Abstract
Schizophrenia is a severe mental disorder. Cognitive deficits are one of the core features of schizophrenia. Multiple domains of cognition (executive function, attention/vigilance, working memory, verbal fluency, visuospatial skills, processing speed, and social cognition) are affected in patients with schizophrenia. Deficits in cognition led to impairment in the real world functioning. Identifying the cognitive deficits and early intervention is required for better functional outcome. This review focuses on conceptual understanding of cognition with its neurobiological correlates in schizophrenia and its different clinical implications.
Keywords: Cognition, cognitive deficits, neurobiological correlates, schizophrenia
Introduction
Schizophrenia is a severe mental disorder with complex and multifactorial etiology. The prevalence of schizophrenia is about 1% worldwide. It is the most common psychotic disorder worldwide with point prevalence of about 4.6/1000 population.[1]
The symptoms of schizophrenia can be broadly categorized into – positive symptoms, negative symptoms, affective symptoms, cognitive symptoms, and aggressive symptoms. Cognitive impairment in schizophrenia causes impairment in real-world functioning and significantly impairs the quality of life.[2] Schizophrenia causes dysfunction of the prefrontal cortex by several mechanisms such as perfusion defect, defective metabolism, and defective synaptic pruning, which is responsible for the higher cognitive functions such as planning, regulation, and execution of goal-directed activities.[2]
Evolution of Understandings About Cognition in Schizophrenia
Previously, cognitive symptoms in schizophrenia are considered to be the major symptoms of schizophrenia, which led to the perception that probably schizophrenia is like premature onset dementia; hence, Benedict Morel and Emil Kraepelin acknowledged this disorder as “demence precoce” and “dementia praecox,” respectively. Subsequently (in the early part of the 19th century), this perception was rejected and schizophrenia is presented as a distinct mental disorder with quite different pathophysiology and psychopathology. Whatever, cognitive symptoms observed in patients with schizophrenia were considered to be secondary to positive or negative symptoms. However, very recently in the last two decades, it was understood that cognitive deficits in schizophrenia are primary and core deficits.[3,4,5] The reasons for which the cognitive deficits in schizophrenia were given special attention as a distinct domain of symptoms are, due to a characteristic pattern of the cognitive symptoms in schizophrenia, stable deficits in cognition persisting throughout the course of illness and persistence of cognitive deficits independent of remission of other symptoms of schizophrenia.[5]
It is also recently understood that the socio-occupational decline in patients with schizophrenia was mostly due to core cognitive deficits.[3,4] Even during the phases of symptomatic remission, these cognitive deficits persist, which can be explained by the persistent brain changes in these patients.[4] Structural brain changes in schizophrenia are frequently seen in the frontotemporal region, which attributes to the impairments in neuropsychological functions.[6]
The impairment of cognition is not only limited to patients suffering from schizophrenia; research evidence are also suggestive of cognitive dysfunction in otherwise normal individuals with high risk of psychosis, first-degree relatives of patients with schizophrenia.[7,8,9] Cognitive deficits are found to exist in patients with schizophrenia as early as before the onset of illness, early phase of illness and remain stable over time in patients not receiving any specific intervention.[9,10] Few recent studies had revealed that cognitive deficits in schizophrenia depend on the age of onset; earlier is the onset, more will be the deficits.[11,12,13] Duration of schizophrenia has little impact on the already existing cognitive deficits.[11,12,13] The deficits in cognition persist even during the phase of remission.[9]
Understanding Cognition and Cognitive Deficits in Schizophrenia
Cognition is an important brain function. It is the sum total of mental processes that enables us to acquire knowledge and keeps us aware of our surroundings and thus enable us to arrive at appropriate judgments. It is cognition that determines skills such as problem-solving, decision-making, and creativity. Some major cognitive domains are summarized in Figure 1.
Figure 1.
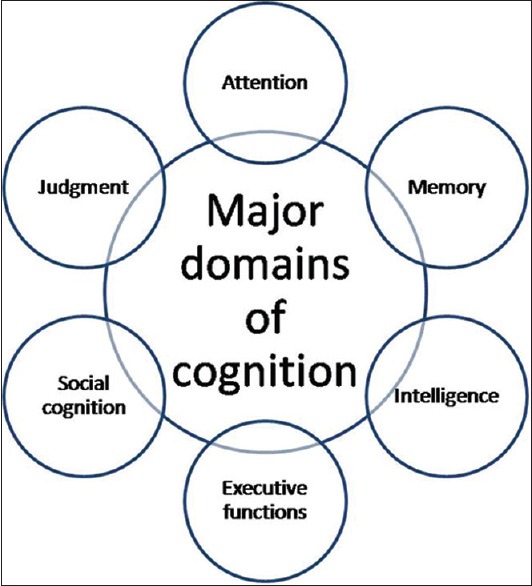
Major domains of cognition
Cognition helps an individual for functioning in the real world. Attention, concentration, memory, intelligence, judgment, executive functions, and social cognition are some major cognitive functions. These cognitive processes help in delivering various functions. Processing speed is the fastness to deliver these functions, which is dependent on the integrity of neuronal network as well as white matters. Impairment in cognitive processing results in difficulty in delivering different tasks leading to disability.
