Abstract
Background
The metabolic syndrome is associated with modest but independent and additive risk of new onset chronic kidney disease (CKD) in several studies. The purpose of our study was to determine whether metabolic syndrome and other cardiovascular risk factors (hyperuricaemia and smoking) are associated with the progression of IgA nephropathy (IgAN).
Methods
Two hundred and twenty three IgAN patients (107 with and 116 without metabolic syndrome) were examined. The primary renal end point was doubling of serum creatinine; secondary end points were reaching eGFR of ≤ 60 ml/min/1,73m2 or eGFR of ≤30 ml/min/1.73 m2, and end-stage renal disease, ESRD (the composite of serum creatinine ≥500 μmol/l, initiation of dialysis treatment or transplantation). The association of metabolic syndrome with renal end points was examined using the Kaplan-Meier method and Cox models.
Results
Metabolic syndrome established at the diagnosis or during follow-up of IgAN patients was significantly associated with the primary renal end point (unadjusted hazard ratio of doubling of serum creatinine, 95% confidence interval: 1.96 (1.17–1.33, p = 0.011). The association remained significant after adjustment for confounders: 1.70 (1.02–3.83, p = 0.040). Results were similar for secondary end points except ESRD which was not associated with the presence of metabolic syndrome. Hyperuricaemia and smoking were independent risk factors of progression. Survival curves stratified on metabolic syndrome status showed significant differences for the end points (p = 0.017–0.001) except for ESRD.
Conclusions
Early diagnosis and treatment of metabolic syndrome, hyperuricaemia and smoking may be an additional cost-effective strategy for preventing the progression of IgAN.
Keywords: cardiovascular risk factors, chronic kidney disease progression, end-stage renal disease, IgA nephropathy, metabolic syndrome
Introduction
The term metabolic syndrome is commonly used to describe the clustering of cardiovascular risk factors, namely central obesity, hypertension, impaired glucose metabolism and dyslipidaemia. Metabolic syndrome is found in over 25% of adults in the USA and in several other industrialized countries, and there appears to be an increasing prevalence in higher age groups [1]. Individuals with metabolic syndrome are at increased risk for cardiovascular diseases as well as cardiovascular and all-cause mortality [2].
The recent interest of nephrologists in metabolic syndrome increased after the publication of Chen et al. [3], demonstrating in a cross-sectional study that metabolic syndrome was associated with a 2.26-fold higher risk (1.68–4.03) of chronic kidney disease (CKD) in a sample representative of the US population. Other cross-sectional studies have also demonstrated a link between metabolic syndrome and CKD (see later). In the only longitudinal study, Kurella et al. [4] demonstrated a significantly increased risk of incident CKD in non-diabetic adults with metabolic syndrome. However, the effects of metabolic syndrome on the progression of CKD beyond the contribution of impaired glucose metabolism and hypertension are far from being established with certainty.
IgA nephropathy (IgAN) is the most common primary glomerulonephritis and is an important cause of end-stage renal disease (ESRD) worldwide [5]. Long-term observation in many countries has shown that IgAN causes ESRD in as many as 40% of patients within 20 years after diagnosis [6, 7]. Clinical presentation is usually with haematuria and with variable degrees of proteinuria. Pathologically, IgAN is characterized by the glomerular deposition of polymeric IgA1 mainly in the mesangium accompanied by mesangial hypercellularity, mesangial matrix expansion, and varying degrees of glomerulosclerosis and interstitial fibrosis. Adverse prognostic indicators include the presence of heavy proteinuria and hypertension, a significant reduction in glomerular filtration rate (GFR) at the time of renal biopsy and the extent of glomerulosclerosis and tubulointerstitial fibrosis on renal pathology [7, 8]. In addition to these known risk factors, other cardiovascular risk factors, such as hypertriglyceridaemia, hyperuricaemia, excessive body weight or cigarette smoking have also been associated with the progression of IgAN in recent studies [9–11]. However, there are no data about the prevalence of metabolic syndrome in IgAN patients, and there have not been any reports of an association between metabolic syndrome and the progression of IgAN.
The purpose of the present study was to determine whether there are differences in the progression of IgAN according to the presence of metabolic syndrome and other cardiovascular risk factors at the time of diagnosis and during the course of IgAN. We emphasized that the clustering of cardiovascular risk factors is associated with a more severe progression of IgAN.
Materials and methods
Study population
We examined 240 biopsy-proven IgAN patients with normal or mild to moderately decreased renal function (CKD Stage 1–3) at the time of the diagnosis of IgAN. All of the patients were diagnosed in the Nephrology Center, Medical Faculty, University of Pécs, Hungary and followed-up in 3- to 6-month intervals by the same two nephrologists, TK and JN. Seventeen patients were not included in the statistical analyses of this study because of insufficient clinical data at the time of the diagnosis of IgAN. Further exclusion criteria were: secondary IgAN cases, rapidly progressive crescentic patients, patients with nephrotic syndrome and immunosuppressive treatment. The analysed cohort included 223 patients.
