Abstract
Cisternostomy is defined as opening the basal cisterns to atmospheric pressure. This technique helps to reduce the intracranial pressure in severe head trauma as well as other conditions when the so-called sudden “brain swelling” troubles the surgeon.
We elaborated the surgical anatomy of this procedure as well as the proposed physiology of how cisternostomy works. This novel technique may change the current trends in neurosurgery.
Keywords: Craniocerebral trauma, Cisternostomy, Membrane of liliequist, Virchow robin spaces
Introduction
Head injury is one of the most common causes of neurosurgical admissions, morbidity and mortality. The surgical option for this common and complex problem was done by the residents not employing microsurgery or any surgical advances over the past century. Although the advancement in ICU care has been developed to reduce the mortality for head trauma treatment, it is not an alternative to microneurosurgery. We proposed a modern microsurgical treatment to head injury and discussed the anatomy as well as the proposed physiology to this procedure.
Surgical anatomy of cisternostomy
Opening cisterns in a tight brain is a difficult procedure. Retracting a tight and noncompliant brain was a problem in neurosurgical practice for over a century.1 However, the skullbase approach provides a solution to this problem, making it possible to access to the optico-carotid cistern in an extradural fashion.
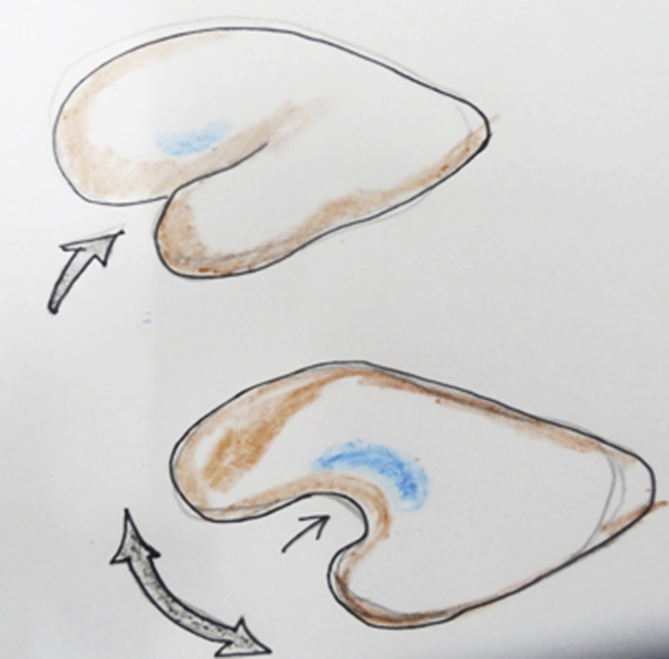
The dura of the frontal lobes and the temporal lobes are adherent to each other and the anterior clinoid process can be considered to be “buried” between these two lobes.2 Opening up these lobes is very important for approaching the cisterns. However, the key to opening these lobes up is the right plane, which is provided by the correct incision of the orbito-meningeal band (Fig. 1).3
Fig. 1.
Orbito-meningeal band.
After a fronto-temporal craniotomy, the correct incision of the lateral orbito-meningeal band results in a plane where one can separate the frontal dura over the anterior clinoid process and the temporal dura over the lateral wall of the cavernous sinus resulting in uncovering the anterior clinoid process as well as opening the fold of the frontal and temporal lobes in a more direct lateral pathway to the cisterns (Fig. 2, Fig. 3).
Fig. 2.
Opening of orbito-meningeal band and “unfurling” of the brain to reach the basal cisterns.
