Abstract
Background
Health care violence is a significant worldwide problem with negative consequences on both the safety and well-being of health care workers as well as workplace activities. Reports examining health care violence in Saudi Arabia are limited and the results are conflicting.
Objective
To estimate the prevalence and determine the demographic and occupational characteristics associated with workplace violence in primary care centers in Riyadh, Saudi Arabia.
Methods
A cross-sectional study included 270 health care workers in 12 family medicine centers in Riyadh during November and December 2014. A structured self-administered questionnaire was used to estimate the frequency, timing, causes, reactions, and consequences of workplace violence plus participants’ demographic and occupational data.
Results
A total 123 health care workers (45.6%) experienced some kind of violence over 12 months prior to the study. These included physical (6.5%) and nonphysical violence (99.2%), including verbal violence (94.3%) and intimidation (22.0%). Offenders were patients (71.5%) in the majority of cases, companions (20.3%), or both (3.3%). Almost half (48.0%) of health care workers who experienced violence did nothing, 38.2% actively reported the event, and 13.8% consulted a colleague. A significant association of workplace violence was found with working multiple shifts, evening or night shift, and lack of an encouraging environment to report violence.
Conclusion
Workplace violence is still a significant problem in primary care centers. The high frequency of violence together with underreporting may indicate the inefficiency of the current safety program. More safety programs and training activities for health care workers, efficient reporting system, and zero tolerance policies need to be implemented to minimize workplace violence against health workers.
Keywords: health care workers, violence, primary health care, Saudi Arabia, workplace violence, assaults
Introduction
Working in health care is a potentially violent occupation.1 Providing care services at primary care centers require health care workers (HCWs) to closely interact with patients and their families, often under difficult circumstances.2 Patients and their relatives may behave aggressively or violently either due to their medical conditions, side effects of their medications, or dissatisfaction with the services provided by the health care facilities Patients and their families may also have a history of violent behavior or feel frustrated and angry as a result of the patient’s circumstances.2
There was no consistent definition of workplace violence found in the literature, with variable definitions used in different studies.3 The World Health Organization (WHO) defined violence as: “The intentional use of physical force or power, threatened or actual, against another person or against oneself or a group of people that results in or has a high likelihood of resulting in injury, death, psychological harm, mal-development or deprivation.”4 The National Institute for Occupational Safety and Health of the US Centers for Disease Control and Prevention defined workplace violence as: “violent acts (including physical assault and threats of assault) directed toward persons at work or on duty.”5 Adapted from the European Commission, the WHO defined workplace violence as incidents where staff are abused, threatened, or assaulted in circumstances related to their work, including commuting to and from work, and involving an explicit or implicit challenge to their safety, well-being, or health.6
According to WHO, violence appears as physical violence or psychological violence in different forms, which may often overlap.6,7 Physical violence was defined as the use of physical force against another person that results in physical, sexual, or psychological harm. It may include beating, kicking, slapping, stabbing, shooting, pushing, biting, and pinching. Psychological violence was defined as intentional use of power, including verbal abuse, threats, intimidation, bullying/mobbing, and harassment.4,6,7 Verbal violence or abuse was defined as excessive use of language to undermine someone’s dignity and security through insults or humiliation.3,8 The National Institute for Occupational Safety and Health defined threats as the expressions of intent to cause harm, including verbal threats, threatening body language, and written threats.5 Intimidation is a intentional form of psychological violence that causes a normal person to experience fear or fright.2
Several studies worldwide examined the incidence and/or prevalence of violence against HCWs. However, differences in study methodology, definition of violence, duration covered, and type of HCWs examined make comparing rates from different studies difficult or inaccurate. It was reported that violence-related claims per person, per year, from the health care sector is higher than other occupations known for high violence incidences, such as individuals working at hotels, restaurants, educational institutions, and governmental services.2 In a workplace violence survey done in 2008 involving 1,377 HCWs from all regions of the US, 74% of HCWs reported that workplace violence is experienced occasionally, 19% frequently, and 2% always.9 In a large, cross-sectional survey of 11,095 HCWs in 19 hospitals in Japan, 36% experienced workplace violence by patients or their relatives in the past year.10 In another large study done in 21 public hospitals across two Australian states between 2004 and 2006, 38% of nurses experienced emotional abuse during the previous five shifts. Additionally, 21% reported threat of violence and 14% experienced physical violence.11
The frequency of health care violence is not similar in all locations. The risk was reported to be highest in emergency departments, psychiatric units, geriatric units, and acute care units.3,5,12
A number of studies in the Arabic region examined the workplace violence of HCWs. In a cross-sectional study done in 2010 among 970 nurses working in four hospitals and 12 primary health care centers in Egypt, 28% reported at least one type of violence.13 In another cross-sectional study done in 2011 among 227 nurses working in emergency departments in 12 provinces of Jordan, it was shown that 76% of the nurses were exposed to at least one type of violence.14 In a similar study among 240 HCWs in five public hospitals in Palestine, it was shown that 80% of the HCWs were exposed to at least one type of violence.15
There are many factors that increased the risk of workplace violence against HCWs. Those factors are either related to offenders, coworkers, or the workplace environment.1,5,10 The significant factors for patients reported in different studies and review reports included: mental health disorders such as schizophrenia, anxiety, acute stress reaction, dementia, suicidal ideation, alcohol and drug intoxication, male sex, older age, being a victim of violence, and having access to firearms. Factors related to HCWs included serving volatile patients in emergency departments and psychiatric units, understaffed working conditions (especially during meal times and visiting hours), working alone, and long working hours. However, there were conflicting findings for age, sex, and other demographic characteristics and conflicting findings for the type of job, with a likely higher risk factor for nurses. Factors related to the workplace included long waiting times for getting service, overcrowded conditions, uncomfortable waiting rooms, poor environmental design, and poorly lit corridors, rooms, parking lots, and other areas; and unrestricted movement of the public, inadequate security and lack of surveillance video cameras, lack of staff training, and lack of policies for preventing and managing violence.
