Abstract
Objective
To examine the associations between multiple aspects of social support—perceived support, structural support, and community integration—and mental health difficulties in younger and older male veterans. Drawing from Socioemotional Selectivity Theory (SST), we hypothesized that greater support would be more strongly negatively related to mental health difficulties in older than younger veterans.
Design
Cross-sectional web survey of younger and older male veterans drawn from a contemporary, nationally representative sample of veterans residing in the United States.
Setting
Data were drawn from the National Health and Resilience in Veterans Study (NHRVS).
Participants
Participants were 290 younger male veterans (mean age=37.0, SD=6.9, range=21–46) and 326 older male veterans (mean age=81.7, SD=3.2, range=78–96).
Measurements
Participants completed measures of socio-demographic and military characteristics, perceived and structural social support, community integration, and mental health difficulties.
Results
In contrast to SST, higher perceived support was associated with fewer mental health difficulties in younger but not older veterans. In line with SST, community integration was associated with fewer mental health difficulties in older but not younger veterans. Structural support was not associated with mental health difficulties in either group.
Conclusion
Results of this study provide mixed support for SST and suggest that different aspects of social support may help promote the mental health of younger and older male U.S. veterans. Promotion of community engagement may protect mental health in older veterans, while promotion of functional social support may protect mental health in younger veterans.
Keywords: veterans, social support, mental health, age differences
Although a large literature demonstrates the protective effect of social support on mental health in older and younger veterans,1,2 systematic research into whether different types of social support may be more beneficial in certain stages of life among veterans is lacking. Socioemotional Selectivity Theory (SST) states that as people enter older age they become more aware of time limitations in life, and thus concern themselves with maintaining emotionally close relationships and decreasing the experience of negative emotions.3 While social network size tends to decrease as people age, satisfaction with social support tends to increase, and it has been suggested that this satisfaction is protective for older adults’ health.4 The aim of the present study was to examine whether these patterns of social support and aging apply to veterans, a group that is at increased risk for mental health difficulties such as posttraumatic stress disorder (PTSD) and depression compared to the general U.S. population.5, 6
Existing research with civilians provides some evidence that older age may increase the buffering effects of social support on mental health. The stress-buffering model of social support asserts that the psychological and material resources provided by others protect individuals from the negative impacts of stress and related mental health difficulties. This protection may come from encouraging better coping or reducing perceptions of threatening events.7 Age, however, may impact the degree of this buffering effect, such that the buffering effects of social support are greater among older adults compared to younger adults.8 Kafetsios and Sideridis found that perceived satisfaction with social support was more strongly positively associated with well-being in middle-aged adults (age 35–66) compared with younger adults (ages 18–34).9
The present study extends past research with civilians to veterans because of veterans’ heightened risk for mental health difficulties. Not only are some veterans exposed to combat and trauma, but most veterans face stressors such as frequent changes in residence, rigorous physical and mental training, separation from family members, and the threat of physical harm, all of which likely affect mental health. Veterans also have the unique social experience of adjusting to civilian life and reintegrating into society after service, which can be challenging.10 While these experiences related to military service often occur early in life, they may continue to impact the psychological and physical development of individuals throughout the lifespan.11 Stressors may also be exacerbated in old age. For example, being retired from work may make PTSD symptoms worse because there is more time to think and less distraction from painful memories.12 Some older adults experience Late-Onset Stress Symptomatology (LOSS), which can be triggered when older adults reflect on earlier parts of their life and their role in wars, even after having functioned well since exiting the military. It also remains to be determined whether different types of support, such as perceived support, structural support, and community integration, are more protective for older compared to younger veterans. Perceived support is the person’s subjective impression of available social support, including emotional (e.g. nurturing support), instrumental (e.g. material assistance), informational resources (e.g. advice), and positive social interaction (e.g. social activities). Structural support is the size and complexity of one’s social network, including the number of friends and family. Finally, community integration is a person’s involvement in broader social networks, such as participation in community activities.13–15 In the present study, we draw from SST to hypothesize that older veterans would benefit more from social support compared to younger veterans in terms of protecting their mental health, and this would be the case for perceived support, structural support, and community integration. However, we also acknowledge that older and younger veterans have had historically different lives, such as being exposed to different wars and events, and there may be cohort effects that are independent of SST effects.16
Methods
Data were drawn from the National Health and Resilience in Veterans Survey (NHRVS), a nationally representative study of U.S. veterans. The main focus of the NHRVS is to characterize the prevalence and correlates of major psychiatric disorders and healthy aging in a contemporary, nationally representative sample of U.S. veterans. For this study we utilized cross-sectional data from Wave 1, conducted from October to December 2011.