Definition of metabolic syndrome
All IgAN patients were analysed to determine whether criteria for metabolic syndrome were met by using a modified NCEP ATP III (National Cholesterol Education Programme—Adult Treatment Panel III) definition of metabolic syndrome [12]. Metabolic syndrome was defined as any three or more of the following criteria: (i) fasting plasma glucose level of 5.6 mmol/L or higher or impaired glucose tolerance; (ii) triglyceride level of 1.7 mmol/L or higher or lipid-lowering drug treatment; (iii) high-density lipoprotein (HDL) cholesterol level <1.0 mmol/L for men and <1.3 mmol/L for women or drug treatment; (iv) body mass index (BMI) ≥30 kg/m2; (v) hypertension with blood pressure ≥130/85 mmHg or antihypertensive treatment.
Study measurements
Demographic, anthropometric and laboratory data as well as information about lifestyle habits were collected on all participants at the time of diagnosis and at each follow-up visit. Blood was collected by venepuncture after an overnight fast of at least 10 h at all follow-up examinations. The Central Laboratory of Medical Faculty, University of Pécs measured all serum chemistry levels in fresh samples with commercially available reagents. The glomerular filtration rate (eGFR; mL/min/1.73 m2) was estimated with the Chronic Kidney Disease Epidemiology Collaboration equation [13]. BMI was calculated as weight in kilograms divided by the square of the height in metres.
Definition of progression of IgAN
The primary renal outcome was the doubling of serum creatinine, secondary renal outcomes were the decrease of eGFR to ≤60 mL/min/1.73 m2, or to ≤30 mL/min/1.73 m2 or reaching ESRD (defined as the composite of a serum creatinine ≥500 µmol/L or the initiation of dialysis treatment or transplantation).
Statistical analysis
Data analysis was performed using the SPSS software program version 13.0 (SPSS Inc., Chicago, IL, USA). Continuous variables with normal distribution were expressed as mean ± standard deviation and were compared by using Student's t-tests. Variables with non-normal distribution were compared by the Mann–Whitney U-test, and categorical variables were expressed as percentage and compared by the χ2 test. The mean renal survival time until the selected end points was calculated using the Kaplan–Meier method. Differences between the calculated mean renal survival times were compared using the log-rank test. The effect of confounders was assessed by Cox regression analysis.
Confounders were determined a priori based on theoretical considerations and by examining baseline covariate associations with metabolic syndrome and with the renal end points [14]. Multivariate models were constructed with sequential adjustments for age and gender as well as for age, gender, uric acid, eGFR, smoking and angiotensin-converting enzyme inhibitors/angiotensin II receptor blocker (ACEis/ARB). A value of P < 0.05 was considered statistically significant.
Results
Baseline clinical data
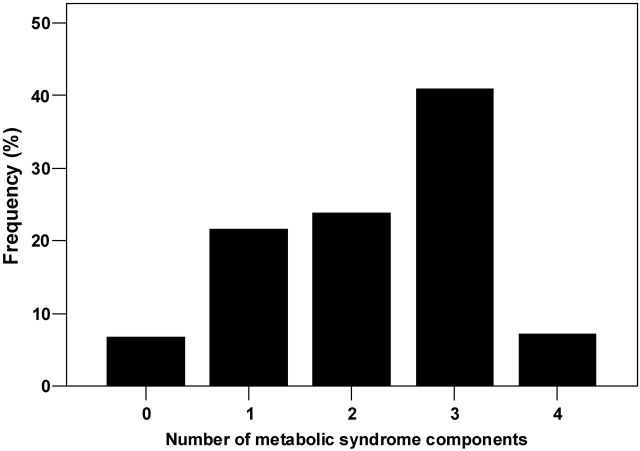
The mean age of the 223 participants included in the analytic cohort was 36.4 ± 13.0 years, 72% were male and 28% were female. Metabolic syndrome was already present in 17% of participants (38 patients) at the diagnosis of IgAN and was diagnosed de novo in a further 31% of participants (69 patients) during the follow-up period. Analysing all (n = 223) IgAN patients together at the end of the follow-up period, the prevalence of zero, one, two, three and four parameters of the metabolic syndrome was 15 (7%), 48 (22%), 53 (24%), 91 (41%) and 16 (7%), respectively (Figure 2). Sixty-eight (31%) patients were obese and impaired carbohydrate metabolism [impaired glucose tolerance (IGT), impaired fasting glucose (IFG) or diabetes mellitus] was present in 77 (35%) patients, HDL cholesterol was low in 108 (48%) patients, hypertriglyceridaemia was present in 133 (60%) patients and elevated blood pressure or antihypertensive treatment was present in 195 (87%) patients at the end of the follow-up period. Analysing together hypertriglyceridaemia, lower HDL cholesterol and statin treatment, 151 (68%) patients were dyslipidaemic.
Fig. 2.
Frequency of metabolic syndrome components at the end of follow-up.