Data examining the incidence and prevalence of health care violence in Saudi Arabia are very limited. A cross-sectional study among 258 HCWs working in two public hospitals in Riyadh during 2011 showed that 67% of HCWs experienced some sort of violence in the prior 12 months: 95% verbal, 12% physical, or 11% both.16 In the study by Algwaiz et al16 cited earlier, violence was defined as any aggressive behavior against health workers, including physical assault or verbal aggression, as reported by the respondents themselves. In another study done among primary HCWs in Al-Hassa, 28% of the 1,091 primary HCWs who completed a self-administered questionnaire experienced at least one violent event during the past year.17 The type of violence experienced was psychological in 89% of the events, physical in 5% of the events, and both emotional and physical in 6% of the events. In the study by El-Gilany et al,17 cited earlier, violence was defined according to the WHO definition. The authors of the earlier two studies concluded that the results are difficult to generalize to other hospitals in Saudi Arabia as they were self-reported data done in a single sector of HCWs.16,17 Additionally, few studies examined the independent risk factors for health care violence, including socio-demographics, and occupational factors of HCWs in primary care centers.
Study objectives
The current study was done to estimate the prevalence of workplace violence among primary HCWs in Family and Community centers of Prince Sultan Military Medical City, Riyadh, Saudi Arabia, and determine possible association with demographic and occupational characteristics of participants.
Subjects and methods
This is a cross-sectional study conducted during November and December 2014 in four Family and Community centers at Prince Sultan Military Medical City, in Riyadh, Saudi Arabia. HCWs working at the four centers for at least 1 year were asked to answer a self-administered questionnaire.
Sample size estimation
Considering previous data examining the frequency of health care-related violence locally and internationally and assuming the level of violence among our HCWs to be 50%, for 95% confidence interval (CI), the sample size was estimated to be 267, and increased to 300 to ensure a good response rate. Personal invitations were sent to the study population after they were obtained through a convenience sampling.
Data collection
A structured self-administered questionnaire was developed by the researcher based on previous similar literature16,17,20 and International Labour Office/International Council of Nurses/WHO/Public Services International questionnaire.6 The study questionnaire had two main sections consisting of demographic characteristics (age, sex, marital status, occupation, and nationality) and occupational characteristics, including violence-related characteristics (see Tables 1–3).
Table 1.
Demographic characteristics of the primary HCWs in Family and Community Centers, PSMMC, Riyadh (2014)
| Characteristics | Number | % |
|---|---|---|
| Sex | ||
| Male | 110 | 40.9 |
| Female | 159 | 59.1 |
| Age | ||
| Mean ± standard deviation | 35.9±8.9 | |
| Age group | ||
| ≤30 | 102 | 38.6 |
| 31–40 | 95 | 36.0 |
| >40 | 67 | 25.4 |
| Marital status | ||
| Single | 74 | 27.5 |
| Married | 179 | 66.5 |
| Divorced/widow | 16 | 5.9 |
| Occupation | ||
| Doctor | 133 | 49.3 |
| Nurse | 75 | 27.8 |
| Other HCWs | 62 | 23.0 |
| Pharmacist | 21 | 7.8 |
| Technician | 15 | 5.6 |
| Clerk | 19 | 7.0 |
| Others | 7 | 2.6 |
| Nationality | ||
| Saudi | 163 | 60.4 |
| Non-Saudi | 107 | 39.6 |
| Filipino | 15 | 32.6 |
| Egyptian | 10 | 21.7 |
| Sudanese | 6 | 13.0 |
| Jordanian | 4 | 8.7 |
| Syrian | 4 | 8.7 |
| Others | 7 | 15.2 |
Abbreviations: HCW, health care worker; PSMMC, Prince Sultan Medical Military City.
Table 2.
Occupational characteristics of the primary health care workers in Family and Community Centers, PSMMC, Riyadh (2014)
| Characteristics | Number | % |
|---|---|---|
| Working multiple shifts | ||
| No | 195 | 72.5 |
| Yes | 74 | 27.5 |
| Shift time worked | ||
| Morning shift | 258 | 95.6 |
| Nonmorning shift | 78 | 28.9 |
| Evening shift | 75 | 27.8 |
| Night shift | 17 | 6.3 |
| Number of coworkers in the same working place | ||
| 1–5 | 92 | 34.2 |
| 6–10 | 80 | 29.7 |
| >10 | 97 | 36.1 |
| Sex of served patient | ||
| Male | 20 | 7.4 |
| Female | 45 | 16.7 |
| Both males and females | 204 | 75.8 |
| Presence of encouragement to report a violence event | ||
| No | 193 | 72.0 |
| Yes | 67 | 25.0 |
| I do not know | 8 | 3.0 |
| Availability of a violence reporting system | ||
| No | 61 | 22.8 |
| Yes | 157 | 58.8 |
| I do not know | 49 | 18.4 |
| In case of system, awareness about how to use | ||
| No | 46 | 29.3 |
| Yes | 110 | 70.1 |
| I do not know | 1 | 0.6 |
| In case of system, the system is effective | ||
| No | 38 | 24.7 |
| Yes | 108 | 70.1 |
| I do not know | 8 | 5.2 |
Abbreviation: PSMMC, Prince Sultan Medical Military City.
