Abstract
Although severe gynaecological pathology during delivery and negative outcome have been shown to be related with posttraumatic stress disorder (PTSD) little is known about traumatic experiences following regular delivery, at the expected time and with a healthy child. The objective of our study was to determine the prevalence of PTSD during postpartum period after vaginal delivery and its risk factors. The sample included 126 primiparous women. Monthly, for the next three months, the women were assessed for PTSD using the gold standard interview for PTSD, Clinician-Administered PTSD Scale (CAPS). Risk factors were assessed including sociodemographic variables, personal medical history and clinical variables. After the first month, 2.4% women had acute full PTSD and another 9.5% had clinically significant level of PTSD symptoms. Following the second and the third month, partial PTSD was found in 5.9% and 1.3% of the women, respectively, and none of participants had full PTSD. Obstetrical interventions were the only significant risk factor for the development of PTSD. Symptoms of postpartum PTSD are not rare after a traumatic delivery, and associated with specific obstetrical risk factors. Awareness of these risk factors may stimulate interventions to prevent this important and neglected postpartum disorder.
Posttraumatic stress disorder (PTSD) is characterized by symptoms of re-experiencing, avoidance and hyperarousal, as well as social and professional dysfunction at least a month after exposure to a traumatic event1. PTSD after delivery was described in literature since the 1970s2,3,4,5,6,7,8. Studies suggest that not only severe gynaecological pathology during delivery and a negative outcome can be a traumatic experience for the mother, but that normal delivery (at the expected time with a healthy child) can also cause PTSD3,4,5.
Prevalence of postpartum diagnosis of PTSD varies in the range of 0–6.9% (2% on average), but significant levels of symptoms of the subthreshold PTSD could be present in 1.5–33.1% of all parturients3,9,10,11,12,13.
Postpartum PTSD has a significant influence on mother and baby’s daily and long-term functioning, a high comorbidity rate with other mental disorders, but remains rarely recognised and treated in routine clinical practice. Consequences of postpartum PTSD include: refusal to breastfeed the new-born, attachment problems, partner and intimacy avoidance, low self-esteem and low self-adequacy. These women associate their delivery to pain, fear or sorrow, or have traumatic amnesia5. It is unclear which biological and psychological risk factors are crucial for the development of postpartum PTSD. This indicates the urge for research in this field.
Risk factors for PTSD after delivery are mostly the same as for PTSD after any other trauma, with some specificity related to the event14, but not much is known about specific risk factors for PTSD after regular vaginal delivery. These risk factors might be pre-traumatic, peritraumatic and posttraumatic.
Possible pre-traumatic factors include sociodemographic factors5,6,15, personality traits5,7, tocophobia13, history of previous psychological problems4,10,13,14,15,16 or the number of previous deliveries9,15,16. Risk factors related to delivery include: mode and duration of delivery6,9,12,17, obstetric factors and complicated deliveries6,14,16, pain5,9 and epidural analgesia9,18, intensive fear for own or baby’s life4,5,15, sleep disturbances19 or peripartal dissociation13. Certain factors can be related to pre-, peri- and postpartum period (e.g. lack of social and medical support or traumatic experiences)3,4,5,13,14,15. Physiological measures as heart rate and blood pressure levels or low cortisol levels as parameters of sympathetic activation have been also suggested as potential risk factors for consecutive PTSD20,21,22.
Many of the listed risk factors are not studied together in the population of primiparous women with vaginal delivery. The study of postpartum PTSD requires a multidimensional approach since this disorder is a result of synergy of multiple risk factors, including biological vulnerability, psychological experiences and social influences.
The objectives of our study were to determine the prevalence of postpartum PTSD and to evaluate possible risk factors. The present study explored different risk factors: sociodemographic, obstetrical procedures, applied medications, epidural analgesia, biological (heart rate and blood pressure), and social support (partner’s presence) for postpartum PTSD in a unique population of primiparous women with vaginal delivery. This is the first study, as far as we are aware, on postpartum PTSD in Southeast Europe.