Baseline characteristics of IgAN patients with and without metabolic syndrome are summarized in Table 1. There were no significant differences in the age, sex, follow-up time or number of smokers between the two groups. Patients with metabolic syndrome had higher uric acid levels in addition to the expected higher values for BMI, triglyceride, glucose and lower HDL cholesterol level that define metabolic syndrome. At the time of the diagnosis of IgAN, the eGFR of patients with metabolic syndrome was lower (73.6 ± 31.8 versus 82.2 ± 27.7 mL/min/1.73 m2 in patients without metabolic syndrome, P < 0.05). However, at the end of the follow-up period, the difference between the eGFR of the two groups was more substantial (46.8 ± 31.6 versus 67.4 ± 35.3 mL/min/1.73 m2, P < 0.001). The systolic and diastolic blood pressures of patients with metabolic syndrome were significantly higher (Table 1), and significantly more patients were treated with ACEi/ARB in the metabolic syndrome group (P < 0.001).
Table 1.
Baseline characteristics of patients with and without metabolic syndrome
| Metabolic syndrome (n = 107) | No metabolic syndrome (n = 116) | P-value | |
|---|---|---|---|
| Age | 37.9 ± 13.8 | 34.9 ± 12.2 | 0.089 |
| Follow-up (months) | 146.6 ± 112.5 | 146.1 ± 99.4 | 0.589 |
| Sex (M/F) | 81 (76%)/26 (24%) | 80 (69%)/36 (31%) | 0.296 |
| Parameters of metabolic syndrome | |||
| BMI (kg/m2) | 30.8 ± 4.8 | 24.9 ± 3.4 | <0.001 |
| Systolic BP (Hgmm) | 143 ± 20 | 136 ± 19 | 0.005 |
| Diastolic BP (Hgmm) | 89 ± 12 | 85 ± 12 | 0.014 |
| Hypertension (Y/N) | 105 (98%)/2 (2%) | 90 (78%)/26 (22%) | <0.001 |
| Triglyceride (mmol/L) | 2.18 ± 1.21 | 1.59 ± 1.55 | <0.001 |
| HDL (mmol/L) | 1.21 ± 0.48 | 1.39 ± 0.39 | <0.001 |
| Blood sugar (mmol/L) | 6.32 ± 1.44 | 5.10 ± 0.81 | <0.001 |
| Uric acid (mmol/L) | 390 ± 124 | 351 ± 118 | 0.006 |
| Smoking (Y/N) | 27 (25%)/79 (75%) | 30 (26%)/83 (74%) | 0.879 |
| Renal function | |||
| eGFR at the diagnosis (mL/min/1.73 m2) | 73.6 ± 31.8 | 82.2 ± 27.7 | <0.05 |
| eGFR at the end of follow-up (mL/min/ 1.73 m2) | 46.8 ± 31.6 | 67.4 ± 35.3 | <0.001 |
| Drugs | |||
| ACEi/ARB (Y/N) | 92 (86%)/15 (14%) | 73 (63%)/43 (37%) | <0.001 |
| Statins (Y/N) | 48 (45%)/59 (55%) | 19 (16%)/97 (84%) | <0.001 |
Data expressed as mean ± standard deviations and number of participants (for categorical variables).
BMI, body mass index; BP, blood pressure; HDL, high-density lipoprotein; eGFR, estimated glomerular filtration rate; ACEi, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker. Comparisons were made by t-tests or χ2 tests.
Association of metabolic syndrome with progression of IgAN
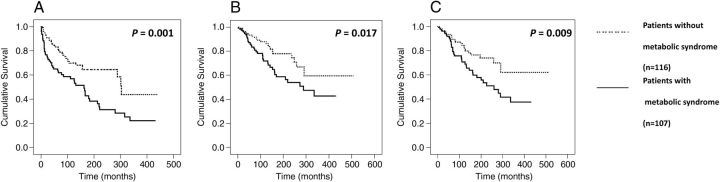
Survival curves stratified on metabolic syndrome status showed statistically significant differences in the time to reach three different end points for the renal outcome: the doubling of serum creatinine (P = 0.009, Figure 1A), eGFR ≤60 mL/min/1.73 m2 (P = 0.001, Figure 1B) and eGFR ≤30 mL/min/1.73 m2 (P = 0.017, Figure 1C). The difference in time to reach the composite end point of ESRD (defined as the composite of a serum creatinine ≥500 µmol/L or the initiation of dialysis treatment or transplantation) was not significant (P = 0.2).
Fig. 1.
Time to reach the different end points (Kaplan–Meier analysis). (A) Time to doubling of serum creatinine (months). (B) Time to reach eGFR ≤60 mL/min/1.73 m2 (months). (C) Time to reach eGFR ≤30 mL/min/1.73 m2 (months).