Table 3.
The characteristics of violence experienced over the last 12 months by primary HCWs in Family and Community Centers, PSMMC, Riyadh (2014)
| Characteristics | Number | % |
|---|---|---|
| Time of violent event | ||
| Morning shift | 86 | 70.5 |
| Evening/night shift | 31 | 25.4 |
| Both | 5 | 4.1 |
| Place of violent event | ||
| Inside workplace | 121 | 99.2 |
| Outside workplace | 0 | 0.0 |
| Both | 1 | 0.8 |
| Frequency of violent event | ||
| Once or more a month | 72 | 59.5 |
| Less than once a month | 49 | 40.5 |
| Identity of offender | ||
| Patient | 88 | 71.5 |
| Companion | 25 | 20.3 |
| Both patient and companion | 4 | 3.3 |
| HCWs | 6 | 4.9 |
| Age of offender | ||
| ≤20 | 9 | 7.3 |
| 21–45 | 75 | 61.0 |
| ≥46 | 39 | 31.7 |
| Sex of the offender | ||
| Male | 81 | 65.9 |
| Female | 37 | 30.1 |
| Both male and female | 5 | 4.1 |
| Cause of violence | ||
| Lack of penalty for offender | 61 | 49.6 |
| Misunderstanding | 50 | 40.7 |
| Unmet service demand | 45 | 36.6 |
| Overcrowding | 41 | 33.3 |
| Long waiting time | 40 | 32.5 |
| Reaction to injury | 1 | 0.8 |
| Others | 7 | 5.7 |
| Violent event was preventable | ||
| No | 20 | 16.3 |
| Yes | 102 | 82.9 |
| I don’t know | 1 | 0.8 |
Abbreviations: HCW, health care worker; PSMMC, Prince Sultan Medical Military City.
The study outcome was the frequency of health care-related violence. The current study used the definition of violence based on the WHO and US Centers for Disease Control and Prevention definitions.4,5
With regard to validation of the questionnaire, experts in family and community medicine as well as researchers in the same field reviewed it. The questionnaire was slightly modified based on the expert suggestions. Then, the questionnaire was piloted on 20 volunteer HCWs with very positive feedback. The questionnaire was readministered after a week to the same HCW of the pilot study to check test–retest reliability. The correlation coefficient of violence questions from the two administrations was 0.95. Two different bilingual translators translated the questionnaire forward and backward.
Ethical considerations
The Research and Ethics Committee at Prince Sultan Military Medical City approved the study before starting data collection. All data were kept confidential and used only for research. Written informed consent was deemed not necessary for this study as no patients were involved.
Statistical procedures
All categorical variables were presented as frequencies and percentages, while continuous variables were presented as mean and standard deviations. The frequency of violence was calculated by dividing the number of those who answered yes to the question “Did you have any kind of workplace violence over the past 12 months?” by the total number of HCWs who answered the questions. To detect demographic and occupational characteristics associated with workplace violence, chi-square or Fisher’s exact test, as appropriate, was used for categorical variables and Student’s t-test was used for continuous variables. Logistic regression analysis was run using violence as outcome with demographic and occupational characteristics as predictors in order to detect factors independently associated with workplace violence. All P-values were two-tailed. A P-value <0.05 was considered significant. SPSS software (release 16.0, SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
Results
A total of 270 primary HCWs were included in the current analysis. The demographic and characteristics of participants are shown in Tables 1 and 2, respectively. The majority (72.0%) of HCWs reported a lack of an encouraging environment for reporting violent events in their workplace. The majority (58.8%) of HCWs reported availability of a violence reporting system at their workplace. The rest either reported lack of such a system (22.8%) or that they did not know if such a system existed (18.4%). Among those who reported the availability of a violence reporting system at their workplace (N=157), 70.1% know how to use the reporting system and 70.1% believed that the system was effective. A total of 123 HCWs (45.6%) experienced some kind of violence over the 12 months prior to the study (Figure 1). As shown in Figure 2, the reported violence included physical (6.5%), nonphysical (99.2%), verbal (94.3%), and intimidation (22.0%). The majority (79.7%) of those who experienced violence experienced a single type of violence, while 20.3% experienced more than one type of violence (Figure 3). The characteristics of violence experienced by HCWs are shown in Table 3. Most (70.5%) violent events occurred during morning shifts, while 25.4% occurred in evening or night shifts and 4.1% in both morning and nonmorning shifts. Almost all (99.2%) of the violent events occurred inside the workplace. The majority (59.5%) of violent events occurred at a rate of one or more a month with 40.5% occurring at a rate of less than once a month. In a majority of the cases (71.5%), patients were the offenders with companions being 20.3% and 3.3% were both. However, 4.9% of the offenders were other HCWs. The age of the majority (61.0%) of offenders was between 21 and 45 years old, with 31.7% of them ≥46 years old and 7.3% ≤20 years old. Most (65.9%) of the offenders were male, with 30.1% female, and in 4.1% of cases, both a male and a female committed the violent act. HCWs who experienced violence reported that the violence was caused by lack of penalty for the offender (49.6%), misunderstandings (40.7%), unmet service demands (36.6%), overcrowding (33.3%), long waiting times (32.5%), reactions to injury (0.8%), and other causes (5.7%). The majority (82.9%) of the HCWs believed that the violent event was preventable. The reactions of HCWs to violence and its consequences are shown in Table 4. Almost half (48.0%) of the HCWs who experienced violence did nothing. On the other hand, 38.2% of the HCWs actively reported the violence they experienced to their supervisors (30.9%), to police (4.9%), or requested to move from the workplace. Approximately 14.5% of HCWs who experienced violence passively reacted to the violence by consulting a colleague or friend (13.8%) or discussing the violence with the offender and resolving the conflict (0.8%). Among those who did not report the violence (N=77), the reasons for not reporting included the belief that reporting is not an efficient reaction (69.4%), fear of losing their jobs (12.5%), reason unknown (11.1%), and other causes (6.9%). The violent events ended with the following consequences: nothing changed (56.6%), reduction in work performance (31.1%), feeling ashamed or guilty (4.9%), feeling sad or stressed (2.5%), and other consequences (4.9%). The majority of HCWs who experienced violence were either unsatisfied (45.9%) or very unsatisfied (25.4%) with the way the violent event was managed. Comparisons of demographic and occupational characteristics between HCWs who reported violence and those who did not report violence are shown in Tables 5 and 6, respectively. Occupation was significantly associated with violence (P=0.045), with violence being highest for clerks (68.4%) followed by pharmacists (61.9%), doctors (44.4%), technicians (40.0%), and finally nurses (36.0%).