Cognitive impairments are one type of core symptoms in schizophrenia. Patients with chronic schizophrenia are impaired in a wide range of cognitive functions which include verbal memory, working memory, motor speed, attention, executive functions, and verbal fluency.[14,15,16,17]
Nearly four out of every five individuals suffering from schizophrenia exhibit some sort of cognitive deficits which hamper the normal functioning of the individuals.[18] The cognitive deficits in schizophrenia can be attributed to the under-activity of N-methyl-d-aspartate receptors.[19] Nair et al., in a recent meta-analysis, established that insight for psychosis has strong correlation with the important cognitive parameters such as executive function, memory, and intelligence as well as total cognition.[20] Cognitive dysfunction in schizophrenia is believed to be an endophenotype which manifests across the schizophrenia spectrum disorders.[21] Most dysfunctional cognitive functions attribute to the disrupted cortico-striato-thalamo-cortical network.[21]
Attention and vigilance
Attention refers to processes of how an individual becomes receptive for external or internal stimuli.[22] The critical attributes of attention are focus, selectivity, exclusiveness, and vigilance. Attention requires rapid encoding of information.
In schizophrenia, attention impairment is a core cognitive deficit.[23] Perhaps deficient rapid encoding of information is responsible for attention impairments in schizophrenia.[24]
Learning and memory
Memory is the outcome of learning. The human memory is a complex system by which an individual registers, stores, retains, and retrieves information.[22]
In schizophrenia, different domains of learning and memory are affected. Studies suggest that working memory, visuospatial memory, and verbal memory are common to be affected in schizophrenia.[3] In schizophrenia, there also occurs impairment of emotional modulation of memory and attention.[25] They initially take longer time to encode information than do normal people; however, they tend to perform better with repeated exposure.[26,27,28] They do not use effective learning strategies, such as semantic clustering, not even when told to cluster the information. However, they tend to show intact recognition memory[29] thus, suggesting more impairment in explicit compared with implicit memory.[30]
Working memory
Working memory refers to a multicomponent cognitive system that is serving to hold a limited amount of information “online” for a short period of time and to simultaneously manipulate the information so that it is available for further cognitive processing, or to guide response selection relevant for a specific context.[31] The working memory system comprises the core executive domain with two short-term storage systems of information, visuospatial network for visual information, and the articulatory loop for phonological information.[32]
It has been argued that impaired working memory is the core cognitive deficit in schizophrenia, associating with the clinical picture and the functional consequences of the disorder.[33,34] Both verbal and nonverbal working memories are dysfunctional in schizophrenia.[29,35,36] Working memory plays an important role during the encoding process. Seidman et al. found that during a verbal learning task in which the words can be semantically clustered, the differences between schizophrenia patients and healthy controls were eliminated when the results were controlled for scores in a working memory task.[37] It is likely that abnormalities in working and strategic memory contribute substantially to the verbal encoding deficit in schizophrenia as well as to other cognitive functions.
Executive function
Executive functions involve the use of information rather than the fundamental processing of information and refer to the processes by which an individual realizes purposeful behavior.[22] The unique skills used for expansion, modulation, and implementation of goal-directed activities are the executive functions of the brain, which is the amalgamation of several complex mental abilities.
Patients with schizophrenia have deficits in executive function and theory of mind.[38] The deficits of executive function and theory of mind seem to be independent of each other.[38] Dysfunction of the executive function is not only limited to patients of schizophrenia but also reported in their healthy first-degree relatives.[39,40] Executive dysfunction in schizophrenia leads to impairment in maintenance and shifting of the responses according to situation and dysfunctional goal-directed activity.[23,41,42]
Information processing and processing speed
The term information processing is used to describe the process of taking information and encoding it in such a way that it can be understood and recalled when appropriately cued. Memory and perception are stages in information processing.[43] Processing speed is the rapidity by which information processing occurs.
Many neurocognitive tests require subjects to process information rapidly and can be compromised by impairments in processing speed. Standard examples of this type of task are the coding tasks, which have been found to demonstrate the most severe deficits in schizophrenia.[44]
Problem-solving
Problem-solving is the complex mental processes of using previously learned information to identify solutions to new problems. Patients with schizophrenia, who are impaired on measures of executive functions, have difficulty adapting to the rapidly changing world around them.
