Abstract
Background
Despite common use of proprioceptive retraining interventions in people with chronic, idiopathic neck pain, evidence that proprioceptive dysfunction exists in this population is lacking. Determining whether proprioceptive dysfunction exists in people with chronic neck pain has clear implications for treatment prescription.
Purpose
The aim of this study was to synthesize and critically appraise all evidence evaluating proprioceptive dysfunction in people with chronic, idiopathic neck pain by completing a systematic review and meta-analysis.
Data Sources
MEDLINE, CINAHL, PubMed, Allied and Complementary Medicine, EMBASE, Academic Search Premier, Scopus, Physiotherapy Evidence Database (PEDro), and Cochrane Collaboration databases were searched.
Study Selection
All published studies that compared neck proprioception (joint position sense) between a chronic, idiopathic neck pain sample and asymptomatic controls were included.
Data Extraction
Two independent reviewers extracted relevant population and proprioception data and assessed methodological quality using a modified Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement.
Data Synthesis
Thirteen studies were included in the present review. Meta-analysis on 10 studies demonstrated that people with chronic neck pain perform significantly worse on head-to-neutral repositioning tests, with a moderate standardized mean difference of 0.44 (95% confidence interval=0.25, 0.63). Two studies evaluated head repositioning using trunk movement (no active head movement thus hypothesized to remove vestibular input) and showed conflicting results. Three studies evaluated complex or postural repositioning tests; postural repositioning was no different between groups, and complex movement tests were impaired only in participants with chronic neck pain if error was continuously evaluated throughout the movement.
Limitations
A paucity of studies evaluating complex or postural repositioning tests does not permit any solid conclusions about them.
Conclusions
People with chronic, idiopathic neck pain are worse than asymptomatic controls at head-to-neutral repositioning tests.
Neck pain is estimated to affect 10% to 20% of the population every year (with a global point prevalence of 4.9%)1,2 and up to two thirds of people at some point in their life.3 It carries a large personal burden; it is second only to back pain in disability-adjusted life-years (DALYs) and represents one fifth of total DALYs attributed to musculoskeletal conditions.4 Although neck pain is generally thought to have a favorable prognosis, one third of people go on to develop chronic neck pain.5 Furthermore, pain severity remains high 12 months following the onset of idiopathic neck pain.6 In Australia alone, chronic pain costs $34.3 billion annually (direct and indirect costs); neck pain is the fifth largest contributor to this cost.7
Although neck pain can be attributed to traumatic disorders (eg, fracture, whiplash-associated disorder) or inflammatory disorders,8 the majority of neck pain does not have a discernible cause and is considered idiopathic. Clinical practice guidelines for chronic neck pain recommend conservative treatment, including exercise and manual therapy, guided by impairment- and function-related assessment of the neck.9 Clinical texts specifically recommend the assessment and management of proprioceptive dysfunction for people with neck pain.10 Joint position sense (JPS) or joint position error (JPE) is often used to evaluate proprioceptive ability, and the most commonly used test involves assessing an individual's ability to relocate to neutral head and neck posturing (or to a target position) after active or passive neck movement.10
Evidence from randomized controlled trials suggests that proprioceptive-targeted treatment improves JPS at the neck and results in pain reduction.11,12 However, despite the fact that assessment and retraining of proprioceptive function has become part of musculoskeletal practice,13 clear evidence that proprioceptive dysfunction occurs in people with idiopathic neck pain is lacking. To date, there has been no attempt to systematically evaluate the evidence in this area.
This lack of evidence for proprioceptive dysfunction in idiopathic neck pain has important implications for understanding the mechanism by which proprioceptive-targeted treatments might work. For example, should people with nontraumatic neck pain not have proprioceptive dysfunction compared with healthy controls, this finding would suggest that proprioceptive-targeted treatment is unlikely to be exerting its effect on pain by addressing biomechanical contributors to pain or that the improvement in JPS seen in proprioceptive-targeted treatment may be a natural feature of recovery. Thus, we aimed to synthesize and critically appraise the evidence by completing a systematic review and meta-analysis to determine whether people with chronic idiopathic neck pain have proprioceptive dysfunction compared with those without neck pain.
Method
Data Sources and Searches
Studies were identified through electronic searches on the following databases from their relative date of inception to August 30, 2014: MEDLINE (via OvidSP), CINAHL (via EBSCOhost), PubMed, Allied and Complementary Medicine (via OvidSP), EMBASE (via OvidSP), Academic Search Premier (via EBSCOhost), Scopus, Cochrane Collaboration, and Physiotherapy Evidence Database (PEDro).
Key words related to joint position sense, neck, and pain were used in the search strategy. Relevant subject headings were determined specifically for each database (see Appendix 1 for the MEDLINE search strategy). In all studies for which full text was retrieved, the reference lists were manually searched to identify additional potentially eligible studies. We conducted this review using an a priori protocol (available from Dr Stanton upon request).
Study Selection
Studies were included if they recruited human adults (≥18 years of age) with chronic idiopathic neck pain (>3 months), reported a measure of neck proprioception, and compared neck proprioception performance of participants with neck pain with either a pain-free control group or with values from a normative database.
Studies were excluded if neck pain was due to a specific cause (eg, traumatic injury, whiplash-associated disorder), if experimental neck pain was evaluated, or if participants had a previous history of neck surgery. Furthermore, presence of a concurrent condition that could affect JPS or accuracy of reporting (eg, Alzheimer disease, dementia, traumatic brain injury), known disease affecting the nervous system (eg, multiple sclerosis, stroke, Parkinson disease), and known disease affecting the vestibular system (eg, Ménière disease, benign paroxysmal positional vertigo) resulted in exclusion. In terms of study design restrictions, only case studies were excluded.
Titles and abstracts of the studies identified by the search strategy were independently screened by 2 reviewers (H.B.L. and K.J.C.) to determine potentially relevant studies. Full texts of potentially relevant studies were retrieved and evaluated for eligibility by the same reviewers. Any disagreements were resolved via consensus; if consensus could not be reached, a third, independent reviewer (T.R.S.) resolved the dispute.
Data Extraction and Quality Assessment
Data extraction was performed by 2 independent reviewers (H.B.L. and K.J.C.) using a customized, pilot-tested data extraction form. Any discrepancies between reviewers were resolved via consensus or consultation with a third reviewer (T.R.S.). Relevant data were extracted, including: author, date, study design, sample size, participant demographics (age, sex, pain duration), condition-specific information (pain intensity, pain duration, neck-related disability), method of proprioceptive assessment (equipment used, measurement method), proprioceptive outcome measure used (absolute repositioning error, constant error), and repositioning results specific to each group (mean or median, standard deviation or interquartile range). When data were missing, authors were emailed a maximum of 3 times, after which data were considered unretrievable.