Figure 1.
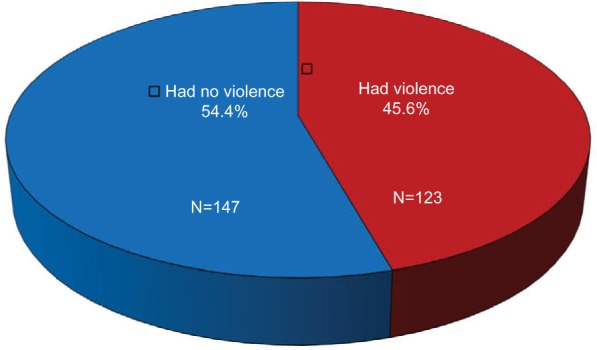
Frequency of having any kind of violence over the last 12 months among primary health care workers in Family and Community Center, PSMMC, Riyadh (2014).
Abbreviation: PSMMC, Prince Sultan Medical Military City.
Figure 2.
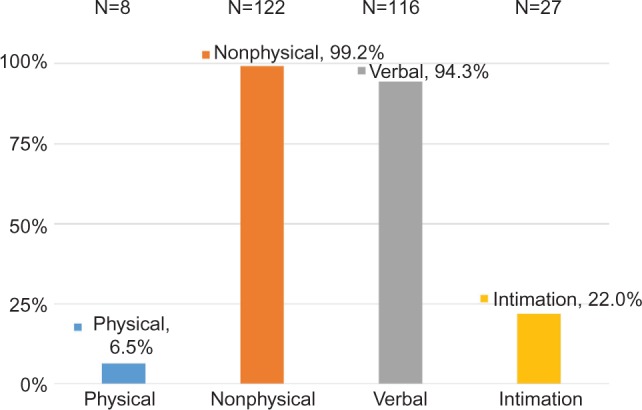
Type of violence experienced over the last 12 months by primary health care workers in Family and Community Centers, PSMMC, Riyadh (2014).
Abbreviation: PSMMC, Prince Sultan Medical Military City.
Figure 3.
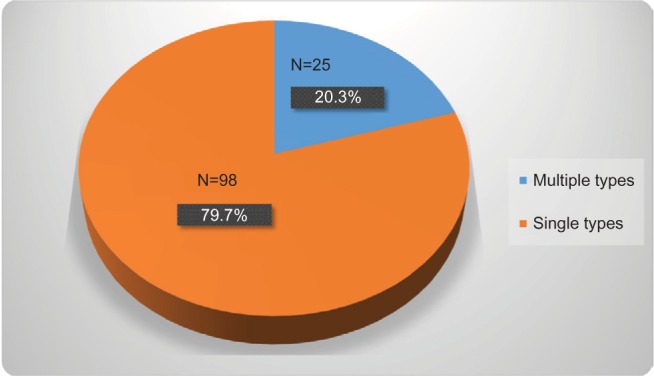
Multiplicity of violence types experienced over the last 12 months by primary health care workers in Family and Community Centers, PSMMC, Riyadh (2014).
Abbreviation: PSMMC, Prince Sultan Medical Military City.
Table 4.
Reaction to and consequences of violence experienced over the last 12 months by primary health care workers in Family and Community Centers, PSMMC, Riyadh (2014)
| Reaction to and consequences of the violent event | Number | % |
|---|---|---|
| Reaction to the violent event | ||
| Nothing | 59 | 48.0 |
| Passive reporting/reaction | 18 | 14.5 |
| Consult colleague or friend | 17 | 13.8 |
| Discuss with offender and solve it | 1 | 0.8 |
| Active reporting/reaction | 47 | 38.2 |
| Report to supervisor | 38 | 30.9 |
| Report to police or security | 6 | 4.9 |
| Request to move from workplace | 3 | 2.4 |
| Reason for not reporting the violent event | ||
| Not an efficient reaction | 50 | 69.4 |
| Fear from losing my job | 9 | 12.5 |
| Do not know | 8 | 11.1 |
| Others | 5 | 6.9 |
| Felt ashamed or guilty | 1 | 1.4 |
| Fear from revenge | 1 | 1.4 |
| Consider the patient situation | 1 | 1.4 |
| Patient did apologize | 1 | 1.4 |
| Choose to ignore | 1 | 1.4 |
| Consequences of the violent event | ||
| Nothing | 69 | 56.6 |
| Reduced my work performance | 38 | 31.1 |
| Felt ashamed or guilty | 6 | 4.9 |
| Felt sad or stressed | 3 | 2.5 |
| I was punished | 1 | 0.8 |
| Offender was punished | 1 | 0.8 |
| I was injured and needed medical care | 1 | 0.8 |
| Others | 3 | 2.5 |
| Level of satisfaction with consequences | ||
| Very satisfied | 1 | 0.8 |
| Satisfied | 5 | 4.1 |
| Neutral | 29 | 23.8 |
| Unsatisfied | 56 | 45.9 |
| Very unsatisfied | 31 | 25.4 |
Abbreviation: PSMMC, Prince Sultan Medical Military City.
