Abstract
COPD is the third-largest killer in the world, and certainly takes a toll on the health care system. Recurrent COPD exacerbations accelerate lung-function decline, worsen mortality, and consume over US$50 billion in health care spending annually. This has led to a tide of payment reforms eliciting interest in strategies reducing preventable COPD exacerbations. In this review, we analyze and discuss the evidence for COPD action plan-based self-management strategies. Although action plans may provide stabilization of acute symptomatology, there are several limitations. These include patient-centered attributes, such as comprehension and adherence, and nonadherence of health care providers to established guidelines. While no single intervention can be expected independently to translate into improved outcomes, structured together within a comprehensive integrated disease-management program, they may provide a robust paradigm.
Keywords: exacerbations, self-management, integrated disease-management program
Introduction
COPD is a leading cause of death worldwide, with an estimated prevalence of almost 10% in adults aged ≥40 years.1 Approximately 50% of patients with COPD have at least one exacerbation per year, and over 20% are readmitted within 30 days, with a total of nearly 800,000 hospitalizations and US$50 billion in health care costs annually.2–4 This has led the Centers for Medicare and Medicaid Services to impose financial penalties for hospitals with 30-day readmissions after COPD exacerbations, as part of the Hospital Readmissions Reduction Program. Consequently, it is not surprising that last few years have seen a significant interest in self-management strategies to reduce recurrent exacerbations and hospitalizations. The aim of this review was to examine the utility of COPD action plan-based self-management strategies in acute exacerbations of COPD (AECOPD) and discuss its impact on outcomes.
Action plans: definitions and components
Action plans have been well studied in asthma for decades, and have had more of an established role compared to COPD. A PubMed search (conducted November 2015) for “action plans” along with “asthma” yielded over 400 results compared to 69 results for “COPD”. Traditionally defined as a personalized document generated by health professionals, action plans are intended to promote self-management of exacerbations that may otherwise necessitate acute care, via the patient’s early recognition of an exacerbation and self-initiation of interventions (typically antibiotics and oral corticosteroids). Asthma action plans rely on the variability in symptomatology and peak expiratory flow thought to reflect changes in asthma severity. Although not shown to improve mortality and morbidity, these appear to be protective against severe asthma exacerbations.5,6 More recent data, however, suggest that asthma action plans may not confer additional benefit to patients already receiving subspecialty care.7 COPD action plans on the other hand have been sparsely investigated.
Role of steroids in COPD exacerbations
For decades, oral steroids have played a quintessential role in the management of hospitalized patients with AECOPD. Two previous randomized controlled trials – a Veterans Affairs study8 and a similar study9 – demonstrated that corticosteroids played an integral role in treating inpatient AECOPD. A recent review by Self et al10 specifically investigating the role of oral steroids in the setting of COPD action plans found that two11,12 (of five) published randomized controlled trials containing a total of 933 patients provided evidence of reduced rates of hospitalization by the use of comprehensive COPD action plans, while the others13–15 showed no differences in rates of rehospitalization. While there was no effect on overall mortality, oral steroids appeared to increase time to next exacerbation.
COPD action plans universally integrate oral steroids in the self-management of AECOPD. However, there is no consensus on the length of corticosteroid therapy. Among hospitalized patients, prior studies have shown that a 2-week therapy course was equivalent or noninferior to extended 6-week tapers of corticosteroids after COPD exacerbations.16 More recently, a randomized controlled trial enrolled 314 COPD patients that had presented to the emergency room (ER) for acute exacerbations (289 were admitted), and randomized them to 5 days versus 14 days of 40 mg prednisone therapy. The authors reported that a 5-day course of prednisone was noninferior to a 14-day course in terms of likelihood of exacerbation in the subsequent 180 days, time to next exacerbation, and hospital readmissions.17 A systematic review comparing different durations of oral steroids similarly concluded that a 5-day course might be comparable to a 14-day course for most patients.18 These data suggest that a 5-day course may be adequate in treating AECOPD. While oral steroids have been shown to be equally efficacious to systemic steroids in hospitalized patients,19 few studies have compared the efficacy of inhaled corticosteroids to oral steroids.20 Inhaled steroids have not been studied in the setting of an action plan for AECOPD, which typically utilizes short courses of oral steroids.
Role of antibiotics in COPD exacerbations
The majority of patients with AECOPD are treated with antibiotics. However, the efficacy of antibiotics remains less certain for outpatient (versus inpatient) treatment of AECOPD, partly due to the available data being mainly from prospective nonrandomized studies (Table 1). Earlier studies have shown an overall decrease in treatment failures (resolution of symptoms), as well as relapse rates, in patients with AECOPD that received antibiotics when compared to patients that did not receive outpatient antibiotics.21,22 Also the presence of green (purulent) sputum was found to be 94.4% sensitive and 77% specific for the yield of a high bacterial load and the likelihood of patients to benefit most from antibiotic therapy.23 A subsequent study by Allegra et al indicated that change in sputum color, especially from yellowish to brownish, was associated with bacterial exacerbations, and their study found an increased yield of Gram-negative and Pseudomonas aeruginosa/Enterobacteriaceae-type organisms.24 In contrast, in a smaller study (n=22), Brusse-Keizer et al found a weak association between bacterial load and sputum color in patients admitted with AECOPD.25
Table 1.
