Abstract
Context:
Childhood tuberculosis is a major public health problem in developing countries with tubercular meningitis being a serious complication with high mortality and morbidity.
Aim:
To study the clinicopathological as well as radiological profile of childhood tuberculous meningitis (TBM) cases.
Settings and Design:
Prospective, observational study including children <14 years of age with TBM admitted in a tertiary care hospital from Western India.
Subjects and Methods:
TBM was diagnosed based on predefined criteria. Glassgow coma scale (GCS) and intracranial pressure (ICP) was recorded. Staging was done as per British Medical Council Staging System. Mantoux test, chest X-ray, cerebrospinal fluid (CSF) examination, neuroimaging, and other investigations were done to confirm TB.
Statistical Analysis Used:
STATA software (version 9.0) was used for data analysis. Various risk factors were determined using Chi-square tests, and a P< 0.05 was considered significant.
Results:
Forty-seven children were included, of which 11 (24.3%) died. Fever was the most common presenting symptom, and meningismus was the most common sign. Twenty-nine (62%) children presented with Stage III disease. Stage III disease, low GCS, and raised ICP were predictors of mortality. Findings on neuroimaging or CSF examination did not predict mortality.
Conclusions:
Childhood TBM presents with nonspecific clinical features. Stage III disease, low GCS, lack of Bacillus Calmette–Guérin vaccination at birth and raised ICP seem to the most important adverse prognostic factors.
Keywords: Children, developing country, meningitis, mortality, tuberculosis
Introduction
India has one of the highest burdens of tuberculosis (TB) globally, accounting for around 20% of all new TB cases annually.[1] It is estimated that childhood TB constitutes 10–20% of all TB cases in high burden countries,[2] accounting for 8–20% of TB-related deaths.[3] Approximately, 25% of pediatric TB cases are extrapulmonary, with tuberculous meningitis (TBM) being the most severe form. Worldwide, TBM accounts for majority of the deaths due to TB.[1] A study from South Africa (a high burden country) reported TB to be the commonest cause of childhood meningitis.[4] TBM continues to be an important cause of morbidity (especially neurologic handicap) in children from resource-poor countries. Due to suboptimal performance of the diagnostic tests, TBM diagnosis requires vital clinical information coupled with supportive investigations (biochemical, immunological, and radiological).[5] There have been few studies looking at the clinico-patho-radiological spectrum of this disease in children from India,[6] with fewer addressing the outcome predictors.[7,8] This prospective, observational study was designed to address this issue.
Subjects and Methods
Children of 3 months to 14 years of age with suspected TBM admitted to a tertiary care hospital from Western India were included in the study. TBM was suspected based on following features: Fever and/or a cough for ≥2 weeks, neurological symptoms (irritability, refusal to feed, headache, vomiting, altered sensorium, abnormal movements or seizure) with weight loss or poor weight gain. The diagnosis of TBM was based on the clinical case definition by Doerr et al. [Text box 1].[9] Ethical clearance was obtained from the Institute Ethics Committee and a written informed consent was taken from either of the parents/legal guardian before enrollment. TBM cases on treatment, those with underlying chronic illness or malignancy or HIV, and those on immunosuppressive therapy were excluded. Demographic data, immunization, contact with TB, and socioeconomic status were recorded.[10] Detailed clinical examination, anthropometry, and the presence of Bacillus Calmette–Guérin (BCG) scar were recorded.[11] The level of consciousness (modified Glassgow coma scale (GCS)), signs of raised intracranial pressure (ICP) and meningeal irritation was noted. Staging of tubercular meningitis was done as per British Medical Council Staging System [Text box 2].[12]
Text box 1.
Clinical case definition of tuberculous meningitis devised by Doerr et al.

Text box 2.
