Abstract
The case of a six-month-old child with pancreatoblastoma is presented. Pancreatoblastoma is a rare primary neoplasm of childhood, usually presenting in children ranging from 2 −8 years old. The radiologic findings vary from solid to complex masses. This case is unusual due to the young age of the patient.
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging
Introduction
Pancreatoblastoma is a rare primary neoplasm of childhood. It was reported for the first time in 1957 [1]. Pancreatoblastoma usually affects children ranging from one to eight years old and elderly individuals [2, 3, 4]. It usually occurs in children under the age of 7 years and is often misdiagnosed as neuroblastoma or hepatoblastoma, with the chief complaints being a palpable mass with anorexia and vomiting. At microscopy, pancreatoblastoma resembles partially differentiated acini of fetal origin [5, 6]. The tumor is clinically silent and large at the time of presentation. The symptoms are usually due to the mass effect and include: vomiting, constipation and pain [7].
Case Report
A six month-old female child was admitted to the hospital for evaluation of abdominal distention, jaundice and a palpable abdominal mass. Laboratory values showed high bilirubin levels suggesting biliary obstruction.
An abdominal ultrasound demonstrated a 14.6 × 13.1 cm heterogeneous mass with cystic and solid components and a few centrally echogenic foci consistent with calcifications in the subhepatic region. This mass displaced small bowel loops ventrally and the right kidney posterior and inferiorly. The mass also compressed the extrahepatic bile ducts and was associated with intrahepatic biliary ductal dilatation. Due to the sonographic features of the mass, neuroblastoma was initially diagnosed (Fig. 1). CT was performed to identify the origin and involvement of other abdominal structures (Figure 2, Figure 3, Figure 4). Afterwards, the patient was taken to the operating room where a partial surgical resection of the mass was performed and histopathology confirmed the lesion to be a pancreatoblastoma (Figs. 5-6). Unfortunately, the patient’s bile ducts were injured during surgery, and the patient died eight days later from this complication.
Figure 1.

6-month-old child with pancreatoblastoma. Sonography shows a complex abdominal mass, with a few echogenic foci centrally dispersed consistent with calcifications.
Figure 2.
6-month-old child with pancreatoblastoma. Contrast-enhanced CT demonstrates a well defined retroperitoneal heterogeneous mass, unevenly enhancing, with cystic areas consistent with hemorrhage or tumor necrosis, displacing the right kidney, bowel loops and the liver posterior, anterior and laterally respectively in A. Figures B and C show the superior mesenteric vessels and the remnant pancreatic parenchyma (arrows).
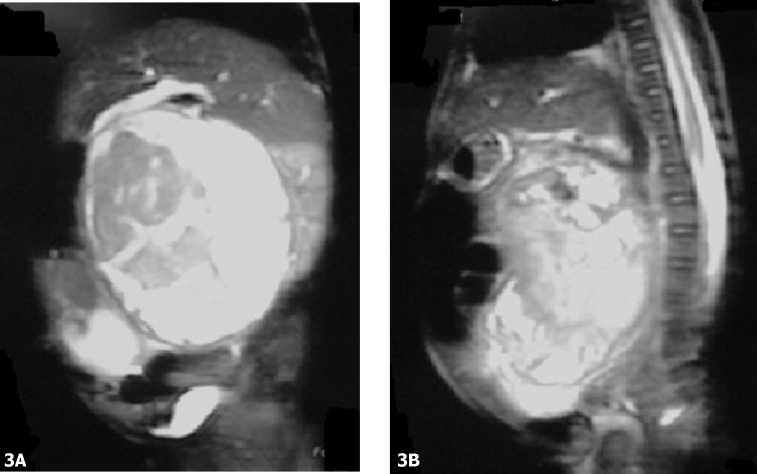
Figure 3.
6-month-old child with pancreatoblastoma. A, Coronal and B, sagittal (b) T2-weighted MR demonstrates a large heterogeneous mass with high signal intensity areas consistent with cystic necrosis and isointense areas compared to the spleen that represents the solid component of the tumor. Cephalad and lateral displacement of the liver and spleen respectively is shown.
Figure 4.

6-month-old child with pancreatoblastoma. Bivalved gross specimen of the tumor resected during surgery.
Figure 5.