Summary of studies evaluating effectiveness of COPD action plan
| Study | Bourbeau et al11 | Sridhar et al13 | Sedeno et al32 | Effing et al14 | Rice et al12 | Fan et al15 |
|---|---|---|---|---|---|---|
| Study design | RCT | RCT | Retrospective analysis of multicenter RCT | Prospective 2×2 factorial trial | Single-blinded RCT | RCT |
| Patients, n | 96 (I) and 95 (C) | 61 (I) and 61 (C) | 85 (I) and 81(C) | 70 (I) and 72 (C) | 372 (I) and 371 (C) | 209 (I) and 217 (C) |
| Exclusion of comorbidities | No | Yes | No | Yes | No | No |
| Severe exacerbation (>1 hospitalization/year) | Yes | No | Yes | No | No | Yes |
| Action-plan coordinator | Nurses, RT, and physiotherapist | RN | Case manager | RN | RT | Case managers |
| Education format and follow-up | Flip-chart modules: 1 hour/week at home for 7–8 weeks Weekly telephone calls for 8 weeks, then monthly for 1 year |
Nurse phone calls every month and home visits every 3 months | Home teaching: 1 hour/week for 7–8 weeks Weekly telephone calls for 8 weeks, then monthly for 1 year |
Four small-group 2-hour self-management sessions Telephone calls at 4, 13, and 26 weeks |
Single 1- to 1.5-hour group-education session Monthly phone calls |
Four individual 90-minute weekly sessions Phone calls: once a month for 3 months, then every 3 months |
| Action plan | ||||||
| Initial steroid | No | Yes | No | Yes | Yes | Yes |
| Initial steroid + Abx | Yes | No | Yes | No | No | No |
| Conditional Abx addition | No | Yes | No | Yes | Yes | Yes |
| Follow-up period | 1 year | 2 years | 1 year | 1 year | I year | 1 year |
| Definition of exacerbation/AP triggers | Change in respiratory symptoms lasting for minimum 24 hours and respiratory status to return to baseline for at least 72 hours | Unscheduled need for health care, need for steroid tablets, or antibiotics for worsening of their COPD | Change in one of three respiratory symptoms lasting >24 hours | A clear negative change in two major symptoms or one major and one minor symptom from baseline for at least 2 consecutive days | GOLD criteria | Increase in or new onset of one or more respiratory symptoms for at least 2 days |
| Decrease in AECOPD | No | No | No | No, but fewer exacerbation days in I group | Yes | No |
| Decrease in ER visits and hospital admissions | Yes | No | Yes | No (trend) | Yes | No |
| Reduced urgent physician visits | Yes | Yes | Yes | Yes | Not assessed | Not assessed |
| Mortality | Not assessed | Mortality benefit in intervention group | Not assessed | Not assessed | No benefit | Increased mortality in the intervention group |
| Cost-effective? | Not assessed | Yes | Not assessed | Yes | Not assessed | Not assessed |
Abbreviations: RCT, randomized controlled trial; ER, emergency room; AECOPD, acute exacerbation of COPD; I, intervention; C, control; resp, respiratory; Abx, antibiotic; AP, action plan; RT, respiratory therapist; RN, registered nurse; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
More recently, Llor et al showed in a randomized trial of antibiotics for exacerbations of mild-to-moderate COPD that antibiotic use was associated with a higher chance of clinical cure, as well as longer time to next exacerbation.26 Using data from the placebo arm of this trial, Miravitlles et al evaluated predictors of failure (defined as incomplete resolution, persistence, or worsening of symptoms that require treatment or hospitalization) without antibiotics. They reported that increase in sputum purulence and elevated C-reactive protein concentration was associated with an increased risk of failure without antibiotics.27 Roede et al reported in a population-based cohort study that adding antibiotics to oral steroids was associated with a reduced risk of subsequent exacerbation, especially in patients with recurrent exacerbations, and also reduced risk of all-cause mortality.28
Overall, while these data do not suggest robust efficacy, they do justify the clinical practice of addition of antibiotics for the management of AECOPD, particularly when recurrent and associated with sputum purulence (Table 1). Choosing an optimal antimicrobial agent remains one of the challenges, since a third to two-thirds of exacerbations may be caused by viruses, while bacterial infections appear to trigger about half of AECOPD.29,30
Self-management using COPD action plans and outcomes
Although COPD action plans have not been formally investigated, several studies have included them as part of a comprehensive-care program (in patients with at least one exacerbation in the preceding year), and reported their effects on reducing ER visits, hospital admissions, and/or overall effect on quality of life (Table 2). A recent Cochrane review concluded that self-management interventions in patients with COPD are associated with improved health-related quality of life and reduction in respiratory-related hospital admissions.31
Table 2.
Summary of studies investigating role of antibiotics in COPD exacerbation
| Study | Anthonisen et al21 | Stockley et al23 | Allegra et al24 | Roede et al28 | Llor et al26 | Miravitlles et al27 |
|---|---|---|---|---|---|---|
| Study design | Double-blind RCT | Prospective cohort | Prospective cohort | Retrospective data analysis | Multicenter double-blind placebo-controlled RCT | Data analysis of placebo arm of RCT |
| Patients | 182 (I) and 180 (C) outpatients with AECOPD | 121 Outpatients with AECOPD | 315 Outpatients with AECOPD | 842 Outpatients with AECOPD | 156 (I) and 152 (C) outpatients with AECOPD | 152 Outpatients with AECOPD |
| Disease severity | Any COPD | Any COPD | Moderate-to-severe COPD | Any COPD | Mild-to-moderate COPD | Mild-to-moderate COPD |
| Methods | Patients who developed AECOPD treated with Abx vs placebo | Patients with AECOPD assessed with sputum analysis + Abx prescription to patients with green purulent sputum | Qualitative and quantitative sputum analysis of patients that developed AECOPD | Comparison of long-term risk of subsequent exacerbation after treatment with steroid alone vs combination steroid and Abx | Patients were randomized to receive amoxicillin/clavulanate 125/500 mg TID vs placebo TID for 8 days during AECOPD | Assessment of failure rate in patients with AECOPD that did not receive Abx therapy |
| Results | Increased success rate with Abx (68%) vs placebo (55%) Reduced failure rate with deterioration: Abx (10%) vs placebo (19%) Faster rate of peak-flow recovery in Abx group |
Positive bacterial culture if purulence (84%) vs mucoid (38%) Purulent sputum 94.4% sensitive and 77% specific for yield of high bacterial load |
Absence of bacterial growth in mucoid (22%) vs purulent (5%) sputum samples Gram-negative and P. aeruginosa/Enterobacteriaceae isolated more frequently in sputum when FEV1 <35% |
Treatment of AECOPD with steroid and Abx combination increased the median time from second to third AECOPD (199 vs 258 days) | 74.1% (I) versus 59.9% (C) achieved end of therapy cure Median time to next exacerbation 233 days versus 160 days CRP >40 mg/L predicted failure with placebo |
Increased clinical failure without Abx (19.9%) vs with Abx (9.5) Only factor associated with risk of treatment failure was sputum purulence and CRP >40 mg/L |
| Adverse effects (antibiotic group) | No | Not assessed | NA | Not assessed | Yes (mainly GI-related) | NA |
| Major findings/conclusions | Abx treatment during AECOPD associated with earlier resolution of symptoms | Patients with purulent sputum likely to benefit from Abx therapy High CRP seen in patients with sputum purulence |
Purulent sputum associated with bacterial growth in AECOPD Deepening sputum color associated with increased yield of Gram-negative bacteria |
Abx addition to oral CS associated with reduced risk of subsequent exacerbations and decreased risk of all-cause mortality | Abx use associated with increase in median time to next exacerbation CRP a useful marker for treatment response | Among Anthonisen criteria, only sputum purulence predicts failure without Abx |
Abbreviations: RCT, randomized controlled trial; AECOPD, acute exacerbation of COPD; I, intervention; C, control; CRP, C-reactive protein; Abx, antibiotic; FEV1, forced expiratory volume in 1 second; P. aeruginosa, Pseudomonas aeruginosa; TID, ter in die (thrice daily); GI, gastrointestinal; NA, not applicable; CS, corticosteroid.