Methods
Participants
The study included 150 women who were recruited consecutively according to eligibility (inclusion and exclusion criteria) and was carried out at the Institute of Mental Health in Belgrade and the University Clinic of Obstetrics and Gynaecology “Narodni Front” from 2011–2012. The study received approval of the Ethical Committees of both institutions. Methods were carried out in accordance with the approved guidelines. All the participants signed the informed consent and were eligible if they were primiparous aged 18 or over, with or without any specific traumatic event until the delivery term (37–40 weeks of gestation). All of them were citizens of Belgrade. The exclusion criteria were the following: in vitro fertilisation pregnancy; weight below 45 or above 100 kg; psychoactive substance abuse; a prior history of PTSD and treatment for it; history of psychiatric disorders; history of head injury (involving confusion, loss of consciousness or amnesia); medical history of Cushing’s syndrome, current infectious disease or diabetes; taking medications that can interfere with the HPA axis during pregnancy or delivery (steroids, beta blockers, indomethacin); exposure to trauma that reflects ongoing victimisation (domestic violence) to which the subject was likely to be re-exposed during the study period. Women who had caesarean section were not eligible for the study.
Eight women refused to participate in the study due to “blood sampling fear”. Of the 150 parturients, one was excluded because of damaged serum sample due to sample transportation problems. One hundred and twenty-six women completed the one month follow-up interview, and seventy seven (51.3%) parturients completed the whole study. This rate of participants’ drop out does not differ from previously published data in PTSD studies in which it was estimated to be 50%23. No difference was found between those who remained in the study and those who withdrew regarding age (t = −0.786; p = 0.433), length of marriage (Z = −0.052; p = 0.959), educational level (Х2 = 2.834, р = 0,105), or frequency of epidural analgesia (Х2 = 0.000, р = 1.000).
The data about drug treatment during labour and delivery were collected. In accordance with hospital protocol, oxytocin (Syntocinon) was given to women as continuous intravenous drip. Epidural analgesia was applied at the time of cervix dilatation of 3–5 cm or depending on intensity and frequency of contractions (contractions at 2–5 minutes and lasting 45–60 seconds). Evaluation of specific obstetrical traumatic experience was based on objective measurements and included forceps delivery, vacuum extraction and breech presentation of the foetus.
Procedures
The interviews were conducted during the home visits or at the Institute of Mental Health during three months after delivery.
Cardiovascular measures
Blood pressure was measured during the first two hours after delivery. After measuring women’s heart rate (beats per minute) by a trained nurse, blood pressure (mmHg) was measured while the parturient was still lying and had rested for at least five minutes.
Psychological measures
During the next three months, women were screened monthly for PTSD by Clinician-Administered PTSD Scale (CAPS)24. Traumatic experience of delivery was assessed by the A criteria of the DSM IV classification (APA, 1994), according to work of Alcorn et al.25. In CAPS, the symptoms of clusters B, C and D are rated for both frequency and intensity and these two scores are summed up to provide severity ratings. Additional questions are used to assess criteria A, E and F. A symptom was considered present if frequency was recorded as ≥1 and intensity as ≥2. PTSD diagnosis was made if a patient had at least 1 positive item from B cluster, 3 from C and 2 from D cluster and the total score above 45. Partial PTSD was diagnosed if the CAPS total score was ≥1925. In the reliability test, Cronbach alpha coefficient was 0.793 indicating that the CAPS has good internal consistency.
We estimated the following risk factors: sociodemographic, history of previous psychological problems, obstetrical factors and complicated deliveries, epidural analgesia, applied medications, cardiovascular measures (heart rate and blood pressure) and social support (partner’s presence). The data about the risk factors were collected by the clinical interview, from the medical records, by blood pressure measuring and with applied PTSD scale.
