Abstract
Myositis ossificans circumscripta (MOC) is a kind of self-localized, benign and tumor-like lesions often seen in adults, with approximately 75% of cases caused by trauma. We reported a case of non-traumatic MOC occurred at the elbow joint in a 9-year old child and it has been excised by surgery. After 18 months follow-up, a favorable outcome has been achieved with the Broberg-Morrey score of 100. We suggest that surgical resection should be done as soon as the diagnosis is confirmed.
Keywords: Myositis ossificans circumscripta, Children, Elbow joint
Introduction
Myositis ossificans circumscripta (MOC) is a kind of self-localized, benign and tumor-like lesions, with approximately 75% of cases caused by trauma.1 MOC is usually seen in adults with the age ranging from 20 to 40 years, but rarely seen in children.2 MOC most frequently occurs in the region where there is high risk of injury, such as the flexor muscles of the upper arm, the quadriceps femoris, and the abductor muscles of the thigh,3 and rarely found in intra-articular area.4 We report a non-traumatic MOC at elbow joint in a child.
Case report
A 9-year old boy complained of right elbow pain, swelling, and aggravated restricted movement in past 4 months. The patient and his parents denied any injury history. At the local hospital, X-ray of the right elbow joint did not show any bone abnormalities. Blood test showed leukocyte 14.00 × 109/L, C-reactive protein (CRP) 13.66 mm/L, allergic C-reactive protein (CRP) >10 mm/L, and a normal alkaline phosphatase (ALP) level. He also got a lower-grade fever in 5 days besides disorder of the elbow joint. Then this boy was diagnosed with right upper limb cellulitis and treated by cefazolin and etimicin, but no obvious improvement was seen. Then a palpable mass was seen inside the right elbow, which was confirmed bone-like structure by computed tomography (CT) examination 3 months ago. The first pathological biopsy was made for tumor inside the right elbow, and the sample indicated osteoid osteoma change. After administration of non-steroidal anti-inflammatory drugs for 2 months, his symptoms were not remitted.
On admission to our hospital, a physical examination found a convex skin lesion at the right medial elbow joint presented sized 6 cm × 7 cm × 5 cm, local skin temperature was slightly high, the colour was red, local tenderness was not obvious, and the surrounding tissue boundaries was clear. The elbow joint movement was limited with the flexion and extension of about 120° (range from 20° to 140°). Forearm pronation and supination were nearly normal. Broberg-Morrey score was 87. The X-ray of the right elbow joint revealed distal ossification myositis of the right upper arm (Fig. 1).
Fig. 1.
The anterior-posterior and lateral radiographs of the right elbow joint showing distal ossification myositis of the right upper arm.
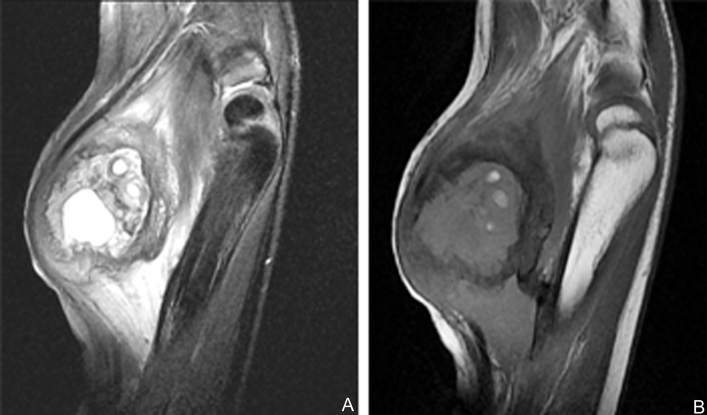
MRI found that the distal anteromedial right upper arm had soft tissue mass, and myositis ossificans and inflammatory edema were considered. Besides multiple cystic lesions, the distal humerus and ulna olecranon had mild bone marrow edema (Fig. 2). In order to differentiate characters of the tumor, a pathological biopsy was done inside the right elbow joint. The pathological results indicate mature trabecular bone and some fibrous tissue hyperplasia, but tumor cells were not seen.
Fig. 2.
A round mass sized about 5.53 cm × 4.10 cm × 5.87 cm was seen in front of the distal humerus. MRI scan showed multiple cystic lesions and mild bone marrow edema in the distal humerus and ulna olecranon.
We conducted surgical excision via the former biopsy approach under general anesthesia and a sized 6 cm × 7 cm × 5 cm mass was removed. We found the bottom of the neoplasm was in the medial condyle cortex of the humerus, with irregular bone structure and dark red liquid. Histopathologic result conformed the features of MOC (Fig. 3).