In a prospective randomized controlled trial, Bourbeau et al evaluated the effect of disease-specific self-management intervention on hospitalizations in COPD patients.11 COPD patients with at least one hospitalization for COPD in the previous year were divided into a usual-care group and a self-management group. Patients in the self-management group received comprehensive patient education along, with a customized action plan that consisted of a symptom-monitoring list and prescriptions consisting of antibiotics and oral steroids for 10–14 days to be initiated promptly when symptom changes were noted. The study noted a significant decrease in hospital admissions and exacerbation rates in the self-management group when compared to the usual-care group.
In another randomized controlled trial, Sridhar et al used a hospital database to identify patients admitted for AECOPD in the 4 years prior to the study who had not previously undergone pulmonary rehabilitation (PR).13 All patients randomized to the intervention group (versus usual care) underwent PR and self-management education and were given a written COPD action plan. Nurses made monthly telephone calls and quarterly home visits for a period of 2 years and reinforced self-management education. While the authors found no difference in the rate of hospital readmissions, there was an overall reduction in the number of urgent outpatient physician visits, with a number needed to treat of 1.79. Interestingly, there was a significant reduction in COPD-related deaths in the intervention group (one of six deaths) compared to the control group (eight of 12 deaths; P=0.015).
In a retrospective analysis by Sedeno et al, COPD patients were randomly assigned to usual care or to a comprehensive self-management program that included a written action plan with prescription of antibiotics and prednisone for self-administration in the event of an exacerbation, and case-manager support with scheduled phone calls.32 There were a total of 661 exacerbations among the 166 patients studied. While the authors did not find any difference in the frequency of exacerbations between the two groups, there was a significant decrease in exacerbations that led to hospitalizations in the action-plan group (17.2% vs 36.3%, P<0.001). This was associated with a change in patient behavior as part of self-management (more than 50% patients promptly self-treated their exacerbations with prescribed antibiotics and prednisone).
Effing et al prospectively studied the effects of self-management along with an action plan on severity of COPD exacerbations in patients that underwent a mandatory smoking-cessation program prior to randomization.14 A total of 142 moderate-to-severe COPD patients were randomized to the control group (received self-management education alone) or the intervention group (also received action plan). There was a trend toward fewer exacerbation days and hospital admissions, which was statistically significant only in patients with high exacerbation days per year. Although the frequency of exacerbations was identical in both groups, the authors found a significant reduction in health care contact in the intervention group (P=0.043) that seemed to translate into cost savings.
Rice et al conducted a randomized controlled trial at five Veterans Affairs medical centers, where 743 patients with spirometrically confirmed COPD that were at high risk (hospitalization, home oxygen use, or steroid use in the prior year) of hospital admission were randomized to usual care or a simple disease-management arm.12 Patients in the disease-management arm received a written action plan and an educational intervention, during which they attended a single 1- to 1.5-hour group-education session conducted by a respiratory therapist. This was followed by monthly phone calls made by the case manager. The study found a significant reduction in the frequency of COPD-related hospitalizations and ER visits (0.82 per patient in usual care versus 0.48 per patient in intervention group, P<0.001). Additionally, the study also reported a statistically significant decrease in incidence of hospitalizations for cardiac or pulmonary conditions other than COPD and for all causes of hospitalizations and ER visits. In contrast, Fan et al performed a randomized controlled trial in 426 COPD patients that had required hospitalization in the prior year and randomized them to usual care or comprehensive-care intervention (comprised of educational intervention and written action plan with prescriptions).15 The education program run by case managers consisted of four individual 90-minute weekly sessions using an educational booklet, followed by group sessions, and monthly phone calls thereafter that were mainly focused on various aspects of self-management. The study found no difference in the incidence of exacerbations or COPD-related hospitalizations (27% versus 24%, P=0.62). Somewhat surprisingly, however, the study had to be prematurely terminated, due to increased mortality in the intervention group versus usual care (28 overall deaths versus ten, P=0.003; ten COPD-related deaths versus three, P=0.053; intervention group versus usual care, respectively). Of note, although the action plan was designed for patients to initiate treatment within 48 hours of onset of exacerbation symptoms, there was no difference in the actual initiation of treatment between the groups in either prednisone (6.4 days versus 7.7 days, P=0.48) or antibiotics (7 days versus 6.8 days, P=0.84). Interestingly, at a 6-month follow-up after the intervention was stopped, there was no significant difference in deaths (overall or COPD-related) between the groups.