Metabolic syndrome was significantly associated with the progression of IgAN in unadjusted Cox models for three different renal end points eGFR ≤60 mL/min/1.73 m2, eGFR ≤30/mL/min/1.73 m2 and the doubling of serum creatinine (Table 2). The association remained significant after adjustment for confounders (Table 2). The association, however, was not significant for the end points of ESRD in neither unadjusted nor adjusted Cox models (Table 2). At the analysis of the effect of single traits of metabolic syndrome: obesity (yes/no, Y/N), hypertension (Y/N), dyslipidaemia (Y/N), dysglycaemia (Y/N) and complete metabolic syndrome on the prognosis of IgAN hypertension and complete metabolic syndrome were the two strongest influencing parameters (Table 3).
Table 2.
Crude and adjusted hazard ratios (95% CIs) of various renal end points associated with the presence of metabolic syndrome
| Doubling of serum creatinine | GFR |
Composite of ESRD | ||
|---|---|---|---|---|
| ≤60 mL/min/1.73 m2 | ≤30 mL/min/1.73 m2 | |||
| Unadjusted | 1.95 (1.16–3.28) | 2.04 (1.30–3.10) | 1.90 (1.11–3.24) | 1.46 (0.80–2.66) |
| P = 0.011 | P = 0.002 | P = 0.019 | P = 0.207 | |
| Adjusted for age, gender | 1.85 (1.10–3.11) | 2.15 (1.37–3.37) | 1.84 (1.07–3.14) | 1.41 (0.78–2.57) |
| P = 0.019 | P = 0.001 | P = 0.025 | P = 0.251 | |
| Adjusted for age, gender, uric acid, eGFR, smoking | 1.81 (1.07–3.08) | 2.04 (1.28–3.26) | 1.81 (1.05–3.13) | 1.36 (0.74–2.50) |
| P = 0.027 | P = 0.003 | P = 0.033 | P = 0.320 | |
| Adjusted for age, gender, uric acid, eGFR, smoking, ACEi/ARB | 1.70 (1.02–2.83) | 2.11 (1.31–3.40) | 1.64 (0.94–2.87) | 1.29 (0.69–2.41) |
| P = 0.040 | P = 0.002 | P = 0.081 | P = 0.419 | |
Table 3.
Crude hazard ratios (95% CI) of various end points associated with the presence of single metabolic syndrome components and metabolic syndrome itself
| Doubling of serum creatinine | GFR |
Composite of ESRD | ||
|---|---|---|---|---|
| ≤60 mL/min/1.73 m2 | ≤30 mL/min/1.73 m2 | |||
| Obesity (Y/N) | 0.95 (0.54–1.66) | 1.52 (1.05–2.20) | 1.29 (0.77–2.15) | 1.25 (0.67–2.32) |
| P = 0.852 | P = 0.026 | P = 0.334 | P = 0.484 | |
| Hypertension (Y/N) | 5.73 (1.40–23.46) | 4.50 (1.83–11.02) | 5.93 (1.45–24,24) | 3.89 (0.94–16.07) |
| P = 0.015 | P = 0.001 | P = 0.013 | P = 0.061 | |
| Dyslipidaemia (Y/N) | 1.65 (0.94–2.92) | 1.44 (0.97–2.14) | 1.64 (0.95–2.85) | 1.32 (0.69–2.53) |
| P = 0.082 | P = 0.073 | P = 0.077 | P = 0.395 | |
| Dysglicaemia (Y/N) | 0.67 (0.41–1.10) | 0.60 (0.42–0.86) | 0.67 (0.42–1.09) | 0.88 (0.49–1.60) |
| P = 0.116 | P = 0.005 | P = 0.110 | P = 0.680 | |
| Metabolic syndrome (Y/N) | 1.87 (1.12–3.12) | 2.04 (1.42–2.93) | 1.98 (1.20–3.25) | 1.470 (0.81–2.66) |
| P = 0.016 | P < 0.001 | P = 0.007 | P = 0.207 | |
In Cox regression analysis, higher uric acid level was also an independent risk factor for three different renal end points:
eGFR ≤60 mL/min/1.73 m2 [hazard ratio (HR) associated with a 1 mmol/L higher serum uric acid level: 1.003; 95% confidence interval (95% CI) 1.001–1.005].
eGFR ≤30 mL/min/1.73 m2 (HR 1.002; 95% CI 1.001–1.005) and
ESRD (HR 1.004; 95% CI 1.001–1.006).
Smoking was significantly associated with ESRD (HR 2.024; 95% CI 1.046–3.920).
Discussion
Our study showed that metabolic syndrome established at the time of diagnosis or during the follow-up of IgAN was significantly associated with the primary renal end point and remained significant after adjustment for confounders. Results were similar for the secondary end points except for ESRD. Hyperuricaemia was also an independent risk factor for all secondary end points, and smoking was an independent risk factor for ESRD. Survival curves stratified on metabolic syndrome status showed significant differences for the association with the various end points except for ESRD.