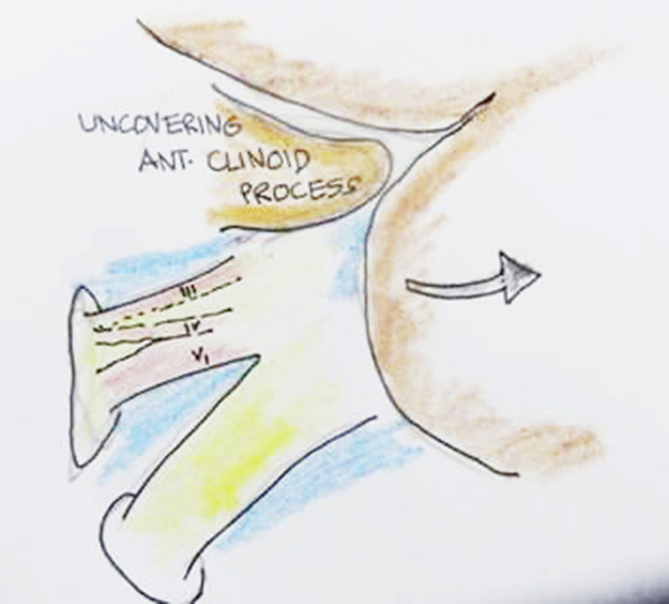
Fig. 3.
Opening of the cavernous region and the anterior clinoid process.
The uncovered anterior clinoid process can be removed easily with rongeurs. If the temporal dura is then separated over the cavernous sinus and the frontal dura is lifted up, one can extradurally reach to the base of the brain where the cisterns are located. After that, a linear dural incision can be placed just above the optic nerve to make use of a lateral subfrontal corridor. Minimal to moderate brain retraction is necessary to reach the inter-optic cistern. There is usually a large amount of blood which comes out following retraction of the orbitofrontal region initially and if the pressure is very high, brain may also herniate. However, this maneuver makes the brain lax and then one can retract the arachnoid covering the optico-carotid cistern and let out the blood. This is the most important maneuver in cisternostomy and for a beginner, all the steps may not be easy. For a decompressive hemicraniectomy, the patient is in supine position, with the head slightly extended and turned to the opposite side about 15°. Then expose the sphenoid ridge upto the superior orbital fissure with a rongeur and open the dura as basal as possible. After that the same lateral subfrontal route may be employed to reach the inter-optic cistern. Once the doctor has this surgical experience and when very tense dura is encountered, the technique mentioned above may be useful.
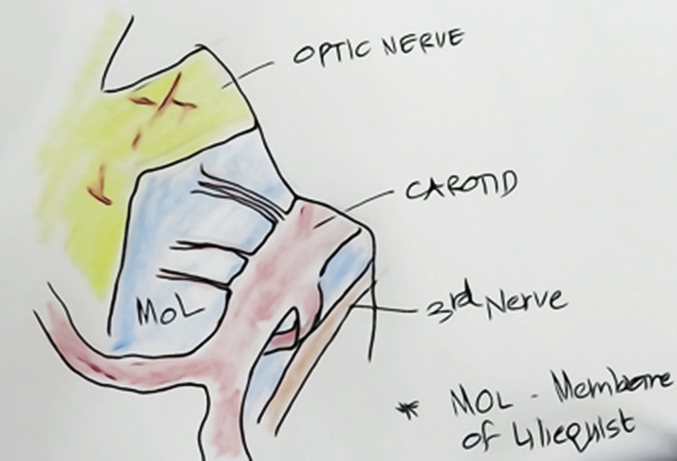
Once the optico-carotid cisterns and the lateral carotid cisterns are opened, the brain becomes lax enough to open the membrane of Liliequist through one of these windows. The membrane of Liliequist is a double-layered membrane through which the third nerve and the posterior communicating artery traverse from the anterior cranial fossa to the posterior cranial fossa (Fig. 4).4, 5
Fig. 4.
Optico-carotid and the lateral carotid cisterns along with membrane of liliequist.
