Abstract
Purpose
To explore the possible surgical factors related with nonunion in femoral shaft fracture following intramedullary nailing.
Methods
We retrospectively analyzed totally 425 patients with femoral shaft fracture in level I urban trauma center, including 254 males and 171 females, with an average age of 37.6 (ranging from 21 to 56) years old. The inclusion criteria included: (1) traumatically closed fracture of femoral shaft, with preoperative films showing non-comminuted fracture, such as transverse fracture, oblique fracture or spiral fracture; (2) closed reduction and fixation with interlocking intramedullary nail at 3–7 days after trauma; (3) complete follow-up data available. The relationship between the following factors (fracture site, reduction degree, direction of nail insertion and nail size) and nonunion was studied.
Results
The incidence of femoral nonunion was 2.8% in patients with closed simple fracture undergoing interlocking intrameduallary nailing, including 11 cases of hypertrophic nonunion. Nonunion was related significantly to distal fracture, unsatisfactory reduction and unreamed nail (p < 0.05). There was no significant difference between antegrade nail and retrograde nail (p > 0.05).
Conclusions
Nonunion in femoral shaft facture following interlocking intramedullary nailing is related to fracture site, fracture reduction and nail diameter. The choice of reamed nails or unreamed nails depends on the fracture site and reduction degree.
Keywords: Femoral shaft fracture, Nonunion, Interlocking intramedullary nailing, Surgery
Introduction
Interlocking intramedullary nailing is a widely accepted treatment for the patients with femoral shaft fracture, with the union rate reported from 85% to 100%.1, 2, 3 Nonunion is a common problem for orthopaedic surgeons. Though with a low incidence, it usually requires multiple procedures to achieve union, which increases the cost and is disadvantageous to the recovery. Recent studies have attempted to identify possible risk factors leading to nonunion following intramedullary nailing in femoral shaft fracture in order to reduce nonunion.4, 5
Open fracture or open reduction is associated with diaphyseal nonunions owing to local blood damage. Closed reduction followed by intramedullary nail fixation is one of ideal surgical methods because it can provide strong internal fixation with a mini-incision but not interfering with local blood supply at the fracture site. Nonunions, however, do occur in these conditions, even in patients with simple femoral fracture, which indicates that other factors, such as the stability of the nail construct, act on fracture healing. The purpose of this study in a series of patients with simple femoral shaft fracture was to evaluate the role of unstable fixation in femoral nonunion, and to find surgical factors resulting in nonunion. Fracture site (proximal or distal), reduction degree (anatomic reduction or unsatisfactory reduction), nail insertion (antegrade or retrograde) and nail size (reamed or unreamed) are considered as relevant factors in the stability of internal fixation. A thorough understanding of these factors and their influence on bone healing may guide us to achieve better operative outcomes and prevent nonunion.
Materials and methods
Six hundred and seventy-two femoral shaft fractures in skeletally mature patients were treated with intramedullary nailing in our department from August 2004 to August 2011. To evaluate the effect of nail stability on union, two doctors were asked to screen the cases from all these patients with medical records and X-ray films available. The inclusion criteria were as follow: (1) traumatically closed fracture of femoral shaft, with preoperative films showing non-comminuted fracture, such as transverse fracture, oblique fracture or spiral fracture; (2) closed reduction and fixation with interlocking intramedullary nail 3–7 days after trauma; (3) complete follow-up data available.
Totally 425 patients were included according to the abovementioned standard, 254 males and 171 females, with an average age of 37.6 (ranging from 21 to 56) years old. Twelve cases among them were diagnosed with diaphyseal nonunion, 3 women and 9 men. Nonunion was defined as a clinically and radiographically unhealed fracture that required additional procedures as determined by the attending surgeon at postoperative 8 months. There was 1 atrophic nonunion and 11 hypertrophic nonunions. Two other doctors who were blind to the study design were asked to read the preoperative and postoperative films and analyzed the condition of the nailing, including fracture site, reduction degree, direction of nail insertion and nail size. Proximal fracture was defined as the fracture between 2 cm distal to lesser trochanter and femoral isthmus; distal fracture was defined as the fracture distal to the femoral isthmus. Satisfactory reduction referred to anatomical reduction; unsatisfactory reduction referred to over 2 mm separation or angulation displacement. Nail size meant reamed nail or unreamed nail.
Fisher's exact test and χ2 test were used to evaluate the significance of the independent variables. p < 0.05 was considered significantly different.
Results
The incidence of femoral nonunion was 2.8% in patients with closed simple fracture undergoing interlocking intrameduallary nailing. Eleven cases of them had hypertrophic nonunions, characterized by evident callus formation but with clear fracture line. Patients' distribution related to various studied factors is shown in Table 1. Nonunion was correlated significantly with distal fracture, unsatisfactory reduction and undreamed nail (p < 0.05). There was no significant difference between antegrade nail and retrograde nail (p > 0.05).