Statistical analysis
Data are presented as mean ± SD or N (%). The Chi-squared test was used to compare categorical variables, while the t-test and Mann-Whitney U-test were used for comparisons of continuous data. The linear mixed model was used for longitudinal data analysis. Data were analyzed using SPSS 20.0 (IBM, corp.) statistical package. All p-values less than 0.05 were considered significant.
Results
Sample characteristics
Sociodemographic and clinical characteristics of the sample are presented in Tables 1 and 2. One hundred and two (81.6%) women were married with the mean length of marriage of 20.1 months (SD = 32.3) and there were no divorced women or widows.
Table 1. Age and clinical characteristics of the sample.
| mean ± SD (Min-Max) | |
|---|---|
| Age | 29.7 ± 4.0 (20.0–42.0) |
| Weight (kg) | 75.2 ± 9.0 (53.0–99.0) |
| Heart rate (n/min) | 78.7 ± 10.9 (56.0–110.0) |
| Systolic blood pressure (mmHg) | 114.0 ± 10.8 (90.0–150.0) |
| Diastolic blood pressure (mmHg) | 71.5 ± 8.4 (60.0–100.0) |
Legend: kg- kilogram; n/min-number/minute; mmHg- millimeter of mercury.
Table 2. Sociodemographic characteristics of the sample and applied medications.
| Category | n | % | |
|---|---|---|---|
| Education | Elementary school | 1 | 0.8% |
| High school | 56 | 44.4% | |
| College | 14 | 11.1% | |
| University degree | 55 | 43.7% | |
| Marital status | Single | 6 | 4.8% |
| Married | 102 | 81.6% | |
| Common-law marriage | 17 | 13.6% | |
| Living with partners | No | 6 | 4.8% |
| Yes | 119 | 95.2% | |
| Employed | No | 29 | 23.0% |
| Yes | 97 | 77.0% | |
| Family history | No | 115 | 91.3% |
| Yes | 11 | 8.7% | |
| Applied pain killers | No | 117 | 92.9% |
| Yes | 9 | 7.1% | |
| Applied anxiolytics | No | 117 | 92.9% |
| Yes | 9 | 7.1% | |
| Epidural analgesia | No | 36 | 28.6% |
| Yes | 90 | 71.4% | |
| Partner was present during labour | No | 121 | 96.0% |
| Yes | 5 | 4.0% |
Comparing the data of all delivered women in Belgrade during 2012, obtained from the Institute of Public Health of Belgrade with our sample, there was no difference regarding age (p = 0.178) (27). The main difference was that obstetrical interventions were more frequent in our sample (p < 0.001).
Nine (7.1%) parturients received the pain killer Dolantin (meperidine hydrochloride), a synthetic opioid analgesic, in a dosage of 50 mg intramuscular (i.m.), once during the delivery. Also, nine (7.1%) women received 10 mg i.m. of diazepam once during labour. Epidural analgesia as a cocktail of fentanyl and bupivacaine hydrochloride was applied to 90 (71.4%). The obstetrical traumatic experience occurred in 12 (9.5%) women; forceps delivery was applied in 1 (0.8%), vacuum extraction in 10 (7.9%) women, and breech presentation of the foetus in 1 (0.8%) delivery.
Prevalence of PTSD
The full PTSD was diagnosed in 3 (2.4%) parturients after the first month of delivery, and after the next two months there were no parturients with this diagnose. The partial PTSD was found in 15 (11.9%) women one month after delivery, 5 (5.9%) after two months and one (1.3%) after three months. We analysed parturients with full and partial PTSD together as the “PTSD group”. After the first assessment there were no new cases of parturients with PTSD symptoms.