Participants
The NHRVS sample was drawn from a research panel of more than 50,000 households that was developed and maintained by GfK Knowledge Networks, Inc. (Menlo Park, CA). GfK manages a probability-based, online non-volunteer access survey panel called KnowledgePanel®, which is a nationally representative sample of adults that covers approximately 98% of U.S. households, including cell-phone only households. The total NHRVS sample includes 3,157 participants, 64.1% of whom are over the age of 60 years old, 89.8% who are male, and 83.6% who are white/Non-Hispanic. As the majority of the sample is male, the impact of social support on health may vary by sex, and there would not be enough statistical power to evaluate gender differences, we restricted our study sample to male veterans, which totaled 2,836 individuals (mean age=63.3, SD=12.4, range 21–93). Because the unweighted age distribution of the NHRVS sample was skewed towards the older age range, we further limited our study sample to the lower (≤10th percentile) and upper (≥90th percentile) ranges of ages using an extreme groups approach (EGA). According to Preacher et al., EGA is the optimal design for detecting interactions and during the exploratory phase of research when the form of the relationship is not yet fully understood.17 Although we have theoretical rationale for the existence and direction of the effect of social support on mental health by age, our study is still somewhat exploratory. Using this method, the younger group comprised of 290 men with a weighted mean age of 37.0 (SD=6.9, range= 21–46) years and the older group included 326 men with a weighted mean age of 81.7 (SD=3.2; range=71–96). Other demographic, health, and psychosocial characteristics are described in Table 1.
Table 1.
Sample characteristics: Younger versus Older Veterans
| Younger Veterans raw n (weighted % or mean [SD]) |
Older Veterans raw n (weighted % or mean [SD]) |
|
|---|---|---|
| N | 290 (57.1%) | 326 (42.9%) |
| Demographics | ||
| Age*** | 37.0 (6.9) | 81.7 (3.2) |
| Caucasian race/ethnicity*** | 207 (61.1%) | 298 (91.4%) |
| Some college or higher education | 235 (62.9%) | 278 (66.9%) |
| Married/living with partner | 222 (71.9%) | 243 (70.9%) |
| Currently Employed*** | 228 (76.6%) | 16 (6.6%) |
| Metropolitan residence | 246 (83.8%) | 279 (83.3%) |
| Household income≥$60K*** | 157 (49.2%) | 135 (32.9%) |
| Military characteristics | ||
| Enlisted in military*** | 288 (99.8%) | 218 (67.9%) |
| Branch | ||
| Army** | 90 (25.9%) | 141 (41.9%) |
| Navy* | 71 (22.7%) | 90 (30.4%) |
| Air Force | 56 (16.7%) | 70 (18.2%) |
| Marine Corps** | 56 (27.9%) | 13 (4.8%) |
| Other Branch | 17 (6.9%) | 8 (3.7%) |
| Combat veteran | 128 (41.0%) | 139 (46.5%) |
| VA main source of healthcare** | 60 (22.9%) | 34 (14.2%) |
| Health characteristics | Mean (SD) | Mean (SD) |
| Physical health difficulties factor*** | −0.28 (0.90) | 0.47 (0.98) |
| Cognitive functioning*** | 84.6 (19.9) | 90.5 (10.3) |
| Mental health difficulties factor*** | 0.21 (1.1) | −0.41 (0.44) |
| Mental Health Treatment | ||
| Any treatment ever*** | 77 (30.2%) | 40 (14.5%) |
| Any current treatment*** | 58 (16.9%) | 13 (5.4%) |
| Prescription medication*** | 49 (14.4%) | 11 (3.4%) |
| Psychotherapy or counseling*** | 36 (12.1%) | 6 (3.7%) |
| Psychosocial characteristics | Mean (SD) | Mean (SD) |
| Number of lifetime traumas*** | 3.7 (3.1) | 2.6 (2.2) |
| Social support factors | ||
| Perceived Support*** | 18.6 (5.5) | 20.6 (4.2) |
| Structural support*** | 5.5 (4.9) | 11.4 (10.4) |
| Community integration*** | 3.6 (1.7) | 5.1 (1.5) |
| Satisfaction with: | ||
| Family relationships** | 3.7 (1.1) | 4.4 (0.7) |
| Social relationships** | 3.5 (1.1) | 4.1 (0.8) |
Note. SD=standard deviation, Continuous variables were compared using independent t-tests; categorical variables were compared using chi-squared tests; degrees of freedom for chi-squared tests=1, except for Branch=4; degrees of freedom for t-tests=808.