Due to the lack of an agreed-upon “gold standard” critical appraisal tool for observational studies, the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)14 was used to guide risk of bias assessment at an individual study level. Items relevant to bias in case-control study designs also were assessed (Appendix 2). Studies were independently assessed by 2 reviewers (H.B.L. and K.J.C.), and disagreements were resolved by consensus.
Data Synthesis and Analysis
For the purposes of this review, data were analyzed in 3 groups: (1) head-to-neutral repositioning tests; (2) vestibular controlled head repositioning tests (head stationary, trunk movement used to achieve relative head movement); and (3) complex or postural repositioning tests (tests involving complex movement or postural patterns that differed from traditional repositioning tests). For head-to-neutral repositioning tests, results were subgrouped based on the type of neck and head movement assessed (eg, rotation, flexion, extension, side flexion).
Due to differences in JPS outcomes used (absolute error and constant error) and the units of these outcomes (centimeters versus degrees), standardized mean differences (SMDs) were calculated to compare results among studies. Standardized mean differences were calculated by subtracting the mean JPS of the asymptomatic population from the mean JPS of the neck pain population and dividing this result by the pooled standard deviation of JPS from both populations. The size of the effect was interpreted using Cohen's recommendations, where d=0.2, d=0.5, and d=0.8 represent small, moderate, and large effects, respectively.15
Data were pooled with Review Manager 5.2 software16 using a random effects inverse-variance approach. Pooling was considered when 2 or more studies provided results on similar neck proprioceptive tasks, using similar proprioceptive outcomes. When a single study reported multiple tests (ie, measured JPS for both flexion and rotation) on the same sample, the sample size was adjusted appropriately in the analysis. Furthermore, when studies reported JPS for left- and right-sided movements separately (eg, left rotation and right rotation), if these values were not significantly different, an average of the means and variances was taken to produce one value. When more than one measurement system was used to evaluate JPS within a study, the system with the highest reliability and accuracy was used for pooling. Last, a post hoc sensitivity analysis was performed for head-to-neutral repositioning tests evaluating only subgroup pooled effects (no overall pooled effect). This analysis allowed us to characterize subgroup effect size estimates without the sample size reductions necessary when estimating overall pooled effect.
The chi-square test was used to detect statistically significant heterogeneity, and the I2 statistic was used to estimate the amount of heterogeneity. Statistically significant heterogeneity was considered present when P<.10 for the chi-square test. Substantial heterogeneity was considered present when I2>60%.17 Last, tau—the estimated SD of the underlying effects across studies—was used to convey the absolute between-study variability of these effects (ie, on the same scale as that used for SMDs). When applicable, we added and subtracted (2 × tau) from the pooled effect, resulting in an approximate 95% range of underlying effects (ie, in the range that 95% of the effects would lie).
Role of the Funding Source
Dr Stanton was supported by a Canadian Institute for Health Research Postdoctoral Training Fellowship (ID223354) and a National Health and Medical Research Council Early Career Fellowship (ID 1054041). Dr Moseley was supported by a National Health and Medical Research Council Research Fellowship (ID1061279). The funders played no role in study design, collection, analysis, interpretation of data, writing of the report, or the decision to submit the manuscript for publication. They accept no responsibility for the content.
Results
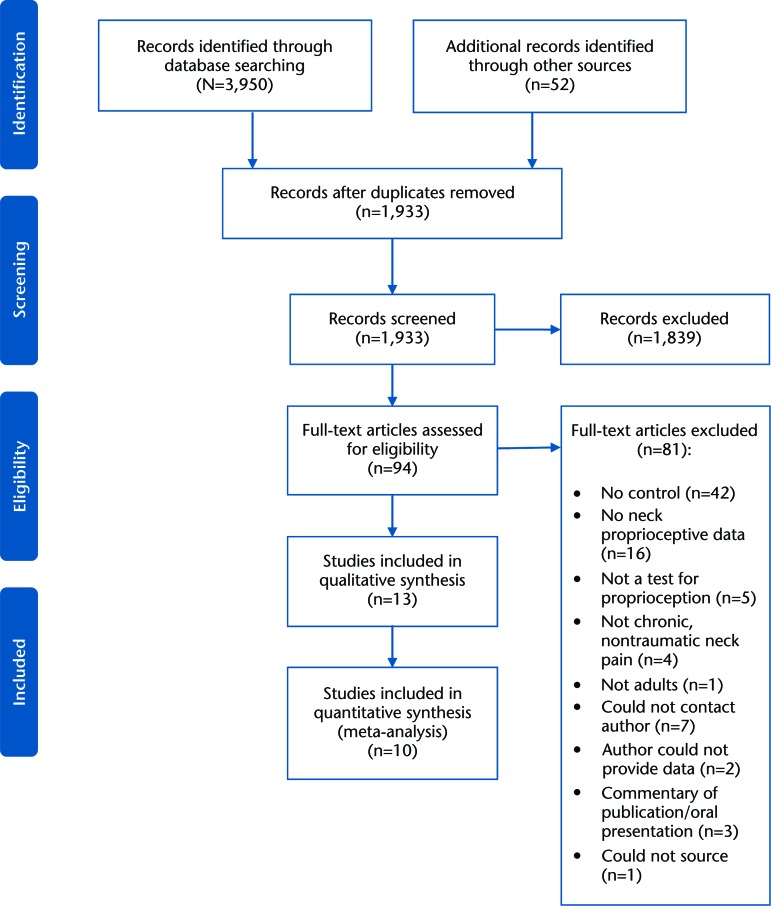
The search strategy resulted in 1,933 potentially relevant studies, following removal of duplicates. Of these potentially relevant studies, 1,839 were excluded on the basis of title and abstract review; the full text was retrieved for 94 studies. Of these 94 studies, 10 authors were emailed to confirm if eligibility criteria were met: 1 author provided data specific to nontraumatic neck pain (original study had a mixed sample of participants with traumatic and nontraumatic neck pain), allowing for study inclusion18; 2 authors confirmed that further information could not be supplied (resulting in exclusion of the studies)12,19; and the remaining authors20–26 could not be contacted (maximum of 3 email attempts), thus these articles were excluded (unsure if chronic, idiopathic pain). Eighty-one studies did not meet the eligibility criteria, resulting in inclusion of 13 studies in the present review18,27–38 (see Fig. 1 for the PRISMA flow diagram). The most common reason for study exclusion was lack of a healthy control group.
Figure 1.
The PRISMA flow diagram describing the screening and review process.