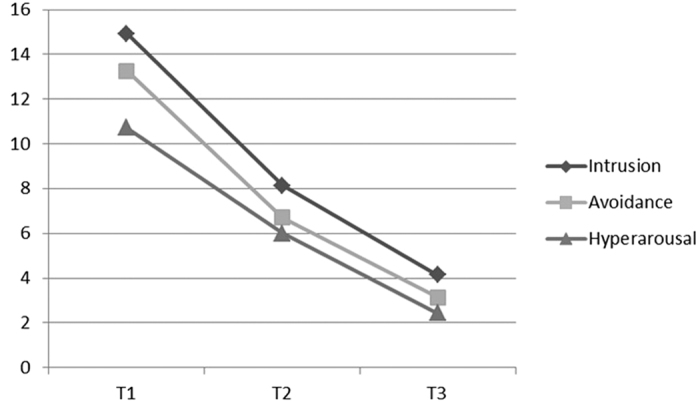
The severity of intrusive, avoidance and hyperarousal PTSD symptoms in the whole sample during the three months since delivery are presented in Table 3. After the first month, the majority of parturients (66.7%) had mild PTSD according to CAPS, and none of them had an extremely high score of PTSD symptoms. We have found that 64.3% of the parturients with PTSD symptoms after the first month did not have the symptoms after the second month, and 92.9% of them recovered after the third month.
Table 3. Descriptive statistics of the clusters of PTSD symptoms (CAPS score) after 1, 2 and 3 months of delivery.
| Symptoms | Month |
||
|---|---|---|---|
| 1st | 2nd | 3rd | |
| Intrusive | 14.9 ± 5.6 (8.0–26.0) | 8.1 ± 3.5 (4.0–17.0) | 4.1 ± 3.5 (0.0–12.0) |
| Avoidance | 13.3 ± 5.4 (4.0–22.0) | 6.7 ± 4.3 (0.0–15.0) | 3.1 ± 2.3(0.0–8.0) |
| Hyperarousal | 10.7 ± 3.1 (4.0–16.0) | 6.0 ± 2.6 (2.0–10.0) | 2.4 ± 1.9 (0.0–6.0) |
| Total | 38.9 ± 12.4 (20.0–60.0) | 20.9 ± 8.9 (10.0–39.0) | 9.9 ± 6.7 (3.0–26.0) |
Data are presented as mean ± SD (Min-Max).
An analysis by the linear mixed model of parturients with PTSD symptoms has shown that the total PTSD symptoms significantly decreased (F = 89.141, р < 0.001) during the three months of follow up, the same as the intrusive (F = 56.934, p < 0.001), avoidance (F = 64.795, p < 0.001) and hyperarousal (F = 138.845, p < 0.001) symptoms (Fig. 1).
Figure 1. Intensity of PTSD symptoms decreased during the three months of follow up after delivery.
Risk factors for PTSD
There were no significant differences for the sociodemographic data or clinical characteristics of the sample between the PTSD group and the parturients without PTSD symptoms. P varied from 0.152–1.000. Only the variable “being married” showed a trend to be significant (Z = −1.767, p = 0.077) (Tables 4 and 5).
Table 4. Sample details of the parturients with and without PTSD symptoms.
