Abstract
We present the case of a 55-year-old woman with a presumed ganglion cyst associated with the anterior cruciate ligament (ACL), demonstrated by MRI. The ACL is an uncommon location for ganglion cysts to occur.
Abbreviations: ACL, anterior cruciate ligament; MRI, magnetic resonance imaging; PCL, posterior cruciate ligament
Introduction
Ganglion cysts are common findings around the knee and other joints but association with either the anterior cruciate (ACL) or posterior cruciate ligament (PCL) is considered rare. These cysts are often symptomatic.
Case Report
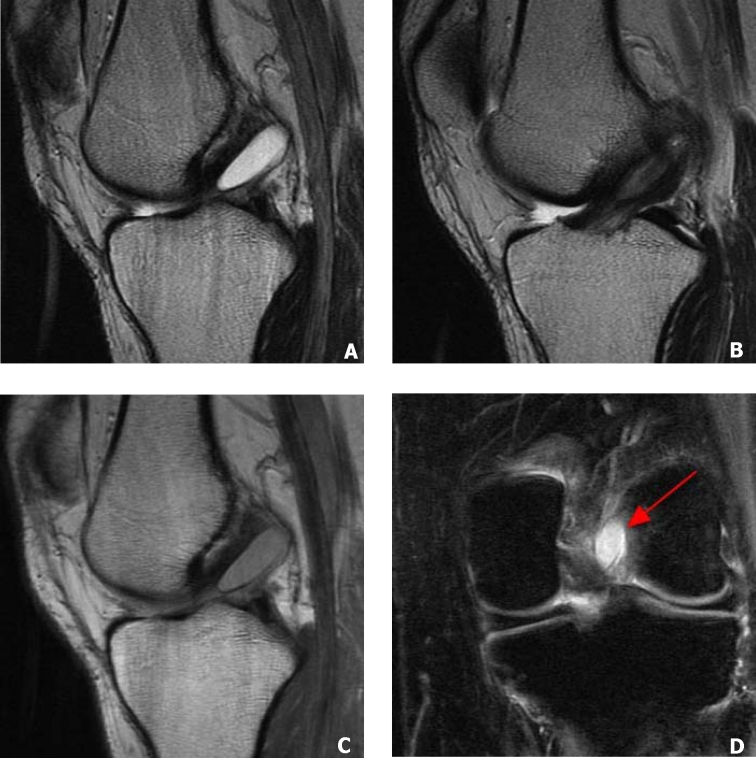
A 55-year-old woman was referred for magnetic resonance imaging (MRI) of her left knee for persistent knee pain spanning several months. She reported no history of trauma, nor any symptoms of infection. The MRI showed a 2cm cystic lesion embedded within the ACL fibers (Fig. 1). The cyst was well-circumscribed and of intermediate signal intensity on proton density and high signal intensity on T2-weighted imaging. The PCL and menisci were normal. There was no effusion nor bone edema. Based on imaging findings the presumptive diagnosis of an ACL ganglion cyst was made. The patient was not surgically treated, nor was the cyst aspirated.
Figure 1.
55-year-old woman with ACL ganglion cyst. A, Sagittal T2-weighted image shows the ganglion cysts as a bright, well-circumscribed oval region paralleling the fibers of the ACL. Incidentally there is a high riding patella. B, Sagittal T2-weighted image, which shows intact ACL fibers and the periphery of the ganglion cyst. C, Sagittal proton density-weighted images shows the cyst to be of intermediate signal intensity. D, Coronal fat saturated proton density-weighted image which shows a portion of the bright cyst (arrow) in the region of the ACL.
Discussion
Ganglion cysts are cystic structures, which contain a yellow viscous fluid surrounded by a thin capsule [8]. They are commonly found around the joints with a particular affinity for the wrist [1, 2, 8]. They are much less common in and around the knee and when found, are most often associated with the joint capsule or meniscus. Additional reported locations include the tendons, muscles, bone and the infrapatellar fat pad [1, 2, 3, 12]. Though rare, there is also an association with both the ACL and PCL [1, 4, 8]. In most cases this is unilateral, although there is at least one reported case of bilateral cruciate ligament cysts, which appears to be an exception [11].