Groups differ significantly at *p<0.05,
p<0.01, or
p<.0.001.
Procedures
KnowledgePanel® members are recruited through national random samples by telephone or postal mail. Using this method, Knowledge Networks is able to include households with listed or unlisted numbers, those with or without telephones, cell phone-only households, as well as those with and without Internet access. If households did not have Internet or computer access, Knowledge Networks provided it to them. To be included in the NHRVS study, participants had to self-identify as veterans during their initial entry to the panel, where they were asked about previous or current service in the U.S. Armed forces, Military Reserves, or National Guard. Of the 4,750 veterans sampled for the NHRVS, 3,408 (71.7%) responded to an invitation to participate and completed a screening question to confirm their study eligibility (current or past active military status). Of these respondents, 3,188 (93.5%) confirmed their current or past active military status and, of these, 3,157 (92.6%) completed a confidential, 60-minute online survey. This survey assessed information regarding demographics and military history, medical and psychiatric status, and psychosocial functioning. To generalize to the general population of U.S. veterans, post-stratification weights were computed by statisticians at GfK Knowledge Networks, Inc. and applied to inferential statistics, based on demographic distributions (e.g. age, gender, race/ethnicity, education, census region, metropolitan area) of the most contemporaneous 2011 Current Population Survey.18 This study was approved by the Human Subjects Subcommittee of the VA Connecticut Healthcare System. All participants provided informed consent.
Assessments
Mental Health Difficulties
To limit the number of study variables, especially those that were highly correlated, exploratory factor analyses using a promax rotation were conducted to reduce variables into composite scores. Raw scores for related measures were entered into the analyses, and those factors with eigenvalues >1.00 were extracted into factor scores. This procedure was conducted to derive mental and physical health difficulties factors, which were analyzed as an outcome and covariate, respectively. The mental health difficulties factor (eigenvalue: 2.49; 83.1% variance explained) was comprised of scores on depression (factor loading: 0.942) and anxiety (factor loading: 0.918) symptom scores from the Patient Health Questionnaire-4,19 and scores on the Posttraumatic Stress Disorder Checklist (PCL-C)20 (factor loading: 0.873). These measures assess the presence of current mental distress (PHQ-4: past two weeks, PCL: past month). A log transformation was applied to the composite score (Ln(1+mental health difficulties factor) to correct for non-normality. Higher scores, which represent standardized factor scores, are indicative of greater mental health difficulties.
Perceived social support
Perceived social support was measured using a 5-item version of the Medical Outcomes Study (MOS) social support scale.21,22 This measure had excellent internal consistency in both the younger (α=0.92) and older (α=0.88) subsamples, as well as the full sample (α=0.91). This scale includes questions assessing emotional/informational, tangible, affectionate support and positive social interactions.21 None of the participants had a z-score lower or greater than 3 on this measure.
Structural support
Structural support was assessed using a single item, “About how many close friends and relatives do you have (people you feel at ease with and can talk to about what is on your mind)? Responses that had a z-score higher than 3 were considered outliers and excluded (n=13).
Community integration
Community integration was assessed using a single item: “I feel well integrated in my community (e.g., regularly participate in community activities)” from 1 (strongly disagree) to 7 (strongly agree). None of the participants had a z-score lower or greater than 3 on this measure.
Covariates
Socio-demographic and military characteristics. Participants provided socio-demographic information including race/ethnicity, education, marital status, employment, residence, and income. Participants also answered questions about military characteristics, such as whether or not they had enlisted or been drafted; what branch they had served in; and whether the VA was their main source of healthcare. Combat exposure was evaluated by asking participants, “Did you ever serve in a combat or war zone?”
The physical health difficulties factor (eigenvalue: 1.34, 67.0% variance explained) included 1) the sum of medical conditions from a list of 20 conditions (e.g. asthma, heart disease, etc.; factor loading: 0.818), and 2) the score on the 6-item Somatization subscale of the Brief Symptom Inventory-1823 (factor loading: 0.818). Higher factor scores represent greater physical health difficulties.
Cognitive functioning was evaluated using the Medical Outcomes Study Cognitive Functioning Scale-Revised.24 This 6-item scale assesses past-month difficulties in six cognitive domains, including reasoning, concentration and thinking, confusion, memory, attention and psychomotor speed. Higher scores indicate better functioning.
Mental health treatment. Individuals responded first to the question, “Have you ever received mental health treatment (e.g. prescription medication or psychotherapy for a psychiatric or emotional problem)? Individuals who endorsed this question were asked whether they were currently taking prescription medication and/or receiving psychotherapy or counseling for a psychiatric or emotional problem.