| PTSD symptoms | t/Z/X2 | p | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| Age | 28.93 ± 3.63 | 29.86 ± 4.10 | −0.827 | 0.410 | |
| Type of partnership | single | 2 (13.3%) | 4 (3.6%) | 3.194 | 0.183 |
| married | 12 (80.0%) | 90 (81.8%) | |||
| common-law marriage | 1 (6.7%) | 16 (14.5%) | |||
| Living with partner | Yes | 13 (86.7%) | 106 (96.4%) | 2.716 | 0.152 |
| No | 2 (13.3%) | 5 (3.6%) | |||
| Educational level | Primary school | 0 (0.0%) | 1 (0.9%) | 0.457 | 0.572 |
| High school | 5 (33.3%) | 51 (45.9%) | |||
| College | 3 (20.0%) | 11 (9.9%) | |||
| University degree | 46 (74.2%) | 52 (81.3%) | |||
| Employment | Yes | 12 (80.0%) | 85 (76.6%) | 0.087 | 1.000 |
| No | 3 (20.0%) | 26 (23.4%) | |||
| Family history | Yes | 1 (6.7%) | 10 (9.0%) | 0.091 | 1.000 |
| No | 14 (93.3%) | 101 (91.0%) | |||
| Applied pain killers | Yes | 1 (6.7%) | 8 (7.2%) | 0.006 | 1.000 |
| No | 14 (93.3%) | 103 (92.8%) | |||
| Applied anxiolytics | Yes | 1 (6.7%) | 8 (7.2%) | 0.006 | 1.000 |
| No | 14 (93.3%) | 103 (92.8%) | |||
| Epidural analgesia | Yes | 10 (66.7%) | 80 (72.1%) | 0.189 | 0.762 |
| No | 5 (28.6%) | 31 (27.9%) | |||
| Partner’s presence | Yes | – | 5 (4.5%) | 0.704 | 0.632 |
| No | 15 (100%) | 106 (95.5%) | |||
| Obstetrical interventions | Yes | 9 (75.0%) | 3 (25.0%) | 50.346 | <0.001 |
| No | 6 (5.3%) | 108 (94.7%) | |||
Legend: The data are presented as n (%) or mean ± SD; t-t-test; X2-Chi-squared test; Z- Mann-Whitney U-test.
Table 5. Clinical characteristics of the parturients with and without PTSD symptoms.
| PTSD symptoms |
t | p | ||
|---|---|---|---|---|
| Yes | No | |||
| Weight (kg) | 73.87 ± 10.90 | 75.41 ± 8.81 | −0.617 | 0.539 |
| Systolic blood pressure (mmHg) | 111.33 ± 7.18 | 114.37 ± 11.22 | −1.419 | 0.169 |
| Diastolic blood pressure (mmHg) | 70.67 ± 7.76 | 71.62 ± 8.56 | −0.410 | 0.683 |
| Heart rate (n/min) | 79.93 ± 8.55 | 78.56 ± 11.23 | 0.456 | 0.649 |
Legend: The data are presented as mean ± SD; t-t-test; p-sign; kg- kilogram; n/min-number/minute; mmHg- millimeter of mercury.
The most important finding is that the PTSD group of parturients had significantly more obstetrical interventions during delivery (Х2 = 50.346, р < 0.001). The univariate analysis has shown that the only statistically significant predictor of PTSD were obstetrical interventions (X2 = 50.436, p < 0.01). Multivariate binary logistic regression confirmed statistically significant relation of obstetrical interventions and PTSD, while no other predictors were significant (OR 53.5; Adj OR = 144.8).
Discussion
Women can experience delivery as traumatic and develop PTSD which is neglected both by gynaecologists and psychiatrists. The objective of our study was to evaluate the prevalence of postpartum PTSD and potential risk factors for the disorder in a unique sample of primiparous women with vaginal delivery. Our main findings show that 2.4% of parturients developed full PTSD after the first month since delivery and that specific obstetrical traumatic experiences during delivery are a risk factor for postpartum PTSD. No other sociodemographic variable, applied medication or epidural analgesia were significantly connected to development of PTSD symptoms.
The majority of delivered women in our study have not experienced their delivery as traumatic–only 15 of 126 (11.9%) did so after the first month and all of them had some symptoms of PTSD. Our findings of 2.4% parturients with full PTSD, after the first month of delivery, are in line with the previously published data on prevalence of postpartum PTSD3,9,10,11,12,13. Both full and partial PTSD in our sample had a decrease in intensity in the first three months which confirms the assumption that most people spontaneously recover after exposure to trauma27,28 although some authors suggest that symptom severity decreases in patients with partial PTSD while it persists in patients with full PTSD29. Cultural differences could influence the prevalence of PTSD, along with stigma of mental health issues. As an example of this we would like to stress out that in our sample only 4% of partners were present during delivery which significantly differs from the percent in, for instance, England30. It could be discussed if this finding suggests that women in our sample lack social (partner’s) support during labour and delivery (social support has been known to be an important protective factor for preventing PTSD)31.