Table 1.
Case distribution by different surgical factors (n).
| Fracture site |
Fracture reduction |
Direction of nail |
Pattern of insertion |
|||||
|---|---|---|---|---|---|---|---|---|
| Item | Proximal | Distal | Satisfactory | Unsatisfactory | Antegrade | Retrograde | Reamed | Unreamed |
| Fracture | 146 | 279 | 270 | 155 | 334 | 91 | 243 | 182 |
| Nonunion | 3 | 9 | 4 | 8 | 10 | 2 | 5 | 7 |
| p | <0.05 | <0.05 | >0.05 | <0.05 | ||||
Surgical characteristics of all 12 patients with nonunion are demonstrated in Table 2. Among all 12 patients, 9 suffered from distal femoral fracture, 10 underwent antegrade nailing, 8 presented unsatisfactory reduction and 7 received unreamed nail fixation.
Table 2.
Surgical characteristics of all 12 patients with nonunion.
| Fracture site |
Fracture reduction |
Direction of nail |
Pattern of insertion |
|||||
|---|---|---|---|---|---|---|---|---|
| Case No. | Proximal | Distal | Satisfactory | Unsatisfactory | Antegrade | Retrograde | Reamed | Unreamed |
| 1 | + | + | + | + | ||||
| 2 | + | + | + | + | ||||
| 3 | + | + | + | + | ||||
| 4 | + | + | + | + | ||||
| 5 | + | + | + | + | ||||
| 6 | + | + | + | + | ||||
| 7 | + | + | + | + | ||||
| 8 | + | + | + | + | ||||
| 9 | + | + | + | + | ||||
| 10 | + | + | + | + | ||||
| 11 | + | + | + | + | ||||
| 12 | + | + | + | + | ||||
Discussion
Nonunion of the femoral shaft facture represents a challenge for orthopaedic surgeons and a serious socioeconomic problem for the patients mainly due to blood supply damage or inadequate fracture stability.6 Avascular change at the fracture site resulted from open fracture or open reduction leads to atrophic nonunion occasionally, while unstable fixation contributes to hypertrophic nonunion. In this study, 425 patients with closed femoral shaft fracture underwent close reduction and intramedullary nailing. As a result, nonunion occurred in 12 cases, including 11 cases of hypertrophic nonunions, which suggested that unstable fixation attributed a lot to this kind of nonunion following nailing.
Diameter of the nail is usually a key issue with regard to the stability of intramedullary nail. Reaming allows the insertion of a larger nail, which provides a greater stability, but may induce a greater periosteal reaction. The literature reported a fewer nonunions associated with reamed nailing than with unreamed nailing.7, 8 Two hundred and twenty-four patients were enrolled in a multicenter, prospective, randomized clinical trial by Canadian Orthopaedic Trauma Society.9 Eight of 107 fractures (7.5%) in the group without reaming had a nonunion compared with two of 121 fractures (1.7%) in the group with reaming. They concluded that intramedullary nailing of femoral shaft fractures without reaming resulted in a significantly higher rate of nonunion compared with intramedullary nailing with reaming. Despite the clinical success achieved by intramedullary nailing after reaming, several concerns have been proposed on the biological consequences of reaming. Reaming disrupts the cortical blood flow, causing various extent of thermal necrosis in cortical bone. Elevated intramedullary pressures associated with reaming can also result in marrow embolization, which may trigger the development of adult respiratory distress syndrome.10, 11 These limitations prevent reaming technique from a wide application.
Totally 243 simple fractures accepted a reamed nail in our study, and 5 patients were found with nonunion. Interestingly, all the fractures of the 5 cases were at the distal femur. This suggested that reamed nailing can provide a strong enough stability for a proximal fracture, but it sometimes fails for the fractures distal to isthmus. For a distal fracture, a large antegrade nail can stabilize the proximal and the isthmus. But the distal femoral medullary cavity is bigger, and the two distal locking screws can not limit the nail, which decreases the stability of this construct. Thus the micromotion across the fracture gap prevents bone healing. A blocking screw helps to control the nail, and is used for reduction as well as treatment of nonunion.12, 13
Retrograde nailing is effective for stabilization of femoral shaft fractures. It was once thought to provide a higher healing rate than antegrade nail, especially in cases of distal fracture. Papadokostakis et al14 evaluated the efficacy of retrograde nailing in the treatment of distal femur fractures and femoral shaft fractures with a systematic review of the literature. He found that the patients with femoral shaft fractures had a mean time to union of 3.2 months, while the union rate was 94.2%; the rate of knee pain, malunion and re-operation was 24.5%, 7.4% and 17.7%, respectively. So he concluded that retrograde intramedullary nailing be a reliable treatment option mainly for distal femoral fractures. However, in the management of diaphyseal fractures, retrograde intramedullary nailing was associated with high rate of knee pain and low rate of fracture union.15 In our research, there was no significant difference in nonunion rate between antegrade nail and retrograde nail.
