Abstract
Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome is a rare complex of structural abnormalities of the female urogenital tract. A 17-year-old girl with uterine didelphys associated with OHVIRA syndrome presented with progressive development of cyclic lower abdominal discomfort and a large abdominopelvic mass. We describe the findings from ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), the first case report of this syndrome to examine all three different imaging modalities in a single patient. We also review the literature on OHVIRA syndrome and discuss important considerations relevant to radiologists and other clinicians.
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging
Case report
A 17-year-old nulligravida female presented to a regional emergency department for evaluation of left-lower-quadrant bulging and pain. She reported progressively increasing lower abdominal distension, with pain as well as discomfort over the prior two months, which was cyclically associated with the onset of menses. The patient additionally reported symptoms of increased urinary frequency and urgency in addition to constipation. On review, she denied fever, abnormal vaginal discharge, or perceived change in menstrual flow.
The patient experienced regular cycles every 23 days with 5 to 8 days of flow since menarche at age 13. She reported only mild dysmenorrhea, managed with nonsteroidal anti-inflammatory drugs (NSAIDs) before the onset of her current symptoms. The patient acknowledged initiating sexual activity over the prior six months but had recently discontinued activity secondary to discomfort. Her medical history was significant for a congenitally absent left kidney diagnosed antenatally as well as right vesicourethral reflux that was surgically corrected at age 7.
On evaluation in the emergency department, the patient was afebrile with normal vital signs. Laboratory findings included white-blood-cell count (7,800 cells/microliter), hematocrit (32.9%), and serum creatinine (0.8 mg/dL). A pregnancy test was negative. A large, tense, protuberant mass, extending from the anterior vaginal vault to slightly beyond her umbilicus, was noted on physical examination. The external genitalia were within normal limits. Pelvic examination was limited in the emergency room because of the tense swelling and compression of the anterior vaginal wall.
Transabdominal sonography demonstrated an absent left kidney and a large, tubular, cystic pelvic mass, at least 18×11 cm, with low-level internal echoes displacing the pelvic organs to the right (Fig. 1). The uterus and right ovary were displaced to the right. The left ovary was pushed posteriorly and to the left. The right and left ovaries appeared normal and were 3.6 × 2.6 × 2.7 cm and 3.2 × 2.9 × 1.9 cm in dimensions, respectively. The uterus was measured as 5.4 × 3.4 × 2.2 cm. Transvaginal sonography was not performed due to patient discomfort.
Figure 1.

17-year-old girl with uterine didelphys associated with OHVIRA syndrome. Longitudinal transabdominal sonographic image through the pelvis demonstrates a markedly dilated vagina, approximately 18×11 cm, containing echogenic material consistent with blood product.
She was referred to a gynecologist out of initial concern for a pelvic malignancy. An abdominal/pelvic CT confirmed an absent left kidney and a large low-attenuating, nonenhancing midline pelvic mass, approximately 11×12×18 cm. This was connected with a low-attenuating, nonenhancing convoluted longitudinal structure in the left pelvis, consistent with a hydrometrocolpos and left hydrosalpinx (Fig. 2). The hydrometrocolpos displaced and partially obstructed the distal right ureter, with attendant mild right hydronephrosis (Fig. 3). Both ovaries appeared normal.
Figure 2.

17-year-old girl with uterine didelphys associated with OHVIRA syndrome. Coronal-reformatted, contrast-enhanced CT image demonstrates a blood-filled, markedly dilated vagina (large single arrow), normal right hemiuterine horn (arrowhead), and distended left hemiuterine horn (small paired arrows) with an attenuation of 70 Hounsfield units, suggesting the presence of blood in it.
Figure 3.
