Abstract
Paroxysmal nocturnal haemoglobinuria (PNH) also known as 'Marchiafava Micheli syndrome' is a rare condition which can lead to both acute and chronic forms of renal failure through renal tubular haemosiderin deposition. A 45-year-old lady with underlying PNH, presented with complaints of fever, productive cough followed by dark coloured urine. Investigations revealed pancytopenia with a markedly raised creatinine from her baseline (from 65 mmol/L to 385 mmol/L) consistent with acute kidney injury (AKI). Renal biopsy confirmed the diagnosis of haeme nephropathy. The renal impairment improved rapidly and normalised over a period of 5 days with alkaline diuresis (AD). The patient did not require haemodialysis unlike most other reported cases of AKI secondary to haeme nephropathy in PNH. This is the second reported case of AKI in PNH which was successfully treated with AD alone emphasizing the role of AD as a promising therapeutic strategy in this condition.
Keywords: paroxysmal nocturnal haemoglobinuria, alkaline diuresis
Introduction
Paroxysmal nocturnal haemoglobinuria (PNH) is an extremely rare acquired clonal disorder of hematopoiesis also termed as Marchiafava syndrome. PNH is a misnomer as the haemoglobinuria happens throughout the day. Haemolysis, thrombosis and bone marrow suppression are cardinal features of this condition (Enneking, 1928[6]). Although infrequent, acute kidney injury is a serious and recognised complication. Patients usually present with renal impairment following a bout of haemolysis. Acute renal failure is usually fully reversible with haemodialysis but can occasionally be fatal (Nishimura et al., 2004[11]). We hereby present a case report of acute kidney injury in PNH which was successfully treated with alkaline diuresis (AD) alone.
Case Report
A 45-year-old lady was diagnosed to have PNH in October 2007 based on history, positive Ham's test and immunophenotyping showing reduced CD 59 and CD 55 expression. Since diagnosis, she had recurrent admissions due to pancytopenia. In the most recent admission, she presented with complaints of fever and productive cough preceding passing out dark-red coloured urine. The urine output was good with no other urinary symptoms.
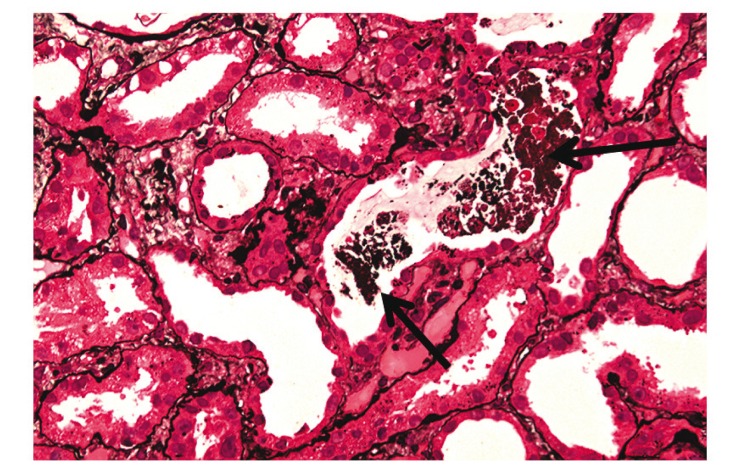
Laboratory investigations showed pancytopenia; haemoglobin of 5.9 g/dL, white cell count of 3.5 X 109/dL and platelet of 104 X 10 9 dL. Her renal profile had always been normal. However, during this admission her creatinine was 385 mmol/L ( normal range 45-95 mmol/L) and the urea was 23 mg/dL. The electrolytes and blood pH were normal. Urine FEME was positive for haemoglobin and negative for protein, nitrite and leucocytes. Ultrasound of the kidneys was normal with no evidence of renal vein thrombosis. Renal biopsy showed haeme pigment deposition in the distal convoluted tubules (Figure 1(Fig. 1)). Based on the above findings, the diagnosis of haeme nephropathy in paroxysmal nocturnal haemoglobinuria was made. The patient was treated with antibiotics for chest infection, transfused with packed cells and was given Danazol 200 mg bd. She was given intravenous fluids 5 litres over 24 hours with intravenous furosemide 40 mg bd. Her urine was alkalinised with intravenous 1.4 % sodium bicarbonate at 50 mls per hour. The target level for her urine pH was more than 7.
Figure 1. Renal biopsy specimen with H & E stain showing distal convoluted tubules with haemosiderin deposition (arrows) under 40x magnification.