The criteria for metabolic syndrome diagnosis were set-up originally to identify those individuals most likely to develop cardiovascular diseases [15]. There is no doubt nowadays that the patients with metabolic syndrome are at significantly higher risk for CKD too, as summarized by a number of review articles and by the recent meta-analysis of Thomas et al. [16–22]. Most of the observational studies discussed in these papers found a significant association between metabolic syndrome and CKD. The odds ratios for CKD in the different studies were: 2.60 in the National Health And Nutrition Examination Survey III (NHANES III) database [3], 1.43 in the Atherosclerosis Risk in Communities study [4], 1.3 in American Indians [23], 1.54 in Japanese adults [24], 1.88 in the Tehran Lipid and Glucose Study [25], 1.64 in the Inter-Asia study [26], 1.31 in hypertensive African Americans [27], 1.31 in the Hong-Kong Diabetes Registry [28], 1.77 in Korean adults [29], 1.74 [30] and 1.42 [31] in Chinese adults as well as 1.30 in non-diabetic Taiwanese adults [32]. However, the majority of the studies were cross-sectional and, as such, unable to establish a cause-effect relationship between metabolic syndrome and the reduction in kidney function, and also unable to determine if metabolic syndrome is associated with longitudinal changes in kidney function. In this study, we detected a significant association between metabolic syndrome and the progressive loss of kidney function except in ESRD, suggesting a potential effect of metabolic syndrome on the early progression of IgAN. The lower eGFR level of patients with metabolic syndrome seen at the time of diagnosis of IgAN suggests a potential effect of metabolic syndrome on the incidence of the renal disease too. Our observation that metabolic syndrome did not associate with the progression of IgAN in the end-stage of IgAN is in agreement with the results of the study of Lee et al. [33] on CKD patients participating in the CKD prevention programme regulated by the Public Health Bureau of Taiwan.
Among the components of metabolic syndrome, diabetic and hypertensive injuries, the two major aetiologies of CKD worldwide, have been well studied and described. Concerning the association between IgAN and diabetes, Fliser et al. [34] published that insulin resistance and hyperinsulinaemia are already present in patients with incipient renal disease, among others in IgAN patients. In our present study, we found impaired glucose regulation (IGT, IFG or diabetes mellitus) in 77 (35%) patients. It is known that IgAN can also be superimposed on diabetic nephropathy or can be the only renal abnormality of diabetic patients. The association between IgAN and diabetes may not be coincidental, because the intraglomerular hypertension and hyperfiltration as well as biochemical alterations in the glomeruli of diabetic patients may facilitate the deposition of IgA1 immune complexes or aggregates. Furthermore, the abnormalities of the IgA immune system are common in Type 2 diabetes [35].
Hypertension is common in CKD patients and, similar to the general population, it predicts cardiovascular morbidity and mortality. Hypertensive CKD patients with metabolic syndrome have an excess cardiovascular risk. The relationship between blood pressure and mortality is U-shaped; low mean and diastolic blood pressure predicts early mortality [36]. As we already mentioned in the introduction, the progression in IgAN is more severe in the presence of hypertension and strict blood-pressure control portents renal protection in IgAN [37]. In our study, among the parameters of metabolic syndrome, hypertension had the greatest influence on the prognosis of IgAN.
Obesity has been associated with an increased risk for the incidence of CKD and for ESRD in several epidemiological studies [38–41]. In the examined populations, obesity as indicated by the elevated BMI was associated with decreased renal function and ESRD independent of the presence of hypertension and diabetes. Weight loss has a protective effect against the progression of CKD [40]. Higher BMI shows a seemingly paradoxical association with better survival in advanced CKD and in ESRD, which could be related to a better nutritional status in patients with elevated BMI [42].Concerning IgAN patients, obesity was a predictive factor not only for the development of hypertension, but also for chronic renal failure and obese patients have glomerular enlargement and ultrastructural modification of the glomerular basement membrane [9, 43].
Dyslipidaemia, in particular atherogenic dyslipidaemia (high triglyceride and low HDL cholesterol), has been recognized as an independent risk factor for the development and progression of CKD in observational studies and in meta-analyses [44, 45]. Furthermore, the progressive decline in renal function may engender inflammation and oxidative stress, which could in turn induce various metabolic alterations, such as insulin resistance and diabetes, elevation of arterial blood pressure and hypertriglyceridaemia, leading to potential vicious cycles. In the study of Syrjänen et al. [10], elevated triglyceride levels were associated with progressive IgAN.
Recent epidemiologic and experimental evidence suggests a role for hyperuricaemia not only as a marker of reduced kidney function but also as a causal risk factor for the development and progression of renal disease [46, 47]. Serum uric acid was a GFR-independent long-term predictor of acute and chronic renal insufficiency in the Jerusalem Lipid Research Clinic cohort study [48]. There is a close connection between hypertension and hyperuricaemia and at the re-evaluation of metabolic syndrome; Reaven [15] suggested to include hyperuricaemia among the criteria of metabolic syndrome. In the only previous study on IgAN patients, hyperuricaemia was found to be a predictor of poor prognosis similarly to our investigation [10].
An association between smoking and CKD has been found in various studies, including in lupus patients, polycystic kidney disease, primary glomerular diseases and diabetic nephropathy [49–52]. In the present study, smoking was significantly associated with the progression to ESRD, similar to the study by Yamamoto et al. [11] who, however, examined the smoking status only at time of diagnosis of IgAN.