Table 5.
Demographic characteristics of the primary HCWs by violence status in Family and Community Centers, PSMMC, Riyadh (2014)
| HCWs characteristic | No violence | Violence | P-value | ||
|---|---|---|---|---|---|
|
| |||||
| N | % | N | % | ||
| Sex | |||||
| Male | 57 | 51.8 | 53 | 48.2 | 0.501 |
| Female | 89 | 56.0 | 70 | 44.0 | |
| Age | |||||
| Mean ± standard deviation | 36.2±9.4 | 35.6±8.4 | 0.565 | ||
| Age group | |||||
| ≤30 | 58 | 56.9 | 44 | 43.1 | 0.518 |
| 31–40 | 47 | 49.5 | 48 | 50.5 | |
| >40 | 38 | 56.7 | 29 | 43.3 | |
| Marital status | |||||
| Single | 40 | 54.1 | 34 | 45.9 | 0.673 |
| Married | 99 | 55.3 | 80 | 44.7 | |
| Divorced/widow | 7 | 43.8 | 9 | 56.2 | |
| Occupation | |||||
| Doctor | 74 | 55.6 | 59 | 44.4 | 0.045 |
| Nurse | 48 | 64.0 | 27 | 36.0 | |
| Other HCWs | 25 | 40.3 | 37 | 59.7 | |
| Pharmacist | 8 | 38.1 | 13 | 61.9 | |
| Technician | 9 | 60.0 | 6 | 40.0 | |
| Clerk | 6 | 31.6 | 13 | 68.4 | |
| Others | 2 | 28.6 | 5 | 71.4 | |
| Nationality | |||||
| Saudi | 86 | 52.8 | 77 | 47.2 | 0.493 |
| Non-Saudi | 61 | 57.0 | 46 | 43.0 | |
Abbreviations: HCW, health care worker; PSMMC, Prince Sultan Medical Military City.
Table 6.
Occupational characteristics of the primary health care workers by violence status in Family and Community Centers, PSMMC, Riyadh (2014)
| HCWs occupational characteristic | No violence | Violence | P-value | ||
|---|---|---|---|---|---|
|
| |||||
| N | % | N | % | ||
| Working multiple shifts | |||||
| No | 120 | 61.2 | 76 | 38.8 | <0.001 |
| Yes | 27 | 36.5 | 47 | 63.5 | |
| Shift time worked | |||||
| Morning shift | 119 | 62.0 | 73 | 38.0 | <0.001 |
| Evening or night shift | 28 | 35.9 | 50 | 64.1 | |
| Number of coworkers in the same working place | |||||
| 1–5 | 46 | 50.0 | 46 | 50.0 | 0.559 |
| 6–10 | 44 | 55.0 | 36 | 45.0 | |
| >10 | 56 | 57.7 | 41 | 42.3 | |
| Sex of served patient | |||||
| Male | 11 | 55.0 | 9 | 45.0 | 0.978 |
| Female | 25 | 55.6 | 20 | 44.4 | |
| Both | 110 | 53.9 | 94 | 46.1 | |
| Presence of encouragement to report violence | |||||
| No/do not know | 99 | 49.3 | 102 | 50.7 | 0.006 |
| Yes | 46 | 68.7 | 21 | 31.3 | |
| Availability of a violence reporting system | |||||
| No/do not know | 59 | 53.6 | 51 | 46.4 | 0.696 |
| Yes | 88 | 56.1 | 69 | 43.9 | |
| In case of system, awareness about how to use | |||||
| No/do not know | 26 | 55.3 | 21 | 44.7 | 0.904 |
| Yes | 62 | 56.4 | 48 | 43.6 | |
| In case of system, the system is effective | |||||
| No/do not know | 25 | 54.3 | 21 | 45.7 | 0.807 |
| Yes | 61 | 56.5 | 47 | 43.5 | |
Abbreviations: HCW, health care worker; PSMMC, Prince Sultan Medical Military City.
Those who worked more than one shift per day reported significantly more frequent violence than those who worked only one shift (63.5% vs 38.8%, P<0.001). Those who were working evening or night shifts reported significantly more frequent violence than those who were working morning shifts (64.1% vs 38.0%, P<0.001). Those who lacked an encouraging environment to report the violence reported significantly more frequent violence than those who had an encouraging environment (50.7% vs 31.3%, P=0.006). On the other hand, demographic characteristics, such as age, sex, marital status, and nationality, were not significantly associated with violence. Similarly, occupational characteristics, such as the number of coworkers, sex of patient, and the availability of a violence reporting system, were not significantly associated with violence.