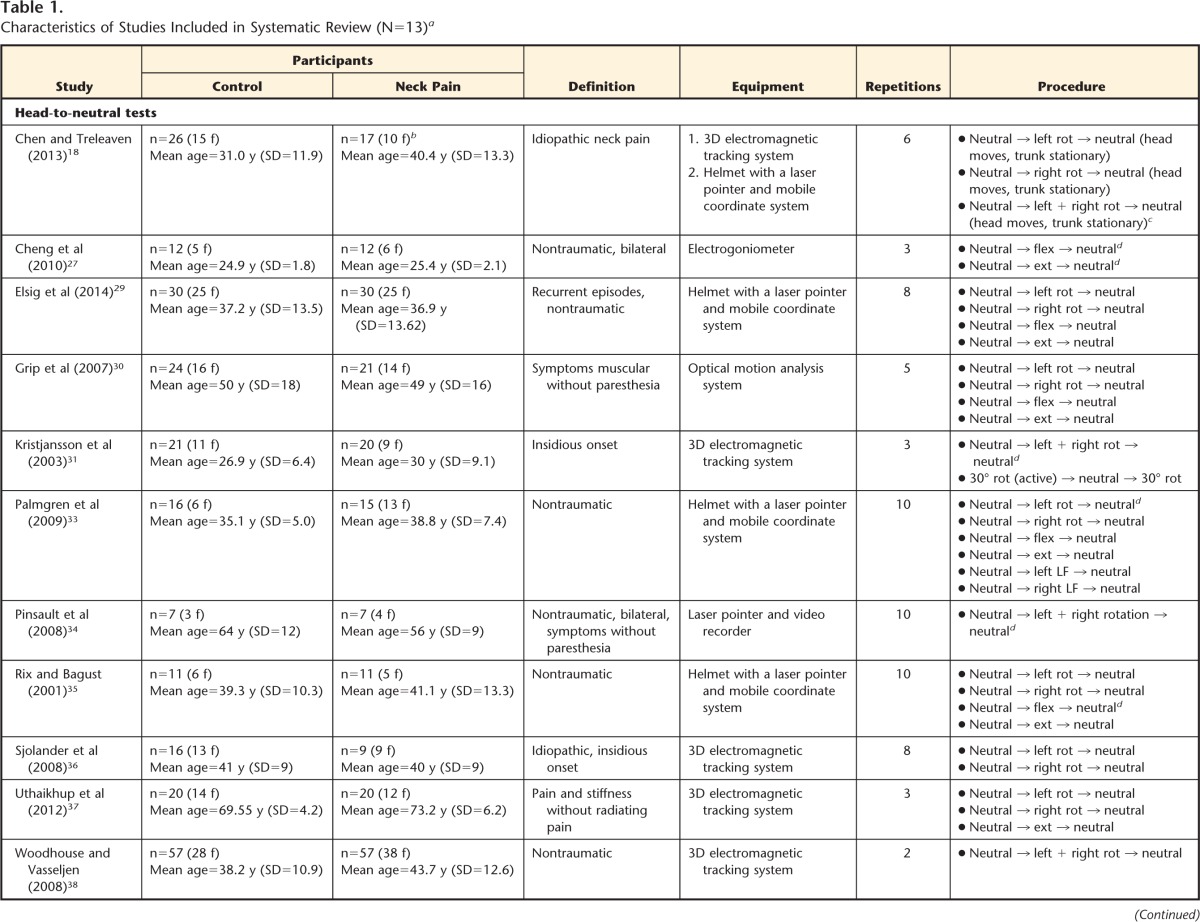
Characteristics of Included Studies
In the 13 studies, 587 participants (286 with idiopathic neck pain, 301 controls) underwent testing of cervical JPS (see Tab. 1 for full summary details). The mean number of participants per study was 42 (SD=24), with a mean age of 39.8 years (SD=12.9). All participants with neck pain had pain for at least 3 months, although there was little overall consistency in eligibility criteria across studies. All but one study18 excluded patients with a current or past history of neck trauma (however, data for patients without trauma were received from that study18). The authors of 9 studies explicitly stated that participants with neurological impairment specific to the neck were excluded,18,27–30,34–37 and the authors of 4 studies explicitly stated that they excluded participants with vestibular impairment.18,29,33,36
Table 1.
Characteristics of Studies Included in Systematic Review (N=13)a
n=number of participants recruited (prior to dropout or loss to follow-up), f=female, LF=lateral flexion, rot=rotation, ext=extension, flex=flexion, 3D=3-dimensional, Cx=cervical, VAS=visual analog scale.
b Additional information provided by author.
c Significant difference (P<.05) between participants with neck pain and healthy controls for the helmet with laser pointer test of Chen and Treleaven.18
d Significant difference (P<.05) between participants with neck pain and healthy controls.
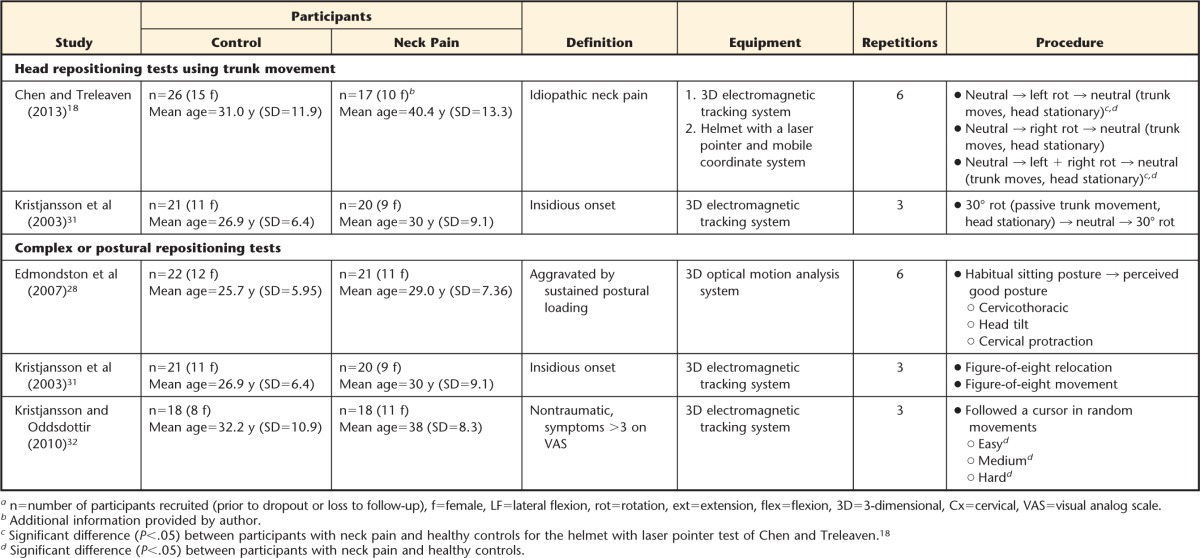
Risk of Bias of Included Studies
The results of the risk of bias assessment are shown in Table 2. Critical appraisal revealed a spread in methodological quality. Common areas of bias were lack of use of accepted diagnostic criteria for chronic neck pain and lack of reporting of validity and reliability of all proprioceptive measurement tools. Furthermore, all studies had high selection bias (no study reported randomly selecting or consecutively recruiting participants), and only 31% of the studies (4/13) blinded the outcome assessor to participant group. Agreement between reviewers was high, with 95% scoring agreement.