Our study is notable for the well-characterized nature of the study population and the long follow-up of the patients by the same two nephrologists. Our study also has a number of limitations that have to be considered when interpreting the findings. This was a single-centre study hence the external validity of our findings may be limited. We lacked measurements of waist circumference as a better measure of abdominal obesity. Instead, we used BMI which is an acceptable alternative used in the World Health Organization classification of metabolic syndrome. This modification of the NCEP ATP III classification of metabolic syndrome we used was also used by Lea et al. examining the metabolic syndrome and the risk of progressive CKD in hypertensive African Americans [27]. Our study did not involve and discuss proteinuria as a predictor of the progression of CKD, because proteinuria could be a clinical characteristic of IgAN and also a consequence of metabolic syndrome.
This is the first study describing the frequent prevalence of metabolic syndrome at the time of diagnosis and during the follow-up of IgAN patients, and supporting the role of metabolic syndrome in the progression of IgAN. Hyperuricaemia and smoking seem to also be important risk factors of progression in IgAN. In conclusion, the early diagnosis and treatment of metabolic syndrome and hyperuricaemia, and cessation of smoking could be an added beneficial cost-effective strategy in the prevention of the progression of IgAN and in the prevention of the development of cardiovascular diseases, on the basis of the close connection between the progression of CKD and cardiovascular diseases.
Conflict of interest statement
None declared.
Acknowledgements
Part of this material was presented at the American Society of Nephrology Kidney Week 2011 November 10–13, Philadelphia, PA, USA. Dr Kovesdy is an employee of the US Department of Veterans Affairs. The opinions expressed in this paper are those of the authors’ and they do not necessarily reflect the opinions of the US Department of Veterans Affairs.
Funding. This study was supported by SROP-4.2.2/B-10/1/2010-0029 Supporting Scientific Training of Talented Youth at the University of Pécs.
References
- 1.Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 2.Lakka HM, Laaksonen DE, Lakka TA, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–2716. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 3.Chen J, Muntner P, Hamm LL, et al. The metabolic syndrome and chronic kidney disease in US adults. Ann Intern Med. 2004;140:167–174. doi: 10.7326/0003-4819-140-3-200402030-00007. [DOI] [PubMed] [Google Scholar]
- 4.Kurella M, Lo JC, Chertow GM. Metabolic syndrome and the risk for chronic kidney disease among nondiabetic adults. J Am Soc Nephrol. 2005;16:2134–2140. doi: 10.1681/ASN.2005010106. [DOI] [PubMed] [Google Scholar]
- 5.Schena FP, Pesce F. Epidemiology and ancestral difference. In: Lai KN, editor. Recent Advances in IgA Nephropathy. New Jersey: World Scientific Publishing Co.; 2009. pp. 9–20. [Google Scholar]
- 6.Berthoux CB, Mohey H. Clinical course of primary IgA nephropathy. In: Lai KN, editor. Recent Advances in IgA Nephropathy. New Jersey: World Scientific Publishing Co.; 2009. pp. 107–120. [Google Scholar]
- 7.Floege J, Feehally J. IgA nephropathy: recent developments. J Am Soc Nephrol. 2000;11:2395–2403. doi: 10.1681/ASN.V11122395. [DOI] [PubMed] [Google Scholar]
- 8.Barrat J, Feehally J. IgA nephropathy. J Am Soc Nephrol. 2005;16:2088–2097. doi: 10.1681/ASN.2005020134. [DOI] [PubMed] [Google Scholar]
- 9.Bonett F, Deplere C, Sassolas A, et al. Excessive body weight as a new independent risk factor for clinical and pathological progression in primary IgA nephritis. Am J Kid Dis. 2001;37:720–727. doi: 10.1016/s0272-6386(01)80120-7. [DOI] [PubMed] [Google Scholar]
- 10.Syrjänen J, Mustonen J, Pasternack A. Hypertriglyceridaemia and hyperuricaemia are risk factors for progression of IgA nephropathy. Nephrol Dial Transplant. 2000;15:34–42. doi: 10.1093/ndt/15.1.34. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto R, Nagasawa Y, Shoji T, et al. Cigarette smoking and progression of IgA nephropathy. Am J Kidney Dis. 2010;56:313–324. doi: 10.1053/j.ajkd.2010.02.351. [DOI] [PubMed] [Google Scholar]
