Abstract
Previous studies have shown that an increased number of axillary lymph nodes with metastatic involvement is associated with nonvisualization of lymph nodes during lymphoscintigraphy. We report a case of nonvisualization of the sentinel node during lymphoscintigraphy in a female with advanced breast cancer to support this association. Although many factors can affect visualization of the sentinel node during lymphoscintigraphy, the presence of advanced metastatic disease involving the lymphatic system must always be considered.
Abbreviations: CT, computed tomography; MRI, magnetic resonance imaging; PET, positron-emitting tomography
Case report
The patient, a 39-year-old female with no family history of breast cancer, initially presented with a palpable left breast mass. A breast ultrasound showed an irregular, solid, macrolobulated mass measuring 21.0 × 19.8 × 15.7 mm in the left breast at the 12 o'clock position. Internal echotexture was heterogeneous, and microcalcifications and vascularity were seen in the mass. The location of the mass correlated to the palpable abnormality in the left breast, and the patient was categorized as BIRADS 4. On ultrasound, a lymph node measuring 12.4 × 12.8 × 7.8 mm was identified in the left axilla, and a lymph node measuring 11.2 × 10.7 × 8.7 mm was identified in the right axilla. Both lymph nodes had imaging characteristics of benign lesions.
Subsequently, the patient underwent ultrasound-guided, vacuum-core biopsy of the breast mass that identified poorly differentiated invasive ductal carcinoma (BIRADS 6). The patient underwent bilateral breast MRI and a mammogram and was scheduled for surgery. On mammogram, breasts were heterogeneously dense, and a mass with associated fine pleomorphic calcifications, linear calcifications, and punctate calcifications was seen in the left breast upper hemisphere at the 12 o'clock position. Anterior and lateral to the group of malignant calcifications, there was a second small clustered group of calcifications. In the right breast, no masses, significant calcifications, or other abnormalities were seen. Magnetic resonance imaging (MRI) of the breasts showed three masses in the upper inner left breast. These masses included a 2.1 × 1.7-cm mass with spiculated margins in the 11 o’clock position, 8 cm from the nipple, which corresponded to the known malignancy. The two additional masses included a 9 × 9-mm enhancing mass in the 10 o’clock position of the left breast, 7 cm from the nipple, and an adjacent 6 × 6-mm enhancing mass. The findings were suspicious for multifocal carcinoma.
The patient underwent a PET-CT scan for staging. Approximately 50 minutes after the intravenous administration of 13.0 mCi of FDG, whole-body PET-CT imaging was performed. The patient's blood glucose level was 86 mg/dl at the time of injection of FDG. Images demonstrated a dominant suspicious lobular soft-tissue mass in the upper inner quadrant of the left breast measuring 1.9 cm, with a maximum SUV of 9.9. Two additional suspicious foci were seen more inferolaterally, at least one of which had an anatomic correlate. These most likely corresponded to the abnormally enhancing foci on the recently performed MRI of the breasts and were consistent with multifocal involvement. Focal metabolic activity was noted corresponding to a benign-appearing, 1.4 × 0.9-cm, low-lying left axillary lymph node (maximum SUV 1.6), and a 1.2-cm lymph node deep to the pectoralis minor muscle with maximum SUV 2.3 (Figure 1A, Figure 1B, Figure 1C). These lymph nodes were suspicious for regional nodal metastases. There was no evidence of suspicious right axillary, mediastinal, or hilar lymph nodes, including locations in the internal mammary chains and in the mediastinal fat surrounding the heart.
Figure 1A.
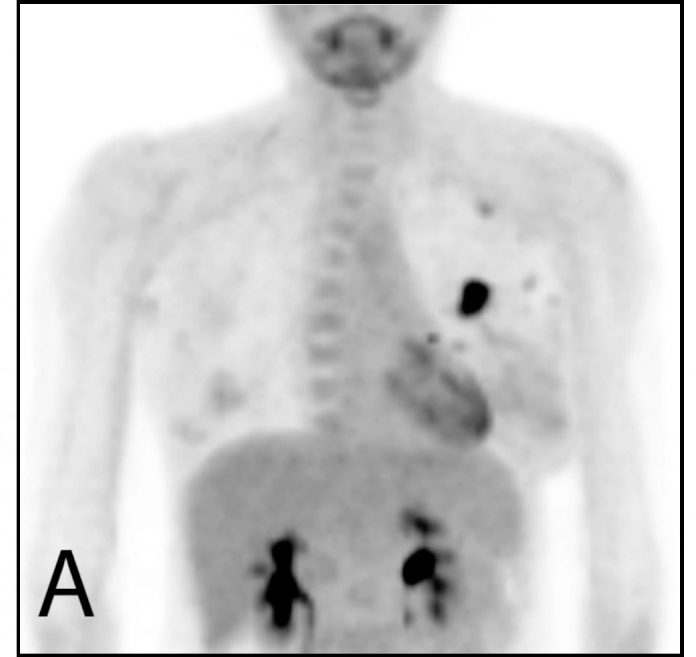
39-year-old woman with advanced breast cancer and nonvisualized sentinel node. Maximum-intensity projection (MIP) image from FDG PET scan demonstrating primary tumor in the left breast as well as left axillary lymph-node involvement.
