Abstract
Complete extra-esophageal migration of a foreign object is rare. Its early and accurate diagnosis by complementary imaging modalities is crucial for a successful extraction. We present a case of ingested wire bristle, which completely traversed the esophageal mucosa to position itself in the soft tissue of the left neck adjacent to the internal carotid artery. We discuss the importance of imaging in the detection of migrating foreign bodies, and raise awareness of this serious complication.
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging
Case report
A 74-year-old man presented to an outpatient clinic with progressive onset of dysphagia and odynophagia four days after a barbeque meal. He remembered a transient swallowing discomfort after taking the first bite of his meal but did not pay much attention to his symptomatology until experiencing a more permanent scraping sensation at his neck and upper thoracic region. The patient was supposed to have an otorhinolaryngologic consultation the following day. However, severe odynophagia forced him to visit the emergency services of our institution the same day. Chest radiograph showed a barely visible curvilinear metallic foreign body superior to the medial aspect of the left clavicle (Fig. 1).
Figure 1.
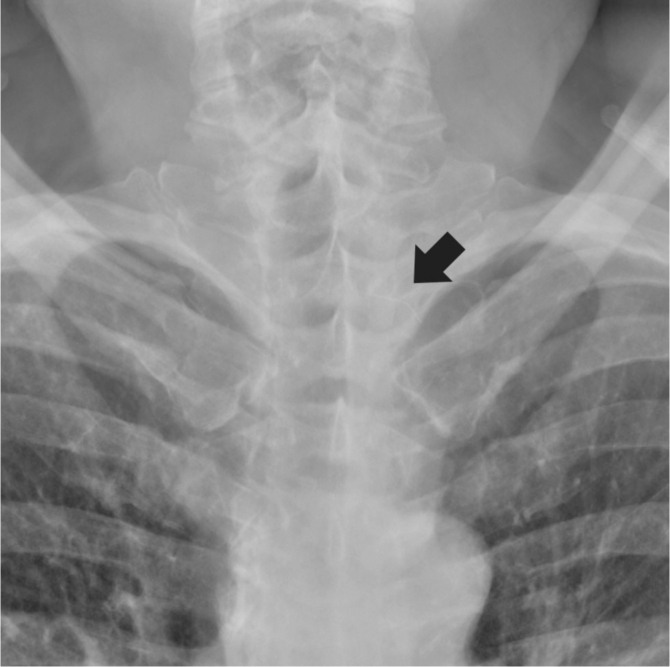
74-year-old man with extra-esophageal ingested wire bristle. Magnified anterior chest radiograph shows a barely visible wire bristle projecting over the left upper thoracic spine (arrow).
A soluble-contrast esophagram showed a small wire extrinsic to the esophagus, and no esophageal perforation. There was, however, a mass effect medial to the wire with right deviation of the opacified proximal esophageal lumen (Fig. 2).
Figure 2.
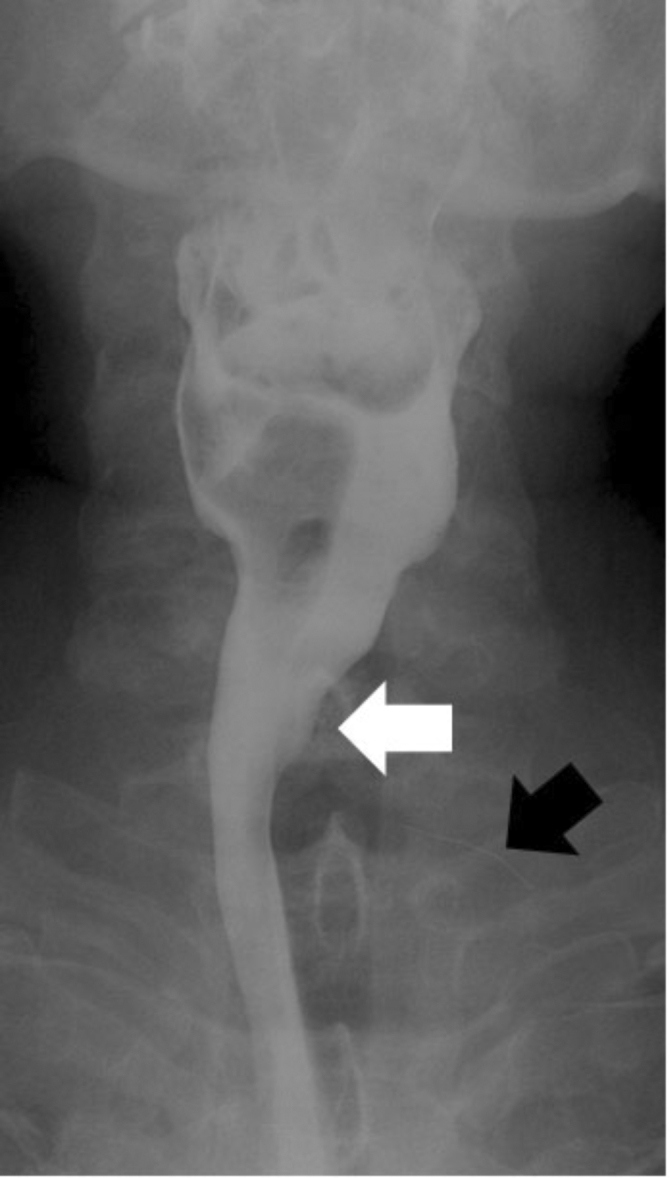
74-year-old man with extra-esophageal ingested wire bristle. Esophagram shows the right deviation of the proximal esophagus (white arrow) secondary to soft-tissue inflammation adjacent to the wire bristle (black arrow). There is no evidence of extra-esophageal contrast leak.