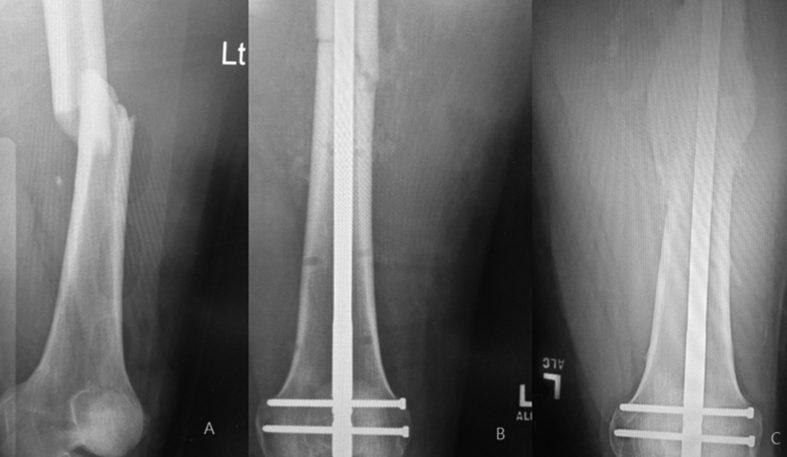
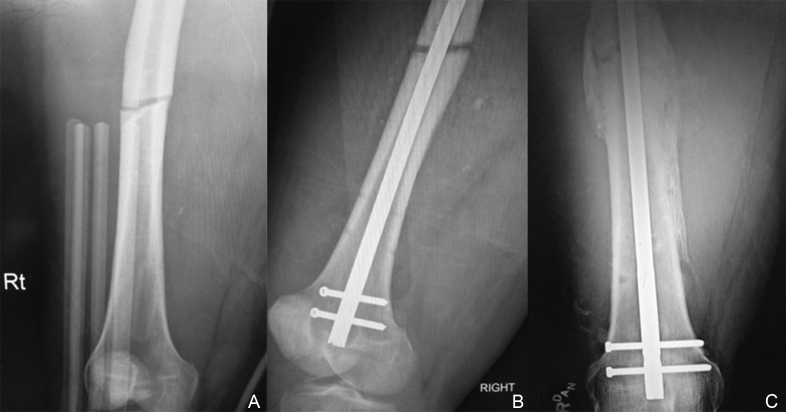
We demonstrated a typical case who suffered from the same fracture in similar sites of both femurs and underwent the same surgery: closed reduction and unreamed retrograde nailing (Fig. 1, Fig. 2). He obtained nonunion in the right femur and union in the left femur 8 months later. His X-ray films taken immediately after surgery were observed retrospectively and it was found that the right femur was reduced inaccurately with a gap of 2 mm. It was concluded that the gap was unfavorable for bridging the fracture and even made the fracture unstable. It turned out to be a hypertrophic nonunion finally. To our acknowledgement, it was the first research that indicated fracture reduction related to nonunion following femoral nailing.
Fig. 1.
Fracture healing of the left femur at postoperative 8 months. A: X-ray showed traumatic fracture at distal femur; B: Postoperative film showed satisfactory reduction and unreamed nailing; C: Plenty of callus and union.
Fig. 2.
Nonunion in the right femur of the same patient at postoperative 8 months. A: X-ray showed traumatic fracture at distal femur; B: Postoperative film showed unreamed nailing but unsatisfactory reduction; C: hypertrophic nonunion were found 8 months following surgery.
Nonunion of femoral shaft fracture is undoubtedly a multifactorial process. Some researchers reported that tobacco use and delayed weight-bearing are risk factors for femoral nonunion after intramedullary nailing for diaphyseal femur fractures.16 But they are not surgical factors and depend on patients' providing. In the present study, we did not take them into account. According to the radiological data and medical records, we found that nonunion in femoral shaft following nailing was related to fracture site, fracture reduction and nail diameter. In most cases, the clinical outcome is not influenced by single factor while some simultaneous factors lead to final nonunion. To a patient with femoral shaft fracture, using a reamed nail or unreamed nail depends on the fracture site and reduction degree.