Figure 1B.

39-year-old woman with advanced breast cancer and nonvisualized sentinel node. FDG PET-CT axial image demonstrating the dominant suspicious lobular soft-tissue mass in the upper inner quadrant of the left breast, measuring 1.9 cm with a maximum SUV of 9.9. Focal metabolic activity was also noted corresponding to a benign-appearing, 1.4 × 0.9-cm, low-lying left axillary lymph node with maximum SUV of 1.6.
Figure 1C.

39-year-old woman with advanced breast cancer and nonvisualized sentinel node. FDG PET-CT axial image demonstrating a 1.2-cm lymph node deep to the pectoralis minor muscle with maximum SUV of 2.3.
The patient was scheduled for surgery, and pre-operative lymphoscintigraphy was performed. She received an intradermal, peri-areolar administration of 110 μCi of filtered Technetium 99m sulfur colloid in a volume of 0.1cc into the upper outer quadrant of the left breast, with emission and transmission imaging of the chest performed at 30 minutes. Lymphatics were visualized cranial to the injection site at 30 minutes; however, no discrete sentinel node was visualized at the time of imaging (Figs. 2A, 2B).
Figure 2.


39-year-old woman with advanced breast cancer and nonvisualized sentinel node. A. Emission image obtained 30 minutes after intradermal, peri-areolar administration of 110 μCi of filtered Technetium 99m sulfur colloid in a volume of 0.1cc into the upper outer quadrant of the left breast demonstrates migration of tracer in the lymphatics cranial to the injection site; however, no sentinel node is visualized at the time of imaging. B. Transmission image obtained 30 minutes post-injection also demonstrates migration of tracer in the lymphatics cranial to the injection site; however, no sentinel node is visualized.
Following lymphoscintigraphy, the Department of Nuclear Medicine was consulted because the surgeons could not detect the sentinel node with the gamma probe in the operating room. The gamma detector was recalibrated, and surgeons were still unable to localize the sentinel node. Upon visual inspection and palpation of the lymph nodes, the surgeon was able to macroscopically detect lymph-node disease. The patient underwent a total left mastectomy, and pathology revealed one of the three sentinel-node specimens positive for metastatic carcinoma and six of the seven left axillary lymph nodes positive for metastatic carcinoma.
Discussion
We hypothesize that although there was migration of the Technetium 99m sulfur colloid by 30 minutes, the tracer did not reach the sentinel node by the time of surgery due to advanced disease that obstructed the flow of lymphatics. Such alteration in lymphatic flow as a result of advanced disease has been described previously with regard to melanoma, penile cancer, and breast cancer (1, 2). In breast cancer, previous studies have shown that an increased number of axillary lymph nodes with metastatic involvement is associated with nonvisualization of lymph nodes during lymphoscintigraphy (3, 4).
Although we believe that the cause of nonvisualization of the sentinel node on lymphoscintigraphy for this patient was extensive disease obstructing the lymphatic system, many other factors can affect visualization of lymph nodes during lymphoscintigraphy. It has previously been reported that age of the patient and tumor size may influence sentinel node detection rates (4, 5). Furthermore, the radiopharmaceutical used, the dose of the pharmaceutical, the particle size of the pharmaceutical, and the injection-to-imaging time may all influence visualization of the sentinel node during lymphoscintigraphy (1). The site of pharmaceutical injection (whether intratumoral vs. extratumoral, intradermal vs. subdermal, or lateral vs. medial to a previous breast scar) can also affect visualization of the sentinel node during lymphoscintigraphy (6, 7, 8, 9, 10, 11, 12). Lastly, it is possible that a blue-dye injection in addition to Technetium 99m sulfur colloid and a gamma probe would have aided in detection of the sentinel node for this patient (13, 14, 15, 16). Use of SPECT imaging in addition to planar imaging may have also provided additional information for sentinel-node localization in this patient (2, 17).