Taken together, these data suggest that the available body of literature on use of action plans in COPD is at best inconclusive. While COPD action plans appear to improve some aspects of COPD exacerbations (reduce severity of exacerbations and/or hospitalizations), they are highly unlikely to have any impact on mortality (Table 2). Unfortunately, the studies lack standardization of action-plan constituents and are flawed with concurrent initiation of one or more self-management strategies, making it nearly impossible to determine which components may have contributed to reported benefit (or lack thereof).
Action plans and self-management strategies may be necessary but not sufficient to improve COPD outcomes
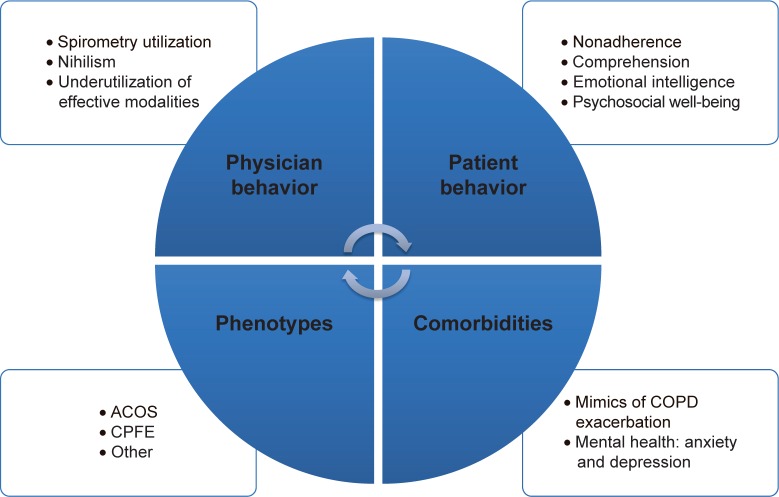
While empowering the patient to better understand the disease process and proactively collaborate with the treating generalist or specialist, self-management strategies still face several challenges limiting their ability to reduce COPD exacerbations and rehospitalizations effectively. When integrated into a multidisciplinary disease-management program, they may be effective in reducing health care utilization.33 Limitations include patient-centered attributes, such as comprehension and what might be called emotional intelligence, which directly affect self-management abilities,34–36 as well as other factors that may not be addressed by simplistic strategies (Figure 1).
Figure 1.
COPD action plans: limitations and barriers.
Abbreviations: ACOS, asthma–COPD overlap syndrome; CPFE, combined pulmonary fibrosis and emphysema.
Patient-centered attributes: psychosocial aspects of COPD
Self-management strategies in COPD often center upon the ability of the patient to identify an exacerbation and trigger the action plan. Therefore, the success of any action plan-based strategy would rely heavily on patient understanding and the ability to actually become effective self-managers. Unfortunately, patients with frequent exacerbations have been reported to have a poor understanding of the term “exacerbation”.37 Just as PR improves exercise capacity but does not seamlessly translate into increased physical activity,38,39 prescription of an action plan cannot be assumed to translate into timely implementation of the same. Indeed, even in the setting of randomized controlled trials with systematic educational interventions, the majority of COPD patients did not implement self-management strategies as prescribed.15,40,41 In one trial, only 42% (75 of 150 enrolled patients with AECOPD) were classified as being successful self-managers demonstrating appropriate use of self-management therapies.41 It seems reasonable to assume that in clinical practice, patient adherence to action plans may be low.
Psychosocial factors may contribute to patient nonadherence toward both pharmacologic and nonpharmacological therapies. Further, exacerbations appear to take a toll on the psychosocial well-being of the patient, and this is underestimated by physicians.37 Negative emotions and lack of psychosocial well-being have been strongly associated with patient nonadherence.42,43 A recent report associated emotional intelligence (the capacity to understand and manage personal thoughts and feelings positively influencing social well-being) in patients with COPD with self-management abilities independent of age and disease severity.34 Interestingly, it is a trainable skill that may be learned and acquired at any age, and may represent a novel form of rehabilitation complementing existing strategies.
Spirometry underutilization
Physician adherence to recommended use of spirometry remains poor and poses a major challenge, especially since three of every four patients with obstructive lung disease have never had spirometry.44–46 How do we reconcile literature that suggests both underdiagnosis47–50 and overdiagnosis45,51–53 of COPD? It is conceivable that there might in fact be an element of misdiagnosis. This had been well reported in the outpatient setting in patients with symptomatology of obstructive lung disease that were clinically diagnosed as COPD.54–56 More recently, we have reported misdiagnosis in patients with frequent exacerbations (more than two hospitalizations or ER visits in the prior year) of severe COPD and asthma.45 Misdiagnosis was found in 26% (87 of 333) of patients, while another 12% (41 of 333) had obstructive lung diseases other than asthma and COPD. Interestingly, spirometry underutilization was found to be an independent risk factor for misdiagnosis. Uptake of major society guidelines requiring a spirometry confirmation of a diagnosis of COPD is disappointingly low.44,57 Prescribing empiric therapies with a clinical diagnosis of COPD (without spirometric confirmation) is the norm and not the exception in current clinical practice. In the real world (versus clinical trials), it may be unrealistic to expect self-management strategies designed for COPD to work in a population where the component of “O” (obstruction) and the very diagnosis is in doubt!