The findings of obstetrical interventions as risk factors for PTSD symptoms are previously recognized in several studies6,8,14,29. Olde12 and Söderquist et al.9 found that emergency caesarean section (EmCS), forceps delivery, vacuum extraction, epidural analgesia and episiotomy are predisposing factors for PTSD symptoms.
Although the experience of intensive pain is correlated with negative assessment of delivery, up-to-date pain-relief techniques did not show expected results18. Studies suggest that women who request epidural analgesia are more anxious and have more probability to experience delivery as traumatic9. In a randomized controlled trial Howell et al. found no different effects of epidural analgesia on women’s birth experience18. In our sample, both groups of parturients (with and without PTSD symptoms) had epidural analgesia equally frequently and so it was not recognised as a risk factor for the development of the PTSD symptoms. Indirectly, we could assume that the PTSD group was not more anxious during labour or delivery (used neither anxiolytics nor epidural analgesia more often).
A limitation of our study is small sample size. In further research, a large sample drop out must be taken into consideration. As a result of small numbers, some differences between groups could not be analysed and possible correlations were not registered. It is possible that the discrepancy between the expected and perceived level of pain is an additional risk factor for traumatic experience5,7 and women’s pain should be measured in correlation with the length of delivery and potential blood loss6,17. During the postpartum period, some healthy women have numerous symptoms (fatigue, sleep disturbance, concentration problems etc.) which could easily be attributable to PTSD, so specific attention should be paid when evaluating these symptoms. However, our study has several strengths. We have used the CAPS scale which is the gold standard interview for PTSD diagnosis and thus avoided possible misdiagnose made by self-report scales14. Our study is a prospective and we included only primiparous women who were prepared for normal vaginal delivery (NVD), although some were delivered with instrumental vaginal delivery (IVD). Sociodemographic data, data on pre-traumatic experiences and personal medical history were collected at the moment of entering the delivery room, before knowing the final mode of delivery. Knowing that the most stressful mode of delivery for women is shown to be IVD, then EmCS, NVD and elective cesarean section9,13, we tried to refine our sample and show that NVD per se could be the source of PTSD. According to the fact that parturients with a prior history of PTSD and treatment for it were not eligible for the study, trauma in our study was specifically related to labour and delivery, which probably reduced the occurrence of postpartum PTSD.
Although not the first study to explore the relationship between delivery and PTSD, our study is the first in Southeast Europe to include only NVD primiparous women and our findings show that NVD is not a risk factor for PTSD. Our study is the first in Southeast Europe to include only NVD primiparous women and our findings show that NVD is not a risk factor for PTSD. The obstetrical complications as an unplanned change significantly increase the likelihood of PTSD. Personality traits, previous stressful experiences, and exposure to traumatic events may have an independent and direct influence on developing posttraumatic stress32, and according to this we suggest that recently delivered women who had obstetrical complications should be screened and treated for PTSD as soon as possible. It has been shown that when treatment is applied early (e.g. cognitive behavioral therapy), during the first month, it can reduce symptoms of PTSD quicker33, which is especially important due to the fact that mother-child bonding is very strong in that period. Implications of our findings could be in the revealing of possible risk factors and vulnerability of parturients with PTSD, which could help professionals to better tailor the prevention measures for PTSD. A close collaboration between gynecologists, psychiatrists and primary care physicians is needed.
Additional Information
How to cite this article: Milosavljevic, M. et al. Posttraumatic Stress Disorder after Vaginal Delivery at Primiparous Women. Sci. Rep. 6, 27554; doi: 10.1038/srep27554 (2016).
Acknowledgments
We would like to thank MDs Zeljka Kosutic, Jelica Vlahovic and Suzana Krsmanovic for helping in sample collection, Ivana Perunicic for assistance in preparation of the database, as well as Professors Dusan Stanojevic and Snezana Rakic for organizing research at the Gynecologic Clinic. We also acknowledge and extend our gratitude to the parturients and their families who participated in this study.
