Abstract
Purpose
Shoulder dislocation is a common joint dislocation managed by the emergency physicians in the emergency departments. Pre- and post-reduction radiographic examinations have long been the standard practice to confirm the presence of dislocation and the successful reduction. However, shoulder ultrasonography has recently been proposed as an alternative to the radiographic examination. This study aimed to assess the accuracy of ultrasonography in evaluating proper reduction of the dislocated joint.
Methods
This was a prospective observational study. All patients with confirmed anterior shoulder dislocation were examined by both ultrasonography and radiography after the attempt for reduction of the dislocated joint. The examiners were blinded to the result of the other imaging modality. Results of the two methods were then compared.
Results
Overall, 108 patients with confirmed anterior shoulder dislocation were enrolled in the study. Ninety-one (84.3%) of the patients were males. Mean age of the participants was (30.11 ± 11.41) years. The majority of the patients had a recurrent dislocation. Bedside ultrasonography showed a sensitivity of 53.8% (95% CI: 29.1%–76.8%) and a specificity of 100% (95% CI: 96.1%–100%) in detecting inadequate reductions. The results of ultrasonography had a statistically significant agreement with the results of radiography (Kappa = 0.672, p < 0.001).
Conclusion
The results suggest that the sensitivity of post-reduction ultrasound is not sufficient for it to serve as a substitute for radiography.
Keywords: Shoulder dislocation, Ultrasonography, Radiography
Introduction
Emergency physicians frequently encounter patients with a shoulder joint dislocation. The shoulder is the most frequently dislocated major joint.1 Anterior glenohumeral dislocations account for more than 50% of all joint dislocations.2 Reduction is attempted in the emergency department (ED), often under conscious sedation. As a common practice, pre- and post-reduction radiographic examinations are performed to ensure the presence of dislocation, to exclude fractures, and to confirm a successful reduction. However, the necessity of routinely obtaining these radiographs from all patients with dislocation has been challenged.2, 3, 4
Ultrasonography is being increasingly used in the EDs as a diagnostic tool. It has been proposed as an alternative to the radiography in evaluating shoulder joint dislocation1, 5, 6 considering its benefits in detecting shoulder pathologies.7, 8 In the evaluation of proper reduction of a dislocated shoulder joint after performing the reduction maneuvers, bedside ultrasonography has the advantages of timely usage and can preclude the need for re-sedation in cases of an inadequate reduction. This in turn can result in a decrease in the cost and the length of patient's stay in the ED. Therefore, bedside ultrasonography can be a good choice as long as it is accurate.
To our knowledge, very few papers that chiefly comprise case reports and small case series have addressed the use of bedside ultrasonography in evaluating the adequacy of the reduction.1, 5, 6, 9 There is an obvious gap in the literature for larger validation studies. We performed a prospective observational study to evaluate the accuracy of the bedside ultrasonography in detecting unsuccessful reductions and to examine whether this diagnostic modality can be safely recommended as a reliable indicator of the post-reduction persistent dislocation.
Materials and methods
This prospective observational study was performed between March 2012 and March 2014 at a university-affiliated trauma center ED where the two principal investigators were on duty as attending emergency physicians. We enrolled all patients with suspected shoulder dislocation presented to the ED in the two-year study interval.
Patients whose anterior shoulder dislocation was further confirmed by the standard radiologic examination were included in the study. A true anteroposterior (true AP) shoulder radiograph was taken as the standard criterion to confirm the anterior shoulder dislocation. In order to have a more homogenous sample, patients with a body mass index (BMI) of 35 or higher were excluded from our study. Other exclusion criteria were: time interval of more than 12 h since the occurrence of the dislocation, multiple trauma or concomitant fractures. Posterior glenohumeral dislocations were also excluded because standard radiography is not accurate enough to show this type of dislocation,10 and according to our hospital's protocol, the suspected posterior dislocations should be managed by an orthopedic surgeon and reduced in the operation room not the emergency department.