Poor problem-solving ability in schizophrenia can be a core deficit or may be secondary to deficit in other major areas of cognition such as task initiation, attention, concentration, and working memory; core deficits in executive functions such as difficulty in shifting task (due to impaired ability to think alternatively), repetition of the errors (perseveration), and slower rate of processing speed may prolong the problem.
Social cognition
Social cognition refers to “the ways social events are interpreted, analyzed and mentally represented.” It also provides an information-processing framework for understanding how the construal of self and others affects social discourse and psychological life.
In studies, social cognitions such as recognition and discrimination of faces and emotions are found to be impaired in patients with schizophrenia, which compromises the socio-occupational life significantly.[45,46] McCleery et al., in their study, found that there was no difference in the severity, pattern, and involvement of different cognitive domains in patients with the first-episode schizophrenia and chronic schizophrenia; however, social cognition and working memory were relatively preserved in the early phase of illness.[47] Compromised cognitive function in schizophrenia results in wrong self-appraisal of empathetic abilities.[48]
Recently, activity of mirror neurons in patients with schizophrenia has been focussed in several studies and it is believed that mirror neurons have a unique role in social cognition though robust evidences are lacking.[49] In schizophrenia, there is dysfunction of the mirror neuron system which may attribute to deficits in social cognition.[49] Impaired cortical inhibition may also have role in impairment of social cognition in patients with schizophrenia.[50]
In several studies, it was found that patients with schizophrenia had gross decline in general intellectual ability on the neuropsychological assessments.[17,23,51,52,53,54] Deterioration of intellectual functioning is not only attributable to decline in performance IQ or verbal IQ, but rather more related to deficits in specific cognitive domains such as attention, processing speed, and working memory.[23,51]
Cognition Assessment Tools in Schizophrenia
Cognitive deficits in patients with schizophrenia cause significant impairment in real world functioning. Identifying cognitive deficits will help in planning for specific therapeutic intervention as well as rehabilitation. Early identification of cognitive deficits helps in early intervention and better outcome.
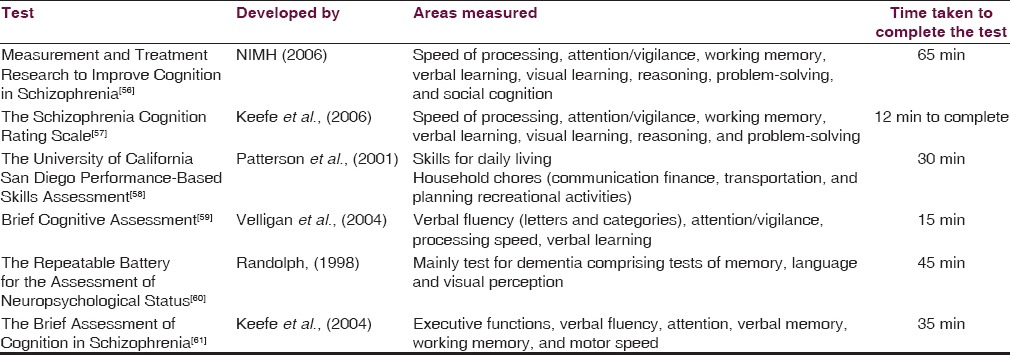
Several tools have been developed to assess cognition comprising of different cognitive tasks employed, especially for patients with schizophrenia. Numerous batteries have been developed which are comprehensive and give detailed description of the multiple domains of cognition. However, such batteries are difficult to be applied in many settings because of the time constraints. The kind of test to be used depends on the research question to be answered. For example, if the research questions want to assess the effectiveness of an intervention, then a detailed evaluation needs to be done while if it involves assessing a particular domain, then a brief battery will do.[55] The details of some of the cognitive test batteries are given below in Table 1.
Table 1.
Summary of important cognitive test batteries
There are several computerized batteries such as the Cambridge Neuropsychological Test Automated Battery,[62] the Cognitive Drug Research Cognitive Assessment System,[63] and the CogTest Battery[64] which have been applied to patients suffering with schizophrenia, but they have certain operational difficulties such as cost, portability, regular software, and hardware version change.
Filling the Gaps
Many strategies have been attempted to improve cognition in patients with schizophrenia. Earlier studies revealed that antipsychotics improve cognition in patients with schizophrenia.[65] Inada et al. in their study on animal models found that antipsychotics stabilize the processing of emotion and cognition.[65] The improvement of cognition due to antipsychotic treatment may be due to improvement of positive symptoms, affective symptoms, or few negative symptoms and unlikely due to improvement of core cognitive deficits.[3] Keedy et al. (2015), in a recent study, concluded that antipsychotic medications improve the functioning of dorsal cortical attention network.[66]
Large studies found that antipsychotics have little role in cognitive deficits due to schizophrenia.[67,68,69] and supplementation of cholinergic, antiglutaminergic, and serotonergic agents may have some role in cognitive enhancement.[69] As per the recent understanding, atypical antipsychotics are not different from typical antipsychotics; so far, the cognitive improvement in schizophrenia is concerned.[70] The above findings suggest that antipsychotic treatment may bring some sort of cognitive improvement indirectly by controlling the positive symptoms, affective symptoms and to some extent the negative symptoms; however, the possibility of improvement in core cognitive deficits are unsatisfactory.[70] Probably some more innovative approach is required to fill this gap.