Trauma characteristics. Sum of total lifetime traumas was also measured using a 15-item version (1-item regarding life-threatening illness or injury added to original 14-item) of the Trauma History Screen,25 which assesses whether certain traumatic events (e.g. physical or sexual abuse, seeing someone die suddenly or get badly hurt or injured, witnessing something horrible or was badly scared during military service, etc) had occurred during an individual’s lifetime.
Data analysis
Data analyses proceeded in four steps. First, to compare the younger and older groups, chi-squared analyses were conducted for categorical outcomes and independent t-tests for continuous outcomes. Second, correlations were conducted to evaluate bivariate associations among all variables. Variables that were significantly correlated with both the independent variables and the outcome were included as covariates in subsequent analyses. Third, to examine the primary hypothesis regarding whether age moderated the relationship between social support (perceived, structural, community integration) and mental health difficulties, multivariate linear regression analyses were conducted in the combined sample (N=619; N=810, weighted). For each of the models, covariates along with the independent variables and age group terms were added simultaneously in the first step, and the interaction terms in the second step. Fourth, to examine the magnitude of effects for perceived support, structural support, and community integration on mental health difficulties, we conducted multivariate linear regression models in the younger (N=290; N=463, weighted) and older (N=326; N=347, weighted) groups separately. For all multivariate models, each set of covariates for that particular analysis was entered simultaneously with the independent variables of interest.
Results
Participant Characteristics: Younger versus Older Group
As shown in Table 1, younger and older veterans differed with respect to several demographic and military characteristics. The younger group was less likely to be white, and more likely to be working and have an annual household income greater than $60,000. Younger individuals were significantly more likely to have enlisted versus being drafted in the military and use the VA as their main source of healthcare; however, the groups did not differ with respect to combat exposure. The majority of the sample had a college or higher education, were married or living with a partner, and were in a metropolitan residence. Less than half of the sample were combat veterans.
Younger individuals had less physical health difficulties; however, they had lower cognitive functioning compared to the older group. Furthermore, the younger group was more likely to have had any past or current mental health treatment (Table 1). The younger group had significantly more lifetime traumas than the older group. The younger group had lower average ratings of perceived social support, structural support, community integration, and satisfaction with relationships compared to the older group (Table 1).