An experienced attending emergency physician interpreted the initial radiographs and confirmed the dislocations. Subsequently, either of the two principal investigators tried to reduce the joint by performing scapula manipulation or traction-counter-traction maneuvers while procedural sedation was applied and cardiovascular monitoring was being performed in all cases. Then, the two principal investigators who had several years of experience in bedside emergency sonography and had received training courses of shoulder ultrasonography in the radiology department performed the ultrasonography of the shoulder. Presence of humeral head in the glenoid fossa was examined to confirm the proper reduction. We used an ultrasound system (Honda Electronics Co., Ltd., Japan, 2100) with a 7-MHz linear probe. Both anterior and lateral approaches were used while the patient was laid in the supine position. A persistent dislocation was assigned as a positive finding.
After the result of the ultrasonography was documented, a post-reduction radiograph was obtained and interpreted by the independent attending physician who had confirmed the dislocations at the first stage. He was blinded to the results of the bedside ultrasonography performed by the principal investigator. Therefore, the interpretation of the radiographs and the sonographic examinations were performed independently and in a double-blind manner. At the end, the two sets of results were collected and then entered into a spreadsheet for later analysis. Fig. 1, Fig. 2 demonstrate the radiographic and ultrasonographic views of the shoulder joint before and after the reduction.
Fig. 1.
Radiographic evaluation of the dislocated shoulder joint, anteroposterior view (A). Post-reduction radiograph shows the head of humerus relocated into the glenoid fossa (B).
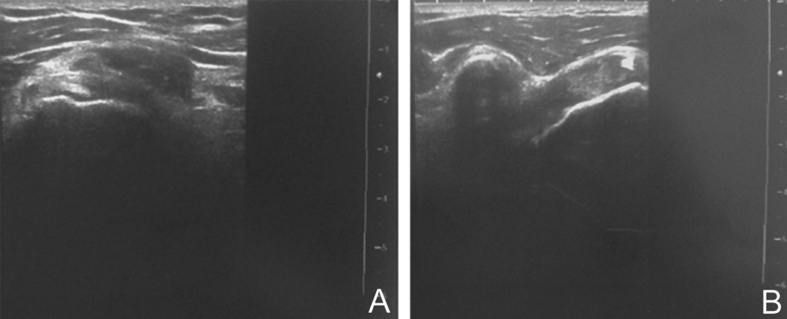
Fig. 2.
Ultrasonographic view of the shoulder joint (anterior approach). The head of humerus is visualized in its normal lateral position to the coracoid process (A: pre-reduction, B: post-reduction).
Statistical analysis was performed using SPSS for Windows (version 14.0, SPSS, Inc. Chicago, IL). Data was presented using descriptive statistics. Student's t and Chi-square tests were used to compare the results of ultrasonography and radiography, and sensitivity and specificity were calculated according to the standard formulas. Kappa agreement coefficient for the two diagnostic modalities was also calculated. Non-parametric tests were considered in case the variables did not obey the normal distribution. p values of 0.05 or less were regarded as statistically significant.
The study was approved by the ethics committee of the corresponding medical university. Written informed consent was obtained from all participants.
Results
Overall, 108 patients with confirmed anterior shoulder dislocation were enrolled in the study. Ninety-one (84.3%) of the patients were males. Mean age of the participants was (30.11 ± 11.41) years with a minimum age of 18 and a maximum of 75 years. The majority (80.6%) had a prior dislocation. Patients who were suffering the first episode of the shoulder dislocation were significantly younger. There was no significant difference between males and females in terms of dislocation recurrence (Table 1).
Table 1.
The association of age and sex with the dislocation recurrence.
| 1st Episode | Recurrence | Total | ||
|---|---|---|---|---|
| Sex | Male | 18 (19.8%)* | 73 (80.2%)* | 91 (100%) |
| Female | 3 (17.6%)* | 14 (82.4%)* | 17 (100%) | |
| Total | 21 | 87 | 108 | |
| Age | 24.0 ± 12.1 | 31.6 ± 10.8 | 30.1 ± 11.4 |
*Numbers in the parenthesis indicate the percentage of cases within the same sex group. Fischer's exact test = 0.041, p = 0.005.