Several nonpharmacological strategies such as cognitive remediation, exercise, and social skill training are now being used for the management of cognitive deficits in such patients. Cognitive remediation therapy is a highly effective modality of intervention which improves the cognitive performance and social functioning.[71,72] This intervention modality can also be effectively used in early-onset schizophrenia in adolescents.[72]
Currently available medications used for the treatment of schizophrenia are unable to address the cognitive deficits.[19] Recent evidence suggest that adenosine and its receptors have role in neuromodulation and brain homeostasis which has a significant role in neuroprotection and cognitive processing.[73] Drugs acting through adenosine receptors likely to influence the cognitive performance and have a great scope for enhancing cognition and neuroprotection in schizophrenia and other disorders such as Alzheimer's disease, Parkinson's disease, and Huntington's disease where cognition is commonly effected.[73] Other agents, which promote neurogenesis and neuroprotection (e.g. anti-inflammatory agents, antioxidants, etc.,) are also likely to offer procognitive effect.[74,75] Research evidence are also in favor of galantamine and memantine for the treatment of cognitive deficits in schizophrenia.[19]
Kalache et al. (2015), in their study, attempted to explore the correlation of cognitive impairment in schizophrenia with functional outcomes across lifespan and found that communication skills, comprehension and planning of recreational activities skills, financial skills, transportation skills, and household management skills depend upon the intactness of cognitive functioning.[76] Hence, improvement of cognitive functioning in schizophrenia is likely to cause improvement in these life skills across life time.[76]
Conclusion
Targeting the cognitive deficits in the early phase of psychosis is likely to be more effective in preventing disability.[4] Insight about cognitive deficits has a lot of clinical implications. Patients with insight to cognitive deficits may have better treatment adherence and are more amenable for cognitive rehabilitation.[77] Cognitive domains have specific neurobiological correlates. Involvement of specific brain regions attributes to the unique pattern of cognitive deficit in patients with schizophrenia. Though there is significant overlapping of the brain areas involved in other psychiatric disorders (e.g. mood disorder, dementia), which also produces overlapping in the mold of cognitive deficits.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bhugra D. The global prevalence of schizophrenia. PLoS Med. 2005;2:e151. doi: 10.1371/journal.pmed.0020151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stip E. Cognition, schizophrenia and the effect of antipsychotics. Encephale. 2006;32((3 Pt 1)):341–50. doi: 10.1016/s0013-7006(06)76162-0. [DOI] [PubMed] [Google Scholar]
- 3.Peuskens J, Demily C, Thibaut F. Treatment of cognitive dysfunction in schizophrenia. Clin Ther. 2005;27(Suppl A):S25–37. doi: 10.1016/j.clinthera.2005.07.015. [DOI] [PubMed] [Google Scholar]
- 4.Nuechterlein KH, Ventura J, Subotnik KL, Bartzokis G. The early longitudinal course of cognitive deficits in schizophrenia. J Clin Psychiatry. 2014;75(Suppl 2):25–9. doi: 10.4088/JCP.13065.su1.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gold JM. Cognitive deficits as treatment targets in schizophrenia. Schizophr Res. 2004;72:21–8. doi: 10.1016/j.schres.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 6.Nickl-Jockschat T, Schneider F, Pagel AD, Laird AR, Fox PT, Eickhoff SB. Progressive pathology is functionally linked to the domains of language and emotion: Meta-analysis of brain structure changes in schizophrenia patients. Eur Arch Psychiatry Clin Neurosci. 2011;261(Suppl 2):S166–71. doi: 10.1007/s00406-011-0249-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bora E, Lin A, Wood SJ, Yung AR, McGorry PD, Pantelis C. Cognitive deficits in youth with familial and clinical high risk to psychosis: A systematic review and meta-analysis. Acta Psychiatr Scand. 2014;130:1–15. doi: 10.1111/acps.12261. [DOI] [PubMed] [Google Scholar]