British Medical Council Staging System for tubercular meningitis

All the recruited children underwent chest X-ray, Mantoux test, and complete hemogram. Additional testing included gastric aspirate for acid-fast Bacilli (AFB), ultrasonography of abdomen and fine needle aspiration cytology from enlarged lymph nodes. A standard tuberculin skin test (5 TU) was used and results read after 72 h (positive: Induration of ≥10 mm; HIV and severe malnutrition: ≥5 mm was considered positive). Cerebrospinal fluid (CSF) analysis was done including the presence of AFB. All the children underwent neuroimaging (plain and contrast enhanced computed tomography or magnetic resonance imaging [MRI]). HIV testing was done where appropriate.
The data were entered into Microsoft excel sheet and analyzed using Stata 9.0 software (STATA Corp, College Station, TX, USA). Descriptive statistics was used along with analysis of risk factors by using Chi-square test or Fisher's test. A P <0.05 was considered statistically significant.
Results
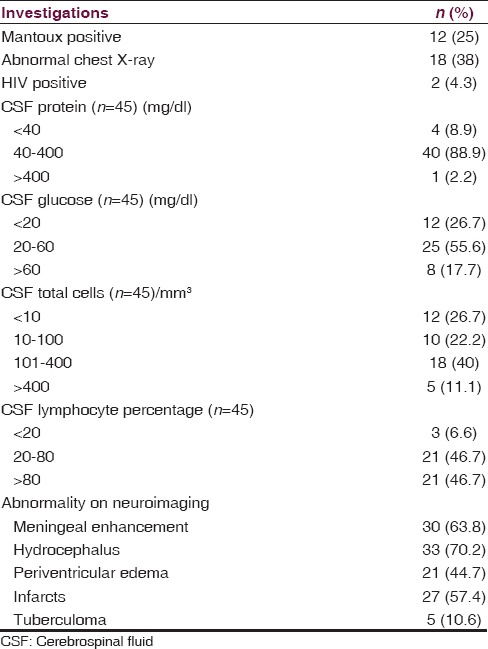
Of 50 TBM cases, 47 met the eligibility criteria and were included. The baseline characteristics and clinical features are presented in Table 1. Majority of children were from lower socioeconomic status (85%) and were malnourished (76.6%). Fever, altered sensorium, and seizure were the most common symptoms. Contact history of TB was positive in 49% cases, 55% of children were BCG vaccinated, Mantoux test was positive in 25% [Table 1]. CSF examination could be done in 45 children (10% had opalescent appearance, no xanthochromia or hemorrhage or cobweb formation was noted). Chest X-ray abnormality was found in 38% [Table 2]. Common abnormalities noted on neuroimaging were: Communicating hydrocephalus (70%), meningeal enhancement (64%), and infarction (45%) [Table 2]. Meningeal enhancement was most commonly observed over the basal cisterns (47%) and cerebral cortex (43%). Infarction was most common in basal ganglion (67%) followed by cortex (41%).
Table 1.
Baseline and clinical characteristics of children with tubercular meningitis

Table 2.
Laboratory and neuroimaging findings in children with tuberculous meningitis
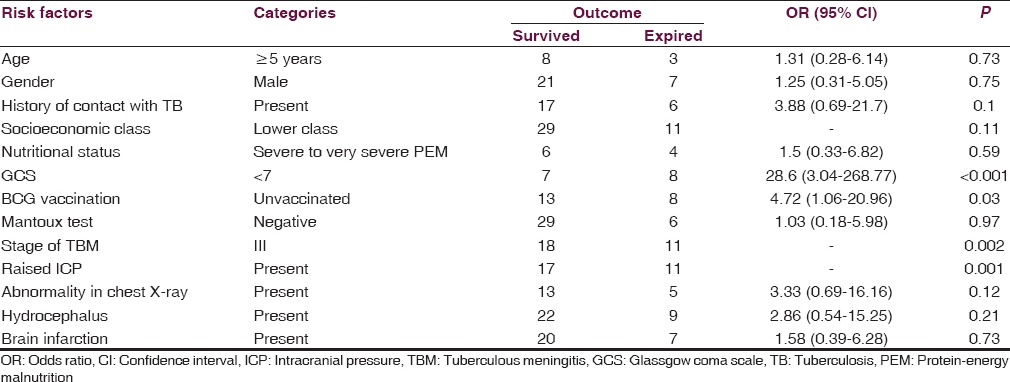
The mortality rate was 23.4% (11 of 47 died). Various risk factors associated with mortality or poor outcome were analyzed. Stage III disease, low GCS, and raised ICP were associated with increased mortality [Table 3], whereas biochemical and cytological parameters did not affect the outcome (data not shown). A significantly increased risk of mortality was found in children who were not vaccinated with BCG at birth.