Effect of Age Group in Moderating Association between Social Support and Mental Health Difficulties
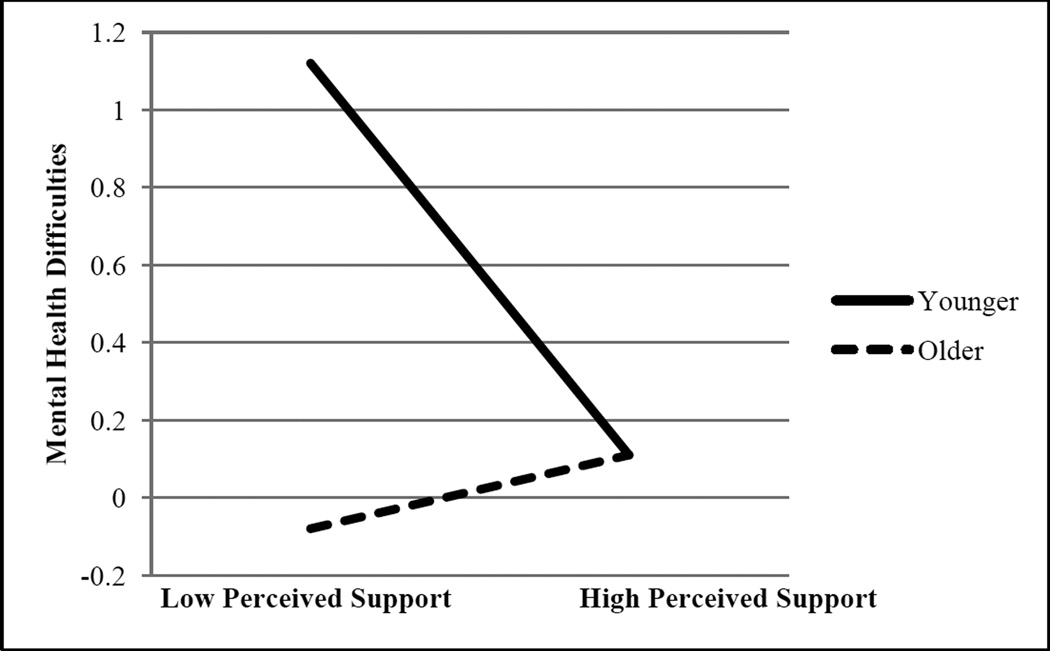
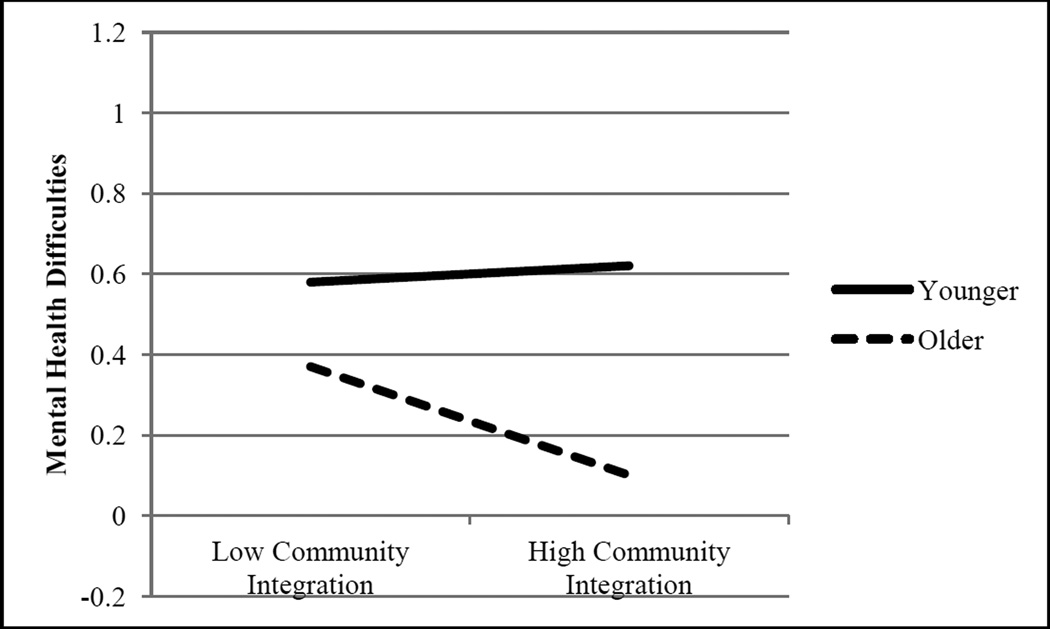
As shown in Table 2, there was a significant interaction of age × perceived support for mental health difficulties. In contrast to our hypothesis, at lower levels of perceived social support, mental health difficulties were significantly greater in the younger compared to the older group, but were at similar levels as the older group in the presence of higher perceived support (Figure 1). There was also a significant interaction for age × community integration on mental health difficulties (Table 2). Unlike perceived support, and as hypothesized, higher community integration was associated with fewer mental health difficulties in the older group compared to the younger group. There was a main effect for community integration, in which higher community integration was associated with fewer mental health difficulties. While mental health difficulties were comparable among younger veterans with high and low community integration, mental health difficulties in the older group with high community integration were significantly lower than those in the low integration group (Figure 2). The interaction for age × structural support on mental health difficulties was not significant. Table 3 shows the magnitudes of each effect for younger and older groups separately.
Table 2.
Summary of Main Effects and Interactions for Age and Social Support Variables Predicting Mental Health Difficulties
| Unadjusted | Adjusteda | ||||||
|---|---|---|---|---|---|---|---|
| Variable | β | t | p | β | t | p | |
| Main effects | |||||||
| Age group | −0.14 | 3.67 | <0.001 | −0.16 | 3.80 | <0.001 | |
| Perceived Support | −0.41 | 11.1 | <0.001 | −0.21 | 6.97 | <0.001 | |
| Structural Support | −0.05 | 1.34 | 0.180 | −0.05 | 1.87 | 0.062 | |
| Community Integration | −0.18 | 4.65 | <0.001 | −0.08 | 2.68 | <0.01 | |
| Constant | 14.4 | <0.001 | 9.67 | <0.001 | |||
| R2 | .35 | .66 | |||||
| Adj. R2 | .35 | .65 | |||||
| Interaction Effects | |||||||
| Age Group × Perceived Support | 0.23 | 6.06 | <0.001 | 0.16 | 5.48 | <0.001 | |
| Age Group × Structural Support | 0.08 | 1.16 | 0.246 | 0.07 | 1.41 | 0.158 | |
| Age Group × Community Integration | 0.08 | 1.90 | 0.058 | −0.07 | 2.72 | 0.007 | |
| Constant | 15.1 | <0.001 | 10.1 | <0.001 | |||
| R2 | .37 | .68 | |||||
| Adj. R2 | .38 | .67 | |||||
Note: Beta = standardized regression coefficient. Statistically significant main effects and interactions (p<0.05) are shown in bold.