- 8.Üçok A, Direk N, Koyuncu A, Keskin-Ergen Y, Yüksel Ç, Güler J, et al. Cognitive deficits in clinical and familial high risk groups for psychosis are common as in first episode schizophrenia. Schizophr Res. 2013;151:265–9. doi: 10.1016/j.schres.2013.10.030. [DOI] [PubMed] [Google Scholar]
- 9.Ventura J, Wood RC, Hellemann GS. Symptom domains and neurocognitive functioning can help differentiate social cognitive processes in schizophrenia: A meta-analysis. Schizophr Bull. 2013;39:102–11. doi: 10.1093/schbul/sbr067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harvey PD. What is the evidence for changes in cognition and functioning over the lifespan in patients with schizophrenia? J Clin Psychiatry. 2014;75(Suppl 2):34–8. doi: 10.4088/JCP.13065su1.08. [DOI] [PubMed] [Google Scholar]
- 11.Fioravanti M, Bianchi V, Cinti ME. Cognitive deficits in schizophrenia: An updated metanalysis of the scientific evidence. BMC Psychiatry. 2012;12:64. doi: 10.1186/1471-244X-12-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rajji TK, Mulsant BH. Nature and course of cognitive function in late-life schizophrenia: A systematic review. Schizophr Res. 2008;102:122–40. doi: 10.1016/j.schres.2008.03.015. [DOI] [PubMed] [Google Scholar]
- 13.Mesholam-Gately RI, Giuliano AJ, Goff KP, Faraone SV, Seidman LJ. Neurocognition in first-episode schizophrenia: A meta-analytic review. Neuropsychology. 2009;23:315–36. doi: 10.1037/a0014708. [DOI] [PubMed] [Google Scholar]
- 14.Saykin AJ, Gur RC, Gur RE, Mozley PD, Mozley LH, Resnick SM, et al. Neuropsychological function in schizophrenia. Selective impairment in memory and learning. Arch Gen Psychiatry. 1991;48:618–24. doi: 10.1001/archpsyc.1991.01810310036007. [DOI] [PubMed] [Google Scholar]
- 15.Harvey PD, Keefe RS. Cognitive impairment in schizophrenia and implications atypical neuroleptics treatment. CNS Spectr. 1997;2:1–11. [Google Scholar]
- 16.Keefe RS. The contribution of neuropsychology to psychiatry. Am J Psychiatry. 1995;152:6–15. doi: 10.1176/ajp.152.1.6. [DOI] [PubMed] [Google Scholar]
- 17.Heinrichs RW, Zakzanis KK. Neurocognitive deficit in schizophrenia: A quantitative review of the evidence. Neuropsychology. 1998;12:426–45. doi: 10.1037//0894-4105.12.3.426. [DOI] [PubMed] [Google Scholar]
- 18.Raffard S, Gely-Nargeot MC, Capdevielle D, Bayard S, Boulenger JP. Learning potential and cognitive remediation in schizophrenia. Encephale. 2009;35:353–60. doi: 10.1016/j.encep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 19.Koola MM, Buchanan RW, Pillai A, Aitchison KJ, Weinberger DR, Aaronson ST, et al. Potential role of the combination of galantamine and memantine to improve cognition in schizophrenia. Schizophr Res. 2014;157:84–9. doi: 10.1016/j.schres.2014.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nair A, Palmer EC, Aleman A, David AS. Relationship between cognition, clinical and cognitive insight in psychotic disorders: A review and meta-analysis. Schizophr Res. 2014;152:191–200. doi: 10.1016/j.schres.2013.11.033. [DOI] [PubMed] [Google Scholar]
- 21.Zaytseva Y, Korsakova N, Agius M, Gurovich I. Neurocognitive functioning in schizophrenia and during the early phases of psychosis: Targeting cognitive remediation interventions. Biomed Res Int. 2013;2013:819587. doi: 10.1155/2013/819587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lezak MD, Howieson DB, Loring DW. Neuropsychological Assessment. 4th ed. New York: Oxford University Press; 2004. [Google Scholar]
- 23.Reichenberg A. The assessment of neuropsychological functioning in schizophrenia. Dialogues Clin Neurosci. 2010;12:383–92. doi: 10.31887/DCNS.2010.12.3/areichenberg. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arango C, Calcedo Barba A, González-Salvador, Calcedo Ordóñez A. Violence in inpatients with schizophrenia: A prospective study. Schizophr Bull. 1999;25:493–503. doi: 10.1093/oxfordjournals.schbul.a033396. [DOI] [PubMed] [Google Scholar]
- 25.Walsh-Messinger J, Ramirez PM, Wong P, Antonius D, Aujero N, McMahon K, et al. Impairment in emotional modulation of attention and memory in schizophrenia. Schizophr Res. 2014;157:63–9. doi: 10.1016/j.schres.2014.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Elvevåg B, Weinberger DR, Suter JC, Goldberg TE. Continuous performance test and schizophrenia: A test of stimulus-response compatibility, working memory, response readiness, or none of the above? Am J Psychiatry. 2000;157:772–80. doi: 10.1176/appi.ajp.157.5.772. [DOI] [PubMed] [Google Scholar]