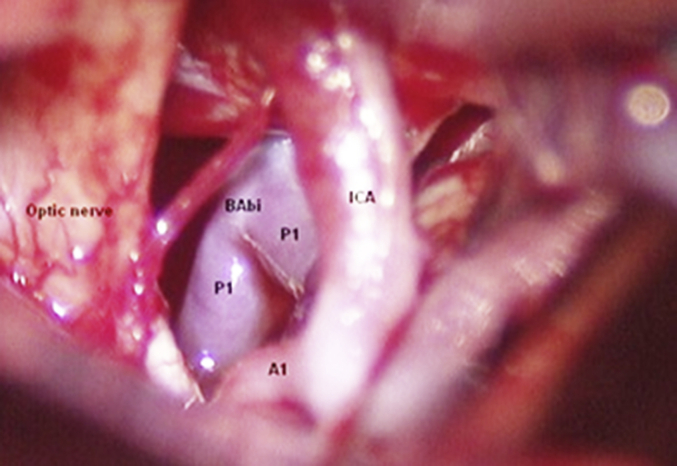
One can follow these structures and open the arachnoid around these structures to reach the basilar complex and the prepontine cistern as well as the interpeduncular cistern (Fig. 5).
Fig. 5.
Visualisation of basilar artery after opening the membrane of liliequist.
Sometimes the posterior clinoid process is very large, which prevents opening of the membrane of Liliequist. In these cases, the posterior clinoid process may be drilled off after opening its dura. This may be done in the window between the carotid and the third nerve or in a very difficult scenario among the A1 segment of anterior cerebral artery, internal carotid artery and the optic nerve. This is an advanced and difficult maneuver and should not be done unless one is experienced.
Once the prepontine cistern and the interpeduncular cistern are opened, the opened cisterns are irrigated copiously with normal saline and a catheter is placed in the prepontine cistern and continuously irrigated. Any small bleeding should be taken care of by this maneuver and the cerebrospinal fluid drainage from the cisterns will be maintained for the next 5 days through the catheter. This catheter may also be used for monitoring intracranial pressure after closure.
Proposed physiology of cisternostomy
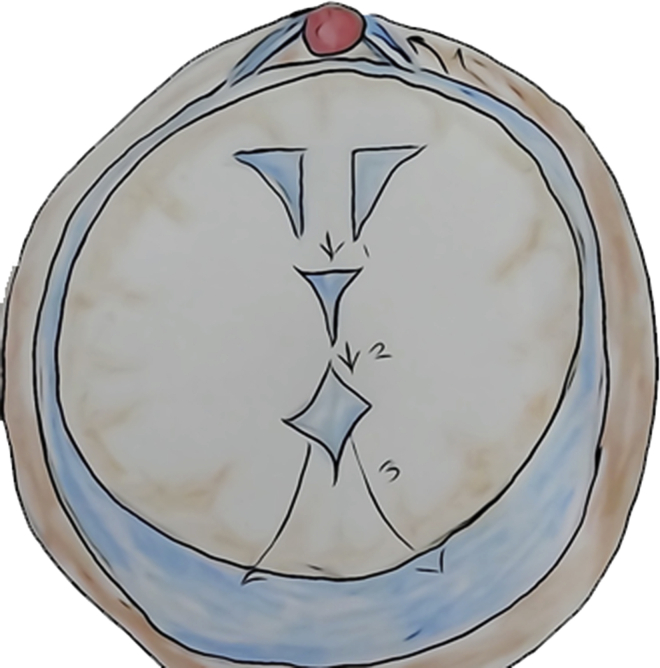
The brain is surrounded by cerebrospinal fluid. Cerebrospinal fluid is produced in the lateral, third and fourth ventricles at a rate of about 500 ml per day. Cerebrospinal fluid passes from the fourth ventricle to the cisterns through the foramen of Magendie and Luschka. The cisterns contain about 120 ml of cerebrospinal fluid. The current theory states that cerebrospinal fluid gets absorbed into the major venous sinuses through arachnoid granulations (Fig. 6).6
Fig. 6.
Normal cerebrospinal fluid flow pathway.