Regression analysis of the factors that were significantly associated with the violence is shown in Table 7. Univariate regression analysis showed significant odds ratio (OR) for working evening or night shift (OR=2.9, 95% CI 1.7–5.0), working multiple shifts (OR=2.7, 95% CI 1.6–4.8), lack of encouraging environment to report violence (OR=2.3, 95% CI 1.3–4.1), and having an occupation other than doctor or nurse (OR=1.9, 95% CI 1.0–3.4). On the other hand, in a multiple regression analysis that included the aforementioned characteristics, working evening or night shifts was the only variable that remained significantly associated with violence (OR=3.1, 95% CI 1.7–5.4, P<0.001).
Table 7.
Logistic regression analysis for violence experienced using significantly associated demographic and occupational characteristics of the primary HCWs in Family and Community Centers, PSMMC, Riyadh (2014)
| HCWs occupational characteristic | Univariate analysis | Multivariate | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | 95% CI | P-value | OR | 95% CI | P-value | |
| Working evening or night shift | 2.9 | 1.7–5.0 | <0.001 | 3.1 | 1.7–5.4 | <0.001 |
| Working multiple shifts | 2.7 | 1.6–4.8 | <0.001 | |||
| Lack of encouragement to report | 2.3 | 1.3–4.1 | 0.006 | |||
| Occupation | ||||||
| Nurses vs doctors | 0.7 | 0.4–1.3 | 0.241 | |||
| Other HCWs vs doctors | 1.9 | 1.0–3.4 | 0.048 | |||
Abbreviations: CI, confidence interval; HCW, health care worker; OR, odds ratio; PSMMC, Prince Sultan Medical Military City.
Discussion
Primary HCWs are the first line of contact with patients seeking primary care services in Saudi Arabia. Therefore, they are vulnerable to violence from patients and family members. The presence of >2,250 centers throughout the Kingdom indicates the large number and importance of HCWs. The current study showed an overall health care violence rate of 46% among primary HCWs in four centers in Riyadh, Saudi Arabia. This was considerably higher than reported before by El-Gilany et al17 in primary care centers in Al-Hassa, where 28% of the primary HCWs examined experienced at least one violent event during the past year. However, the current results were much less than reported by Algwaiz et al16 in two public hospitals in Riyadh, where 67% of HCWs examined experienced some sort of violence in the 12 months prior to the study.
Comparing the current findings to local and international published reports is not an easy task. This is due to the differences in study methodology, definition of violence, duration covered, and type of HCWs examined. The problem is even worse when examining violence against HCWs in primary care centers, as most previous studies examined health care violence in emergency departments, psychiatric units, geriatric units, and acute care units, where risk is perceived to be high.3,5 We were only able to identify a few studies done among primary HCWs in Saudi Arabia and Egypt.13,17 Additionally, the definitions of violence used in local studies were different. For example, El-Gilany et al17 used a comprehensive WHO definition, including sexual harassment and bullying or mobbing, while Algwaiz et al16 used a broader definition defining any aggressive behavior against health workers, including physical assault or verbal aggression as violence, and the respondents self-reported.
Several studies that examined violence against HCWs in settings other than primary care showed that verbal or psychological violence is much higher than physical violence.10,12,21,22 For example, verbal violence was approximately five times higher than physical violence in a study conducted in multiple hospitals in Jordan.14 Additionally, verbal violence was approximately ten times higher than physical violence in a study done in 436 hospitals in the Congo.21 Unlike primary health care centers, physical violence in emergency and psychiatric departments is reported to be higher.3,23,24 For example, 67% of nurses and 51% of doctors working in the emergency department at five hospitals in the US reported physical violence at least once during the prior 6 months.23 Additionally, 35% of HCWs working at a psychiatric hospital in Taiwan reported exposure to physical violence during the last year.24 One explanation for this lower prevalence rate could be that patients visiting primary care centers are less volatile as compared with emergency and psychiatric patients. In addition, patients with mental health disorders or under the influence of alcohol and drug intoxication are more likely to commit physical violence.1
More than half of the HCWs who experienced violence in the current study never reported it to their supervisors or hospital administration. This negative reaction has been reported in several other studies.16,19,23,25 For example, ~36% of primary HCWs in Al-Hassa never reported the violence they experienced. They felt the violence was part of their job, had negative experiences when reporting, and even feared consequences for reporting.16 Additionally, >70% of the violence experienced by HCWs working in public emergency departments in Cyprus was never reported as there was a general belief that workplace violence was a normal part of the work.25 Underreporting of health care violence was linked to lack of support from administration, fear of retaliation, excessive paperwork, and poor reporting mechanisms.33 In our study, underreporting was caused by the belief that reporting was an inefficient reaction and some feared losing their jobs. It also reflected the lack of an encouraging environment for violence reporting, which was expressed by the majority of HCWs in the study. Combining these findings with the fact that the majority of our HCWs reported the availability of a reporting system, it seems that the majority of health care works in the current study did not trust the implemented safety program.