- 12.Grundy SM, Cleeman JI, Daniels SR, et al. Diagnosis and management of the metabolic syndrome: American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 13.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thadhani R, Tonelli M. Cohort studies: marching forward. Clin J Am Soc Nephrol. 2006;1:1117–1123. doi: 10.2215/CJN.00080106. [DOI] [PubMed] [Google Scholar]
- 15.Reaven G. Metabolic syndrome: pathophysiology and implications for management of cardiovascular disease. Circulation. 2002;106:286–292. doi: 10.1161/01.cir.0000019884.36724.d9. [DOI] [PubMed] [Google Scholar]
- 16.Lastra G, Manrique C, McFarlane S, et al. Cardiometabolic syndrome and chronic kidney disease. Curr Diab Rep. 2006;6:207–212. doi: 10.1007/s11892-006-0036-5. [DOI] [PubMed] [Google Scholar]
- 17.Natali A, Pucci G, Boldrini B, et al. Metabolic syndrome: at the crossroads of cardiorenal risk. J Nephrol. 2009;22:29–38. [PubMed] [Google Scholar]
- 18.Zoccali C. Overweight, obesity and metabolic alterations in chronic kidney disease. Contributions Soc Biol Med Sci MASA. 2009;30:17–31. [PubMed] [Google Scholar]
- 19.Locatelli F, Pozzoni P, Del Vecchio L. Renal manifestations in the metabolic syndrome. J Am Soc Nephrol. 2006;17:S81–S85. doi: 10.1681/ASN.2005121332. [DOI] [PubMed] [Google Scholar]
- 20.Ritz E. Metabolic syndrome and kidney disease. Blood Purif. 2008;26:59–62. doi: 10.1159/000110566. [DOI] [PubMed] [Google Scholar]
- 21.Mallamaci F, Leonardis D, Tripepi G. The metabolic syndrome and chronic kidney disease epidemics: severing the link. Port J Nephrol Hypert. 2007;21:71–76. [Google Scholar]
- 22.Thomas G, Sehgal AR, Kashyap SR, et al. Metabolic syndrome and kidney disease: a systematic review and meta-analysis. Clin J Am Soc Nephrol. 2011;6:2364–2373. doi: 10.2215/CJN.02180311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lucove J, Vupputuri S, Heiss G, et al. Metabolic syndrome and the development of CKD in American Indians: the Strong Heart Study. Am J Kidney Dis. 2008;51:21–28. doi: 10.1053/j.ajkd.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 24.Tanaka H, Shiohira Y, Uezu Y, et al. Metabolic syndrome and chronic kidney disease in Okinawa, Japan. Kidney Int. 2006;69:369–374. doi: 10.1038/sj.ki.5000050. [DOI] [PubMed] [Google Scholar]
- 25.Rashidi A, Ghanbarian A, Azizi F. Are patients who have metabolic syndrome without diabetes at risk for developing chronic kidney disease? Evidence based on data from a large cohort screening population. Clin J Am Soc Nephrol. 2007;2:976–983. doi: 10.2215/CJN.01020207. [DOI] [PubMed] [Google Scholar]
- 26.Chen J, Gu D, Chen C-S, et al. Association between the metabolic syndrome and chronic kidney disease in Chinese adults. Nephrol Dial Transplant. 2007;22:1100–1106. doi: 10.1093/ndt/gfl759. [DOI] [PubMed] [Google Scholar]
- 27.Lea J, Cheek D, Thornley-Brown D, et al. Metabolic syndrome, proteinuria, and the risk of progressive CKD in hypertensive African Americans. Am J Kidney Dis. 2008;51:732–740. doi: 10.1053/j.ajkd.2008.01.013. [DOI] [PubMed] [Google Scholar]
- 28.Luk AO, So WY, Ma RC, et al. Metabolic syndrome predicts new onset of chronic kidney disease in 5,829 patients with type 2 diabetes: a 5-year prospective analysis of the Hong Kong Diabetes Registry. Diabetes Care. 2008;31:2357–2361. doi: 10.2337/dc08-0971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jang SY, Kim IH, Ju EY, et al. Chronic kidney disease and metabolic syndrome in a general Korean population: the Third Korea National Health and Nutrition Examination Survey (KNHANES III) Study. J Public Health. 2010;32:538–546. doi: 10.1093/pubmed/fdp127. [DOI] [PubMed] [Google Scholar]
- 30.Zhang LX, Zuo L, Wang F, et al. Metabolic syndrome and chronic kidney disease in a Chinese population aged 40 years and older. Mayo Clin Proc. 2007;82:822–827. doi: 10.4065/82.7.822. [DOI] [PubMed] [Google Scholar]
- 31.Yang T, Chu CH, Hsu CH, et al. Impact of metabolic syndrome on the incidence of chronic kidney disease: a Chinese cohort study. Nephrology. 2012;17:532–538. doi: 10.1111/j.1440-1797.2012.01607.x. [DOI] [PubMed] [Google Scholar]
- 32.Sun F, Tao Q, Zhan S. Metabolic syndrome and the development of chronic kidney disease among 118 924 non-diabetic Taiwanese in a retrospective cohort. Nephrology. 2010;15:84–92. doi: 10.1111/j.1440-1797.2009.01150.x. [DOI] [PubMed] [Google Scholar]