Cross tabulation was used in order to compare the findings of ultrasonography with the results of radiography (Table 2). Ultrasonography had a sensitivity of 53.8% (95% CI: 29.1%–76.8%) in detecting persistent dislocations. All cases that were assigned by the ultrasonography as positive were further confirmed by the radiography to be an unsuccessful reduction. Thus, ultrasonography was 100% specific (95% CI: 96.1%–100%) in detecting persistent dislocations.
Table 2.
Performance of ultrasonography in detecting persistent dislocation.
| Ultrasonographya |
Radiographya |
||
|---|---|---|---|
| Positive | Negative | Total | |
| Positive | 7 | 0 | 7 |
| Negative | 6 | 95 | 101 |
| Total | 13 | 95 | 108 |
A positive test indicates a persistent dislocation.
Agreement between the findings of ultrasonography and the radiologic results was examined using Kappa coefficient as the measure of agreement. A Kappa value of 0.672 was obtained, which was statistically significant (p < 0.001).
Discussion
The notion of routinely obtaining pre- and post-reduction radiographs from all patients has been questioned.2, 3, 4 Earlier studies that challenged this notion suggested that in the majority of cases, physicians are able to accurately determine the joint position according to clinical clues.2, 3, 4, 11 Hendey4 proposed a clinical decision rule for selective radiography based on the mechanism of injury, history of previous dislocations, and the physician's clinical confidence of the dislocation or relocation. The proposed algorithm showed the potential of considerably reducing the utilization of radiography without missing any persistent dislocation. However, the physicians preferred to take a more conservative approach with regard to omitting the radiographs chiefly due to medicolegal concerns.12 Fear of litigation leads physicians to prefer a documented evidence for their decision, rather than merely a subjective clinical guess.
There are two main sources of worry that leads to obtaining a post-reduction radiograph. The first is iatrogenic fracture caused by the reduction maneuvers, which is hardly a concern since it very rarely occurs especially with modern less traumatic reduction techniques.4, 11 The second concern is persistence of the dislocation despite the reduction attempt. Rate of persistent dislocation after the first reduction attempt varies among different studies, and ranges from 0.6%3–3.1%.11 In cases of an unsuccessful reduction, because the medications used for procedural sedation are short-acting agents and their effects wane before the results of radiography are obtained, re-administration of the sedative medication is commonly required to perform a second attempt at reduction.
Based on the aforementioned rationale, the use of bedside ultrasonography has been proposed for confirming the adequate reduction when a procedural sedation is used. Halberg et al1 reported two cases of anterior and posterior shoulder dislocations in which relocation was successfully confirmed by bedside ultrasonography before the patients recovered from sedation. Meanwhile, Yuen et al6 also reported that their team had a two-year experience in utilizing bedside ultrasound for diagnosing anterior shoulder dislocation and confirming the complete reduction. In a series of 5 patients with anterior dislocation, bedside ultrasonography was found by Blakeley et al5 to be accurate in verifying the adequacy of reduction. In two separate case reports by Beck & Chilstrom13 and Mackenzie & Liebmann,10 point-of-care ultrasound was shown to be worthwhile in the rapid assessment and management of suspected posterior shoulder dislocation.
Abbasi et al9 reported a prospective observational study on a convenience sample of patients with suspected shoulder dislocation. The aim was to determine the accuracy of bedside ultrasonography in detecting the dislocation and confirming the relocation. According to this study, ultrasound was 100% sensitive and specific in the detection of shoulder dislocation, pre- and post-reduction.
Our study found a much lower sensitivity in the detection of persistent dislocation after a reduction attempt. In 6 out of 13 cases, ultrasonography suggested that a successful reduction was accomplished while radiography revealed persistence of the dislocation. In other words, persistent dislocation was missed by ultrasonography in nearly half of the cases (46.2%, 95% CI: 23.2%–70.9%). This is an unacceptably high rate, and suggests that we cannot safely rely on the results of bedside ultrasonography for detecting patients in whom the first attempt at reduction is not successful and a second attempt is required.