A considerable number of the HCWs in the current study reported the violence they experienced was caused by a lack of penalty for offenders, misunderstandings, unmet service demands, overcrowding, and long waiting times. These findings were similar to findings from several reports that showed that workplace violence is closely linked to understaffing that resulted in long waiting times and overcrowding.1,5,10,18 We could not find a significant association between being a victim of violence and demographic characteristics, such as age, sex, and marital status. Similarly, no particular sex or age patterns were identified among the HCW victims in Al-Hassa.17 On the other hand, violence was more frequent among male and married nurses in primary health care centers in Egypt.13 Additionally, literature review of studies worldwide showed conflicting findings about age and sex of the violence victim.1,3
Nurses in the current study reported slightly less violence than physicians. Similarly, some studies reported less violence toward nurses than physicians.17 However, the majority of studies reported more violence in nurses than physicians.9,16,19,23 Less violence toward nurses in the current study, as compared with physicians, could relate to underreporting rather than a real finding. Since our sample is a convenient sample, more nurses than physicians could have declined to report the violence they experience for fear of retaliation. Another suggestion is that underreporting of workplace violence among nurses could be due to a desire not to be disloyal to colleagues.27
Occupational characteristics that were linked to violence in the current study included working multiple shifts, working the evening or night shift, and lack of an encouraging environment to report. However, working evening or night shifts was the only independent factor associated with violence. Similarly, several studies in Egypt, Jordan, Palestine, and several other parts of the world showed that the majority of the workplace violence occurred in the evening and night shifts.13–15,28–30 Working the night shift is usually associated with working alone for long hours, both of which were considered risk factors for workplace violence. Additionally, working during the night increases the risk of exposure to more volatile patients due do lax security.1,5,31 It was suggested that maintaining staffing patterns, which would limit workers being alone and limiting after-hour care, and producing firm penalties for offenders are needed to reduce the risk of workplace violence.1,5,7,32
The current study had several strengths and a few limitations. It is one of the few Saudi studies to examine independent risk factors for health care violence among HCWs in primary care centers. In fact, as most previous studies focused on emergency departments and psychiatric units, the current study is one of the few studies worldwide that targeted primary care centers. The current study used the standard WHO definition of violence to allow for better comparison with other studies. The current study not only estimated the frequency of violence among primary care workers but also covered perceived causes, reactions, and consequences. Nevertheless, we acknowledge a few limitations. For example, the convenience sampling used in the current study may limit the generalizability of the findings. Additionally, as the questionnaire was self-administered, recall bias cannot be excluded. However, limited generalizability and recall bias are almost unavoidable limitations in the majority of similar studies.
The findings of the current study revealed several areas that require correction and/or better enforcement of current policies and procedures. Several preventive measures are suggested based on the current study findings such as establishing an effective and safe reporting system and encouraging HCWs to report incidents of violence, ensuring that HCWs have the appropriate education and training and are familiar with the workplace’ policies and procedures, and installing security devices, such as video cameras and good lighting in hallways. Future studies should focus on testing the effects of educational activities and zero tolerance policies on the frequency of workplace violence. “SICOT Declaration of Hyderabad on Violence against Healthcare Workers”33 is a good example of an initiative that raises the concern of and call for more governmental and societal legislations and regulations in facing violence against health workers.
Acknowledgments
Views expressed in this article are the authors’ own and not an official position of the institution or funder.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Gillespie GL, Gates DM, Miller M, Howard PK. Workplace violence in healthcare settings: risk factors and protective strategies. Rehabil Nurs. 2010;35(5):177–184. doi: 10.1002/j.2048-7940.2010.tb00045.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Work Safe BC Preventing violence in health care: five steps to an effective program. 2005. [Accessed January 15, 2015]. Available from: http://www.worksafebc.com/publications/health_and_safety/by_topic/assets/pdf/violhealthcare.pdf?_ga=1.54472365.402846214.1421522511.
- 3.Taylor JL, Rew L. A systematic review of the literature: workplace violence in the emergency department. J Clin Nurs. 2011;20(7–8):1072–1085. doi: 10.1111/j.1365-2702.2010.03342.x. [DOI] [PubMed] [Google Scholar]
- 4.Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors. World Report on Violence and Health. Geneva: World Health Organization; 2002. [Accessed January 15, 2015]. Available from: http://whqlibdoc.who.int/publications/2002/9241545615_eng.pdf?ua=1. [Google Scholar]
- 5.National Institute for Occupational Safety and Health (NIOSH) Violence. Occupational Hazards in Hospitals. 2002. [Accessed January 15, 2015]. Available from: http://www.cdc.gov/niosh/docs/2002-101/pdfs/2002-101.pdf.