Table 2.
Results of Critical Appraisal of Studies Using the Modified Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statementa
✓=yes, ✗=no, ?=unclear.
Characteristics of Proprioceptive Test Methodology and Measurement
Various methods were used to evaluate JPS; however, active head repositioning was used in all studies. Repetitions of each test varied from 2 to 10. Vision was occluded in 11 studies; 2 studies reported testing participants with eyes open (1 evaluating head-to-neutral repositioning27 and 1 evaluating complex repositioning and movement32). Speed of movement instructions and the amount of movement requested (eg, submaximal neck movement versus maximal) varied among included studies. Participants were placed in a seated, stabilized position during proprioceptive testing, with the exception of one study36 that evaluated neck JPS in a standing position.
Various types of equipment were used to evaluate JPS. Six studies used an electromagnetic tracking system,18,31,32,36–38 4 studies used a helmet with a laser pointer and mobile coordinate system,18,29,33,35 2 studies used a 3-dimensional (3D) optical motion analysis system,28,30 1 study used an electrogoniometer,27 and another study used a video recorder and laser pointer.34 Most studies reported JPS in degrees; however, 2 studies reported JPS in metric units (centimeters or millimeters).32,33 Most studies reported JPS as an absolute error (some calculating this measure via root mean square error27,29,35), although 2 studies reported constant error36 and amplitude accuracy.32
Joint Reposition Sense Outcomes
Four authors were contacted for further JPS information; the authors of 3 studies28,29,33 provided the needed data. One author was unable to provide the necessary data35; thus, this study could not be included in the meta-analysis.
Head-to-neutral repositioning tests (passive movement of the head to test position).
Eleven studies performed 31 tests that involved relocation to the neutral head position following passive head and neck movement into flexion, extension, rotation, or lateral flexion. Joint position sense was calculated as the difference between the initial neutral position and the final neutral position returned to after movement. Left- and right-sided data were averaged to produce one JPS value in 4 studies evaluating head-to-neutral repositioning from rotation30,33,36,37 and in 1 study evaluating head-to-neutral repositioning from lateral flexion.33 Combined with insufficient data from 1 study (evaluating 4 tests),35 use of modified JPS evaluation precluding pooling in 1 study,31 and use of 2 measurement systems for the same JPS outcome in 1 study (only one result pooled),18 this evaluation resulted in pooling of data from 19 head-to-neutral repositioning tests.
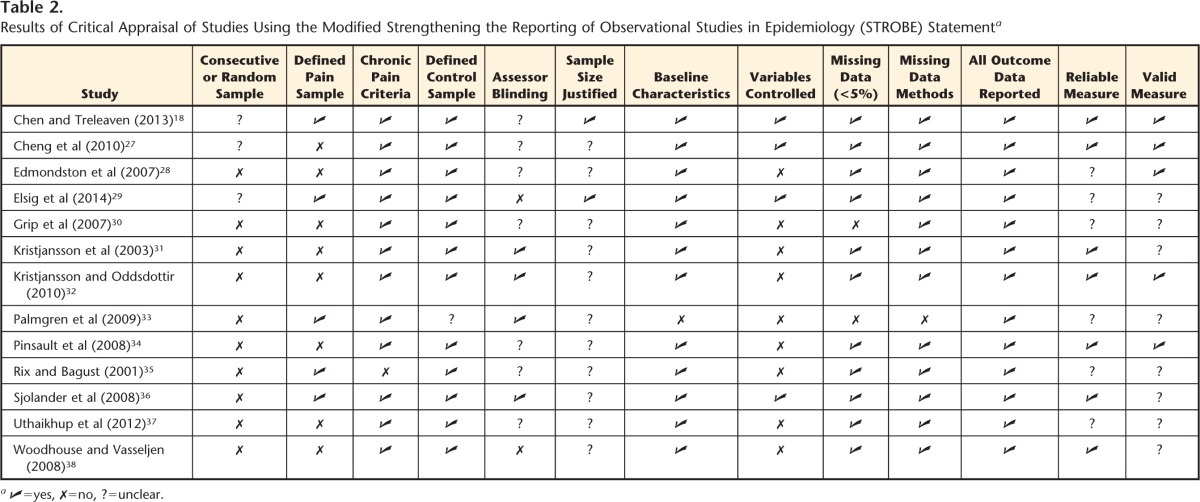
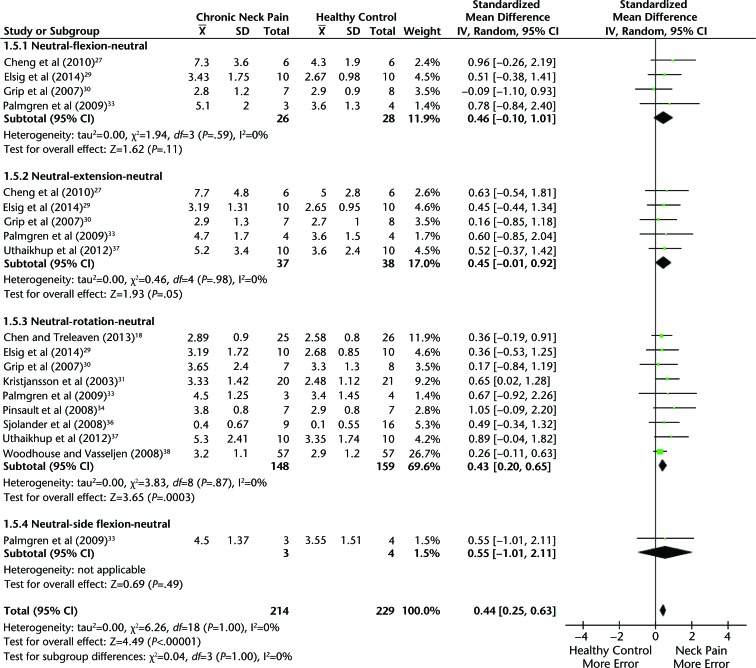
Pooled data showed an overall significant moderate effect of 0.44 (95% confidence interval [CI]=0.25, 0.63; Fig. 2), indicating that participants with chronic, idiopathic neck pain performed worse on a head-to-neutral repositioning test compared with asymptomatic controls. Heterogeneity was low (I2=0%, χ2=6.26, P=1.0, tau=0.00). Subgroup data were largely consistent with this overall effect: 9 studies provided data for head-to-neutral repositioning from rotation, and pooling resulted in a significant moderate effect of 0.43 (95% CI=0.20, 0.65), suggesting that people with neck pain were significantly worse than healthy controls. Again, heterogeneity was low (I2=0%, χ2=3.83, P=.87, tau=0.00). For the rotation subgroup, Chen and Treleaven18 also evaluated JPS using a laser system (3D electromagnetic tracking system data presented in the forest plot) and, consistent with pooled results, found that participants with neck pain had significantly worse JPS than healthy controls (SMD=0.67; 95% CI=0.04, 1.30). Four studies provided data on head-to-neutral repositioning from flexion,18,29,30,33 5 studies evaluated extension,18,29,30,33,37 and 1 study evaluated lateral flexion.33 Pooling the data of these subgroups showed no significant effect for flexion (SMD=0.46; 95% CI=−0.10, 1.01), extension (SMD=0.45, 95% CI=−0.01, 0.92), or lateral flexion (SMD=0.55; 95% CI=−1.01, 2.11). Heterogeneity was low for flexion (I2=0%, χ2=1.94, P=.59, tau=0.00) and extension (I2=0%, χ2=0.46, P=.98, tau=0.00).