While it is unclear how or why ganglion cysts originate, theories include: displacement of synovium into the surrounding tissue, which may occur during development, herniation of synovium into the surrounding tissues, or degenerative and proliferative changes of pluripotential mesenchymal cells following trauma [1, 4]. A common factor linking the development of cruciate ligament ganglion cysts may be trauma, which can cause the release of hyaluronic acid, a mucinous substance. The hyaluronic acid is thought to dissect through the tissue planes producing capsular ducts and eventually coalescing into a cystic structure. Since the ACL is an extrasynovial structure, irritation or trauma to the synovium covering the ACL may initiate the release of hyaluronic acid and the production of mucin causing the development of a ganglion cyst within or adjacent to the cruciate ligament [6].
Common clinical findings associated with cruciate ligament ganglion cysts include pain, decreased range of motion, swelling and joint effusion. In one study of 15 patients, there was no identifiable association with joint instability. Symptoms suggesting internal derangement of the joint, however, are possible [4, 8]. The most common presenting complaint is pain and it may be associated with a meniscal tear [7, 8]. If the cyst is large enough, it may mechanically obstruct the knee during motion. Cysts anterior to the ACL tend to limit extension, while those posterior to the PCL may limit flexion [8, 10]. Unfortunately, history and physical exam alone are not enough to make the diagnosis. Therefore, MRI is needed to further evaluate the joint and correctly diagnose these lesions.
On MRI, ganglion cysts of the cruciate ligaments appear much like any other cystic structure. On T1-weighted imaging they are hypointense in relation to muscle and on T2-weighted imaging are predominately homogeneously hyperintense, while of intermediate signal intensity on proton-weighted sequences. If there is heterogeneity on the T2 images, this is thought to be caused by hemorrhagic debris within the cyst. The cysts vary from lobulated to fusiform in shape and may contain internal septations or be multiloculated [1, 4, 8]. The most common associated abnormality found with a ganglion cyst of the cruciate ligament is a meniscal tear, and less often a joint effusion [1, 4, 7, 8]. Cysts associated with the ACL tend to be fusiform and oriented parallel to its fibers. Despite the intimate association with the ACL fibers, ganglion cysts are infrequently associated with ACL tears [1, 4, 8].
Curative or symptomatic treatment can be accomplished by either open or arthroscopic resection and drainage. Less invasive treatment can be accomplished by CT-guided aspiration. If the cyst is asymptomatic, conservative treatment should be strongly considered [8, 9].
There are other cystic changes that occur in the knee, the most common being ganglion cysts associated with the meniscus. These are diagnosed when there is a cystic structure contiguous with a meniscal tear. Location should aid in separating these lesions from cruciate ligament ganglion cysts [5, 8]. There are also cysts which occur at the attachments of the cruciate ligaments. These are an uncommon finding and unlike true cruciate ligament ganglion cysts, may be associated with tears of the ligament in a minority of cases [5]. Another differential diagnosis to consider is cystic or mucoid degeneration of the ACL, which may coexist with ganglion cysts of the cruciate ligaments. In mucoid degeneration of the cruciate ligaments the ligament fibers may be poorly defined on T1 and proton density-weighted images, but may be more apparent on T2-weighted imaging. There are no discrete cystic areas in mucoid degeneration, which should help to separate it from the more defined ganglion cyst [13]. A final cystic lesion consideration includes popliteal cyst, but this should be easily differentiated based on location.
In conclusion, we have presented a presumed case of a ganglion cyst of the ACL. The patient did not have any surgical treatment so we do not have a definitive tissue diagnosis, but we feel that the imaging features are unique enough to support our diagnosis. While rare, ganglion cysts associated with the cruciate ligaments should be easily recognized based on location and imaging characteristics. Finally, if symptomatic, these lesions are often amenable to treatment.