An emergent CT scan confirmed the extra-esophageal migration of a 2.5-cm metallic wire into the left superior mediastinum, in close proximity to the internal carotid artery (Fig. 3).
Figure 3.
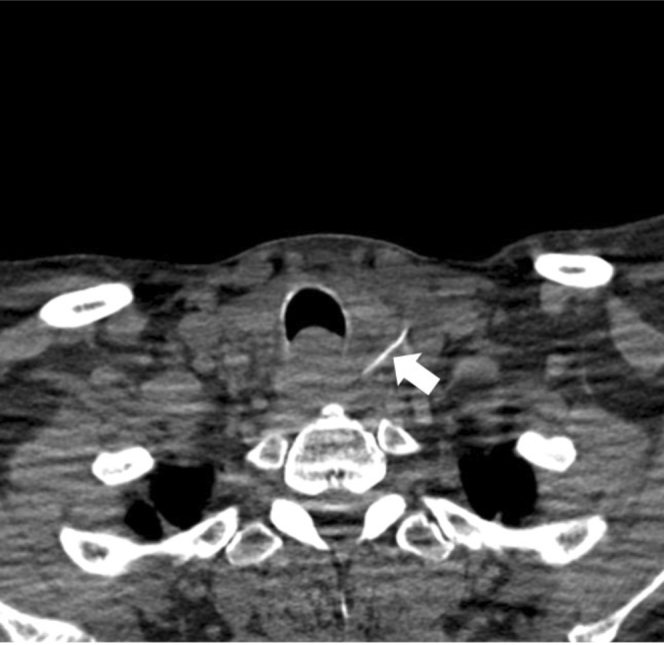
74-year-old man with extra-esophageal ingested wire bristle. Axial CT image shows the wire bristle medial to the left common carotid artery (arrow).
The reformatted oblique CT reconstruction showed the foreign body anterior to C7 and behind the clavicle (Fig. 4).
Figure 4.

74-year-old man with extra-esophageal ingested wire bristle. Reformatted oblique CT reconstruction image shows the metallic foreign body anterior to C7 and posterior to the medial aspect of the left clavicle (arrow).
Rigid esophagoscopy showed an erythematous spot 20 cm from the incisor, suggestive of perforation with mucopurulent discharges. Left-neck surgical exploration was required to extract the swallowed wire bristle. The postoperative course was free of any complication.
Discussion
Because of a potentially high morbidity linked to vascular involvement following esophageal perforation by foreign bodies, prompt and accurate diagnosis is crucial for early surgical intervention. Treating physicians should obtain a pertinent clinical history and recognize symptoms of perforated esophagus with foreign bodies to initiate appropriate radiographic studies. The common triad signs of esophageal perforation are pain, fever, and subcutaneous and/or mediastinal emphysema (1). Pain is often localized to the site of perforation. Neck pain and sternocleidomastoid tenderness may be associated with cervical perforations; substernal pain worsening with swallowing and deep inspiration suggests thoracic perforations. When an esophageal perforation is suspected, upright chest radiographs may suggest the diagnosis in 90% of the cases, with the demonstration of extraesophageal foreign bodies, subcutaneous emphysema, pneumomediastinum, pneumothorax, hydrothorax, and pleural effusion (1, 2). With cervical esophageal perforation, emphysematous air in the neck can be palpated and detected by radiographs in 60% and 95% of all patients, respectively (3, 4). However, with thoracic esophageal perforation, only 30% can be detected by palpation and 40% by radiographs. Conversely, right pleural effusion is seen only in less than 10% of patients with cervical rupture, while left pleural effusion occurs in 50% or more with thoracic injury (3, 4). It should be emphasized that radiographs may not be able to detect soft-tissue emphysema and pleural effusion if taken too soon after perforation.