Table 3.
Factors associated with mortality from tubercular meningitis in children
Discussion
We summarized the clinical, pathological, and radiological features of TBM and investigated characteristics associated with mortality. Children with TBM had nonspecific clinical pictures, boys were commonly affected, Mantoux positivity was in 25%, chest X-ray compatible with TB in 38% cases, and communicating hydrocephalus was the most common neuroimaging finding. Stage III disease, low GCS, and raised ICP were associated with increased mortality.
The male preponderance (1.5:1) observed in the present study was consistent with earlier pediatric studies from India.[6,7] Most common age group affected was <3 years (60%) followed by 3–6 years (16%). Globally, children <5 years of age have been found to be most vulnerable.[13,14,15] Contact with TB could be elicited in about 50% of children in present study, this figure has been reported between 33% and 69% in various studies.[6,14,15] This emphasizes the importance of eliciting contact history and family screening for TB in suspected cases of TBM. Despite being almost universally recommended and potentially highly effective, screening to provide preventive therapy for eligible contacts is still rarely implemented in TB endemic communities.[16]
Though BCG vaccination is included under the universal immunization coverage, only 55% of children were vaccinated in the present study. As BCG vaccination protects against severe froms of TB (e.g., TBM, and disseminated or milliary TB), a lower vaccination coverage could explain a higher prevalence of severe from of TB (e.g., TBM) in the present study.[17] Studies from India and Western countries have clearly documented the effect of BCG vaccine in reducing mortality from TBM.[17,18,19] In a systematic review and metanalysis for treatment outcome of TBM in children, the authors emphasized on the role of BCG vaccination as an invaluable preventive measure for TBM.[19] Our study demonstrated mantoux positivity only at mere 25% in children with TBM. TBM being an extra-pulmonary disease, a low rate of positive mantoux reaction in children with TBM is expected, though the rates vary widely.[6,7,8,14]
Most of the children (62%) in this study were detected at an advanced stage (Stage III). Advanced stage has been found to be the single most important factor associated with poor outcome,[14] and the same has been echoed in our study. Mortality was nil in Stage I or Stage II disease but was 38% in Stage III disease. Cranial nerve palsy has been recognized as an important clinical indicator in differentiating TBM from pyogenic meningitis.[20] In this study, 13% children present with cranial nerve palsy. Around 54% of children having GCS <7 died, and GCS was found to be one of the predictors of mortality in the present study. This has been reported in previous Indian studies.[8] Around 39% of children with raised ICP died, and this was found to be another predictors of mortality. Previous studies also report similar observation.[8]
Abnormal chest X-ray was observed in 38% of patients in this study. A previous study found this figure as 44%.[21] None of the radiological findings (chest X-ray, computed tomography scan, or MRI brain) predicted the mortality. While looking at the CSF findings, patients dying of TBM had higher mean CSF protein values and also CSF lymphocytic pleocytosis compared to those who survived.
The overall mortality in the present study was 23.4%. A previous systematic review reported this figure as 19.3%.[22] However, in 10 years comparative retrospective analysis, one study reported this figure as 8% in children with TBM.[23]
The strengths of the present study are prospective enrollment of children and careful documentation using a standardized predesigned data collection form. The case definition of TBM was also predefined, and the same was also used in a previous study from India, thus making it easier to compare the results. The limitations are: Being a single center study conducted at a tertiary care referral hospital, referral bias cannot be ruled out; TB culture and nucleic acid amplification tests (Genexpert) were not conducted on the CSF specimen; treatment outcome and follow-up of the patients to look for neurological sequelae could not be done.