However, glymphatic system has proven that cerebrospinal fluid from the cisterns (and not from the ventricles) does communicate with the parenchyma through Virchow Robin spaces.7, 8
This procedure has also added implication on waste clearance from metabolically highly active brain following trauma. Failure of clearance of tau proteins through cerebrospinal fluid following paravascular pathways would add up the odds of developing neurodegenerative diseases like Alzheimer disease in the future.9
However for cisternostomy this has different implications. The most common phenomenon in severe head trauma is a diffuse traumatic subarachnoid hemorrhage. This causes cisternal pressure to increase with respect to the “intracerebral pressure”. Cerebrospinal fluid is shifted into the brain parenchyma through Virchow Robin spaces and the brain would swell up and also result in losing compliance with rising intracranial pressure (Fig. 7).
Fig. 7.
Raised cisternal pressure due to the traumatic subarachnoid hemorrage shifts cerebrospinal fluid into the brain, causing raised intracerebral pressure.
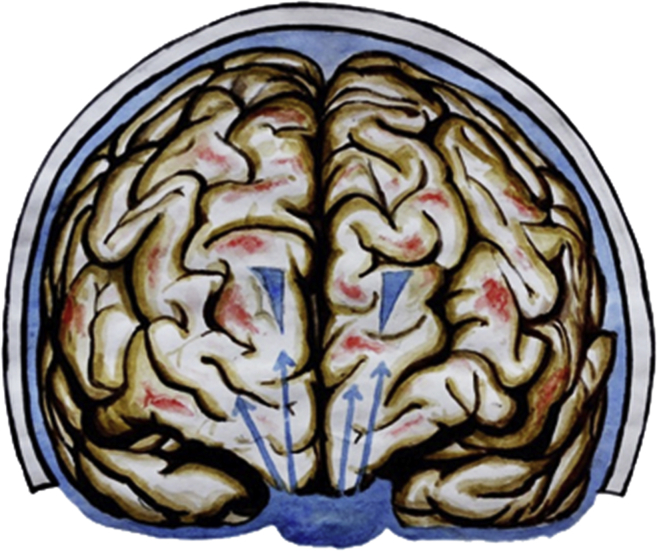
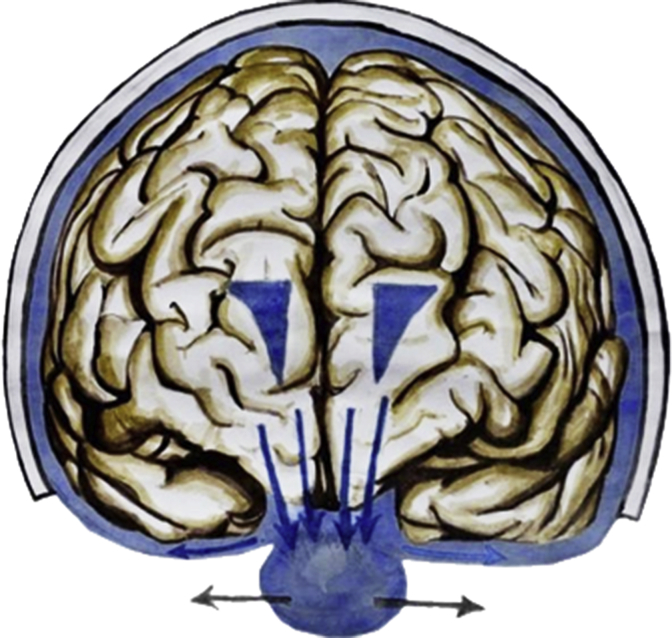
Since the cisterns and the brain communicate, it would be possible to decrease the pressure in both these compartments by opening the cisterns to the atmospheric pressure. This will produce a backshift of cerebrospinal fluid through Virchow Robin spaces, resulting in decreased intra-brain pressure. On the other hand, decompressive hemicraniectomy opens a window above, but it may cause stretch injury to the axons (Fig. 8, Fig. 9).
Fig. 8.