Perforation with foreign objects commonly occurs at the hypopharynx and the esophagus. There are several reasons to account for these particular sites. First, the esophagus is anatomically narrowed at the pyriform fossa, the aortic arch, and the esophagogastric junction (1, 2). Second, the pyriform fossa has a tenuous blood supply with a lack of reinforcing muscle layer. Third, certain cervical spine deformities (for example, diffuse intervertebral hyperostosis, kyphosis, and hypertrophic spurs) can predispose the cervical esophagus to perforation. Injury to the aortic arch and esophagogastric junction has rarely been reported.
CT, with rapid cross-sectional and three-dimensional imaging capability, is presently the modality of choice for extra-esophageal migrating objects. CT provides the best anatomic localization of the foreign body with regard to vital cervical and mediastinal anatomic landmarks and allows the most accurate therapeutic planning (5, 6). In addition, certain indirect CT features such as thickened esophageal wall, mediastinal fluid collections and inflammation, contrast extravasation, and pleural effusion may contribute to the diagnosis of esophageal injury. Contrast esophagraphy is complementary to CT examination in detecting perforations and related complications, such as pneumothorax and pneumomediastinum (7, 8). Due to the potential of barium-induced mediastinitis, a water-soluble agent such as Gastrografin is used initially to detect perforations (8). When the Gastrografin study is negative in the setting of high suspicion for esophageal leaks, a barium study should be considered, because it has better coating properties and can detect smaller leaks (8). A CT scan should be performed first when in doubt, because CT contrast does not interfere with luminal studies.
In conclusion, we present a case of esophageal perforation by wire bristle and discuss the importance of clinical history gathering and the contribution of various imaging modalities to achieve prompt diagnosis and successful extraction of the foreign body. Ingested wire with esophageal perforation is rare but potentially dangerous.
Footnotes
Published: January 31, 2010
References
- 1.Pasricha PJ, Fleischer DE, Kalloo AN. Endoscopic perforations of the upper digestive tract: A review of their pathogenesis, prevention, and management. Gastroenterology. 1994 Mar;106(3):787–802. doi: 10.1016/0016-5085(94)90717-x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Han SY, McElvein RB, Aldrete JS, Tishler JM. Perforation of the esophagus: correlation of site and cause with plain film findings. AJR Am J Roentgenol. 1985 Sep;145(3):537–540. doi: 10.2214/ajr.145.3.537. [PubMed] [DOI] [PubMed] [Google Scholar]
- 3.Younes Z, Johnson DA. The spectrum of spontaneous and iatrogenic esophageal injury: Perforations, Mallory-Weiss tears, and hematomas. J Clin Gastroenterol. 1999 Dec;29(4):306–317. doi: 10.1097/00004836-199912000-00003. [PubMed] [DOI] [PubMed] [Google Scholar]
- 4.Sarr MG, Pemberton JH, Payne WS. Management of instrumental perforations of the esophagus. J Thorac Cardiovasc Surg. 1982 Aug;84(2):211–218. [PubMed] [PubMed] [Google Scholar]
- 5.Campisi P, Stewart C, Forte V. Penetrating esophageal injury by ingestion of a wire bristle. J Pediatr Surg. 2005 Oct;40(10):e15–e16. doi: 10.1016/j.jpedsurg.2005.06.035. [PubMed] [DOI] [PubMed] [Google Scholar]
- 6.Hunter TB, Taljanovic MS. Foreign bodies. Radiographics. 2003 May-Jun;23(3):731. doi: 10.1148/rg.233025137. [PubMed] [DOI] [PubMed] [Google Scholar]
- 7.Dangman BC, Griscom NT. Pediatric case of the day. Esophageal foreign body with perforation and mediastinitis. Radiographics. 1991 Jan;11(1):156–158. doi: 10.1148/radiographics.11.1.1996393. [PubMed] [DOI] [PubMed] [Google Scholar]
- 8.Buecker A, Wein BB, Neuerburg JM, Guenther RW. Esophageal perforation: comparison of use of aqueous and barium-containing contrast media. Radiology. 1997 Mar;202(3):683–686. doi: 10.1148/radiology.202.3.9051016. [PubMed] [DOI] [PubMed] [Google Scholar]