- 33.Lee CC, Sun CY, Wu IW, et al. Metabolic syndrome loses its predictive power in late-stage chronic kidney disease progression — a paradoxical phenomenon. Clin Nephrol. 2011;75:141–149. doi: 10.5414/cnp75141. [DOI] [PubMed] [Google Scholar]
- 34.Fliser D, Pacini G, Engelleiter R, et al. Insulin resistance and hyperinsulinemia are already present in patients with incipient renal disease. Kidney Int. 1998;53:1343–1347. doi: 10.1046/j.1523-1755.1998.00898.x. [DOI] [PubMed] [Google Scholar]
- 35.Nagy J, Kovacs T. Special clinical syndromes. In: Lai KN, editor. Recent Advances in IgA Nephropathy. New Jersey: World Scientific Publishing Co.; 2009. pp. 121–138. [Google Scholar]
- 36.Kövesdy CP, Trivedi BK, Kalantar-Zadeh K, et al. Association of low blood pressure with increased mortality in patients with moderate to severe chronic kidney disease. Nephrol Dial Transplant. 2006;21:1257–1262. doi: 10.1093/ndt/gfk057. [DOI] [PubMed] [Google Scholar]
- 37.Nagy J, Kovács T, Wittmann I. Renal protection in IgA nephropathy requires strict blood pressure control. Nephrol Dial Transplant. 2005;20:1533–1539. doi: 10.1093/ndt/gfh920. [DOI] [PubMed] [Google Scholar]
- 38.Kwan BCH, Murtaugh MA, Beddhu S. Associations of body size with metabolic syndrome and mortality in moderate chronic kidney disease. Clin J Am Nephrol. 2007;2:992–998. doi: 10.2215/CJN.04221206. [DOI] [PubMed] [Google Scholar]
- 39.Kopple JD, Feroze U. The effect of obesity on chronic kidney disease. J Ren Nutr. 2011;21:66–71. doi: 10.1053/j.jrn.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 40.Hsu C-Y, McCulloch CE, Iribarren C, et al. Body mass index and risk for end-stage renal disease. Ann Intern Med. 2006;144:21–28. doi: 10.7326/0003-4819-144-1-200601030-00006. [DOI] [PubMed] [Google Scholar]
- 41.Madero M, Sarnak MJ, Wang Y, et al. Body mass index and mortality in CKD. Am J Kidney Dis. 2007;3:404–411. doi: 10.1053/j.ajkd.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 42.Kovesdy CP, Anderson JE, Kalantar-Zadeh K. Paradoxical association between body mass index and mortality in men with CKD not yet on dialysis. Am J Kid Dis. 2007;49:581–591. doi: 10.1053/j.ajkd.2007.02.277. [DOI] [PubMed] [Google Scholar]
- 43.Tanaka M, Yamada S, Iwasaki Y, et al. Impact of obesity on IgA nephropathy: comparative ultrastructural study between obese and non-obese patients. Nephron Clin Pract. 2009;112:71–78. doi: 10.1159/000213084. [DOI] [PubMed] [Google Scholar]
- 44.Muntner J, Coresh J, Smith J, et al. Plasma lipids and risk of developing renal dysfunction: the atherosclerosis risk in community study. Kidney Int. 2000;58:293–301. doi: 10.1046/j.1523-1755.2000.00165.x. [DOI] [PubMed] [Google Scholar]
- 45.Fried F, Orchard TJ, Kasiske BL. Effect of lipid reduction on the progression of renal disease: a metaanalysis. Kidney Int. 2001;59:260–269. doi: 10.1046/j.1523-1755.2001.00487.x. [DOI] [PubMed] [Google Scholar]
- 46.Feig ID. Uric acid: a novel mediator and marker of risk in chronic kidney disease. Curr Opin Nephrol Hypertens. 2009;18:526–530. doi: 10.1097/MNH.0b013e328330d9d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Obermayr RP, Temml C, Gutjahr G, et al. Elevated uric acid increases the risk for kidney disease. J Am Soc Nephrol. 2008;19:2407–2413. doi: 10.1681/ASN.2008010080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ben-Dov IZ, Kark JD. Serum uric acid is a GFR-independent long-term predictor of acute and chronic renal insufficiency: the Jerusalem Lipid Research Clinic cohort study. Nephrol Dial Transplant. 2011;26:2558–2566. doi: 10.1093/ndt/gfq740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hallan IS, Orth RS. Smoking is a risk factor in the progression to kidney failure. Kidney Int. 2011;80:516–523. doi: 10.1038/ki.2011.157. [DOI] [PubMed] [Google Scholar]
- 50.Yacuob R, Habib H, Lahdo A, et al. Association between smoking and chronic kidney disease: a case control study. BMC Public Health. 2010;10:731–736. doi: 10.1186/1471-2458-10-731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stegmayr BG. A study of patients with diabetes mellitus (type 1) and end-stage renal failure: tobacco usage may increase risk of nephropathy and death. J Intern Med. 1990;228:121–124. doi: 10.1111/j.1365-2796.1990.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 52.Ward MM, Studenski S. Clinical prognostic factors in lupus nephritis: the importance of hypertension and smoking. Arch Intern Med. 1992;152:2082–2088. [PubMed] [Google Scholar]