There was no indication for an urgent dialysis such as hyperkalemia, fluid overload or metabolic acidosis. We kept in mind haemodialysis as the definite next option should she not respond to the regimen described above. Fortunately, after the initial 48 hours of alkaline diuresis, her creatinine improved to 162 mmol/L. With such promising early results, we continued with the same treatment. Over the following 3 days, her creatinine rapidly normalised. She was discharged well with a normal kidney function after 7 days of hospital stay.
Discussion
The earliest description of PNH was by Paul Strübing (1882[14]) who described the case in a 29-year-old cartwright who presented with fatigue, abdominal pain, and severe nocturnal paroxysms of hemoglobinuria. Later, Marchiafava and Micheli threw much light on the disorder and it was Enneking in 1925 who coined the term ‘paroxysmal nocturnal haemoglobinuria’ (Enneking, 1928[6]).
Renal failure in PNH was first described in 1953. Over the years, renal involvement in PNH has become a well recognised potentially serious complication. In PNH, the spectrum of kidney involvement ranges from the acute reversible kidney injury to chronic irreversible kidney disease. Renal failure is the cause of death in up to 18 % of patients. More than half of the patients tend to develop chronic kidney disease secondary to tubular haemosiderin deposition and microvascular thrombosis (Nishimura et al., 2004[11]).
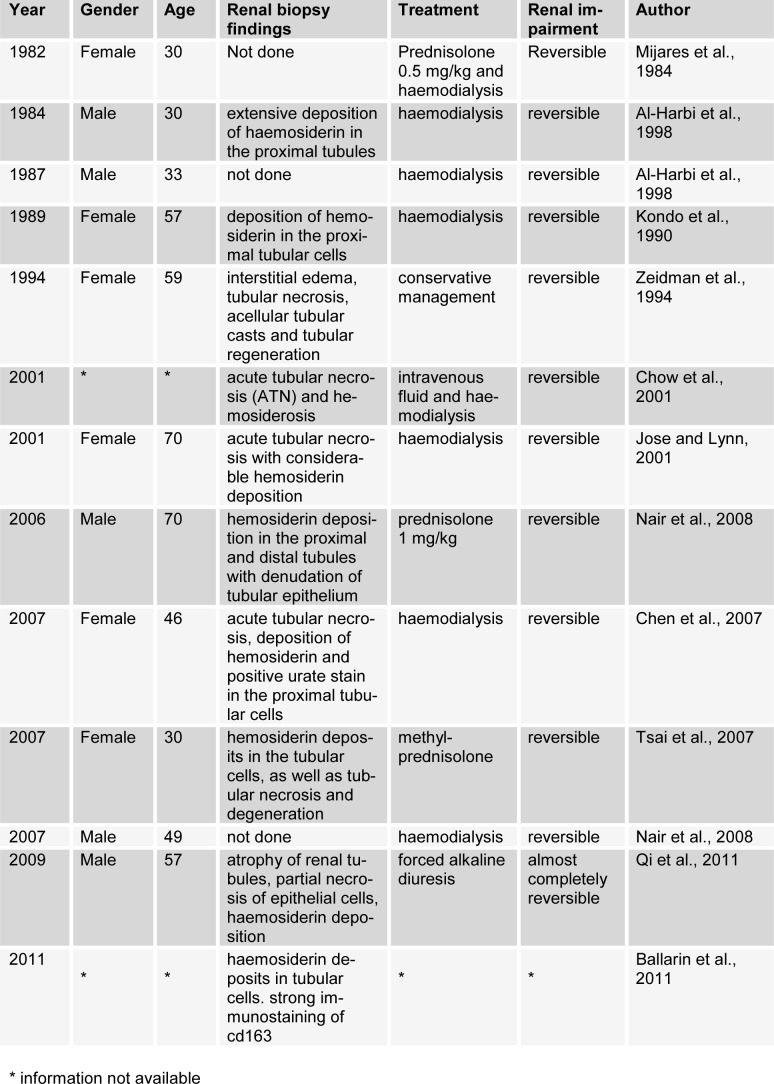
There are several mechanisms that may contribute to acute renal failure in PNH. The commonest mechanism proven by renal biopsy findings of affected patients in the previous case reports was haeme nephropathy with acute tubular necrosis secondary to haemosiderin deposition from intravascular haemolysis (Table 1(Tab. 1); References in Table 1: Mijares et al., 1984[9]; Al-Harbi et al., 1998[1]; Kondo et al., 1990[8]; Zeidman et al., 1994[16]; Chow et al., 2001[5]; Jose and Lynn, 2001[7]; Nair et al., 2008[10]; Chen et al., 2007[4]; Tsai et al., 2007[15]; Qi et al., 2011[12]; Ballarin et al., 2011[2]). Urinary tract infections, renal vein thrombosis and microvascular thrombosis have also been implicated. Renal failure is associated with poorer prognosis in PNH (Nishimura et al., 2004[11]).