Footnotes
Author Contributions M.M. recruited and screened the subjects and wrote the manuscript. M.K. and O.V. helped to prepare the manuscript. I.S., O.V., C.M. and A.P. analysed the data and produced the figure. D.L.T. designed the study, supervised the research and participated in its coordination. D.L.T. and M.O. critically revised manuscript. All authors have read and approved the final manuscript.
References
- American Psychiatric Association (APA). DSM-IV Diagnostic and statistical manual of mental disorders. 4th ed . (American Psychiatric Association, Washington DC, 1994). [Google Scholar]
- Bydlowski M. & Raoul-Duaval A. Un avatar psychique meconnu de la puerperalite: la nervrose traumatique post-obsetricale. (A psychological manifestation unknown within pediatrics: the posttraumatic obstetric neurosis). Perspect Psychiatr . 4, 321–328 (1978). [Google Scholar]
- Creedy D. K., Shochet I. M. & Horsfall J. Childbirth and the development of acute trauma symptoms: incidence and contributing factors. Birth . 27, 104–111 (2000). [DOI] [PubMed] [Google Scholar]
- Czarnocka J. & Slade P. Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br J Clin Psychol. 39, 35–51 (2000). [DOI] [PubMed] [Google Scholar]
- Soet J. E., Brack G. A. & DiIorio C. Prevalence and predictors of women’s experience of psychological trauma during childbirth. Birth . 30, 36–46 (2003). [DOI] [PubMed] [Google Scholar]
- Modarres M., Afrasiabi S., Rahnama P. & Montazeri A. Prevalence and risk factors of childbirth-related post-traumatic stress symptoms. BMC Pregnancy Childbirth. 12, 88 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verreault N. et al. PTSD following childbirth: a prospective study of incidence and risk factors in Canadian women. J Psychosom Res. 73, 257–263 (2012). [DOI] [PubMed] [Google Scholar]
- Garthus-Niegel S., von Soest T., Vollrath M. E. & Eberhard-Gran M. The impact of subjective birth experiences on post-traumatic stress symptoms: a longitudinal study. Arch Women’s Ment Health . 16, 1–10 (2013). [DOI] [PubMed] [Google Scholar]
- Söderquist J., Wijma K. & Wijma B. Traumatic stress after childbirth: the role of obstetric variables. J Psychosom Obstet Gynaecol. 23, 31–39 (2002). [DOI] [PubMed] [Google Scholar]
- Ayers S. Delivery as a traumatic event: prevalence, risk factors, and treatment for postnatal posttraumatic stress disorder. Clin Obstet Gynecol. 47, 552–567 (2004). [DOI] [PubMed] [Google Scholar]
- Maggioni C., Margola D. & Filippi F. PTSD, risk factors, and expectations among women having a baby: a two-wave longitudinal study. J Psychosom Obstet Gynaecol. 27, 81–90 (2004). [DOI] [PubMed] [Google Scholar]
- Olde E., van der Hart O., Kleber R. & van Son M. Posttraumatic stress following childbirth: A review. Clin Psychol Rev. 26, 1–16 (2006). [DOI] [PubMed] [Google Scholar]
- Söderquist J., Wijma B., Thorbert G. & Wijma K. Risk factors in pregnancy for post-traumatic stress and depression after childbirth. BJOG. 116, 672–680 (2009). [DOI] [PubMed] [Google Scholar]
- Grekin R. & O’Hara M. W. Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin Psychol Rev. 34, 389–401 (2014). [DOI] [PubMed] [Google Scholar]
- Zaers S., Waschke M. & Ehlert U. Depressive symptoms and symptoms of post-traumatic stress disorder in women after childbirth. J Psychosom Obstet Gynaecol. 29, 61–71 (2008). [DOI] [PubMed] [Google Scholar]
- Andersen L. B., Melvaer L. B., Videbech P., Lamont R. F. & Joergensen J. S. Risk factors for developing post-traumatic stress disorder following childbirth: a systematic review. Acta Obstet Gynecol Scand. 91, 1261–1272 (2012). [DOI] [PubMed] [Google Scholar]