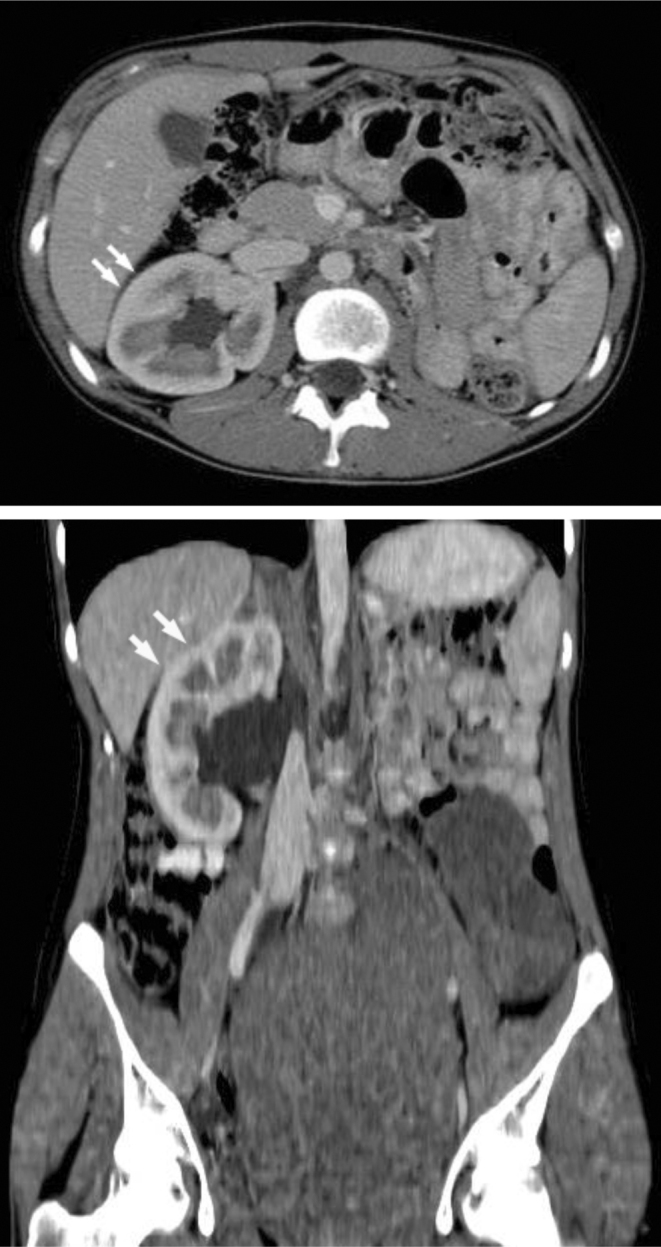
17-year-old girl with uterine didelphys associated with OHVIRA syndrome. Axial contrast-enhanced CT image (top) and coronal-reformatted, contrast-enhanced CT image (above) demonstrate a mildly hypertrophied right kidney (arrows) and an absent left kidney.
The patient was referred to our institution for further evaluation and management of a suspected Müllerian duct anomaly. An abdominopelvic MRI was obtained for further preoperative planning and characterization of anatomy. It showed a massively dilated fluid-filled tubular structure between the rectum and the urinary bladder measuring 21×13×12.4 cm. This midline structure with high T1- and low T2-signal intensity was compatible with a markedly dilated vagina containing blood products and an obstructing low transverse vaginal septum. The dilated vagina was compressing and displacing both the urinary bladder and sigmoid colon (Fig. 4).
Figure 4.

17-year-old girl with uterine didelphys associated with OHVIRA syndrome. Sagittal T2-weighted MR image demonstrates a dilated hemivagina with low T2-signal-intensity contents and corresponding high T1-signal intensity consistent with blood product.
Two additional tubular structures originated bilaterally from the anterosuperior apex of the midline tubular structure, consistent with a uterine didelphys: The left-sided tubular structure was moderately dilated, with an axial diameter of 5.2 cm. The lesion was surrounded by a thick wall that may have represented myometrium. Thus, the lesion was most consistent with a left-sided dilated uterus and/or a dilated left-sided adnexa. The lesion contained fluid with the same MR characteristics as the midline structure, suggesting an open connection (Fig. 5). Above the apex of this tubular structure, a normal left ovary with several follicular cysts was seen. The right-sided tubular structure had a diameter of 2.3 cm, and had a thick wall that may have represented myometrium. The lesion was most consistent with a right-sided nondilated uterus. The lesion was not dilated and did not contain fluid, suggesting no connection with the midline tubular structure (Fig. 6). A normal right ovary with several follicular cysts was seen. An additional dilated, fluid-filled, serpiginous tubular structure medial to the left psoas muscle originated at the expected location of the left kidney and inserted dorsally into the dilated vagina, most likely representing an ectopic left hydroureter. This tubular lesion displaced the left psoas muscle laterally (Fig. 7). The left kidney was again noted to be congenitally absent, while the right kidney was found in orthotopic position and showed a compensatory hypertrophy.
Figure 5.