Figure 2.
Meta-analysis of head-to-neutral proprioceptive repositioning tests. All sample sizes have been reduced to reflect the number of times each study appears in the forest plot. IV=inverse variance, CI=confidence interval.
Rix and Bagust35 (data unable to be pooled) found that people with chronic, idiopathic neck pain were significantly worse than healthy controls when performing relocation to the neutral head position from flexion (P<.03). There were no significant differences between groups (P>.05) for relocation tasks from neck extension or rotation (left or right). Additionally, one study used a variation of the repositioning test that involved participants actively repositioning the head to 30 degrees of neck rotation from a neutral head start position.31 There was no significant difference between groups in error values (SMD=0.44; 95% CI=−0.22, 1.01).
Post hoc sensitivity analysis of main effects for each repositioning test.
We performed this analysis to determine whether the nonsignificant results in subgroups of flexion and extension were due to inadequate power as a result of using sample size reductions for studies that appeared in numerous subgroups (necessary when calculating an overall pooled effect). That the rotation subgroup (9 studies) showed a significant effect but flexion (4 studies) and extension (5 studies) did not, despite similar individual study effect estimates, suggests that this explanation is possible. Thus, we completed a sensitivity analysis that only calculated subgroup pooled effects (ie, full sample size for each study used). This sensitivity analysis confirmed that there was a significant moderate effect estimate for flexion, extension, and rotation subgroups of head-to-neutral repositioning tests, such that people with chronic neck pain performed significantly worse than healthy controls (eFigure).
Head repositioning tests using trunk movement to achieve head and neck position.
Two studies also evaluated rotation JPS using repositioning tests that involved trunk movement to achieve relative head and neck rotation (aiming to remove the influence of vestibular afferents). In one study, participants actively repositioned the head to 30 degrees of neck rotation from a neutral head position, but the initial target position (30° of neck rotation) was achieved by holding the head still and passively moving the trunk.31 There were no significant differences between individuals with neck pain and healthy controls (SMD=0.28; 95% CI=−0.34, 0.89). In the second study, the participant's head was held still for the entire test; the participant actively moved the trunk until the head reached maximal rotation and then actively moved the trunk to relocate the head to a neutral head posturing (labeled “torsion test”).18 Significant impairment in JPS was found in participants with chronic, idiopathic neck pain compared with healthy controls when using an electromagnetic tracking system to evaluate JPS (SMD=0.77; 95% CI=0.20, 1.34), and close to significant effects were found when using a laser pointer system (SMD=0.54; 95% CI=−0.02, 1.10).
Complex or postural repositioning tests.
Three studies used 3 different methods of testing cervical JPS that involved complex or postural repositioning tests. A meta-analysis was not performed on these studies due to differences in JPS assessment methods and differences in the constructs evaluated by these tests.
In one study31 that evaluated complex movement patterns, participants traced a figure-of-eight pattern with their nose, with the aim to return to a neutral position after one repetition (test 4 [relocation task]) or 3 repetitions (test 5 [movement test]). There were no significant differences between participants with neck pain and healthy controls for either test 4 (SMD=0.07; 95% CI=−0.54, 0.68) or test 5 (SMD=−0.32; 95% CI=−0.93, 0.30).
The second study evaluated a combination of repositioning ability and postural memory or sufficiency.28 Participants performed a repositioning test to a self-determined “perceived good posture” from a fully relaxed position. In this perceived good posture position, cervicothoracic angle (CT), head tilt (HT), and cervical protraction (CP) were measured. Errors were calculated by taking the difference between the initial perceived good posture positioning (CT, HT, CP) and 6 relocation tests where participants aimed to replicate the initial perceived good posture position (CT, HT, CP). There were no significant differences between healthy controls and participants with neck pain for CT (SMD=0.60; 95% CI=−0.01, 1.22), HT (SMD=0.16; 95% CI=−0.44, 0.76), or CP (SMD=−0.31; 95% CI=−0.91, 0.29).
Last, one study evaluated JPS using a new method termed “The Fly.”32 In this method, participants followed a moving cursor (the “fly”) on a screen using another cursor aligned to their head position (eyes open during testing). Error (calculated as the distance between cursors) was continuously evaluated. Three tests were performed that differed based on movement pattern difficulty (easy, medium, and difficult). Using this method of JPS evaluation, significant differences were found whereby participants with chronic, nonspecific neck pain performed worse than asymptomatic controls at easy (SMD=0.68; 95% CI=0.01, 1.36), medium (SMD=0.68; 95% CI=0.00, 1.35), and difficult (SMD=0.81; 95% CI=0.12, 1.49) test levels.
Discussion
This systematic review and meta-analysis aimed to synthesize and critically appraise the available evidence for proprioceptive dysfunction in people with chronic, idiopathic neck pain by comparing their JPS with that of asymptomatic controls. Pooled estimates showed that people with chronic, idiopathic neck pain have moderately impaired cervical JPS on head-to-neutral repositioning tests compared with asymptomatic controls. There is limited and conflicting evidence that head repositioning tests that aim to remove the influence of vestibular input (head still, trunk movement) and complex or postural repositioning tests are impaired in people with chronic, idiopathic neck pain.
Strengths and Limitations of the Review
To our knowledge, this is the first review to systematically evaluate cervical JPS in an idiopathic neck pain population. This review conformed to the guidelines suggested by PRISMA,39 and strengths of this review include the use of robust methodology (such as 2 independent reviewers and a sensitive search strategy) and the inclusion of studies not published in English. Although multiple databases were searched, it is possible that a relevant study may have been missed. Thorough searching of relevant studies' lists used in this review likely minimized this possibility.
There are relevant limitations with respect to the level of evidence present: JPS assessment methods varied among the included studies, participants were not randomly or consecutively sampled, sample sizes were generally small, and some studies had baseline differences between neck pain and control groups. Importantly, there was no consistent definition of idiopathic neck pain. Some studies excluded neurological and vestibular disorders, but others did not explicitly state that they excluded these conditions. Last, neck pain severity varied among studies; however, this variation in pain severity also suggests that our findings are likely generalizable.