- 6.International Labor Office. International Council of Nurses. World Health Organization. Public Services International . Workplace Violence in the Health Sector: Country Case Studies Research Instruments: Survey Questionnaire. ILO/ICN/WHO/PSI Joint program on workplace violence in the health sector; Geneva: 2003. [Accessed January 15, 2015]. Available from: http://www.who.int/violence_injury_prevention/violence/interpersonal/en/WVquestionnaire.pdf. [Google Scholar]
- 7.Martino Vd. Workplace Violence in the Health Sector Country Case Studies. Geneva: World Health Organization; 2002. [Accessed January 15, 2015]. Available from: http://cdrwww.who.int/violence_injury_prevention/violence/activities/workplace/WVsynthesisreport.pdf. [Google Scholar]
- 8.National Crime Prevention Strategy . Prevent violence at work. It works; [Accessed January 15, 2015]. Available from: http://www.prevention-violence.com/en/intro.asp. [Google Scholar]
- 9.Hader R. Workplace Violence Survey 2008: unsettling findings: employees safety isn’t the norm in our healthcare settings. Nursing Manage. 2008;39(7):13–19. doi: 10.1097/01.NUMA.0000326561.54414.58. [DOI] [PubMed] [Google Scholar]
- 10.Fujita S, Ito S, Seto K, Kitazawa T, Matsumoto K, Hasegawa T. Risk factors of workplace violence at hospitals in Japan. J Hospital Med. 2012;7(2):79–84. doi: 10.1002/jhm.976. [DOI] [PubMed] [Google Scholar]
- 11.Roche M, Diers D, Duffield C, Catling-Paull C. Violence toward nurses, the work environment, and patient outcomes. J Nurs Scholarsh. 2010;42(1):13–22. doi: 10.1111/j.1547-5069.2009.01321.x. [DOI] [PubMed] [Google Scholar]
- 12.Ridenour M, Lanza M, Hendricks S, et al. Incidence and risk factors of workplace violence on psychiatric staff. Work. 2014;51(1):19–28. doi: 10.3233/WOR-141894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abbas MA, Fiala LA, Abdel Rahman AG, Fahim AE. Epidemiology of workplace violence against nursing staff in Ismailia Governorate, Egypt. J Egyptian Public Health Assoc. 2010;85(1–2):29–43. [PubMed] [Google Scholar]
- 14.ALBashtawy M. Workplace violence against nurses in emergency departments in Jordan. Int Nurs Rev. 2013;60(4):550–555. doi: 10.1111/inr.12059. [DOI] [PubMed] [Google Scholar]
- 15.Kitaneh M, Hamdan M. Workplace violence against physicians and nurses in Palestinian public hospitals: a cross-sectional study. BMC Health Serv Res. 2012;12:469. doi: 10.1186/1472-6963-12-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Algwaiz WM, Alghanim SA. Violence exposure among health care professionals in Saudi public hospitals. A preliminary investigation. Saudi Med J. 2012;33(1):76–82. [PubMed] [Google Scholar]
- 17.El-Gilany AH, El-Wehady A, Amr M. Violence against primary health care workers in Al-Hassa, Saudi Arabia. J Interpers Violence. 2010;25(4):716–734. doi: 10.1177/0886260509334395. [DOI] [PubMed] [Google Scholar]
- 18.Findorff MJ, McGovern PM, Wall M, Gerberich SG, Alexander B. Risk factors for work related violence in a health care organization. Inj Prev. 2004;10(5):296–302. doi: 10.1136/ip.2003.004747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fernandes CM, Bouthillette F, Raboud JM, et al. Violence in the emergency department: a survey of health care workers. CMAJ. 1999;161(10):1245–1248. [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Faris H, Al-Faris E, Naghma N, et al. A history of childhood maltreatment among spouses predicts violence against women. Ann Saudi Med. 2013;33(6):595–600. doi: 10.5144/0256-4947.2013.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muzembo BA, Mbutshu LH, Ngatu NR, et al. Workplace violence towards Congolese health care workers: a survey of 436 healthcare facilities in Katanga province, Democratic Republic of Congo. J Occup Health. 2014;2015;57(1):69–80. doi: 10.1539/joh.14-0111-OA. [DOI] [PubMed] [Google Scholar]
- 22.Silva IV, Aquino EM, Pinto IC. Workplace violence in the healthcare sector: the experience of State health employees in Bahia State, Brazil. Cad Saude Publica. 2014;30(10):2112–2122. doi: 10.1590/0102-311x00146713. [DOI] [PubMed] [Google Scholar]
- 23.Gates DM, Ross CS, McQueen L. Violence against emergency department workers. J Emg Med. 2006;31(3):331–337. doi: 10.1016/j.jemermed.2005.12.028. [DOI] [PubMed] [Google Scholar]
- 24.Chen WC, Hwu HG, Kung SM, Chiu HJ, Wang JD. Prevalence and determinants of workplace violence of health care workers in a psychiatric hospital in Taiwan. J Occup Health. 2008;50(3):288–293. doi: 10.1539/joh.l7132. [DOI] [PubMed] [Google Scholar]
- 25.Vezyridis P, Samoutis A, Mavrikiou PM. Workplace violence against clinicians in Cypriot emergency departments: a national questionnaire survey. J Clin Nurs. 2014;24(9–10):1210–1222. doi: 10.1111/jocn.12660. [DOI] [PubMed] [Google Scholar]
- 26.Arnetz JE, Arnetz BB. Violence towards health care staff and possible effects on the quality of patient care. Soc Sci Med. 2001;52(3):417–427. doi: 10.1016/s0277-9536(00)00146-5. [DOI] [PubMed] [Google Scholar]
- 27.Hockley C. The language used when reporting interfemale violence among nurses in the workplace. Collegian. 2000;7(4):24–29. doi: 10.1016/s1322-7696(08)60387-x. [DOI] [PubMed] [Google Scholar]
- 28.Crilly J, Chaboyer W, Creedy D. Violence towards emergency department nurses by patients. Accid Emerg Nurs. 2004;12(2):67–73. doi: 10.1016/j.aaen.2003.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Mayhew C, Chappell D. Occupational Violence: Types, Reporting Patterns, and Variations between Health Sectors. 2001. [Accessed January 15, 2015]. Available from: http://wwwdocs.fce.unsw.edu.au/orgmanagement/WorkingPapers/WP139.pdf.
- 30.Pai HC, Lee S. Risk factors for workplace violence in clinical registered nurses in Taiwan. J Clin Nurs. 2011;20(9–10):1405–1412. doi: 10.1111/j.1365-2702.2010.03650.x. [DOI] [PubMed] [Google Scholar]
- 31.Clements PT, DeRanieri JT, Clark K, Manno MS, Kuhn DW. Workplace violence and corporate policy for health care settings. Nurs Econ. 2005;23(3):119–124. 107. [PubMed] [Google Scholar]
- 32.Hinsenkamp M. Violence against healthcare workers. Int Orthop. 2013;37(12):2321–2322. doi: 10.1007/s00264-013-2129-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hinsenkamp M. SICOT Declaration of Hyderabad on violence against healthcare workers. Int Orthop. 2014;38(4):685–687. doi: 10.1007/s00264-014-2311-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