Footnotes
Published: July 21, 2009
References
- 1.Recht MP, Applegate G, Kaplan P, Dussault R, Schweitzer M, Dalinka MK, Resnick D. The MR appearance of cruciate ganglion cysts: a report of 16 cases. Skeletal Radiol. 1994 Nov;23(8):597–600. doi: 10.1007/BF02580380. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Andrikoula SI, Vasiliadis HS, Tokis AV, Kosta P, Batistatou A, Georgoulis AD. Intra-articular ganglia of the knee joint associated with the anterior cruciate ligament: a report of 4 cases in 3 patients. Arthroscopy. 2007 Jul;23(7):800.e1–800.e6. doi: 10.1016/j.arthro.2006.05.032. [PubMed] Epub 2006 Nov 27. [DOI] [PubMed] [Google Scholar]
- 3.Yilmaz E, Karakurt L, Ozercan I, Ozdemir H. A ganglion cyst that developed from the infrapatellar fat pad of the knee. Arthroscopy. 2004 Sep;20(7):e65–e68. doi: 10.1016/j.arthro.2004.06.023. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Bui-Mansfield LT, Youngberg RA. Intraarticular ganglia of the knee: prevalence, presentation, etiology, and management. AJR Am J Roentgenol. 1997 Jan;168(1):123–127. doi: 10.2214/ajr.168.1.8976934. [PubMed] [DOI] [PubMed] [Google Scholar]
- 5.McLaren DB, Buckwalter KA, Vahey TN. The prevalence and significance of cyst-like changes at the cruciate ligament attachments in the knee. Skeletal Radiol. 1992;21(6):365–369. doi: 10.1007/BF00241814. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Roeser WM, Tsai E. Ganglion cysts of the anterior cruciate ligament. Arthroscopy. 1994 Oct;10(5):574–575. doi: 10.1016/s0749-8063(05)80017-9. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Parish EN, Dixon P, Cross MJ. Ganglion cysts of the anterior cruciate ligament: a series of 15 cases. Arthroscopy. 2005 Apr;21(4):445–447. doi: 10.1016/j.arthro.2004.12.008. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Huang GS, Lee CH, Chan WP, Taylor JA, Hsueh CJ, Juan CJ, Chen CY, Yu JS. Ganglion cysts of the cruciate ligaments: MR findings with clinical correlation. Acta Radiol. 2002 Jul;43(4):419–424. doi: 10.1080/j.1600-0455.2002.430414.x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Antonacci VP, Foster T, Fenlon H, Harper K, Eustace S. Technical report: CT-guided aspiration of anterior cruciate ligament ganglion cysts. Clin Radiol. 1998 Oct;53(10):771–773. doi: 10.1016/s0009-9260(98)80323-1. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Dinakar B, Khan T, Kumar AC, Kumar A. Ganglion cyst of the anterior cruciate ligament: a case report. J Orthop Surg (Hong Kong) 2005 Aug;13(2):181–185. doi: 10.1177/230949900501300215. [PubMed] [DOI] [PubMed] [Google Scholar]
- 11.Noda M, Kurosaka M, Maeno K, Mizuno K. Case report ganglion cysts of the bilateral cruciate ligaments. Arthroscopy. 1999 Nov-Dec;15(8):867–870. doi: 10.1053/ar.1999.v15.0150862. [PubMed] [DOI] [PubMed] [Google Scholar]
- 12.Jacobson JA, Lenchik L, Ruhoy MK, Schweitzer ME, Resnick D. MR imaging of the infrapatellar fat pad of Hoffa. Radiographics. 1997 May-Jun;17(3):675–691. doi: 10.1148/radiographics.17.3.9153705. [PubMed] [DOI] [PubMed] [Google Scholar]
- 13.Bergin D, Morrison WB, Carrino JA, Nallamshetty SN, Bartolozzi AR. Anterior cruciate ligament ganglia and mucoid degeneration: coexistence and clinical correlation. AJR Am J Roentgenol. 2004 May;182(5):1283–1287. doi: 10.2214/ajr.182.5.1821283. [PubMed] [DOI] [PubMed] [Google Scholar]