Footnotes
Published: September 13, 2010
References
- 1.Kroon B.K. Non-visualization of sentinel lymph nodes in penile carcinoma. Eur J Nucl Med Mol Imaging. 2005;32(9):1096–1099. doi: 10.1007/s00259-005-1822-z. [PubMed] DOI: 10.1007/s00259-005-1822-z. [DOI] [PubMed] [Google Scholar]
- 2.Leijte J.A. Visualization of tumor blockage and rerouting of lymphatic drainage in penile cancer patients by use of SPECT/CT. J Nucl Med. 2009;50(3):364–367. doi: 10.2967/jnumed.108.059733. [PubMed] DOI: 108.059733. [DOI] [PubMed] [Google Scholar]
- 3.Brenot-Rossi I. Nonvisualization of axillary sentinel node during lymphoscintigraphy: is there a pathologic significance in breast cancer? J Nucl Med. 2003;44(8):1232–1237. [PubMed] [PubMed] [Google Scholar]
- 4.Lo Y.F. Clinical relevance of nonvisualized sentinel lymph nodes in unselected breast cancer patients during lymphoscintigraphy. Chang Gung Med J. 2005;28(6):378–386. [PubMed] DOI : 2806/280602 [pii] [PubMed] [Google Scholar]
- 5.Cortes Romera M. [Sentinel lymph node (SN) detection in patients with breast cancer. Influence of tumor size and age of the patient] Rev Esp Med Nucl. 2004;23(1):3–8. doi: 10.1016/s0212-6982(04)72238-7. [PubMed] DOI : 13056054 [pii] [DOI] [PubMed] [Google Scholar]
- 6.Bajen M.T. Subdermal re-injection: a method to increase surgical detection of the sentinel node in breast cancer without increasing the false-negative rate. Eur J Nucl Med Mol Imaging. 2006;33(3):338–343. doi: 10.1007/s00259-005-1931-8. [PubMed] DOI : 10.1007/s00259-005-1931-8. [DOI] [PubMed] [Google Scholar]
- 7.Coelho-Oliveira A. Identification of sentinel node in breast cancer: comparison between peritumoral and periareolar injection of the radiopharmaceutical contrast medium. J Exp Clin Cancer Res. 2004;23(4):567–572. [PubMed] [PubMed] [Google Scholar]
- 8.Imoto S. Mammary lymphoscintigraphy with various radiopharmaceuticals in breast cancer. Ann Nucl Med. 1999;13(5):325–329. doi: 10.1007/BF03164871. [PubMed] [DOI] [PubMed] [Google Scholar]
- 9.Jastrzebski T., Kopacz A., Lass P. Comparison of peritumoral and subareolar injection of Tc99m sulphur colloid and blue-dye for detection of the sentinel lymph node in breast cancer. Nucl Med Rev Cent East Eur. 2002;5(2):159–161. [PubMed] [PubMed] [Google Scholar]
- 10.Motomura K. Intradermal radioisotope injection is superior to subdermal injection for the identification of the sentinel node in breast cancer patients. J Surg Oncol. 2003;82(2):91–96. doi: 10.1002/jso.10200. [PubMed] discussion 96-7. DOI: 10.1002/jso.10200. [DOI] [PubMed] [Google Scholar]
- 11.Shimazu K. Comparison between periareolar and peritumoral injection of radiotracer for sentinel lymph node biopsy in patients with breast cancer. Surgery. 2002;131(3):277–286. doi: 10.1067/msy.2002.121378. [PubMed] DOI: S0039606002429406 [pii] [DOI] [PubMed] [Google Scholar]
- 12.Teal C.B. Nonvisualization of a sentinel lymph node on lymphoscintigraphy requiring reinjection of sulfur colloid in a patient with breast cancer. Clin Nucl Med. 2008;33(6):389–390. doi: 10.1097/RLU.0b013e318170d4b9. [PubMed] DOI: 10.1097/RLU.0b013e318170d4b9 00003072-200806000-00001 [pii] [DOI] [PubMed] [Google Scholar]
- 13.d'Eredita G. Effect of the use of vital dye, lymphoscintigraphy, or a combination for axillary lymphatic mapping and sentinel node biopsy in breast cancer. World J Surg. 2002;26(5):588–590. doi: 10.1007/s00268-001-0272-4. [PubMed] discussion 590-1. DOI: 10.1007/s00268-001-0272-4. [DOI] [PubMed] [Google Scholar]
- 14.Kraft O. [Problems of detection and biopsy examination of sentinel lymph nodes in malignant melanomas and in breast carcinoma] Cas Lek Cesk. 2004;143(6):396–400. [PubMed] discussion 400. [PubMed] [Google Scholar]
- 15.Pandey M., Deo S.V., Maharajan R. Fallacies of preoperative lymphoscintigraphy in detecting sentinel node in breast cancer. World J Surg Oncol. 2005;3(1):31. doi: 10.1186/1477-7819-3-31. [PubMed] 1477-7819-3-31 [pii] 10.1186/1477-7819-3-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sardi A. The benefit of using two techniques for sentinel lymph node mapping in breast cancer. Am Surg. 2002;68(1):24–28. [PubMed] [PubMed] [Google Scholar]
- 17.Lerman H. Lymphoscintigraphic sentinel node identification in patients with breast cancer: the role of SPECT-CT. Eur J Nucl Med Mol Imaging. 2006;33(3):329–337. doi: 10.1007/s00259-005-1927-4. [PubMed] DOI: 10.1007/s00259-005-1927-4. [DOI] [PubMed] [Google Scholar]