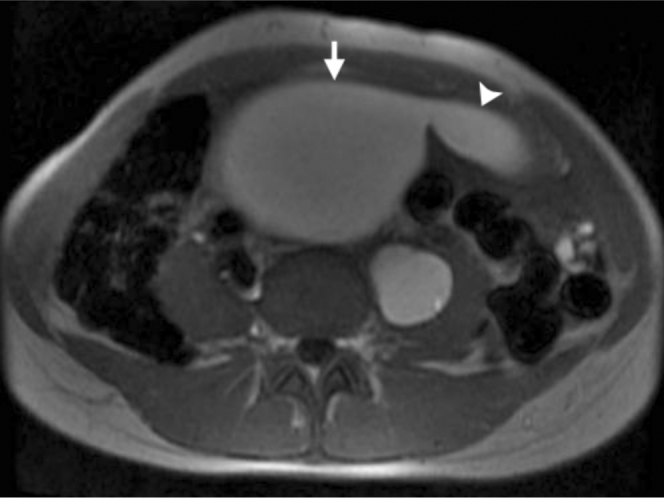
17-year-old girl with uterine didelphys associated with OHVIRA syndrome. Axial T1-weighted MR image demonstrates a left hydrosalpinx (arrowhead) containing high T1-signal-intensity contents consistent with blood products, with an axial diameter of 5.2 cm, originating from a dilated hemivagina (arrow).
Figure 6.
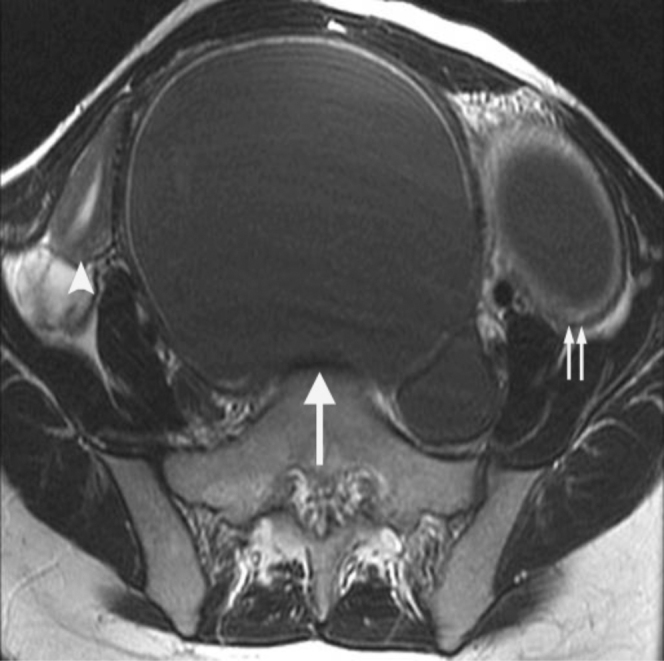
17-year-old girl with uterine didelphys associated with OHVIRA syndrome. Axial T2-weighted MR image demonstrates a dilated vagina with low T2-signal-intensity contents that had corresponding high T1-signal intensity consistent with blood products (large single arrow). Normal-appearing right uterine horn (arrowhead) and dilated left uterine horn with low T2-signal-intensity blood products (small paired arrows) also appear.
Figure 7.
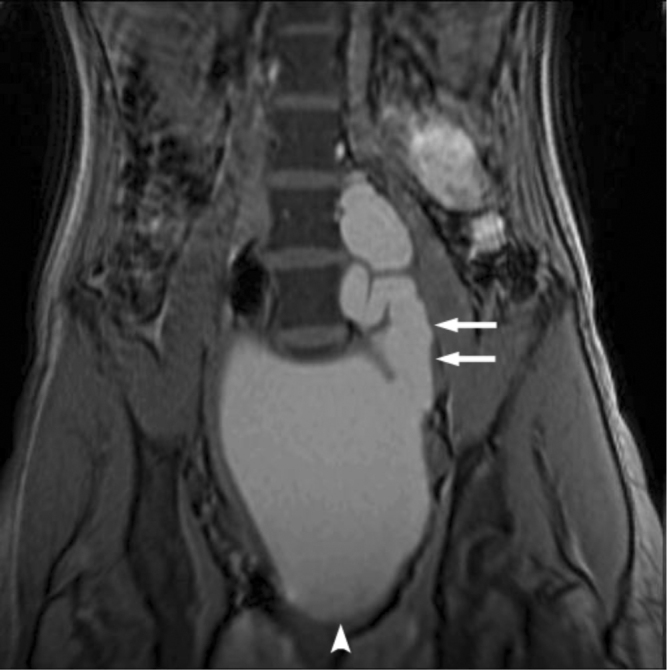
17-year-old girl with uterine didelphys associated with OHVIRA syndrome. Coronal T1-weighted MR image demonstrates an ectopic insertion of a dilated ureter (paired arrows), containing high T1-signal-intensity contents consistent with refluxed blood products, into a dilated left vaginal canal (arrowhead).