Comorbidities
The past decade has improved our understanding of COPD as more of a complex and polygenic disease. Most patients with COPD have major concomitant medical comorbidities that directly or indirectly worsen outcomes.58 Up to 94% of patients have at least one comorbid disease, and almost half of all patients have more than three comorbidities.58,59 High prevalence of obstructive sleep apnea,60 pulmonary embolism,61 and heart failure62 has been reported in a quarter to a half of patients with AECOPD. Although there is a distinct urge to diagnose (and treat) a smoker with cough as COPD, smoking-related pulmonary diseases themselves are a large group of distinct diseases, all of which may present with clinical symptomatology of COPD.63–65 An interesting study investigating the “comorbidome” of COPD evaluated the relationship between 79 comorbidities and risk of death in patients with COPD over a median of 51 months.66 They found 12 comorbidities that negatively influenced survival and increased risk of death. Anxiety and depression have been increasingly identified in frequent exacerbators of COPD, and have recently been implicated to have a direct association with exacerbations and health care utilization.67–69 Patients on long-term oxygen therapy appear to be at risk.70 Depression is a known risk factor for noncompliance with medical treatment and poor outcomes.42 Unfortunately, data suggest that up to two-thirds of patients with concomitant COPD and depression may not receive treatment for their depression.71 Overall, these are missed opportunities for improving outcomes by addressing potentially treatable conditions, possibly within a multidisciplinary program.33
These data beg the question of whether a subset of COPD patients with recurrent hospitalizations have COPD exacerbations or rather exacerbations of symptoms that mimic COPD. Interestingly, a recent investigation using Medicare-claim data from over 26 million inpatient admissions (of which 3.5% were COPD admissions) reported a 30-day COPD readmission rate of 20.2%.2 Only half the readmitted COPD patients were admitted for respiratory-related illnesses, with COPD accountable for only 27.6% of readmissions. These data suggest that a subset of patients with COPD exacerbations may not get readmitted for COPD, and further emphasize the possibility of comorbidities playing an important role in recurrent hospitalizations in patients with COPD. Action plan-based self-management strategies are unlikely to be effective when the driving pathology of the exacerbation is indeed an undiagnosed comorbidity.
Phenotypes: asthma–COPD overlap syndrome
Finally, while phenotypic differentiation of asthma and COPD remains challenging, recent data have now well described an asthma–COPD overlap syndrome that may exist in nearly 20% of patients with obstructive lung disease.72,73 Unfortunately, this phenotype is thought to have increased disease severity and exacerbations than either condition alone.74 It is likely that patients with this phenotype would have systematically been excluded from research investigations of asthma as well as COPD, further complicating extrapolation of existing data to this phenotype. Although not well understood, there has recently been an increasing recognition of a distinct phenotype with coexistence of upper lobe-dominant emphysema and pulmonary fibrosis, termed combined pulmonary fibrosis and emphysema.75,76 While our current understanding of clinically different phenotypes of COPD is growing,77,78 these patients may need stratified medicine and personalized care above and beyond simplistic self-management strategies.
Conclusion
COPD is a multisystem comorbid syndrome and the third-leading cause of death in the US. A transformational change to holistic strategies may be necessary to improve outcomes for this complex multisystem disease. While there is certainly a role for COPD action plan-based self-management strategies, the burden remains on the physician. An accurate diagnosis of COPD with objective confirmation of airflow obstruction is critical prior to consideration of any self-management. Identifying and addressing concomitant comorbidities cannot be overemphasized. Optimizing psychosocial well-being and mental health may be necessary for improving patient adherence and the success of any interventions. Strategies are more likely to be effective when the focus of care is patient-oriented (versus disease-oriented or COPD-specific). This may require a truly multidisciplinary approach. A well-structured integrated program may provide such a platform to improve outcomes in frequent exacerbators of COPD.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28(3):523–532. doi: 10.1183/09031936.06.00124605. [DOI] [PubMed] [Google Scholar]
- 2.Shah T, Churpek MM, Perraillon MC, Konetzka RT. Understanding why patients with COPD get readmitted: a large national study to delineate the Medicare population for the readmissions penalty expansion. Chest. 2015;147(5):1219–1226. doi: 10.1378/chest.14-2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pasquale MK, Sun SX, Song F, Hartnett HJ, Stemkowski SA. Impact of exacerbations on health care cost and resource utilization in chronic obstructive pulmonary disease patients with chronic bronchitis from a predominantly Medicare population. Int J Chron Obstruct Pulmon Dis. 2012;7:757–764. doi: 10.2147/COPD.S36997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miller JD, Foster T, Boulanger L, et al. Direct costs of COPD in the U.S.: an analysis of Medical Expenditure Panel Survey (MEPS) data. COPD. 2005;2(3):311–318. doi: 10.1080/15412550500218221. [DOI] [PubMed] [Google Scholar]
- 5.Cowie RL, Revitt SG, Underwood MF, Field SK. The effect of a peak flow-based action plan in the prevention of exacerbations of asthma. Chest. 1997;112(6):1534–1538. doi: 10.1378/chest.112.6.1534. [DOI] [PubMed] [Google Scholar]