- 27.Chen WJ, Hsiao CK, Hsiao LL, Hwu HG. Performance of the continuous performance test among community samples. Schizophr Bull. 1998;24:163–74. doi: 10.1093/oxfordjournals.schbul.a033308. [DOI] [PubMed] [Google Scholar]
- 28.Volz H, Gaser C, Häger F, Rzanny R, Pönisch J, Mentzel H, et al. Decreased frontal activation in schizophrenics during stimulation with the continuous performance test – A functional magnetic resonance imaging study. Eur Psychiatry. 1999;14:17–24. doi: 10.1016/s0924-9338(99)80711-1. [DOI] [PubMed] [Google Scholar]
- 29.Conklin HM, Curtis CE, Katsanis J, Iacono WG. Verbal working memory impairment in schizophrenia patients and their first-degree relatives: Evidence from the digit span task. Am J Psychiatry. 2000;157:275–7. doi: 10.1176/appi.ajp.157.2.275. [DOI] [PubMed] [Google Scholar]
- 30.Sponheim SR, Steele VR, McGuire KA. Verbal memory processes in schizophrenia patients and biological relatives of schizophrenia patients: Intact implicit memory, impaired explicit recollection. Schizophr Res. 2004;71:339–48. doi: 10.1016/j.schres.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 31.Baddeley A. Working memory. Science. 1992;255:556–9. doi: 10.1126/science.1736359. [DOI] [PubMed] [Google Scholar]
- 32.Baddeley A. The fractionation of working memory. Proc Natl Acad Sci U S A. 1996;93:13468–72. doi: 10.1073/pnas.93.24.13468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goldman-Rakic PS, Selemon LD. Functional and anatomical aspects of prefrontal pathology in schizophrenia. Schizophr Bull. 1997;23:437–58. doi: 10.1093/schbul/23.3.437. [DOI] [PubMed] [Google Scholar]
- 34.Goldman-Rakic PS. The physiological approach: Functional architecture of working memory and disordered cognition in schizophrenia. Biol Psychiatry. 1999;46:650–61. doi: 10.1016/s0006-3223(99)00130-4. [DOI] [PubMed] [Google Scholar]
- 35.Okada A. Deficits of spatial working memory in chronic schizophrenia. Schizophr Res. 2002;53:75–82. doi: 10.1016/s0920-9964(01)00176-1. [DOI] [PubMed] [Google Scholar]
- 36.Park S, Holzman PS. Schizophrenics show spatial working memory deficits. Arch Gen Psychiatry. 1992;49:975–82. doi: 10.1001/archpsyc.1992.01820120063009. [DOI] [PubMed] [Google Scholar]
- 37.Seidman LJ, Stone WS, Jones R, Harrison RH, Mirsky AF. Comparative effects of schizophrenia and temporal lobe epilepsy on memory. J Int Neuropsychol Soc. 1998;4:342–52. [PubMed] [Google Scholar]
- 38.Gavilán JM, García-Albea JE. Executive dysfunction in schizophrenia and its association with mentalizing abilities. Rev Psiquiatr Salud Ment. 2015;8:119–29. doi: 10.1016/j.rpsm.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 39.Snitz BE, Macdonald AW, 3rd, Carter CS. Cognitive deficits in unaffected first-degree relatives of schizophrenia patients: A meta-analytic review of putative endophenotypes. Schizophr Bull. 2006;32:179–94. doi: 10.1093/schbul/sbi048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Szöke A, Schürhoff F, Mathieu F, Meary A, Ionescu S, Leboyer M. Tests of executive functions in first-degree relatives of schizophrenic patients: A meta-analysis. Psychol Med. 2005;35:771–82. doi: 10.1017/s0033291704003460. [DOI] [PubMed] [Google Scholar]
- 41.Shallice T, Burgess P. The domain of supervisory processes and temporal organization of behaviour. In: Roberts AC, Robbins TW, Weiskrantz L, editors. The Prefrontal Cortex Executive and Cognitive Functions. New York: Oxford University Press; 1998. pp. 2–35. [Google Scholar]
- 42.Palmer BW, Heaton RK. Executive dysfunction in schizophrenia. In: Sharma T, Harvey PD, editors. Cognition in Schizophrenia: Impairments, Importance and Treatment Strategies. Oxford, UK: Oxford University Press; 2000. pp. 51–72. [Google Scholar]
- 43.Weinman J. An Outline of Psychology as Applied to Medicine. Bristol: John Wright; 1981. [Google Scholar]
- 44.Dickinson D, Ramsey ME, Gold JM. Overlooking the obvious: A meta-analytic comparison of digit symbol coding tasks and other cognitive measures in schizophrenia. Arch Gen Psychiatry. 2007;64:532–42. doi: 10.1001/archpsyc.64.5.532. [DOI] [PubMed] [Google Scholar]