The final diagnosis on MRI was uterine didelphys, left-obstructed hemivagina in association with ipsilateral renal agenesis (OHVIRA) and remnant left ureter. An overall diagrammatic representation of the anatomy of this patient makes this clearer (Fig. 8).
Figure 8.
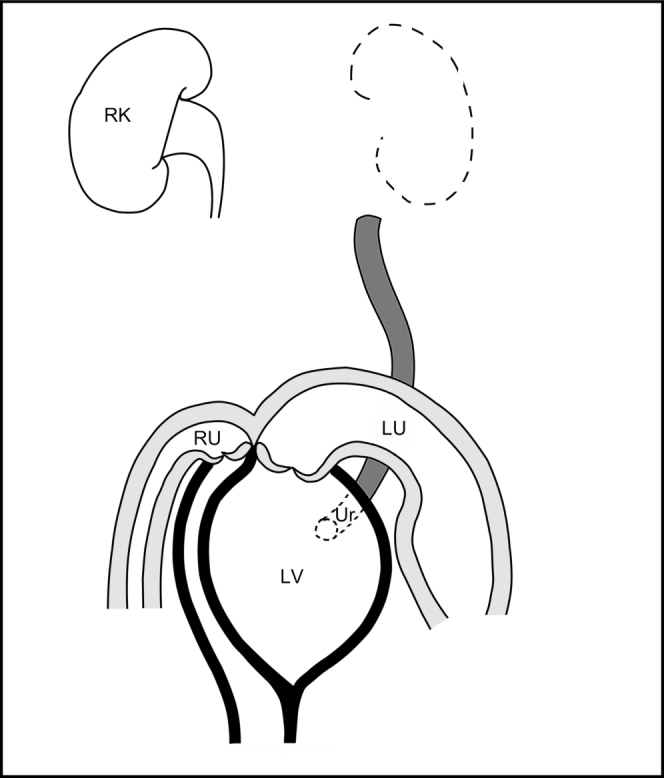
17-year-old girl with uterine didelphys associated with OHVIRA syndrome. Diagrammatic representation of the anatomy of this patient. LV: obstructed left hemivagina dilated with blood product. RU: nondilated right uterine horn. LU: left uterine horn dilated with blood product. Ur: ectopic ureter inserting into the left hemivagina. RK: right kidney.
The patient was taken to the operating room, and an examination under anesthesia was performed. A fluid wave was palpable from the anterior vaginal protuberance through the mass to the level of the umbilicus. The right cervix was noted to be laterally deviated secondary to the left obstructed hemivagina. The fibrotic septum obstructing the left hemivagina was opened with a cruciate incision, and two liters of dark brown hematocolpos were evacuated. The residual septum was then circumferentially excised to fully open and expose the left hemivagina and cervix. The patient was discharged to home the same day from her surgery.
Discussion
Congenital anomalies of the Müllerian tract are estimated to have an overall prevalence of 2% to 3% among women (1). The syndrome of obstructed hemivagina and ipsilateral renal anomaly was initially reported in 1922 and is known as Herlyn-Werner-Wunderlich syndrome or, more recently, by the acronym OHVIRA (2, 3, 4, 5). The OHVIRA syndrome classically occurs in the setting of uterine didelphys or, more rarely, a septate uterus (1, 2). Renal agenesis is the most commonly reported urologic anomaly in OHVIRA syndrome, although other malformations, including renal duplication and multicystic dysplastic kidney, have also been described (2).
The pathogenesis of OHVIRA syndrome is unknown but believed to be multifactorial. Uterine didelphys occurs as a result of fusion failure of the Müllerian ducts. Early high-grade obstruction of the pelvicoureteric junction, resulting in agenesis of ipsilateral kidney, often induces defects in the Müllerian duct at the same level. Because of the close relationship between the development of urinary and reproductive systems, female patients with renal malformations may benefit from evaluation later in life for reproductive structural anomalies (6) and, conversely, women with Müllerian anomalies should be screened for renal abnormalities.