Table 1. Summary of reported cases of acute kidney injury in paroxysmal nocturnal haemoglobinuria.
We believe that a good understanding of the involved pathogenesis is essential to plan the appropriate treatment strategies. In haeme nephropathy, when plasma haptoglobin becomes saturated with haemoglobin, free haemoglobin is filtered by the glomeruli followed by reabsorption in the proximal tubules (Nair et al., 2008[10]). In the most recent case report, CD163 (a haemoglobin scavenger receptor expressed in macrophages) and oxidative stress markers (NADPH-p22 phox and haeme oxygenase-1) were thought to be involved (Ballarín et al., 2011[2]).
A thorough literature search with regard to past reported cases was done and the findings were tabulated (Table 1(Tab. 1)). In the past few decades, there were 13 of such reported cases. It may be mentioned that the vast majority i.e up to 66.7 % of past researchers and clinicians treated AKI in PNH with haemodialysis (Table 1(Tab. 1)). However, in the present case, we attempted AD. This case highlights the role of AD as a simple, non invasive yet effective and promising therapeutic approach to the treatment of AKI in PNH. This is the second reported case of AKI in PNH which was treated with the above method which is otherwise used for treating pigment nephropathy due to rhabdomyolysis and in certain types of drug poisoning such as salicylate and phenobarbitone (Savege et al., 1969[13]; Tsai et al., 2007[15]).
Our rationale for choosing AD was based on the knowledge that AKI in both PNH and rhabdomyolysis share similar if not the same pathogenesis. It was therefore speculated that AD in PNH would yield comparable results with rhabdomyolysis. The renal outcome of this patient supported our hypothesis.
AD involves intravenous administration of sodium bicarbonate (NaHCO3) with either mannitol or loop diuretics. The alkaline pH of urine promotes the solubility of pigments and limits the formation of casts and crystals, while impairing the degradation of haemoglobin into heme and free iron and the associated nephrotoxic effect. The aim of this mode of treatment is to reach a urine pH above 6.5 (Tsai et al., 2007[15]).
Diuresis increases the rate of flow within the nephron which in turn reduces pigment deposition in the tubules. But it is of crucial importance to ensure that intravascular volume is adequate prior to administration of diuretics. The two frequently used diuretics in this setting are mannitol and furosemide. Mannitol is an osmolar diuretic agent that acts by improving renal perfusion, promoting the excretion of myoglobin, heme, and iron and decreasing the oxidative stress in the tubular cells. As opposed to mannitol which acts on the proximal convoluted tubules, furosemide prevents the accumulation of pigments in distal convoluted tubules. Compared to mannitol, furosemide causes more intense diuresis and has the disadvantage of lowering the urine pH (Tsai et al., 2007[15]).
Since 1969, the merits of AD has been studied and experimented especially in intoxications (Savege et al., 1969[13]). Many clinicians in the past did not explore this method in PNH as there is still strong skepticism with regard to its effectiveness in restoring normal kidney function. Whilst the use of AD is actually debatable, early renal recovery had been noted in some patients with rhabdomyolysis. Early initiation of this form of therapy predicted a more favourable outcome (Brown et al., 2004[3]; Tsai et al., 2007[15]).
In conclusion, the authors believe that AD may be an effective stand-alone therapeutic option to consider in AKI secondary to haeme nephropathy in PNH,especially among stable patients. This recommendation, however, is still premature and requires further supporting evidence. The rarity of this condition makes it difficult for more research to be conducted in this area.