- 45.Green MF, Penn DL, Bentall R, Carpenter WT, Gaebel W, Gur RC, et al. Social cognition in schizophrenia: An NIMH workshop on definitions, assessment, and research opportunities. Schizophr Bull. 2008;34:1211–20. doi: 10.1093/schbul/sbm145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ikebuchi E, Nakagome K, Ikezawa S, Miura S, Yamasaki S, Nemoto T, et al. Social cognition of schizophrenia: Bridging gap between brain science and psychosocial intervention. Seishin Shinkeigaku Zasshi. 2012;114:489–507. [PubMed] [Google Scholar]
- 47.McCleery A, Ventura J, Kern RS, Subotnik KL, Gretchen-Doorly D, Green MF, et al. Cognitive functioning in first-episode schizophrenia: MATRICS consensus cognitive battery (MCCB) profile of impairment. Schizophr Res. 2014;157:33–9. doi: 10.1016/j.schres.2014.04.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Konstantakopoulos G, Oulis P, Ploumpidis D, Patrikelis P, Nikitopoulou S, Papadimitriou GN, et al. Self-rated and performance-based empathy in schizophrenia: The impact of cognitive deficits. Soc Neurosci. 2014;9:590–600. doi: 10.1080/17470919.2014.934395. [DOI] [PubMed] [Google Scholar]
- 49.Kato M, Kato Y. Mirror neuron system dysfunction in schizophrenia and its clinical implication. Brain Nerve. 2014;66:665–72. [PubMed] [Google Scholar]
- 50.Mehta UM, Thirthalli J, Basavaraju R, Gangadhar BN. Association of intracortical inhibition with social cognition deficits in schizophrenia: Findings from a transcranial magnetic stimulation study. Schizophr Res. 2014;158:146–50. doi: 10.1016/j.schres.2014.06.043. [DOI] [PubMed] [Google Scholar]
- 51.Bratti IM, Blder RM. Neurocognitive deficits and first-episode schizophrenia: Characterization and course. In: Sharma T, Harvey PD, editors. The Early Course of Schizophrenia. Oxford, UK: Oxford University Press; 2006. pp. 87–110. [Google Scholar]
- 52.Henry JD, Crawford JR. A meta-analytic review of verbal fluency deficits in schizophrenia relative to other neurocognitive deficits. Cogn Neuropsychiatry. 2005;10:1–33. doi: 10.1080/13546800344000309. [DOI] [PubMed] [Google Scholar]
- 53.Fioravanti M, Carlone O, Vitale B, Cinti ME, Clare L. A meta-analysis of cognitive deficits in adults with a diagnosis of schizophrenia. Neuropsychol Rev. 2005;15:73–95. doi: 10.1007/s11065-005-6254-9. [DOI] [PubMed] [Google Scholar]
- 54.Reichenberg A, Harvey PD. Neuropsychological impairments in schizophrenia: Integration of performance-based and brain imaging findings. Psychol Bull. 2007;133:833–58. doi: 10.1037/0033-2909.133.5.833. [DOI] [PubMed] [Google Scholar]
- 55.Kraus MS, Keefe RS. Cognition as an outcome measure in schizophrenia. Br J Psychiatry Suppl. 2007;50:s46–51. doi: 10.1192/bjp.191.50.s46. [DOI] [PubMed] [Google Scholar]
- 56.Nuechterlein KH, Green MF. MATRICS Consensus Cognitive Battery Manual. MATRICS Assessment. 2006 [Google Scholar]
- 57.Keefe RS, Bilder RM, Harvey PD, Davis SM, Palmer BW, Gold JM, et al. Baseline neurocognitive deficits in the CATIE schizophrenia trial. Neuropsychopharmacology. 2006;31:2033–46. doi: 10.1038/sj.npp.1301072. [DOI] [PubMed] [Google Scholar]
- 58.Patterson TL, Goldman S, McKibbin CL, Hughs T, Jeste DV. UCSD performance-based skills assessment: Development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. 2001;27:235–45. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- 59.Velligan DI, DiCocco M, Bow-Thomas CC, Cadle C, Glahn DC, Miller AL, et al. Abrief cognitive assessment for use with schizophrenia patients in community clinics. Schizophr Res. 2004;71:273–83. doi: 10.1016/j.schres.2004.02.027. [DOI] [PubMed] [Google Scholar]
- 60.Randolph C. Repeatable Battery for the Assessment of Neuropsychological Status. The Psychological Corporation, San Antonio, TX. 1998 [Google Scholar]
- 61.Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The brief assessment of cognition in schizophrenia: Reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res. 2004;68:283–97. doi: 10.1016/j.schres.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 62.Robbins TW, Sahakian BJ. Computer methods of assessment of cognitive function. In: Copeland JR, Abou-Saleh MT, Blazers DG, editors. Principles and Practice of Geriatric Psychiatry. Chichester: John Wiley & Sons Ltd.; 1994. pp. 205–9. [Google Scholar]
- 63.Hunter R, Cameron S, Perks S, Wesnes K. The cognitive profile of unmedicated schizophrenic patients in relation to controls. J Psychopharmacol. 1997;11((Suppl)):A74. [Google Scholar]
- 64.CogTest plc. Cogtest (tm) Computerized Cognitive Battery for Clinical Trials. 2002. [Last accessed on 2015 Oct 22]. Available from: http://www.cogtest.com .