Adjusted for any mental health treatment, race, marital status, employment status, education, income, enlistment status, combat veteran status, number of lifetime traumas, cognitive functioning, and physical health difficulties. Final unadjusted main effects model: F(4,715)=85.43, p<0.001; Final unadjusted model with interaction effects: Final adjusted model with main effects: F(15,703)=92.54, p<0.001; Final adjusted model with interaction effects: F(18,700)=83.28, p<0.001).
Figure 1. Interaction of Age Group and Perceived Support in Predicting Mental health difficulties.
Predicted values of mental health difficulties for low perceived support (Mean − 1 SD) and high perceived support (Mean + 1 SD) in adjusted model.
Figure 2. Interaction of Age Group and Community Integration in Predicting Mental health difficulties.
Predicted values of mental health difficulties for low community integration (Mean − 1 SD) and high community integration (Mean + 1 SD) in adjusted model.
Table 3.
Summary of Multiple Regression Analyses of Social Support Variables Predicting Mental Health Difficulties in Younger and Older Groups
| Younger Group | Older Group | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusteda | Unadjusted | Adjustedb | ||||||
| Variable | β | t, p | β | t, p | β | t, p | β | t, p | |
| Perceived Support | −0.49 | 10.24*** | −0.26 | 7.23*** | −0.16 | 2.44* | −0.02 | 0.33, 0.743 | |
| Structural Support | −0.07 | 1.49. 0.137 | 0.05 | 1.66, 0.097 | −0.06 | 0.85, 0.40 | −0.07 | 1.18, 0.24 | |
| Community Integration | −0.15 | 3.26** | 0.01 | 0.42, 0.673 | −0.24 | 3.65*** | −0.20 | 3.40** | |
| R2 | .35 | .72 | .12 | .34 | |||||
| Adj. R2 | .34 | .71 | .11 | .31 | |||||
Note. B = unstandardized regression coefficient; Beta = standardized regression coefficient; statistically significant βs (at p<0.05) are shown in bold;
Statistical significance represented at *p<0.05,
p<0.01, or
p<.0.001.
All F values significant at p<0.001; weighted Ns are reported below.
Adjusted for any mental health treatment, race, marital status, employment status, education, income, enlistment status, combat veteran status, number of lifetime traumas, cognitive functioning, and physical health difficulties. Final unadjusted model in Younger Group: F(3,430)=75.02, p<0.001; Final adjusted model in Younger Group: F(14,419)=80.88, p<0.001; Final unadjusted model in Older Group: F(3,282)=8.15, p<0.001; Final adjusted model in Older Group: F(14,271)=7.65, p<0.001).
Discussion
We found mixed support for our general hypothesis that social support is more protective for the mental health of older compared to younger veterans. While perceived support and community integration were generally associated with better mental health in the entire sample of veterans, higher perceived support was more strongly associated with reduced mental health difficulties for younger than older veterans. However, higher community integration was associated with fewer mental health difficulties for older, but not younger veterans.
First, our findings suggest that community involvement may be especially important for older veterans. Greater participation may increase access to social support, and thus protection from mental distress. Older individuals may have access to health-related information through elder-focused organizations or may interact with individuals who help with stress management. In addition, organizations often offer volunteering opportunities. Older adults who spend more hours volunteering report higher levels of well-being.26 Potential mechanisms may be increased feelings of generativity27,28, greater physical activity,29,30 and protection from social isolation.31 However, it is also important to consider that poor mental health may predict lower community integration, as distressed veterans may be more likely to withdraw from social networks. For example, acceptance of available social support can be especially difficult for individuals with PTSD, who may already have symptoms of avoidance, isolation, and detachment from others.32 Furthermore, it is important to note that our findings showed that older veterans, even those with mental health difficulties, were more socially integrated than younger veterans. One reason may be that there are more community programs for older veterans. Clinicians and community organizers may need to give more attention to community organizations tailored to younger veterans as well.