- 6.Effectiveness of routine self monitoring of peak flow in patients with asthma. BMJ. 1994;308(6928):564–567. No authors listed. [PMC free article] [PubMed] [Google Scholar]
- 7.Sheares BJ, Mellins RB, Dimango E, et al. Do patients of subspecialist physicians benefit from written asthma action plans? Am J Respir Crit Care Med. 2015;191(12):1374–1383. doi: 10.1164/rccm.201407-1338OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niewoehner DE, Erbland ML, Deupree RH, et al. Effect of systemic glucocorticoids on exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1999;340(25):1941–1947. doi: 10.1056/NEJM199906243402502. [DOI] [PubMed] [Google Scholar]
- 9.Davies L, Angus RM, Calverley PM. Oral corticosteroids in patients admitted to hospital with exacerbations of chronic obstructive pulmonary disease: a prospective randomised controlled trial. Lancet. 1999;354(9177):456–460. doi: 10.1016/s0140-6736(98)11326-0. [DOI] [PubMed] [Google Scholar]
- 10.Self TH, Patterson SJ, Headley AS, Finch CK. Action plans to reduce hospitalizations for chronic obstructive pulmonary disease exacerbations: focus on oral corticosteroids. Curr Med Res Opin. 2014;30(12):2607–2615. doi: 10.1185/03007995.2014.934795. [DOI] [PubMed] [Google Scholar]
- 11.Bourbeau J, Julien M, Maltais F, et al. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management intervention. Arch Intern Med. 2003;163(5):585–591. doi: 10.1001/archinte.163.5.585. [DOI] [PubMed] [Google Scholar]
- 12.Rice KL, Dewan N, Bloomfield HE, et al. Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med. 2010;182(7):890–896. doi: 10.1164/rccm.200910-1579OC. [DOI] [PubMed] [Google Scholar]
- 13.Sridhar M, Taylor R, Dawson S, Roberts NJ, Partridge MR. A nurse led intermediate care package in patients who have been hospitalised with an acute exacerbation of chronic obstructive pulmonary disease. Thorax. 2008;63(3):194–200. doi: 10.1136/thx.2007.077578. [DOI] [PubMed] [Google Scholar]
- 14.Effing T, Kerstjens H, van der Valk P, Zielhuis G, van der Palen J. (Cost)-effectiveness of self-treatment of exacerbations on the severity of exacerbations in patients with COPD: the COPE II study. Thorax. 2009;64(11):956–962. doi: 10.1136/thx.2008.112243. [DOI] [PubMed] [Google Scholar]
- 15.Fan VS, Gaziano JM, Lew R, et al. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med. 2012;156(10):673–683. doi: 10.7326/0003-4819-156-10-201205150-00003. [DOI] [PubMed] [Google Scholar]
- 16.Woods JA, Wheeler JS, Finch CK, Pinner NA. Corticosteroids in the treatment of acute exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9:421–430. doi: 10.2147/COPD.S51012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leuppi JD, Schuetz P, Bingisser R, et al. Short-term vs conventional glucocorticoid therapy in acute exacerbations of chronic obstructive pulmonary disease: the REDUCE randomized clinical trial. JAMA. 2013;309(21):2223–2231. doi: 10.1001/jama.2013.5023. [DOI] [PubMed] [Google Scholar]
- 18.Walters JA, Tan DJ, White CJ, Wood-Baker R. Different durations of corticosteroid therapy for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;12:CD006897. doi: 10.1002/14651858.CD006897.pub3. [DOI] [PubMed] [Google Scholar]
- 19.de Jong YP, Uil SM, Grotjohan HP, Postma DS, Kerstjens HA, van den Berg JW. Oral or IV prednisolone in the treatment of COPD exacerbations: a randomized, controlled, double-blind study. Chest. 2007;132(6):1741–1747. doi: 10.1378/chest.07-0208. [DOI] [PubMed] [Google Scholar]
- 20.Maltais F, Ostinelli J, Bourbeau J, et al. Comparison of nebulized budesonide and oral prednisolone with placebo in the treatment of acute exacerbations of chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med. 2002;165(5):698–703. doi: 10.1164/ajrccm.165.5.2109093. [DOI] [PubMed] [Google Scholar]
- 21.Anthonisen NR, Manfreda J, Warren CP, Hershfield ES, Harding GK, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med. 1987;106(2):196–204. doi: 10.7326/0003-4819-106-2-196. [DOI] [PubMed] [Google Scholar]
- 22.Adams SG, Melo J, Luther M, Anzueto A. Antibiotics are associated with lower relapse rates in outpatients with acute exacerbations of COPD. Chest. 2000;117(5):1345–1352. doi: 10.1378/chest.117.5.1345. [DOI] [PubMed] [Google Scholar]
- 23.Stockley RA, O’Brien C, Pye A, Hill SL. Relationship of sputum color to nature and outpatient management of acute exacerbations of COPD. Chest. 2000;117(6):1638–1645. doi: 10.1378/chest.117.6.1638. [DOI] [PubMed] [Google Scholar]
- 24.Allegra L, Blasi F, Diano P, et al. Sputum color as a marker of acute bacterial exacerbations of chronic obstructive pulmonary disease. Respir Med. 2005;99(6):742–747. doi: 10.1016/j.rmed.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 25.Brusse-Keizer MG, Grotenhuis AJ, Kerstjens HA, et al. Relation of sputum colour to bacterial load in acute exacerbations of COPD. Respir Med. 2009;103(4):601–606. doi: 10.1016/j.rmed.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 26.Llor C, Moragas A, Hernandez S, Bayona C, Miravitlles M. Efficacy of antibiotic therapy for acute exacerbations of mild to moderate chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(8):716–723. doi: 10.1164/rccm.201206-0996OC. [DOI] [PubMed] [Google Scholar]
- 27.Miravitlles M, Moragas A, Hernandez S, Bayona C, Llor C. Is it possible to identify exacerbations of mild to moderate COPD that do not require antibiotic treatment? Chest. 2013;144(5):1571–1577. doi: 10.1378/chest.13-0518. [DOI] [PubMed] [Google Scholar]
- 28.Roede BM, Bresser P, Prins JM, Schellevis F, Verheij TJ, Bindels PJ. Reduced risk of next exacerbation and mortality associated with antibiotic use in COPD. Eur Respir J. 2009;33(2):282–288. doi: 10.1183/09031936.00088108. [DOI] [PubMed] [Google Scholar]
