, ultrasonography is the initial diagnostic modality of choice, allowing for precise measurements of intra- or extrahepatic duct dilatation and identification of stones and sludge. Symptoms depend on the age at presentation. Common bile duct malformations should be considered as a differential diagnosis of a cystic mass regardless of the cyst's size or patient's age, especially in children presenting with abdominal pain, jaundice, and palpable mass. To the best of our knowledge, we report the largest choledochal cyst in infancy.
Keywords: Choledochal cyst, Giant, Infant
Introduction
Dilatation of various lengths and severity of the common bile duct (CBD), entitled choledochal cyst, has been detected in utero and usually presents with icterus in infancy, clinically mimicking biliary atresia and neonatal hepatitis1). Younger children and occasionally infants tend to present with painless jaundice, and older children present with recurrent abdominal pain, which was actually due to acute pancreatitis1,2). Postnatally, ultrasonography (US) is the initial diagnostic modality of choice, allowing for precise measurements of intra- or extrahepatic duct dilatation and identification of stones and sludge. Magnetic resonance cholangiopancreatography (MRCP) and endoscopic retrograde cholangiopancreatography (ERCP) has superseded the use of computed tomography (CT) for preoperative anatomical delineation of the pancreaticobiliary tract. Here we present the biggest choledochal cyst reported in infancy in the literature to our knowledge.
Case report
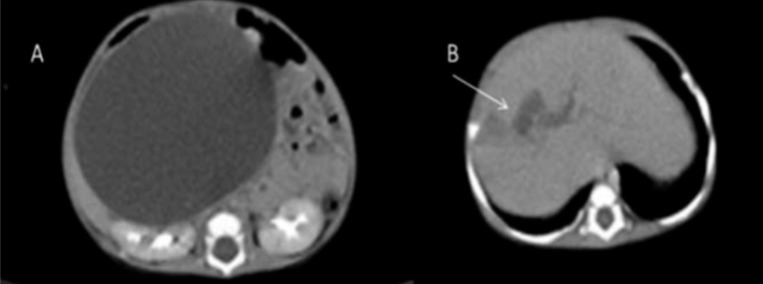
A term female baby was born by normal delivery route after consanguineous marriage, at house, in Syria as the 6th child of her parents. This family was living the civil war in Syria at that time. During 4 months period abdominal distension had increased. Because of restlessness and growing abdominal distension they had admitted to a hospital in Syria. But as a result of investigations they were sent home because of normal laboratory results. After 15 days they admitted to hospital because of jaundice and abdominal cyst was identified by US. She had referred to our hospital (in Turkey) with the preliminary diagnosis of abdomianl cyst and hepatitis developed due to compression of cyst. On her admission, physical examination revealed severe icterus and huge abdominal mass. US revealed giant abdominal cyst with thin wall and liquid-debris level extending from right upper quadrant to pelvic region. There was minimal dilatation at intrahepatic bile ducts. Bilateral ovaries, kidneys, and pancreas were normal. It was suspected that bile duct's dilatation was due to abdominal giant cyst's pressure. Abdominal CT findings were consistent with US (Fig. 1). She was operated with the differential diagnosis of duplication, omental or mesenteric cyst. At operation, a giant type 1a choledochal cyst, 160 mm in diameter, was surprisingly detected (Fig. 2). Roux-en Y hepaticojejeunostomy procedure was performed. Serum levels of bilirubin decreased sharply and the patient was discharged without any problems on the tenth postoperative day.
Fig. 1. Abdominal computed tomography shows a giant cyst pushing on the kidneys (A) and some dilation of the intrahepatic bile ducts (B; arrow).
Fig. 2. Macroscopic appearance of the choledochal cyst (>16 cm).
Discussion
A choledochal cyst is a dilation that encloses the intrahepatic or both extra- and intrahepatic portions of the biliary ducts2). It is classified by Todani et al.3). Type Ia is a cystic dilation of the CBD; type Ib is a focal segmental dilation of the distal CBD; type Ic is a fusiform dilation of both the common hepatic duct and CBD. In type II, the cyst forms a diverticulum from the extrahepatic bile duct. Type III, also known as choledochocele, is a dilation of the distal CBD lying mainly within the duodenal wall. Type IV is essentially type I anatomy with either intrahepatic bile duct cyst (IVa) or choledochocele (IVb). Some authors refer to Caroli's disease with multiple cystic dilations of the intrahepatic biliary tree as type V2,3). In our case there was a cystic dilation of the CBD as a type Ia choledochal cyst with minimal dilatation of intrahepatic bile ducts.