The typical patient with this rare condition usually presents after menarche with nonspecific symptoms of recurrent pelvic pain or dysmenorrhea from progressive distention of the obstructed hemivagina. As in our case, the hematocolpos is commonly detected as a pelvic mass, with initial concern for neoplasm (6, 7). Early and accurate diagnosis is important because prompt therapeutic intervention can relieve symptoms, prevent further complications related to chronic obstructed hematocolpos (such as endometriosis and pelvic adhesions), and maintain reproductive capacity (6). In a reported series of 27 cases, the age at diagnosis varied from 10 to 29 years, with a median age of 14 years (2). Delays in diagnosis were blamed on lack of knowledge of the disease, regular menstruations in context of an incomplete vaginal outlet obstruction, and slow extension of hematocolpos (8). Our patient was essentially asymptomatic until development of a very large hematocolpos, which extended to the level of the umbilicus. The operative report obtained from the patient’s earlier childhood right ureteral reimplantation (performed through a Pfannenstiel incision) did not include any comment on morphology of uterus or adnexa. In the aforementioned large case series, uterine anomalies were not detected and correctly diagnosed in any patients who had previously undergone surgical exploration of the pelvis prior to referral (2).
Sonography is frequently the initial imaging modality for evaluation of suspected Müllerian duct anomalies, given wide availability of ultrasound units and relative low cost. However, it depends highly on the expertise of the operator. It can be difficult to differentiate a hematometra with thin, stretched myometrium from hemorrhagic adnexal masses on ultrasound. MR imaging is an excellent modality for evaluating the frequently complex Müllerian duct anomalies, given its multiplanar capability, superior tissue characterization, and large field of view. MR imaging can accurately depict the uterine contour, shape of uterine cavity, and associated cervical and vaginal anomalies, important in the classification of Müllerian duct anomalies and in surgical planning (9). In addition, MR imaging can provide tissue characterization of the septa (10), characterize the contents of obstructed cavities (for example, simple fluid versus blood), and easily detect any coexisting renal and/or urethral abnormalities.
Primary management of the OHVIRA syndrome is vaginoplasty, to relieve the obstruction. Historically, surgeons advocated a two-stage procedure, with the initial surgery to reduce the hematocolpos and the second to resect the excess septum after a period of wound-healing and vaginal remodeling. A single-stage vaginoplasty, involving complete resection of the septum in a single procedure, is supported by the contemporary literature (2).
A dilated ectopic ureter with insertion into the obstructed left hemivagina was identified in our patient on her initial imaging. The apparent congenital absence of a left kidney on conventional MRI does not, however, fully exclude the possible presence of a small and atrophic kidney. The radiologic identification of a dysplastic kidney can be very challenging; additional diagnostic modalities that may be considered include intravenous urography, Technetium-99m dimercaptosuccinic acid (DMSA) renal scan, and contrast vaginography (11, 12). Clinically, ectopic vaginal ureter in conjunction with a dysplastic kidney can be associated with chronic purulent vaginal discharge (13). Management is directed through either transvaginal ligation of the ureter or laparoscopic transperitoneal nephrectomy. Malignant transformation of ectopic vaginal ureters has been reported in the literature (14, 15).
In summary, pediatricians, gynecologists, radiologists, and pediatric surgeons should consider Müllerian structural anomalies and associated urologic abnormalities among the differential diagnoses in young female patients presenting with a pelvic mass.