- 65.Inada K, Oshibuchi H, Shigooka J. Significance of the pharmacotherapy of schizophrenia in the emotional context processing of cognition. Nihon Shinkei Seishin Yakurigaku Zasshi. 2013;33:101–4. [PubMed] [Google Scholar]
- 66.Keedy SK, Reilly JL, Bishop JR, Weiden PJ, Sweeney JA. Impact of antipsychotic treatment on attention and motor learning systems in first-episode schizophrenia. Schizophr Bull. 2015;41:355–65. doi: 10.1093/schbul/sbu071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Harvey PD, Keefe RS. Studies of cognitive change in patients with schizophrenia following novel antipsychotic treatment. Am J Psychiatry. 2001;158:176–84. doi: 10.1176/appi.ajp.158.2.176. [DOI] [PubMed] [Google Scholar]
- 68.Keefe RS, Bilder RM, Davis SM, Harvey PD, Palmer BW, Gold JM, et al. Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE trial. Arch Gen Psychiatry. 2007;64:633–47. doi: 10.1001/archpsyc.64.6.633. [DOI] [PubMed] [Google Scholar]
- 69.Choi KH, Wykes T, Kurtz MM. Adjunctive pharmacotherapy for cognitive deficits in schizophrenia: Meta-analytical investigation of efficacy. Br J Psychiatry. 2013;203:172–8. doi: 10.1192/bjp.bp.111.107359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Keefe RS. The longitudinal course of cognitive impairment in schizophrenia: An examination of data from premorbid through posttreatment phases of illness. J Clin Psychiatry. 2014;75(Suppl 2):8–13. doi: 10.4088/JCP.13065su1.02. [DOI] [PubMed] [Google Scholar]
- 71.Pillet B, Morvan Y, Todd A, Franck N, Duboc C, Grosz A, et al. Cognitive remediation therapy (CRT) benefits more to patients with schizophrenia with low initial memory performances. Disabil Rehabil. 2015;37:846–53. doi: 10.3109/09638288.2014.946153. [DOI] [PubMed] [Google Scholar]
- 72.Puig O, Penadés R, Baeza I, De la Serna E, Sánchez-Gistau V, Bernardo M, et al. Cognitive remediation therapy in adolescents with early-onset schizophrenia: A randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2014;53:859–68. doi: 10.1016/j.jaac.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 73.Chen JF. Adenosine receptor control of cognition in normal and disease. Int Rev Neurobiol. 2014;119:257–307. doi: 10.1016/B978-0-12-801022-8.00012-X. [DOI] [PubMed] [Google Scholar]
- 74.Amminger GP, Schäfer MR, Papageorgiou K, Klier CM, Cotton SM, Harrigan SM, et al. Long-chain omega-3 fatty acids for indicated prevention of psychotic disorders: A randomized, placebo-controlled trial. Arch Gen Psychiatry. 2010;67:146–54. doi: 10.1001/archgenpsychiatry.2009.192. [DOI] [PubMed] [Google Scholar]
- 75.Javitt DC. Effects of intranasal AL-108 (davunetide) on neurocognition and functional outcome in schizophrenia. Schizophr Res. 2010;117:118–9. [Google Scholar]
- 76.Kalache SM, Mulsant BH, Davies SJ, Liu AY, Voineskos AN, Butters MA, et al. The impact of aging, cognition, and symptoms on functional competence in individuals with schizophrenia across the lifespan. Schizophr Bull. 2015;41:374–81. doi: 10.1093/schbul/sbu114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Balzan RP, Neaves A, Denson LA, Liu D, Galletly C. Cognitive deficit awareness in schizophrenia: Absent, intact, or somewhere in-between? Cogn Neuropsychiatry. 2014;19:471–84. doi: 10.1080/13546805.2014.909311. [DOI] [PubMed] [Google Scholar]