Head-to-Neutral Repositioning Tests
Despite the variability in methods used in the included studies, consistent between-study and between-subgroup effects were seen in the head-to-neutral repositioning tests, suggesting that people with chronic, idiopathic neck pain have poorer performance than asymptomatic controls. Although rotation was the only subgroup to show a significant effect estimate, the sensitivity analysis suggests that this finding was likely due to the flexion and extension subgroups being underpowered once sample sizes were reduced to control for multiple appearances in the meta-analysis. This interpretation is supported by the overlap of studies among subgroups: the study by Cheng et al27 was the only study in the flexion and extension subgroups not also included in the rotation subgroup.
Past research suggests that age may affect JPS, such that as age increases, JPS reduces.40 This hypothesis is supported by findings suggesting that changes in visual, vestibular, and neuromuscular function occur with advancing age.41 The present review suggests that, if age does affect JPS, pain likely has a unique effect above and beyond that of age. Uthaikhup et al37 recruited elderly participants with neck pain and age-matched controls and found proprioceptive dysfunction similar to that seen in younger cohort comparisons (Fig. 1, eFigure). However, the literature on the relationship between age and JPS is conflicting,40,42 suggesting that there may be other factors beyond age that influence JPS.
The absolute difference in JPS (error) between people with chronic neck pain and healthy controls in the tests ranged from 0.1 to 3.0 degrees. The precision of many of the JPS measuring systems ranges from 0.1 to 0.5 degrees.19,27,43 However, such a small difference would not be reliably detectable using clinical methods such as universal goniometry or visual estimation.44 It is unclear what degree of error represents a clinically meaningful impairment in JPS. However, the functional relevance of accurate head movements to facilitate behaviorally appropriate head orientation suggests that precision within this system is essential and thus that even small impairments may be important.
Head Repositioning Tests Using Trunk Movement
One criticism of traditional head repositioning tests is that active head movement during the test may stimulate both neck and vestibular afferents18,45 and thus not specifically measure proprioception. Differentiation of system dysfunction may be important for guiding treatment. Thus, modifications of the traditional JPS tests have been suggested that are more likely to selectively stimulate cervical afferents while avoiding vestibular involvement. In this modified test, the head is kept stationary, and trunk movement is used to induce relative head and neck rotation.18,31 Theoretically, this test would eliminate the vestibular system fully, and only proprioceptive input from the neck would be used to monitor head position.46 Only 2 studies evaluated a modified JPS test that used trunk movement, and they showed conflicting results. One study used passive trunk rotation to induce a neutral head start position (from 30° of neck rotation), with use of active neck rotation to return to the 30 degrees of rotation, and showed no difference between groups.31 The other study used active trunk rotation to induce a maximal neck rotation start position (from a neutral start position), with use of active trunk movement to relocate the head to neutral (thus, with vestibular involvement removed for the whole time), and showed significant impairment in participants with neck pain.18 Thus, based on the limited evidence, it is unclear whether JPS results are specific to proprioceptive dysfunction or whether they include vestibular involvement. Furthermore, nonsignificant findings may be similar to the head-to-neutral repositioning tests whereby single study findings were nonsignificant, but the pooled results were significant. More testing is clearly needed to investigate this theory.
Complex or Postural Repositioning Tests
The evidence for complex or postural repositioning tests is limited and presents conflicting results. Tasks involving repositioning to a “perceived” good postural position showed no differences in error between individuals with neck pain and healthy controls.28 Notably, the reliability and validity of this postural repositioning test to assess proprioception is unknown; therefore, it is unclear how much weight to give to these results. Furthermore, previous work has postulated that tests that are too simple or familiar may be unable to detect proprioceptive dysfunction.47,48 It is interesting to consider that tests requiring repositioning to a self-selected posture28 may reflect an innate postural characteristic that is relatively easy for the individual to reproduce, and unfamiliar postures, defined by the investigator, may show greater differences.
Two studies evaluated complex movement patterns; these findings extend beyond merely proprioceptive evaluation and assess the functional performance of the dynamic feedback system involved in movement control, coordination, and execution as a whole. When error was continuously measured during standardized movement patterns, people with neck pain were significantly less accurate than healthy controls.32 However, when error was evaluated using one point of this movement (figure-of-eight movement pattern of the head, using nose to trace the pattern; error measured at the neutral head position), there were no differences between groups.31 It is perhaps unsurprising that continuously monitored movement would be more sensitive to change or dysfunction than measurement at one point within the movement. Furthermore, it is interesting to consider whether tests that require participants to detect and correct error while performing movement (ie, through integration of visual feedback with motor processes) might detect more functionally relevant dysfunction.
Unanswered Questions and Future Directions
It remains unknown which proprioceptive tests may best reflect clinically relevant dysfunction. Furthermore, it is unclear if performance on certain proprioceptive tests is predictive of clinical outcome. Although some evidence suggests that targeting proprioception can result in improved outcomes in neck pain,11,12 a recent systematic review identified a lack of high-quality studies evaluating proprioceptive training interventions in people with neck or back pain.49 Such knowledge would provide important information for both researchers and clinicians and could possibly direct more individually targeted intervention. Additionally, future testing of proprioceptive dysfunction, regardless of whether determining impairment in a clinical population or evaluating treatment outcomes, would benefit from blinded assessment.
That people with chronic, idiopathic neck pain demonstrate impaired neck proprioception raises the question of where this impairment occurs. There is no inciting trauma or injury in this condition, so it would seem less likely that peripheral mechanoreceptors would be affected. Experimental studies often evaluate the peripheral contribution to proprioception by inducing experimental pain or by impairing muscle spindle function; however, neither approach supports peripheral dysfunction as a sole explanation for the findings of the present review. In experimental neck pain (saline injections into the splenius capitis muscle), JPS is impaired only during head-to-target testing (and only in the rotation direction that evokes pain); head-to-neutral position sense is not impaired.50 This finding suggests that noxious stimuli can influence proprioceptive performance, but only when pain is elicited, which makes it unlikely to explain our review's results. In addition, muscle vibration studies demonstrate that although this method of biasing muscle spindle input reduces the accuracy of JPS in healthy participants, it actually improves JPS acuity in people with neck pain51 and in people with low back pain.52 This finding suggests that the relationship between muscle spindle function and position sense is complex in painful conditions. These findings, in combination with the lack of trauma in idiopathic neck pain, raise the possibility that the proprioceptive dysfunction in idiopathic neck pain stems from spinal or supraspinal causes.