Second, our findings regarding the protective effects of perceived support for younger veterans highlight the importance of fostering emotional, tangible, and informational social support in one-on-one relationships for younger veterans. As younger veterans are less likely to be members of community organizations,33 these close relationships may be especially important. However, this finding may have been driven by lower rates of mental distress and diagnosis in older veterans. Specifically, the lack of significant effect among older adults could have been due to homogeneity in mental health. The findings showing age differences in mental health outcomes, however, are consistent with epidemiological studies, which demonstrate that fewer older adults suffer from depression and anxiety compared to younger adults.34 A proposed mechanism is that coping strategies improve in older adulthood.35 Also, for people who have experienced a traumatic event, it is possible that PTSD symptoms decrease over time.36 We should also note that veterans who survived into their 80s are quite resilient and may represent a healthy survivor cohort. Mortality bias may, at least in part, account for lower psychological distress in this group.
Third, there were no significant associations between mental health and structural support. Other studies have found weak relationships using measures of the quantity of network members.37, 38 The quality of these relationships may be more important for mental health. However, our lack of significant findings may be due to our one-item measure of structural support. Finally, we found that compared to older veterans, younger veterans scored lower on a measure of cognitive functioning and reported a greater number of traumatic life events. While these findings are somewhat counterintuitive, the magnitude of these group differences was small and additional analyses revealed that they were fully mediated by greater psychiatric distress in the younger veteran group (data not shown, available from corresponding author).
The following study limitations should be considered. As the data is cross-sectional, we are unable to establish causality. Reverse causation is also possible such that poor mental health predicts lower social support, perhaps due to the breaking down of social ties as a result of one’s illness over time.32 Also, we are not able to fully disentangle age effects from cohort effects. Older and younger veterans were exposed to different environments that may affect mental health differently. The wars in Afghanistan and Iraq are the longest combat operations since the Vietnam War, which may expose individuals, especially those with multiple deployments, to more trauma.39 Furthermore, the 90 percent survival rate of soldiers wounded during action in Iraq and Afghanistan exceeds that of the Gulf and Vietnam eras. Despite surviving, individuals must cope with these past traumas and physical and psychological injuries.40 It is also difficult to separate cohort from age effects as service era data was unavailable for non-combat veterans. In addition, measures were self-reported and included sensitive information, which introduces bias. Also, the results are not generalizable to middle-aged and female veterans.
Strengths of this study include the use of a nationally representative veteran sample. Also, various types of functional and structural aspects of social support were assessed in one study, which allowed us to compare how they may differentially affect mental health in the younger compared to older veterans. We also used a theoretical framework from which to test hypotheses about age differences in social support and mental health, while also acknowledging potential cohort effects.
This study provides important information on different types of social support and mental health of younger and older male veterans that can inform research and care for veterans. However, future research is needed. First, longitudinal data should be evaluated to identify whether perceived social support and its relationship with mental health across age groups changes over time. Second, researchers need to evaluate the impact of social support on mental health in female and middle-aged veterans. Third, future research should take into account service era as a way to disentangle age from cohort effects. Fourth, research is needed to examine how social support may differentially buffer effects of combat exposure on younger and older veterans’ mental health. Although research suggests that social support can buffer the effects of combat exposure among veterans in general,1,40,41 no research to our knowledge has assessed age differences. To maintain parsimony in testing our hypotheses and because less than half our sample was exposed to combat, we adjusted for combat to produce findings that can be generalized to all male veterans. However, it will be important to consider the role combat may play in the future-time perspective proposed by SST. It is possible that those with greater combat-related trauma exposure, even younger veterans, may view life as finite and thus place a greater emphasize on close, meaningful relationships. When time is limited, for example in the case of serious illness, younger individuals tend to prefer emotionally gratifying social interactions versus new relationships.42 It is also possible that higher trauma exposure may have the opposite effect on younger veterans’ relationships, as violent combat experiences may increase perceived invincibility.43 It may also be that veterans with PTSD isolate themselves, believing that if they trust or get close to others, they will get hurt or damage their relationships.44 Further research on combat exposure from an SST framework is needed.
To conclude, our results can inform future social support interventions targeted towards male veterans of different age groups specifically. The findings suggest that interventions targeting general mental health or global distress in younger male veterans should focus on enhancement of their close relationships and feelings of support; whereas interventions focused on older male veterans encourage integration into the community.
Acknowledgments
Sources of Funding
This study was funded by the Department of Veterans Affairs National Center for Posttraumatic Stress Disorder. Preparation of this report was supported in part by a Research Career Development Award to Dr. Pietrzak from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (NIA Grant P30AG21342) and in part by National Institutes on Health grants (R01AG032284, R01HL089314) and to Dr. Monin from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (NIA Grant P30AG21342) and in part by National Institutes on Health grant (K01 AG042450)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
There are no disclosures to report.