- Bell A. F., White-Traut R., Wang E. C. & Schwertz D. Maternal and umbilical artery cortisol at birth: relationships with epidural analgesia and newborn alertness. Biol Res Nurs. 14, 269–276 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell C. J. et al. A randomised controlled trial of epidural compared with non-epidural analgesia in labour. BJOG. 108, 27–33 (2001). [DOI] [PubMed] [Google Scholar]
- Benfield R. D., Newton E. R., Tanner C. J. & Heitkemper M. M. Cortisol as a biomarker of stress in term human labor: Physiological and methodological Issues. Biol Res Nur . 16, 64–71 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coronas R. et al. Heart rate measured in the acute aftermath of trauma can predict post-traumatic stress disorder: a prospective study in motor vehicle accident survivors. Eur Psychiatry. 26, 508–512 (2011). [DOI] [PubMed] [Google Scholar]
- Bryant R. A., Creamer M., O’Donnell M., Silove D. & McFarlane A. C. Heart rate after trauma and the specificity of fear circuitry disorders. Psychol Med. 41, 2573–2580 (2011). [DOI] [PubMed] [Google Scholar]
- Mouthaan J. et al. The role of acute cortisol and DHEAS in predicting acute and chronic PTSD symptoms. Psychoneuroendocrinology. 45, 179–186 (2014). [DOI] [PubMed] [Google Scholar]
- McFarlane A. C., Barton C. A., Yehuda R. & Wittert G. Cortisol response to acute trauma and risk of posttraumatic stress disorder. Psychoneuroendocrinology. 36, 720–727 (2011). [DOI] [PubMed] [Google Scholar]
- Blake D. D. et al. The development of a Clinician-Administered PTSD Scale. J Trauma Stress. 8, 75–90 (1995). [DOI] [PubMed] [Google Scholar]
- Alcorn K., O’Donovan A., Patrick J., Creedy D. & Devilly G. A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychological Medicine. 40, 1849–1859 (2010). [DOI] [PubMed] [Google Scholar]
- Blake D. et al. Instruction manual, Clinician-Administered PTSD Scale (CAPS). (National Center for Posttraumatic Stress Disorder Behavioral Science Division, Boston Neurosciences Division, West Haven, 2000).
- Zohar J. et al. New insights into secondary prevention in post-traumatic stress disorder. Dialogues Clin Neurosci. 13, 301–309 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meewisse M. L., Olff M., Kleber R., Kitchiner N. J. & Gersons B. P. The course of mental health disorders after a disaster: Predictors and comorbidity. J Trauma Stress. 24, 405–413 (2011). [DOI] [PubMed] [Google Scholar]
- Lapp L. K., Agbokou C., Peretti C. S. & Ferreri F. Management of post traumatic stress disorder after childbirth: a review. J Psychosom Obstet Gynaecol. 31, 113–122 (2010). [DOI] [PubMed] [Google Scholar]
- Redshaw M. & Henderson J. Fathers’ engagement in pregnancy and childbirth: evidence from a national survey. BMC Pregnancy Childbirth. 13, 70 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff M. Bonding after trauma: on the role of social support and the oxytocin system in traumatic stress. Eur J Psychotraumatol . 3, 10 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecic-Tosevski D., Gavrilovic J., Knezevic G. & Priebe S. Personality factors and posttraumatic stress: associations in civilians one year after air attacks. J Pers Disord. 17, 537–549 (2003). [DOI] [PubMed] [Google Scholar]
- Sijbrandij M. et al. Treatment of acute posttraumatic stress disorder with brief cognitive behavioral therapy: a randomized controlled trial. Am J Psychiatry. 164, 82–90 (2007). [DOI] [PubMed] [Google Scholar]