There is some evidence that people with idiopathic neck pain have impairment in implicit motor imagery performance; they are less accurate than healthy controls when making left and right judgments of images of neck and head rotation29 (ie, a task known to assess the function of cortical areas involved in planning, coordination, and execution of movement).53,54 New research has shown improvements in JPS acuity in people with neck pain during mental imagery and action observation, suggesting that changes in proprioceptive input are not a prerequisite for improved position sense.55 Future research could determine whether outcomes similar to those seen with proprioceptive training in people with neck pain (increased proprioceptive acuity and decreased pain) could be attained by targeting these cortical areas using tasks such as left or right judgments.
Appendix 1.
Appendix 1.
MEDLINE Search Strategya
a MH=MeSH heading, TX=text word.
Appendix 2.
Appendix 2.
Risk of Bias Assessment Questions (Informed by Strengthening the Reporting of Observational Studies in Epidemiology [STROBE] Statement Reporting Recommendations)
Footnotes
All authors provided concept/idea/research design. Dr Stanton, Ms Leake, and Professor Moseley provided writing. Dr Stanton, Ms Leake, and Mrs Chalmers provided data collection and data analysis. Dr Stanton provided project management. Professor Moseley provided fund procurement. Dr Stanton, Ms Leake, Mrs Chalmers, and Professor Moseley provided consultation (including review of manuscript before submission). The authors thank Dr Neil O'Connell for assistance with meta-analytical issues.
Dr Stanton was supported by a Canadian Institute for Health Research Postdoctoral Training Fellowship (ID223354) and a National Health & Medical Research Council Early Career Fellowship (ID 1054041). Dr Moseley was supported by a National Health and Medical Research Council Research Fellowship (ID1061279).
References
- 1. Hoy DG, Protani M, De R, Buchbinder R. The epidemiology of neck pain. Best Pract Res Clin Rheumatol. 2010;24:783–792. [DOI] [PubMed] [Google Scholar]
- 2. Hoy DG, March L, Woolf A, et al. The global burden of neck pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73:1309–1315. [DOI] [PubMed] [Google Scholar]
- 3. Côté P, Cassidy JD, Carroll L. The Saskatchewan Health and Back Pain Survey: the prevalence of neck pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976). 1998;23:1689–1698. [DOI] [PubMed] [Google Scholar]
- 4. Murray CJL, Vos T, Lozano R, Naghavi M, et al. Disability-adjusted life years (DALYs) for 291 disease and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–2223. [DOI] [PubMed] [Google Scholar]
- 5. Côté P, Cassidy JD, Carroll LJ, Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004;112:267–273. [DOI] [PubMed] [Google Scholar]
- 6. Hush JM, Lin CC, Michaleff ZA, et al. Prognosis of acute idiopathic neck pain is poor: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2011;92:824–829. [DOI] [PubMed] [Google Scholar]
- 7. The High Price of Pain: The Economic Impact of Persistent Pain in Australia. Sydney, New South Wales, Australia: Access Economics Pty Ltd; 2007. [Google Scholar]
- 8. Bogduk N. Neck pain: an update. Aust Fam Physician. 1988;17:75–80. [PubMed] [Google Scholar]
- 9. Childs JD, Clelland JA, Elliott JM, et al. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability and Health from the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38:A1–A34. [DOI] [PubMed] [Google Scholar]
- 10. Jull G, Falla D, Treleaven J, Sterling M. A therapeutic exercise approach for cervical disorders. In: Boylin JD, Jull GA, eds. Grieve's Modern Manual Therapy. 3rd ed London, United Kingdom: Churchill Livingstone; 2004:451–470. [Google Scholar]
- 11. Revel M, Minguet M, Gergory P, et al. Changes in cervicocephalic kinesthesia after a proprioceptive rehabilitation program in patients with neck pain: a randomized controlled study. Arch Phys Med Rehabil. 1994;75:895–899. [DOI] [PubMed] [Google Scholar]
- 12. Jull G, Falla D, Treleaven J, et al. Retraining cervical joint position sense: the effect of two exercise regimes. J Orthop Res. 2007;25:404–412. [DOI] [PubMed] [Google Scholar]
- 13. Porter SB, ed. Concepts in exercise rehabilitation. In: Tidy's Physiotherapy. 13th ed London, United Kingdom: Butterworth-Heinemann; 2003:471–503. [Google Scholar]
- 14. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cohen J. Statistical Power Analysis for the Behavioural Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1998. [Google Scholar]
- 16. Cochrane Collaboration. Review Manager (Revman). Copenhagen: Nordic Cochrane Centre; 2011. [Google Scholar]
- 17. Higgins JPT, Green S. Cochrane Handbook for Systematic Review of Interventions. Version 5.1.0. 2011. Available at: http://handbook.cochrane.org/ Accessed January 4, 2015.
- 18. Chen X, Treleaven J. The effect of neck torsion on joint position error in subjects with chronic neck pain. Man Ther. 2013;18:562–567. [DOI] [PubMed] [Google Scholar]
- 19. Roren A, Mayoux-Benhamou MA, Fayad F, et al. Comparison of visual and ultrasound based techniques to measure head repositioning in healthy and neck-pain subjects. Man Ther. 2009;14:270–277. [DOI] [PubMed] [Google Scholar]
- 20. De Loose V, Van den Oord M, Burnotte F, et al. Functional assessment of the cervical spine in F-16 pilots with and without neck pain. Aviat Space Environ Med. 2009;80:477–481. [DOI] [PubMed] [Google Scholar]
- 21. Gemmell H, Dunford PJ. A cross-sectional study of the prevalence of neck pain, decreased cervical range of motion and head repositioning accuracy in forwards and backs in rugby union. Clin Chiropractic. 2007;10:187–194. [Google Scholar]
- 22. Nagai T, Abt JP, Sell TC, et al. Neck proprioception, strength, flexibility, and posture in pilots with and without neck pain history. Aviat Space Environ Med. 2014;85:529–535. [DOI] [PubMed] [Google Scholar]
- 23. Revel M, Andre-Deshays C, Minguet M. Cervicocephalic kinesthetic sensibility in patients with cervical pain. Arch Phys Med Rehabil. 1991;72:288–291. [PubMed] [Google Scholar]
- 24. Teng CC, Chai H, Lai DM, Wang SF. Cervicocephalic kinesthetic sensibility in young and middle-aged adults with or without a history of mild neck pain. Man Ther. 2007;12:22–28. [DOI] [PubMed] [Google Scholar]