The incidence of TBM indicates the annual risk of infection, and a robust surveillance system for documenting the occurrence of TBM in young children can improve estimates and monitoring of the TB burden and TB-related deaths in children.[24] Newer and easier scoring systems need to be devised in the lights of ever increasing knowledge for better prediction of outcome of this dreaded disease.[25] Furthermore, the survivors of tubercular meningitis are at a risk of long-term neurological sequelae ranging from residual paresis to subtle neurological deficit in the form of poor scholastic performance or even behavioral abnormalities. This mandates a close and regular follow-up of these children for early intervention.
Conclusion
Tubercular meningitis continues to be associated with high rate mortality in children of countries with high burden of TB. Even with the advancement of scientific knowledge and technologies, including new techniques of laboratory and imaging diagnostic aid, very little prediction can be made regarding the prognosis of children with this dreaded disease. Our study highlighted few important predictors associated with mortality in this age group coupled with a reemphasis on need for early diagnosis, though the challenge remains to devise composite index systems in predicting outcome in TBM in future years.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization (WHO) Global Tuberculosis Report 2013. Geneva: WHO; 2013. [Last accessed on 2015 Dec 15]. Available from: http://www.apps.who.int/iris/bitstream/10665/91355/1/9789241564656_eng.pdf . [Google Scholar]
- 2.Marais BJ, Hesseling AC, Gie RP, Schaaf HS, Beyers N. The burden of childhood tuberculosis and the accuracy of community-based surveillance data. Int J Tuberc Lung Dis. 2006;10:259–63. [PubMed] [Google Scholar]
- 3.Jain SK, Ordonez A, Kinikar A, Gupte N, Thakar M, Mave V, et al. Pediatric tuberculosis in young children in India: A prospective study. Biomed Res Int. 2013;2013:783698. doi: 10.1155/2013/783698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wolzak NK, Cooke ML, Orth H, van Toorn R. The changing profile of pediatric meningitis at a referral centre in Cape Town, South Africa. J Trop Pediatr. 2012;58:491–5. doi: 10.1093/tropej/fms031. [DOI] [PubMed] [Google Scholar]
- 5.van Toorn R, Solomons R. Update on the diagnosis and management of tuberculous meningitis in children. Semin Pediatr Neurol. 2014;21:12–8. doi: 10.1016/j.spen.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 6.Thilothammal N, Krishnamurthy PV, Banu K, Ratnam SR. Tuberculous meningitis in children – Clinical profile, mortality and morbidity of bacteriologically confirmed cases. Indian Pediatr. 1995;32:641–7. [PubMed] [Google Scholar]
- 7.Ramzan A, Nayil K, Asimi R, Wani A, Makhdoomi R, Jain A. Childhood tubercular meningitis: An institutional experience and analysis of predictors of outcome. Pediatr Neurol. 2013;48:30–5. doi: 10.1016/j.pediatrneurol.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Karande S, Gupta V, Kulkarni M, Joshi A. Prognostic clinical variables in childhood tuberculous meningitis: An experience from Mumbai, India. Neurol India. 2005;53:191–5. doi: 10.4103/0028-3886.16407. [DOI] [PubMed] [Google Scholar]
- 9.Doerr CA, Starke JR, Ong LT. Clinical and public health aspects of tuberculous meningitis in children. J Pediatr. 1995;127:27–33. doi: 10.1016/s0022-3476(95)70252-0. [DOI] [PubMed] [Google Scholar]