Fig. 3.
Histopathologic result showed that the mass center was filled with immature fibrous tissue and bone tissue and scattered by lots of chronic inflammatory cells, and the peripheral area was filled with differentiated mature trabecular bone tissue.
Pain was relieved and elbow joint movement was good 11 days later and then he was discharged. The flexion and extension was 110°, pronation and supination was normal. Broberg-Morrey score was 90. At 5 months and 18 months follow-up, elbow joint movement was normal. The patient did not feel any pain, and can deal with daily activities, even playing basketball. The Broberg-Morrey score achieved 100.
Discussion
Non-traumatic MOC is a rarely reported benign heterotopic ossification characterized by the aberrant formation of bone in extra-skeletal soft tissues. Myositis ossificans has different terms such as malignant fibrous histiocytoma, leiomyosarcoma, and synovial sarcoma, as well as malignant soft tissue tumor in its early term, soft tissue malignant tumor with calcification or ossification in medium term, parosteal osteosarcoma in late term. The typical image of myositis ossificans on CT scan can reveal a central radiolucency, surrounded by a dense periphery. MRI shows the performance of high signal on T2WI with low signal ring around it, and the low signal ring in the mature process of lesions will become more and more clear. Soft tissue swelling is the first sign to appear as the initial judgment method of myositis ossificans on plain films. Abnormal images may appear in 2–3 weeks after injury, but generally in 4–5 weeks.
The mechanism of non-traumatic MOC is unclear so far. Studies5 have shown that myositis ossificans has a huge connection with bone morphogenetic protein (BMP) expression which in serum in children may be higher than adults. This point may explain why using cefazolin, etimicin and non-steroidal anti-inflammatory drugs are ineffective.
MOC can be treated conservatively or surgically. Some clinicians favored surgical treatment, but what is the optimal time to do the surgery remains controversial. It is generally believed that surgery could be taken in 9–12 months after injury when local pain or swelling has receded and X-ray showed that localized myositis ossificans was mature. Conner et al6 proposed that surgical intervention should be initiated only when the disease has completely halted. Russo et al7 however, presented a case of non-traumatic myositis ossificans in the left scapula that was associated with severe pain and lacked radiologic evidence of calcification. Early surgical excision resulted in immediate remission of her symptoms.
In our case, the surgical resection was performed 4 months after the appearance of symptoms. Excellent results were achieved during 18 months follow-up, and no reoccurrence or infection complications reported in other literature have happened. In order to avoid the occurrence of soft-tissue contracture and severe osteoporosis, and even pathological fracture, we suggest that surgical resection should be done as soon as the diagnoses is confirmed and patient's condition is permitted.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Bhatia M., Hill J., Macpherson R.I. Radiological case of the month: myositis ossificans circumscripta. Arch Pediatr Adolesc Med. 1995;149:53–54. doi: 10.1001/archpedi.1995.02170130055012. [DOI] [PubMed] [Google Scholar]
- 2.Say F., Coşkun S., Bülbül M. Myositis ossificans on the forearm in a 10-year-old girl. J Pediatr Orthop B. 2015;24:223–225. doi: 10.1097/BPB.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 3.Li J., Zhu L., Hu Y. Clinical analysis of 26 cases of myositis ossificans circumscripta. Chin J Traumatol. 2000;3:124–125. [PubMed] [Google Scholar]
- 4.Leung A.H., Rybak L.D., Rose D.J. Myositis ossificans within the intercondylar notch treated arthroscopically. Skelet Radiol. 2010;39:927–930. doi: 10.1007/s00256-010-0928-y. [DOI] [PubMed] [Google Scholar]
- 5.Kaplan F.S. Skin and bones. Arch Dermatol. 1996;132:815–818. [PubMed] [Google Scholar]
- 6.Conner G.A., Duffy M. Myositis ossificans: a case report of multiple recurrences following third molar extractions and review of the literature. J Oral Maxillofac Surg. 2009;67:920–926. doi: 10.1016/j.joms.2008.06.106. [DOI] [PubMed] [Google Scholar]
- 7.Russo R., Hughes M., Manolios N. Biopsy diagnosis of early myositis ossificans without radiologic evidence of calcification: success of early surgical resection. J Clin Rheumatol. 2010;16:385–387. doi: 10.1097/RHU.0b013e3181fe8c30. [DOI] [PubMed] [Google Scholar]