This malformation primarily affects girls (4:1) and about 80% become symptomatic during childhood. Choledochal cysts remain relatively uncommon in Western Europe and the United States, although they are appreciably more common in Asia. Our patient is an immigrant from the Syria.
Symptoms depend on the age at presentation. Obstructive jaundice is the main presentation symptom in children, but abdominal pain is the commonest symptom in adults. Acute symptoms suggest the presence of complications such as perforation or pancreatitis. The classical triad of pain, jaundice and a palpable mass is uncommon, occurring in no more than 6% in one UK series4). The complications of congenital cystic dilatation of the bile duct are biliary stone formation, progressive biliary cirrhosis with portal hypertension, and carcinoma. Choledochal morphology may affect the type of symptom. Fusiform lesions are never large enough to be palpable while multiple intrahepatic type 4 lesions cause predisposition to stone formation and sepsis.
A wide variety of imaging techniques are available which noninvasively reconstruct biliary anatomy and give an excellent idea of biliary function. Although US is the first described imaging method to determine the CBD cyst, CT, MRCP, and ERCP are superior to assess the extention of the cyst and associated pathologies such as cholangitis, pancreatitis and pancreaticobiliary junction anomaly. In our case, we used US and CT to identify the abdominal mass' origin. Because of the diameter of the cyst, CBD cyst was not thought in the differential diagnosis. For the reasons cited above we did not perform the other imaging modalities. CBD malformations should be kept in mind as a differential diagnosis of the cystic mass regardless of size, and patient's age.
Surgery is the main choice of treatment but some centres in South American and Asia have reported ERCP and sphincterotomy alone as definitive treatment for mild fusiform dilatation although their long-term prognosis is not known3).
At operation, it was difficult to make the differential diagnosis of our giant cyst. The cyst was not originated from ovary, omentum or intestine. It was important to make the dissection of the cyst carefully in order to avoid the iatrogenic injury. Following the diagnosis of choledochal cyst was confirmed, hepaticojejunostomy was easier depending on the wide common hepatic duct of our huge cyst.
Tang et al.5) reported a study that involves 62 children (average age of 2.3 years) who had cysts with the average diameter of 42 mm (range, 12–158 mm). There is no information about the child'a age with the 158-mm cyst. As our knowledge we report the biggest choledocal cyst case in infancy in the literature.
In conclusion, CBD malformations should be kept in mind as a differential diagnosis at the cystic mass regardless of cyst's size, and patient's age, especially in children presented with abdominal pain, jaundice, and palpable mass.
Footnotes
Conflicts of interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Guelrud M, Morera C, Rodriguez M, Jaen D, Pierre R. Sphincter of Oddi dysfunction in children with recurrent pancreatitis and anomalous pancreaticobiliary union: an etiologic concept. Gastrointest Endosc. 1999;50:194–199. doi: 10.1016/s0016-5107(99)70224-5. [DOI] [PubMed] [Google Scholar]
- 2.Kerkar N, Norton K, Suchy FJ. The hepatic fibrocystic diseases. Clin Liver Dis. 2006;10:55–71. doi: 10.1016/j.cld.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263–269. doi: 10.1016/0002-9610(77)90359-2. [DOI] [PubMed] [Google Scholar]
- 4.Stringer MD, Dhawan A, Davenport M, Mieli-Vergani G, Mowat AP, Howard ER. Choledochal cysts: lessons from a 20 year experience. Arch Dis Child. 1995;73:528–531. doi: 10.1136/adc.73.6.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tang ST, Yang Y, Wang Y, Mao YZ, Li SW, Tong QS, et al. Laparoscopic choledochal cyst excision, hepaticojejunostomy, and extracorporeal Roux-en-Y anastomosis: a technical skill and intermediate-term report in 62 cases. Surg Endosc. 2011;25:416–422. doi: 10.1007/s00464-010-1183-y. [DOI] [PubMed] [Google Scholar]