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Shroeder J.E., Mosheiff R., Khoury A. The outcome of closed, intramedullary exchange nailing with reamed insertion in the treatment of femoral shaft nonunions. J Orthop Trauma. 2009;23:653–657. doi: 10.1097/BOT.0b013e3181a2a337. [DOI] [PubMed] [Google Scholar]
- 2.Basumallick M.N., Bandopadhyay A. Effect of dynamization in open interlocking nailing of femoral fractures. A prospective randomized comparative study of 50 cases with a 2-year follow-up. Acta Orthop Belg. 2002;68:42–48. [PubMed] [Google Scholar]
- 3.Karadimas E.J., Papadimitriou G., Theodoratos G. The effectiveness of the antegrade reamed technique: the experience and complications from 415 traumatic femoral shaft fractures. Strateg Trauma Limb Reconstr. 2009;4:113–121. doi: 10.1007/s11751-009-0071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malik M.H., Harwood P., Diggle P. Factors affecting rates of infection and nonunion in intramedullary nailing. J Bone Jt Surg Br. 2004;86:556–560. [PubMed] [Google Scholar]
- 5.Giannoudis P.V., MacDonald D.A., Matthews S.J. Nonunion of the femoral diaphysis. The influence of reaming and non-steroidal anti-inflammatory drugs. J Bone Jt Surg Br. 2000;82:655–658. doi: 10.1302/0301-620x.82b5.9899. [DOI] [PubMed] [Google Scholar]
- 6.Gelalis I.D., Politis A.N., Arnaoutoglou C.M. Diagnostic and treatment modalities in nonunions of the femoral shaft: a review. Injury. 2011;43:980–988. doi: 10.1016/j.injury.2011.06.030. [DOI] [PubMed] [Google Scholar]
- 7.Duan X., Li T., Mohammed A.Q. Reamed intramedullary nailing versus unreamed intramedullary nailing for shaft fracture of femur: a systematic literature review. Arch Orthop Trauma Surg. 2011;131:1445–1452. doi: 10.1007/s00402-011-1311-8. [DOI] [PubMed] [Google Scholar]
- 8.Reynders P.A., Broos P.L. Healing of closed femoral shaft fractures treated with the AO unreamed femoral nail. A comparative study with the AO reamed femoralnail. Injury. 2000;31:367–371. doi: 10.1016/s0020-1383(00)00005-x. [DOI] [PubMed] [Google Scholar]
- 9.Canadian Orthopaedic Trauma Society Nonunion following intramedullary nailing of the femur with and without reaming. Results of a multicenter randomized clinical trial. J Bone Jt Surg Am. 2003;85:2093–2096. [PubMed] [Google Scholar]
- 10.Husebye E.E., Lyberg T., Opdahl H. Cardiopulmonary response to reamed intramedullary nailing of the femur comparing traditional reaming with a one-step reamer-irrigator-aspirator reaming system: an experimental study in pigs. J Trauma. 2010;69:E6–E14. doi: 10.1097/TA.0b013e3181d27928. [DOI] [PubMed] [Google Scholar]
- 11.Kanakaris N.K., Morell D., Gudipati S. Reaming irrigator aspirator system: early experience of its multipurpose use. Injury. 2011;42:S28–S34. doi: 10.1016/S0020-1383(11)70009-2. [DOI] [PubMed] [Google Scholar]
- 12.Gao K.D., Huang J.H., Li F. Treatment of aseptic diaphyseal nonunion of the lower extremities with exchange intramedullary nailing and blocking screws without open bone graft. Orthop Surg. 2009;1:264–268. doi: 10.1111/j.1757-7861.2009.00041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ostrum R.F., Maurer J.P. Distal third femur fractures treated with retrograde femoral nailing and blocking screws. J Orthop Trauma. 2009;23:681–684. doi: 10.1097/BOT.0b013e3181ad61f2. [DOI] [PubMed] [Google Scholar]
- 14.Papadokostakis G., Papakostidis C., Dimitriou R. The role and efficacy of retrograding nailing for the treatment of diaphyseal and distal femoral fractures: a systematic review of the literature. Injury. 2005;36:813–822. doi: 10.1016/j.injury.2004.11.029. [DOI] [PubMed] [Google Scholar]
- 15.El Moumni M., Schraven P., ten Duis H.J. Persistent knee complaints after retrograde unreamed nailing of femoral shaft fractures. Acta Orthop Belg. 2010;76:219–225. [PubMed] [Google Scholar]
- 16.Taitsman L.A., Lynch J.R., Agel J. Risk factors for femoral nonunion after femoral shaft fracture. J Trauma. 2009;67:1389–1392. doi: 10.1097/TA.0b013e318182afd0. [DOI] [PubMed] [Google Scholar]