We found the specificity of ultrasonography to be perfect. So there may be some benefit in a positive test because it indicates that the reduction is not successful and another attempt should be made. However, a negative test cannot be used to confirm a successful reduction.
There is a discrepancy between our results and the results obtained by Abbasi et al,9 despite the fact that the sample size and characteristics, equipment, technique, and experience of the shoulder ultrasonographers are comparable in both studies. The only methodological difference lies in involving expert radiologists in verifying the interpretation of X-ray and sonographic imaging in Abbasi's study,9 which is not feasible in our study. On the other hand, assuming “unsuccessful reduction” as the positive result of the test, the lower limit of the 95% confidence interval for the calculated sensitivity in the Abbasi's study would be as low as 34.2%, which is aligned with the low sensitivity obtained in our study.
It is important to note that a persistent dislocation is relatively rare, and to reliably exclude a rare event we need larger sample sizes to let the rare event show itself. In validation studies, sample size requirements depend on several factors including the hypothesized values of sensitivity and specificity, the desired degree of precision at a specified confidence level, and the estimated prevalence of the studied condition in the target population.14 For instance, given the anticipated sensitivity of 90% and a precision of 10%, i.e. a sensitivity range of 80%–100%, for a 95% confidence level, a sample size of around 700 will be required.15 Neither our study nor Abbasi's study9 utilized sample sizes of this scale. Despite the low number of persistent dislocations in our study, only about half of them were detected by the ultrasonography. Thus, even in the absence of larger studies it can be concluded that this test is not good enough in fulfilling the proposed goal.
Our study has several limitations. First of all, the results of ultrasonography can vary extensively depending on the experience of the operator. As a result, the accuracy of findings cannot be extrapolated to other situations. Another limitation of our study is that due to some technical problems we used a single radiographic view, i.e. true AP instead of the three standard AP, lateral, and scapular Y views. In addition, the emergency physicians' interpretations of the imaging were not confirmed by an expert radiologist. Therefore, one can argue that the number of true inadequate reductions might have been under-calculated. In this case, the actual sensitivity would be even lower than what we have obtained. However, since we just included the anterior dislocation, the true AP could be sufficient for detecting inadequate reductions. Furthermore, the emergency physicians were proficient in the field of shoulder imaging as they had specific trainings and experiences under supervision of expert radiologists. Thus, this should not be a significant concern. Finally, the clinical clues to the complete or unsuccessful reduction were not addressed. We can look at this issue from another perspective. Physician's clinical certainty of the joint's position and clues such as surface anatomy and shoulder contour, neurovascular signs, and the feeling of a “clunk” during the reduction procedure has been proposed by the previous investigators as diagnostic factors that can reduce the need to obtain unnecessary radiographs. Some authors have even gone a step further by suggesting that imaging should be reserved for the cases that physical examination is inconclusive; otherwise, it would indicate a “hyposkillia” or “subluxation of clinical skills”.16
In our study, ultrasound had inadequate sensitivity for the detection of persistent dislocation. We suggest that the accuracy of a combination of ultrasonography and the physician's clinical suspicion should be compared with the clinical findings alone and/or selective radiographic examinations. This is a fruitful area for further investigations. It is recommended to explore utilization of the bedside ultrasonography as a supplement to the clinical clues in order to increase the sensitivity of the diagnostic approach. Considering the advantages of the bedside ultrasonography over radiography which includes a reduced stay, cost and radiation exposure, and bearing in mind the apprehension of litigation that leads the physicians to prefer the use of additional confirmatory tests, we believe that development of a valid clinical decision rule comprised by both the physical examination and the bedside ultrasonography would cover both ends of the spectrum of concerns.
In conclusion, post-reduction ultrasound is not sensitive enough to serve as a substitute for radiography in detecting persistent dislocations.
Acknowledgment
This study was the thesis of Dr. Kaveh Sineh-Sepehr to achieve a specialist degree in Emergency Medicine. It was supported in part by Mashhad University of Medical Sciences (Grant number: 93-04-38-27864).