References
- 1.Al-Harbi A, Alfurayh O, Sobh M, Akhtar M, Tashkandy MA, Shaaban A. Paroxysmal nocturnal hemoglobinuria and renal failure. Saudi J Kidney Dis Transp. 1998;9:147–151. [PubMed] [Google Scholar]
- 2.Ballarín J, Arce Y, Torra BR, Diaz EM, Manzarbeitia F, Ortiz A. Acute renal failure associated to paroxysmal nocturnal haemoglobinuria leads to intratubular haemosiderin accumulation and CD163 expression. Nephrol Dial Transplant. 2011;26:3408–3411. doi: 10.1093/ndt/gfr391. [DOI] [PubMed] [Google Scholar]
- 3.Brown CV, Rhee P, Chan L, Evans K, Demetriades D, Velmahos GC. Preventing renal failure in patients with rhabdomyolysis: do bicarbonate and mannitol make a difference? J Trauma. 2004;56:1191–1196. doi: 10.1097/01.ta.0000130761.78627.10. [DOI] [PubMed] [Google Scholar]
- 4.Chen SC, Hung CC, Hsu CP, Chiu YW, Liu YC, Tsai JC, et al. Recurrent acute renal failure in a patient with aplastic anemia-paroxysmal nocturnal hemoglobinuria syndrome: a case report. Kaohsiung J Med Sci. 2007;23:579–583. [PubMed] [Google Scholar]
- 5.Chow KM, Lai FM, Wang AY, Chan YL, Tang NL, Li PK. Reversible renal failure in paroxysmal nocturnal hemoglobinuria. Am J Kidney Dis. 2001;37(2):E17. doi: 10.1053/ajkd.2001.21361. [DOI] [PubMed] [Google Scholar]
- 6.Enneking J. Eine neue Form intermittierender Haemoglobinurie (Haemoglobinuria paroxysmalis nocturia) Klin Wochenschr. 1928;7:2045. [Google Scholar]
- 7.Jose MD, Lynn KL. Acute renal failure in a patient with paroxysmal nocturnal hemoglobinuria. Clin Nephrol. 2001;56:172–174. [PubMed] [Google Scholar]
- 8.Kondo H, Uga S, Kaihara A, Kawada M, Yamano T. [Acute renal failure in a case of paroxysmal nocturnal hemoglobinuria - a review of literature in Japan]. Nihon Jinzo Gakkai shi. 1990;32:835–840. (Ger). [PubMed] [Google Scholar]
- 9.Mijares RP, Praga M, Izaguirre A, Angulo P, Urquizu C, Lopez de Novales E. Paroxysmal nocturnal hemoglobinuria presenting as acute renal failure. Nephron. 1984;38:69–70. doi: 10.1159/000183283. [DOI] [PubMed] [Google Scholar]
- 10.Nair RK, Khaira A, Sharma A, Mahajan S, Dinda AK. Spectrum of renal involvement in paroxysmal nocturnal hemoglobinuria: report of three cases and a brief review of the literature. Int Urol Nephrol. 2008;40:471–5. doi: 10.1007/s11255-008-9356-5. [DOI] [PubMed] [Google Scholar]
- 11.Nishimura J, Kanakura Y, Ware RE, Shichishima T, Nakakuma H, Ninomiya H, et al. Clinical course and flow cytometric analysis of paroxysmal nocturnal hemoglobinuria in the United States and Japan. Medicine (Baltimore) 2004;83:193–207. doi: 10.1097/01.md.0000126763.68170.46. [DOI] [PubMed] [Google Scholar]
- 12.Qi K, Zhang XG, Liu SW, Yin Z, Chen XM, Wu D. Reversible acute kidney injury caused by paroxysmal nocturnal hemoglobinuria. Am J Med Sci. 2011;341:68–70. doi: 10.1097/MAJ.0b013e3181f515b9. [DOI] [PubMed] [Google Scholar]
- 13.Savege TM, Ward JD, Simpson BR, Cohen RD. Treatment of severe salicylate poisoning by forced alkaline diuresis. Br Med J. 1969;1(5635):35–6. doi: 10.1136/bmj.1.5635.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strübing P. Paroxysmale Haemoglobinurie. Deutsche Med Wochenschr. 1882;8:1–17. [Google Scholar]
- 15.Tsai C-W, Wu V-C, Lin W-C, Huang J-W, Wu M-S. Acute renal failure in a patient with paroxysmal nocturnal hemoglobinuria. Kidney Int. 2007;71:1187. doi: 10.1038/sj.ki.5002179. [DOI] [PubMed] [Google Scholar]
- 16.Zeidman A, Chagnac A, Wisnovitz M, Mittelman M. Haemolysis-induced acute renal failure in paroxysmal nocturnal haemoglobinuria. Nephron. 1994;66:112. doi: 10.1159/000187779. [DOI] [PubMed] [Google Scholar]