- 29.Rohde G, Wiethege A, Borg I, et al. Respiratory viruses in exacerbations of chronic obstructive pulmonary disease requiring hospitalisation: a case-control study. Thorax. 2003;58(1):37–42. doi: 10.1136/thorax.58.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seemungal T, Harper-Owen R, Bhowmik A, et al. Respiratory viruses, symptoms, and inflammatory markers in acute exacerbations and stable chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;164(9):1618–1623. doi: 10.1164/ajrccm.164.9.2105011. [DOI] [PubMed] [Google Scholar]
- 31.Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014;3:CD002990. doi: 10.1002/14651858.CD002990.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sedeno MF, Nault D, Hamd DH, Bourbeau J. A self-management education program including an action plan for acute COPD exacerbations. COPD. 2009;6(5):352–358. doi: 10.1080/15412550903150252. [DOI] [PubMed] [Google Scholar]
- 33.Jain VV, Allison R, Beck SJ, et al. Impact of an integrated disease management program in reducing exacerbations in patients with severe asthma and COPD. Respir Med. 2014;108(12):1794–1800. doi: 10.1016/j.rmed.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 34.Benzo RP, Kirsch JL, Dulohery MM, Abascal-Bolado B. Emotional intelligence: a novel outcome associated with wellbeing and self-management in chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2016;13(1):10–16. doi: 10.1513/AnnalsATS.201508-490OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bryant J, McDonald VM, Boyes A, Sanson-Fisher R, Paul C, Melville J. Improving medication adherence in chronic obstructive pulmonary disease: a systematic review. Respir Res. 2013;14:109. doi: 10.1186/1465-9921-14-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lareau SC, Yawn BP. Improving adherence with inhaler therapy in COPD. Int J Chron Obstruct Pulmon Dis. 2010;5:401–406. doi: 10.2147/COPD.S14715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kessler R, Stahl E, Vogelmeier C, et al. Patient understanding, detection, and experience of COPD exacerbations: an observational, interview-based study. Chest. 2006;130(1):133–142. doi: 10.1378/chest.130.1.133. [DOI] [PubMed] [Google Scholar]
- 38.Ng LW, Mackney J, Jenkins S, Hill K. Does exercise training change physical activity in people with COPD? A systematic review and meta-analysis. Chron Respir Dis. 2012;9(1):17–26. doi: 10.1177/1479972311430335. [DOI] [PubMed] [Google Scholar]
- 39.Garcia-Aymerich J, Pitta F. Promoting regular physical activity in pulmonary rehabilitation. Clin Chest Med. 2014;35(2):363–368. doi: 10.1016/j.ccm.2014.02.011. [DOI] [PubMed] [Google Scholar]
- 40.Bischoff EW, Hamd DH, Sedeno M, et al. Effects of written action plan adherence on COPD exacerbation recovery. Thorax. 2011;66(1):26–31. doi: 10.1136/thx.2009.127621. [DOI] [PubMed] [Google Scholar]
- 41.Bucknall CE, Miller G, Lloyd SM, et al. Glasgow supported self-management trial (GSuST) for patients with moderate to severe COPD: randomised controlled trial. BMJ. 2012;344:e1060. doi: 10.1136/bmj.e1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160(14):2101–2107. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 43.Turan O, Yemez B, Itil O. The effects of anxiety and depression symptoms on treatment adherence in COPD patients. Prim Health Care Res Dev. 2014;15(3):244–251. doi: 10.1017/S1463423613000169. [DOI] [PubMed] [Google Scholar]
- 44.Han MK, Kim MG, Mardon R, et al. Spirometry utilization for COPD: how do we measure up? Chest. 2007;132(2):403–409. doi: 10.1378/chest.06-2846. [DOI] [PubMed] [Google Scholar]
- 45.Jain VV, Allison DR, Andrews S, Mejia J, Mills PK, Peterson MW. Misdiagnosis among frequent exacerbators of clinically diagnosed asthma and COPD in absence of confirmation of airflow obstruction. Lung. 2015;193(4):505–512. doi: 10.1007/s00408-015-9734-6. [DOI] [PubMed] [Google Scholar]
- 46.Sokol KC, Sharma G, Lin YL, Goldblum RM. Choosing wisely: adherence by physicians to recommended use of spirometry in the diagnosis and management of adult asthma. Am J Med. 2015;128(5):502–508. doi: 10.1016/j.amjmed.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 47.Albers M, Schermer T, Molema J, et al. Do family physicians’ records fit guideline diagnosed COPD? Fam Pract. 2009;26(2):81–87. doi: 10.1093/fampra/cmp005. [DOI] [PubMed] [Google Scholar]
- 48.Bednarek M, Maciejewski J, Wozniak M, Kuca P, Zielinski J. Prevalence, severity and underdiagnosis of COPD in the primary care setting. Thorax. 2008;63(5):402–407. doi: 10.1136/thx.2007.085456. [DOI] [PubMed] [Google Scholar]
- 49.Martinez CH, Mannino DM, Jaimes FA, et al. Undiagnosed obstructive lung disease in the United States: associated factors and long-term mortality. Ann Am Thorac Soc. 2015;12(12):1788–1795. doi: 10.1513/AnnalsATS.201506-388OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Walters JA, Hansen EC, Walters EH, Wood-Baker R. Under-diagnosis of chronic obstructive pulmonary disease: a qualitative study in primary care. Respir Med. 2008;102(5):738–743. doi: 10.1016/j.rmed.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 51.Ghattas C, Dai A, Gemmel DJ, Awad MH. Over diagnosis of chronic obstructive pulmonary disease in an underserved patient population. Int J Chron Obstruct Pulmon Dis. 2013;8:545–549. doi: 10.2147/COPD.S45693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schermer TR, Smeele IJ, Thoonen BP, et al. Current clinical guideline definitions of airflow obstruction and COPD overdiagnosis in primary care. Eur Respir J. 2008;32(4):945–952. doi: 10.1183/09031936.00170307. [DOI] [PubMed] [Google Scholar]
- 53.Zwar NA, Marks GB, Hermiz O, et al. Predictors of accuracy of diagnosis of chronic obstructive pulmonary disease in general practice. Med J Aust. 2011;195(4):168–171. doi: 10.5694/j.1326-5377.2011.tb03271.x. [DOI] [PubMed] [Google Scholar]
- 54.Tinkelman DG, Price DB, Nordyke RJ, Halbert RJ. Misdiagnosis of COPD and asthma in primary care patients 40 years of age and over. J Asthma. 2006;43(1):75–80. doi: 10.1080/02770900500448738. [DOI] [PubMed] [Google Scholar]