- 10.Kumar N, Shekhar C, Kumar P, Kundu AS. Kuppuswamy's socioeconomic status scale-updating for 2007. Indian J Pediatr. 2007;74:1131–2. [PubMed] [Google Scholar]
- 11.Khadilkar VV, Khadilkar AV, Choudhury P, Agarwal KN, Ugra D, Shah NK. IAP growth monitoring guidelines for children from birth to 18 years. Indian Pediatr. 2007;44:187–97. [PubMed] [Google Scholar]
- 12.British Medical Research Council. Streptomycin treatment of tuberculous meningitis. Br Med J. 1948;1:582–97. [Google Scholar]
- 13.Humphries MJ, Teoh R, Lau J, Gabriel M. Factors of prognostic significance in Chinese children with tuberculous meningitis. Tubercle. 1990;71:161–8. doi: 10.1016/0041-3879(90)90069-k. [DOI] [PubMed] [Google Scholar]
- 14.van Well GT, Paes BF, Terwee CB, Springer P, Roord JJ, Donald PR, et al. Twenty years of pediatric tuberculous meningitis: A retrospective cohort study in the western cape of South Africa. Pediatrics. 2009;123:e1–8. doi: 10.1542/peds.2008-1353. [DOI] [PubMed] [Google Scholar]
- 15.Lee LV. Neurotuberculosis among Filipino children: An 11 years experience at the Philippine Children's Medical Center. Brain Dev. 2000;22:469–74. doi: 10.1016/s0387-7604(00)00190-x. [DOI] [PubMed] [Google Scholar]
- 16.Hill PC, Rutherford ME, Audas R, van Crevel R, Graham SM. Closing the policy-practice gap in the management of child contacts of tuberculosis cases in developing countries. PLoS Med. 2011;8:e1001105. doi: 10.1371/journal.pmed.1001105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kelekçi S, Karabel M, Karabel D, Hamidi C, Hosoglu S, Gürkan MF, et al. Bacillus Calmette-Guérin is a preventive factor in mortality of childhood tuberculous meningitis. Int J Infect Dis. 2014;21:1–4. doi: 10.1016/j.ijid.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Kumar R, Dwivedi A, Kumar P, Kohli N. Tuberculous meningitis in BCG vaccinated and unvaccinated children. J Neurol Neurosurg Psychiatry. 2005;76:1550–4. doi: 10.1136/jnnp.2005.065201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chiang SS, Khan FA, Milstein MB, Tolman AW, Benedetti A, Starke JR, et al. Treatment outcomes of childhood tuberculous meningitis: A systematic review and meta-analysis. Lancet Infect Dis. 2014;14:947–57. doi: 10.1016/S1473-3099(14)70852-7. [DOI] [PubMed] [Google Scholar]
- 20.Moghtaderi A, Alavi-Naini R, Rashki S. Cranial nerve palsy as a factor to differentiate tuberculous meningitis from acute bacterial meningitis. Acta Med Iran. 2013;51:113–8. [PubMed] [Google Scholar]
- 21.Solomons RS, Goussard P, Visser DH, Marais BJ, Gie RP, Schoeman JF, et al. Chest radiograph findings in children with tuberculous meningitis. Int J Tuberc Lung Dis. 2015;19:200–4. doi: 10.5588/ijtld.14.0634. [DOI] [PubMed] [Google Scholar]
- 22.Graham SM, Donald PR. Death and disability: The outcomes of tuberculous meningitis. Lancet Infect Dis. 2014;14:902–4. doi: 10.1016/S1473-3099(14)70872-2. [DOI] [PubMed] [Google Scholar]
- 23.Miftode EG, Dorneanu OS, Leca DA, Juganariu G, Teodor A, Hurmuzache M, et al. Tuberculous meningitis in children and adults: A 10-year retrospective comparative analysis. PLoS One. 2015;10:e0133477. doi: 10.1371/journal.pone.0133477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Styblo K, Sutherland I. The epidemiology of tuberculosis in children. Bull Int Union Tuberc. 1982;57:133–9. [PubMed] [Google Scholar]
- 25.Alarcón F, Moreira J, Rivera J, Salinas R, Dueñas G, Van den Ende J. Tuberculous meningitis: Do modern diagnostic tools offer better prognosis prediction? Indian J Tuberc. 2013;60:5–14. [PubMed] [Google Scholar]