6-month-old child with pancreatoblastoma. High power photomicrograph shows acinar structures within pancreatic tissue typical of pancreatoblastoma (H & E).
Discussion
Pancreatoblastoma is a rare primary neoplasm of childhood, usually presenting in children ranging from 2 −8 years old [2]. This case is interesting because our patient presented at a much earlier age.
Pancreatic tumors in children are exceptionally rare, causing less than 0.2% of pediatric deaths due to malignancy. Pancreatoblastoma has been reported in children, teens and elderly populations [2, 8, 9, 10]. The congenital form is associated with Beckwith-Wiedemann syndrome and has been characterized as a cystic form [9, 11]. The risk of a malignancy (nephroblastoma, hepatoblastoma, rhabdomyosarcoma and pancreatoblastoma) associated with Beckwith-Wiedemann syndrome is reported to be about 4%.
Lee et al [12] described the radiologic findings in patients with pancreatoblastoma. The tumors were depicted as large, well defined, multilobulated masses with enhancing septa at CT. Histologically, pancreatoblastoma is characterized by the presence of squamous corpuscles and aggregates or large epithelioid cells with formation of acini [1].
The AFIP recently reviewed 10 cases of pancreatoblastoma, and reported that the tumors may initially appear to be pancreatic or hepatic. Pancreatoblastomas are usually heterogenous with well-defined margins and definite enhancement. On MR, the tumors usually demonstrate low to intermediate signal on T1W images and high signal intensity on T2W images. Calcification, ascites and dilatation of the pancreatic or biliary ducts are not commonly reported. Adenopathy and vascular invasion are rarely detected on imaging studies [13].
The differential diagnosis of pancreatoblastoma should also include lymphoma, retroperitoneal sarcoma, hematoma, and solid and papillary epithelial neoplasms [14]. Since our patient was significantly younger than the usual age range for pancreatoblastoma, the differential diagnosis also included neuroblastoma, non-Hodgkin lymphoma and hepatoblastoma. Hepatoblastoma was ruled out since the mass was shown to be extrahepatic with the liver displaced superiorly. While non-Hodgkin lymphoma may also present as an abdominal mass, the hepatic involvement is typically diffuse with involvement of other organs, as opposed to discreet masses noted in this case. These tumors also behave very aggressively with large size at initial presentation, and are often associated with local and distant spread.
The primary treatment of pancreatoblastoma is surgical resection. The role of adjuvant chemotherapy for a surgically resectable tumor is uncertain, although chemotherapy is commonly used on an empiric basis [15]. Radiotherapy and chemotherapy are added for metastatic or recurrent disease [16]. The prognosis is good for patients with a resectable mass [17].
Footnotes
Published: July 15, 2009
References
- 1.Becker W. Pancreatoduodenectomy for carcinoma of the pancreas in an infant; report of a case. Ann Surg. 1957;145:864–870. doi: 10.1097/00000658-195706000-00008. [PubMed] discussions, 870-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shorter N, Glick R, Klimstra D, Brennan M, Laquaglia M. Malignant pancreatic tumors in childhood and adolescence: The Memorial Sloan-Kettering experience, 1967 to present. J Pediatr Surg. 2002;37:887–892. doi: 10.1053/jpsu.2002.32897. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Kloppel G, Maillet B. Classification and staging of pancreatic nonendocrine tumors. Radiol Clin North Am. 1989;27:105–119. [PubMed] [PubMed] [Google Scholar]
- 4.Friedman A, Edmonds P. Rare pancreatic malignancies. Radiol Clin North Am. 1989;27:177–190. [PubMed] [PubMed] [Google Scholar]
- 5.Horie A, Yano Y, Kotoo Y, Miwa A. Morphogenesis of pancreatoblastoma, infantile carcinoma of the pancreas: report of two cases. Cancer. 1977;39:247–254. doi: 10.1002/1097-0142(197701)39:1<247::aid-cncr2820390138>3.0.co;2-f. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Cubilla A, Fitzgerald P. Classification of pancreatic cancer (nonendocrine) Mayo Clin Proc. 1979;54:449–458. [PubMed] [PubMed] [Google Scholar]
- 7.Passmore S, Berry P, Oakhill A. Recurrent pancreatoblastoma with inappropriate adrenocorticotrophic hormone secretion. Arch Dis Child. 1988;63:1494–1496. doi: 10.1136/adc.63.12.1494. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang C, Perrin E, Hertzler J, Brough A. Cystadenoma of the pancreas with cytomegalovirus infection in a female infant. Arch Pathol Lab Med. 1980;104:7–8. [PubMed] [PubMed] [Google Scholar]
- 9.Klimstra D, Wenig B, Adair C, Heffess C. Pancreatoblastoma. A clinicopathologic study and review of the literature. Am J Surg Pathol. 1995;19:1371–1389. doi: 10.1097/00000478-199512000-00005. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Levey J, Banner B. Adult pancreatoblastoma: a case report and review of the literature. Am J Gastroenterol. 1996;91:1841–1844. [PubMed] [PubMed] [Google Scholar]
- 11.Drut R, Jones M. Congenital pancreatoblastoma in Beckwith-Wiedemann syndrome: an emerging association. Pediatr Pathol. 1988;8:331–339. doi: 10.3109/15513818809042976. [PubMed] [DOI] [PubMed] [Google Scholar]
- 12.Lee JY, Kim IO, Kim WS. CT and US findings of pancreatoblastoma. J Comput Assist Tomogr. 1996;20:370–374. doi: 10.1097/00004728-199605000-00007. [PubMed] [DOI] [PubMed] [Google Scholar]
- 13.Montemarano H, Lonergan GJ, Bulas DI, Selby DM. Pancreatoblastoma: imaging findings in 10 patients and review of the literature. Radiology. 2000;214:476–482. doi: 10.1148/radiology.214.2.r00fe36476. [PubMed] [DOI] [PubMed] [Google Scholar]
- 14.Ros PR, Mortele KJ, Lee S, Pelsser V. CT and MRI of the Abdomen and Pelvis: a Teaching File. Wolters Kluwer Lippincott Williams & Wilkins; Philadelphia, PA: 2006. [Google Scholar]
- 15.Chung EM, Travis MD, Conran RM. Pancreatic tumors in children: radiologic-pathologic correlation. Radiographics. 2006;26:1211–1238. doi: 10.1148/rg.264065012. [PubMed] [DOI] [PubMed] [Google Scholar]
- 16.Willnow U, Willberg B, Schwamborn D. Pancreatoblastoma in children. Case report and review of the literature. Eur J Pediatr Surg. 1996;6:369–372. doi: 10.1055/s-2008-1071019. [PubMed] [DOI] [PubMed] [Google Scholar]
- 17.Chun Y, Kim W, Park K. Pancreatoblastoma. J Pediatr Surg. 1997;32:1612–1615. doi: 10.1016/s0022-3468(97)90465-6. [PubMed] [DOI] [PubMed] [Google Scholar]