Footnotes
Published: January 24, 2010
References
- 1.Shavell VI, Montgomery SE, Johnson SC, Diamond MP, Berman JM. Complete septate uterus, obstructed hemivagina, and ipsilateral renal anomaly: pregnancy course complicated by a rare urogenital anomaly. Arch Gynecol Obstet. 2009 Sep;280(3):449–452. doi: 10.1007/s00404-008-0919-6. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Smith NA, Laufer MR. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertil Steril. 2007 Apr;87(4):918–922. doi: 10.1016/j.fertnstert.2006.11.015. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Gholoum S, Puligandla PS, Hui T, Su W, Quiros E, Laberge JM. Management and outcome of patients with combined vaginal septum, bifid uterus, and ipsilateral renal agenesis (Herlyn-Werner-Wunderlich syndrome) J Pediatr Surg. 2006 May;41(5):987–992. doi: 10.1016/j.jpedsurg.2006.01.021. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Herlyn U, Werner H. [Simultaneous occurrence of an open Gartner-duct cyst, a homolateral aplasia of the kidney and a double uterus as a typical syndrome of abnormalities] Geburtshilfe Frauenheilkd. 1971 Apr;31(4):340–347. [PubMed] [PubMed] [Google Scholar]
- 5.Wunderlich M. [Unusual form of genital malformation with aplasia of the right kidney] Zentralbl Gynakol. 1976;98(9):559–562. [PubMed] [PubMed] [Google Scholar]
- 6.Orazi C, Lucchetti MC, Schingo PM, Marchetti P, Ferro F. Herlyn-Werner-Wunderlich syndrome: uterus didelphys, blind hemivagina and ipsilateral renal agenesis. Sonographic and MR findings in 11 cases. Pediatr Radiol. 2007 Jul;37(7):657–665. doi: 10.1007/s00247-007-0497-y. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Stassart JP, Nagel TC, Prem KA, Phipps WR. Uterus didelphys, obstructed hemivagina, and ipsilateral renal agenesis: the University of Minnesota experience. Fertil Steril. 1992 Apr;57(4):756–761. doi: 10.1016/s0015-0282(16)54955-3. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Zurawin RK, Dietrich JE, Heard MJ, Edwards CL. Didelphic uterus and obstructed hemivagina with renal agenesis: case report and review of the literature. J Pediatr Adolesc Gynecol. 2004 Apr;17(2):137–141. doi: 10.1016/j.jpag.2004.01.016. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Tanaka YO, Kurosaki Y, Kobayashi T, Eguchi N, Mori K, Satoh Y, Nishida M, Kubo T, Itai Y. Uterus didelphys associated with obstructed hemivagina and ipsilateral renal agenesis: MR findings in seven cases. Abdom Imaging. 1998 Jul-Aug;23(4):437–441. doi: 10.1007/s002619900375. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Carrington BM, Hricak H, Nuruddin RN, Secaf E, Laros RK, Jr., Hill EC. Mullerian duct anomalies: MR imaging evaluation. Radiology. 1990 Sep;176(3):715–720. doi: 10.1148/radiology.176.3.2202012. [PubMed] [DOI] [PubMed] [Google Scholar]
- 11.Son le T, Thang le C, Hung le T, Tram NT. Single ectopic ureter: diagnostic value of contrast vaginography. Urology. 2009 Aug;74(2):314–317. doi: 10.1016/j.urology.2009.02.067. [PubMed] [DOI] [PubMed] [Google Scholar]
- 12.Yu HT, Chao A, Wang CJ, Chao AS, Lai CY, Wang CR, Huang YC. Integrated imaging studies and endoscopic management of purulent vaginal discharge in a 6-year-old: vaginal ectopic ureter associated with ipsilateral dysplastic kidney. Eur J Obstet Gynecol Reprod Biol. 2009 Feb;142(2):160–161. doi: 10.1016/j.ejogrb.2008.10.004. [PubMed] [DOI] [PubMed] [Google Scholar]
- 13.Jain KA. Ectopic vaginal insertion of an obstructed duplicated ureter in an adult female: demonstration by magnetic resonance imaging. Clin Imaging. 2007 Jan-Feb;31(1):54–56. doi: 10.1016/j.clinimag.2006.07.001. [PubMed] [DOI] [PubMed] [Google Scholar]
- 14.Jaidane M, Slama A, Bibi M. A tumor of an ectopic ureter mimicking uterine cervix adenocarcinoma: case report and brief review. Int Urogynecol J Pelvic Floor Dysfunct. 2009 Apr 29 doi: 10.1007/s00192-009-0893-y. [PubMed] [DOI] [PubMed] [Google Scholar]
- 15.Sameshima H, Nagai K, Ikenoue T. Single vaginal ectopic ureter of fetal metanephric duct origin, ipsilateral kidney agenesis, and ipsilateral rudimentary uterine horn of the bicornuate uterus. Gynecol Oncol. 2005 Apr;97(1):276–278. doi: 10.1016/j.ygyno.2004.12.012. [PubMed] [DOI] [PubMed] [Google Scholar]