- 25. Van den Oord MHAH, De Loose V, Sluiter JK, Frings-Dresen MHW. Neck strength, position sense, and motion in military helicopter crew with and without neck pain. Aviat Space Environ Med. 2010;81:46–51. [DOI] [PubMed] [Google Scholar]
- 26. Wibault J, Vaillant J, Vuillerme N, et al. Using the cervical range of motion (CROM) device to assess head repositioning accuracy in individuals with cervical radiculopathy in comparison to neck-healthy individuals. Man Ther. 2013;18:403–409. [DOI] [PubMed] [Google Scholar]
- 27. Cheng CH, Wang JL, Lin JJ, et al. Position accuracy and electromyographic responses during head reposition in young adults with chronic neck pain. J Electromyogr Kinesiol. 2010;20:1014–1020. [DOI] [PubMed] [Google Scholar]
- 28. Edmondston S, Chan H, Wing NG, et al. Postural neck pain: an investigation of habitual sitting posture, perception of “good” posture and cervicothoracic kinaesthesia. Man Ther. 2007;12:363–371. [DOI] [PubMed] [Google Scholar]
- 29. Elsig S, Luomajoki H, Sattelmayer M, et al. Sensorimotor tests, such as movement control and laterality judgment accuracy, in persons with recurrent neck pain and controls: a case-control study. Man Ther. 2014;19:555–561. [DOI] [PubMed] [Google Scholar]
- 30. Grip H, Sundelin G, Gerdle B, Karlsson JS. Variations in the axis of motion during head repositioning: a comparison of subjects with whiplash-associated disorders or non-specific neck pain and healthy controls. Clin Biomech (Bristol, Avon). 2007;22:865–873. [DOI] [PubMed] [Google Scholar]
- 31. Kristjansson E, Dall'Alba P, Jull G. A study of five cervicocephalic relocation tests in three different subject groups. Clin Rehabil. 2003;17:768–774. [DOI] [PubMed] [Google Scholar]
- 32. Kristjansson E, Oddsdottir GL. “The Fly”—a new clinical assessment and treatment method for deficits of movement control in the cervical spine: reliability and validity. Spine. 2010;35:E1298–E1305. [DOI] [PubMed] [Google Scholar]
- 33. Palmgren PJ, Andreasson D, Eriksson M, Hagglund A. Cervicocephalic kinesthetic sensibility and postural balance in patients with nontraumatic chronic neck pain: a pilot study. Chiropr Osteopat. 2009;17:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pinsault N, Vuillerme N, Pavan P. Cervicocephalic relocation test to the neutral head position: assessment in bilateral labyrinthine-defective and chronic, nontraumatic neck pain patients. Arch Phys Med Rehabil. 2008;89:2375–2378. [DOI] [PubMed] [Google Scholar]
- 35. Rix GD, Bagust J. Cervicocephalic kinesthetic sensibility in patients with chronic, nontraumatic, cervical spine pain. Arch Phys Med Rehabil. 2001;82:911–919. [DOI] [PubMed] [Google Scholar]
- 36. Sjolander P, Michaelson P, Jaric S, Djupsjobacka M. Sensorimotor disturbances in chronic neck pain: range of motion, peak velocity, smoothness of movement, repositioning acuity. Man Ther. 2008;13:122–131. [DOI] [PubMed] [Google Scholar]
- 37. Uthaikhup S, Jull G, Sungkarat S, Treleaven J. The influence of neck pain on sensorimotor function in the elderly. Arch Gerontol Geriatr. 2012;55:667–672. [DOI] [PubMed] [Google Scholar]
- 38. Woodhouse A, Vasseljen O. Altered motor control patterns in whiplash and chronic neck pain. BMC Musculoskelet Disord. 2008;9:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Open Med. 2009;3:e123–e130. [PMC free article] [PubMed] [Google Scholar]
- 40. Vuillerme N, Pinsault N, Bouvier B. Cervical joint position sense is impaired in older adults. Aging Clin Exp Res. 2008;20:355–358. [DOI] [PubMed] [Google Scholar]
- 41. Ahmed MS, Matsumura B, Cristian A. Age-related changes in muscles and joints. Phys Med Rehabil Clin N Am. 2005;16:19–39. [DOI] [PubMed] [Google Scholar]
- 42. Demaille-Wlodyka S, Chiquet CH, Lavaste JF, et al. Cervical range of motion and cephalic kinesthesis: ultrasonographic analysis by age and sex. Spine. 2007;32:254–261. [DOI] [PubMed] [Google Scholar]
- 43. Jordan K, Dziedzic K, Jones PW, et al. The reliability of the three-dimensional FASTRAK measurement system in measuring cervical spine and shoulder range of motion in healthy subjects. Rheumatology. 2000;39:382. [DOI] [PubMed] [Google Scholar]
- 44. de Koning CHP, van den Heuvel SP, Staal JB, et al. Clinimetric evaluation of active range of motion measures in patients with non-specific neck pain: a systematic review. Eur Spine J. 2008;17:905–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Karnath HO, Sievering D, Fetter M. The interactive contribution of neck muscle proprioception and vestibular stimulation to subjective “straight ahead” orientation in main. Exp Brain Res. 1994;101:140–146. [DOI] [PubMed] [Google Scholar]
- 46. Taylor JL, McCloskey DI. Proprioception in the neck. Exp Brain Res. 1988;70:351–360. [DOI] [PubMed] [Google Scholar]
- 47. Rothwell JC, Traub MM, Day BL, et al. Manual motor performance in a deafferented man. Brain. 1982;105:515–542. [DOI] [PubMed] [Google Scholar]
- 48. Nougier V, Bard C, Fleury M, et al. Control of single-joint movements in deafferented patients: evidence for amplitdue coding rather than position control. Exp Brain Res. 1996;109:473–482. [DOI] [PubMed] [Google Scholar]
- 49. McCaskey MA, Schuster-Amft C, Wirth B, et al. Effects of proprioceptive exercises on pain and function in chronic neck- and low back pain rehabilitation: a systematic literature review. BMC Musculoskelet Disord. 2014;15:382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Malmstrom EM, Westergen H, Fransson PA, et al. Experimentally induced deep cervical muscle pain distorts head on trunk orientation. Eur J Appl Physiol. 2013;113:2487–2499. [DOI] [PubMed] [Google Scholar]
- 51. Beinert K, Keller M, Taube W. Neck muscle vibration can improve sensorimotor function in patients with neck pain. Spine J. 2015;13:514–521. [DOI] [PubMed] [Google Scholar]
- 52. Brumagne S, Cordo P, Lysens R, et al. The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine (Phila Pa 1976). 2000;25:989–994. [DOI] [PubMed] [Google Scholar]
- 53. Parsons LM. Integrating cognitive psychology, neurology, and neuroimaging. Acta Psychol. 2001;107:155–181. [DOI] [PubMed] [Google Scholar]
- 54. Parsons LM, Fox PT. The neural basis of implicit movements used in recognising hand shape. Cogn Neuropsychil. 1998;15:583–615. [Google Scholar]
- 55. Beinert K, Preiss S, Huber M, Taube W. Cervical joint position sense in neck pain: immediate effects of muscle vibration versus mental training interventions. Eur J Phys Rehabil Med. 2015;51:825–832. [PubMed] [Google Scholar]