- 55.Izquierdo JL, Martin A, de Lucas P, Rodriguez-Gonzalez-Moro JM, Almonacid C, Paravisini A. Misdiagnosis of patients receiving inhaled therapies in primary care. Int J Chron Obstruct Pulmon Dis. 2010;5:241–249. doi: 10.2147/copd.s11123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Collins BF, Ramenofsky D, Au DH, Ma J, Uman JE, Feemster LC. The association of weight with the detection of airflow obstruction and inhaled treatment among patients with a clinical diagnosis of COPD. Chest. 2014;146(6):1513–1520. doi: 10.1378/chest.13-2759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Global Initiative for Chronic Obstructive Lung Disease . Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease. Bethesda (MD): GOLD; 2015. [Accessed April 20, 2016]. Available from: http://www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html. [Google Scholar]
- 58.Hillas G, Perlikos F, Tsiligianni I, Tzanakis N. Managing comorbidities in COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:95–109. doi: 10.2147/COPD.S54473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sharafkhaneh A, Petersen NJ, Yu HJ, Dalal AA, Johnson ML, Hanania NA. Burden of COPD in a government health care system: a retrospective observational study using data from the US Veterans Affairs population. Int J Chron Obstruct Pulmon Dis. 2010;5:125–132. doi: 10.2147/copd.s8047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Soler X, Gaio E, Powell FL, et al. High prevalence of obstructive sleep apnea in patients with moderate to severe chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2015;12(8):1219–1225. doi: 10.1513/AnnalsATS.201407-336OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tillie-Leblond I, Marquette CH, Perez T, et al. Pulmonary embolism in patients with unexplained exacerbation of chronic obstructive pulmonary disease: prevalence and risk factors. Ann Intern Med. 2006;144(6):390–396. doi: 10.7326/0003-4819-144-6-200603210-00005. [DOI] [PubMed] [Google Scholar]
- 62.Rutten FH, Cramer MJ, Lammers JW, Grobbee DE, Hoes AW. Heart failure and chronic obstructive pulmonary disease: an ignored combination? Eur J Heart Fail. 2006;8(7):706–711. doi: 10.1016/j.ejheart.2006.01.010. [DOI] [PubMed] [Google Scholar]
- 63.Caminati A, Cavazza A, Sverzellati N, Harari S. An integrated approach in the diagnosis of smoking-related interstitial lung diseases. Eur Respir Rev. 2012;21(125):207–217. doi: 10.1183/09059180.00003112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Margaritopoulos GA, Vasarmidi E, Jacob J, Wells AU, Antoniou KM. Smoking and interstitial lung diseases. Eur Respir Rev. 2015;24(137):428–435. doi: 10.1183/16000617.0050-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Walsh SL, Nair A, Desai SR. Interstitial lung disease related to smoking: imaging considerations. Curr Opin Pulm Med. 2015;21(4):407–416. doi: 10.1097/MCP.0000000000000178. [DOI] [PubMed] [Google Scholar]
- 66.Divo M, Cote C, de Torres JP, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(2):155–161. doi: 10.1164/rccm.201201-0034OC. [DOI] [PubMed] [Google Scholar]
- 67.Xu W, Collet JP, Shapiro S, et al. Independent effect of depression and anxiety on chronic obstructive pulmonary disease exacerbations and hospitalizations. Am J Respir Crit Care Med. 2008;178(9):913–920. doi: 10.1164/rccm.200804-619OC. [DOI] [PubMed] [Google Scholar]
- 68.Jennings JH, Digiovine B, Obeid D, Frank C. The association between depressive symptoms and acute exacerbations of COPD. Lung. 2009;187(2):128–135. doi: 10.1007/s00408-009-9135-9. [DOI] [PubMed] [Google Scholar]
- 69.Ng TP, Niti M, Tan WC, Cao Z, Ong KC, Eng P. Depressive symptoms and chronic obstructive pulmonary disease: effect on mortality, hospital readmission, symptom burden, functional status, and quality of life. Arch Intern Med. 2007;167(1):60–67. doi: 10.1001/archinte.167.1.60. [DOI] [PubMed] [Google Scholar]
- 70.Paz-Diaz H, Montes de Oca M, Lopez JM, Celli BR. Pulmonary rehabilitation improves depression, anxiety, dyspnea and health status in patients with COPD. Am J Phys Med Rehabil. 2007;86(1):30–36. doi: 10.1097/phm.0b013e31802b8eca. [DOI] [PubMed] [Google Scholar]
- 71.Yohannes AM, Baldwin RC, Connolly MJ. Prevalence of sub-threshold depression in elderly patients with chronic obstructive pulmonary disease. Int J Geriatr Psychiatry. 2003;18(5):412–416. doi: 10.1002/gps.851. [DOI] [PubMed] [Google Scholar]
- 72.Postma DS, Reddel HK, ten Hacken NH, van den Berge M. Asthma and chronic obstructive pulmonary disease: similarities and differences. Clin Chest Med. 2014;35(1):143–156. doi: 10.1016/j.ccm.2013.09.010. [DOI] [PubMed] [Google Scholar]
- 73.Soriano JB, Davis KJ, Coleman B, Visick G, Mannino D, Pride NB. The proportional Venn diagram of obstructive lung disease: two approximations from the United States and the United Kingdom. Chest. 2003;124(2):474–481. doi: 10.1378/chest.124.2.474. [DOI] [PubMed] [Google Scholar]
- 74.Menezes AM, Montes de Oca M, Perez-Padilla R, et al. Increased risk of exacerbation and hospitalization in subjects with an overlap phenotype: COPD-asthma. Chest. 2014;145(2):297–304. doi: 10.1378/chest.13-0622. [DOI] [PubMed] [Google Scholar]
- 75.Cottin V, Cordier JF. Combined pulmonary fibrosis and emphysema: an experimental and clinically relevant phenotype. Am J Respir Crit Care Med. 2005;172(12):1605. doi: 10.1164/ajrccm.172.12.1605a. author reply 1605–1606. [DOI] [PubMed] [Google Scholar]
- 76.Jankowich MD, Rounds SI. Combined pulmonary fibrosis and emphysema syndrome: a review. Chest. 2012;141(1):222–231. doi: 10.1378/chest.11-1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Agusti A. Phenotypes and disease characterization in chronic obstructive pulmonary disease: toward the extinction of phenotypes? Ann Am Thorac Soc. 2013;10(Suppl):S125–S130. doi: 10.1513/AnnalsATS.201303-055AW. [DOI] [PubMed] [Google Scholar]
- 78.Burgel PR, Sethi S, Kim V. Chronic obstructive pulmonary disease phenotypes: past, present, and future. Ann Am Thorac Soc. 2015;12(3):289–290. doi: 10.1513/AnnalsATS.201501-011ED. [DOI] [PubMed] [Google Scholar]