Opening of the cisterns reverses the cisternal pressure gradient, causing cerebrospinal fluid to flow back into the cisterns, thus decreasing the brain pressure.
Fig. 9.
Decompressive hemicraniectomy allows extracalvarial herniation, leading to further deterioration due to axonal stretch and altered blood flow dynamics.
The drainage of cerebrospinal fluid from the cisterns for the next 5 days is beneficial because the lactate, tau and free radicals which would have been present within the injured brain is washed out, minimizing the secondary damage.10, 11, 12
Conclusion
The surgical treatment of head injury which is the most common neurosurgical problem in the developing world has been sidelined for over a hundred years. Residents and young neurosurgeons were practicing a century old surgery based on physiological principles which does not incorporate the modern advances. The procedure of cisternostomy uses microsurgical principles to decrease the intracerebral pressure and reduce secondary damage. Although it is primarily useful in severe head trauma, other cases such as intraoperative malignant brain edema, edema in intracerebral hemorrhage and subarachnoid bleeding will also be suitable for opening cisterns. We believe that every neurosurgical residents and young neurosurgeons should be trained to access and open cisterns as well as to handle the vessels within the cisterns as a part of their training.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Andrews R.J., Bringas J.R. A review of brain retraction and recommendations for minimizing intraoperative brain injury. Neurosurgery. 1993;33:1052–1063. doi: 10.1227/00006123-199312000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Huynh-Le P., Natori Y., Sasaki T. Surgical anatomy of the anterior clinoid process. J Clin Neurosci. 2004;11:283–287. doi: 10.1016/j.jocn.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Fukuda H., Evins A.I., Burrell J.C. The meningo-orbital band: microsurgical anatomy and surgical detachment of the membranous structures through a frontotemporal craniotomy with removal of the anterior clinoid process. J Neurol Surg B Skull Base. 2014;75:125–132. doi: 10.1055/s-0033-1359302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brasil A.V., Schneider F.L. Anatomy of Liliequist's membrane. Neurosurgery. 1993;32:956–960. [PubMed] [Google Scholar]
- 5.Lü J., Zhu X.I. Microsurgical anatomy of Liliequist's membrane. Minim Invasive Neurosurg. 2003;46:149–154. doi: 10.1055/s-2003-40743. [DOI] [PubMed] [Google Scholar]
- 6.Brodbelt A., Stoodley M. CSF pathways: a review. Br J Neurosurg. 2007;21:510–520. doi: 10.1080/02688690701447420. [DOI] [PubMed] [Google Scholar]
- 7.Yang L., Kress B.T., Weber H.J. Evaluating glymphatic pathway function utilizing clinically relevant intrathecal infusion of CSF tracer. J Transl Med. 2013;11:107. doi: 10.1186/1479-5876-11-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iliff J.J., Wang M., Liao Y. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4 doi: 10.1126/scitranslmed.3003748. 147ra111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang J.Z., Xia Y.Y., Grundke-Iqbal I. Abnormal hyperphosphorylation of tau: sites, regulation, and molecular mechanism of neurofibrillary degeneration. J Alzheimers Dis. 2013;33:S123–S139. doi: 10.3233/JAD-2012-129031. [DOI] [PubMed] [Google Scholar]
- 10.Lama S., Auer R.N., Tyson R. Lactate storm marks cerebral metabolism following brain trauma. J Biol Chem. 2014;289:20200–20208. doi: 10.1074/jbc.M114.570978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iliff J.J., Chen M.J., Plog B.A. Impairment of glymphatic pathway function promotes tau pathology after traumatic brain injury. J Neurosci. 2014;34:16180–16193. doi: 10.1523/JNEUROSCI.3020-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O'Connell K.M., Littleton-Kearney M.T. The role of free radicals in traumatic brain injury. Biol Res Nurs. 2013;15:253–263. doi: 10.1177/1099800411431823. [DOI] [PubMed] [Google Scholar]