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Halberg M.J., Sweeney T.W., Owens W.B. Bedside ultrasound for verification of shoulder reduction. Am J Emerg Med. 2009;27:e5–6. doi: 10.1016/j.ajem.2008.05.023. [DOI] [PubMed] [Google Scholar]
- 2.Harvey R.A., Trabulsy M.E., Roe L. Are postreduction anteroposterior and scapular Y views useful in anterior shoulder dislocations? Am J Emerg Med. 1992;10:149–151. doi: 10.1016/0735-6757(92)90049-4. [DOI] [PubMed] [Google Scholar]
- 3.Hendey G.W., Kinlaw K. Clinically significant abnormalities in postreduction radiographs after anterior shoulder dislocation. Ann Emerg Med. 1996;28:399–402. doi: 10.1016/s0196-0644(96)70004-5. [DOI] [PubMed] [Google Scholar]
- 4.Hendey G.W. Necessity of radiographs in the emergency department management of shoulder dislocations. Ann Emerg Med. 2000;36:108–113. doi: 10.1067/mem.2000.108314. [DOI] [PubMed] [Google Scholar]
- 5.Blakeley C.J., Spencer O., Newman-Saunders T. A novel use of portable ultrasound in the management of shoulder dislocation. Emerg Med J. 2009;26:662–663. doi: 10.1136/emj.2008.069666. [DOI] [PubMed] [Google Scholar]
- 6.Yuen C.K., Mok K.L., Kan P.G. Bedside ultrasound for verification of shoulder reduction with the lateral and anterior approaches. Am J Emerg Med. 2009;27:503–504. doi: 10.1016/j.ajem.2009.01.037. [DOI] [PubMed] [Google Scholar]
- 7.Helweg G., Moriggl B., Sperner G. Ultrasound diagnosis of the shoulder. Radiologe. 1996;36:971–980. doi: 10.1007/s001170050166. [DOI] [PubMed] [Google Scholar]
- 8.Tan S., Fairbairn K., Kirk J. Shoulder ultrasound. Biomed Imaging Interv. 2006;2:e58. doi: 10.2349/biij.2.4.e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abbasi S., Molaie H., Hafezimoghadam P. Diagnostic accuracy of ultrasonographic examination in the management of shoulder dislocation in the emergency department. Ann Emerg Med. 2013;62:170–175. doi: 10.1016/j.annemergmed.2013.01.022. [DOI] [PubMed] [Google Scholar]
- 10.Mackenzie D.C., Liebmann O. Point-of-care ultrasound facilitates diagnosing a posterior shoulder dislocation. J Emer Med. 2013;44:976–978. doi: 10.1016/j.jemermed.2012.11.080. [DOI] [PubMed] [Google Scholar]
- 11.Tannebaum R.D., Kondabala R.K., Stockmal P.J. Postreduction radiographs for anterior shoulder dislocation: a reappraisal. Ann Emerg Med. 2001;37:418–419. doi: 10.1067/mem.2001.113955. [DOI] [PubMed] [Google Scholar]
- 12.Hendey G.W., Chally M.K., Stewart V.B. Selective radiography in 100 patients with suspected shoulder dislocation. J Emerg Med. 2006;31:23–28. doi: 10.1016/j.jemermed.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Beck S., Chilstrom M. Point-of-care ultrasound diagnosis and treatment of posterior shoulder dislocation. Am J Emerg Med. 2013;31:e3–5. doi: 10.1016/j.ajem.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Buderer N.M. Statistical methodology: I. Incorporating the prevalence of disease into the sample size calculation for sensitivity and specificity. Acad Emerg Med. 1996;3:895–900. doi: 10.1111/j.1553-2712.1996.tb03538.x. [DOI] [PubMed] [Google Scholar]
- 15.Malhotra R.K., Indrayan A. A simple nomogram for sample size for estimating sensitivity and specificity of medical tests. Indian J Ophthalmol. 2010;58:519–522. doi: 10.4103/0301-4738.71699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lewin M.R. Subluxation of clinical skills. Ann Emerg Med. 2014;63:271. doi: 10.1016/j.annemergmed.2013.09.032. [DOI] [PubMed] [Google Scholar]