Contributor Information
Melissa R. Weiner, Social and Behavioral Sciences, Yale School of Public Health, Yale School of Medicine
Joan K. Monin, Social and Behavioral Sciences, Yale School of Public Health, Yale School of Medicine
Natalie Mota, U.S. Department of Veterans Affairs National Center for Posttraumatic Stress Disorder, VA Connecticut Healthcare System, Department of Psychiatry, Yale School of Medicine
Robert H. Pietrzak, U.S. Department of Veterans Affairs National Center for Posttraumatic Stress Disorder, VA Connecticut Healthcare System, Department of Psychiatry, Yale School of Medicine
References
- 1.Pietrzak RH, Johnson DC, Goldstein MB, et al. Psychosocial buffers of traumatic stress, depressive symptoms, and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom: The role of resilience, unit support, and post-deployment social support. J Affect Disord. 2010;120:188–192. doi: 10.1016/j.jad.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 2.Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu Rev Clin Psychol. 2005;1:255–291. doi: 10.1146/annurev.clinpsy.1.102803.143948. [DOI] [PubMed] [Google Scholar]
- 3.Carstensen LL, Charles S. Emotion in the second half of life. Curr Dir Psychol Sci. 1998;7:144–149. [Google Scholar]
- 4.Luong G, Charles ST, Fingerman KL. Better with age: Social relationships across adulthood. J Soc Pers Relat. 2011;28:9–23. doi: 10.1177/0265407510391362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoge CW, Castro CA, Messer SM, et al. Combat duty in Iraq and Afghanistan, Mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 6.Sorrell JM, Durham S. Meeting the Mental Health Needs of the Aging Veteran Population: A Challenge for the 21st Century. Psychosoc Nurs Ment Health Serv. 2011;49:22–25. doi: 10.3928/02793695-20101207-01. [DOI] [PubMed] [Google Scholar]
- 7.Cohen S. Social relationships and health. Am Psychol. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- 8.Matt GE, Dean A. Social support from friends and psychological distress among elderly persons: moderator effects of age. J Health Soc Behav. 1993;34:187–200. [PubMed] [Google Scholar]
- 9.Kafetsios K, Sideridis GD. Attachment, social support, and well-being in youth and older adults. J Health Psychol. 2006;11:836–875. doi: 10.1177/1359105306069084. [DOI] [PubMed] [Google Scholar]
- 10.Sayer NA, Noorbaloochi S, Frazier P, et al. Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatr Serv. 2010;61:589–597. doi: 10.1176/ps.2010.61.6.589. [DOI] [PubMed] [Google Scholar]
- 11.Spiro A, Schnurr PP, Aldwin CM. A life-span perspective on the effects of military service. J Geriatr Psychiatry. 1997;30:91–128. [Google Scholar]
- 12.U.S. Department of Veteran Affairs. Aging Veterans and Posttraumatic Stress Symptoms [National Center for PTSD website] [Accessed September 18, 2015];2015 Sep 2; Available at: http://www.ptsd.va.gov/public/types/war/ptsd-older-vets.asp.
- 13.Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. 2001;78:458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Langford CP, Bowsher J, Maloney JP, et al. Social support: a conceptual analysis. J Adv Nurs. 1997;25:95–100. doi: 10.1046/j.1365-2648.1997.1997025095.x. [DOI] [PubMed] [Google Scholar]
- 15.Jacobson DE. Types and timing of social support. J Health Soc Behav. 1986;27:250–264. [PubMed] [Google Scholar]
- 16.Felton BJ. Cohort variation in happiness: Some hypotheses and exploratory analyses. Int J Aging Hum Dev. 1987;25:27–42. doi: 10.2190/5LC0-LFA2-30VW-UGBV. [DOI] [PubMed] [Google Scholar]
- 17.Preacher KJ, Rucker DD, MacCallum RC, et al. Use of the extreme groups approach: A critical reexamination and new recommendations. Psychol Methods. 2005;10:178–192. doi: 10.1037/1082-989X.10.2.178. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Census Bureau. Current Population Survey. 2010 Oct; Available http://www.census.gov/cps/.
- 19.Kroenke K, Spitzer RL, Williams JB, et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- 20.Weathers F, Litz B, Herman D, et al. The PTSD Checklist (PCL): reliability, validity, and diagnostic utility. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; October, 1993; San Antonio, TX. [Google Scholar]
- 21.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 22.Amstadter AB, Begle AM, Cisler JM, et al. Prevalence and correlates of poor self-rated health in the United States: the national elder mistreatment study. Am J Geriatr Psychiatry. 2010;18:615–623. doi: 10.1097/JGP.0b013e3181ca7ef2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Derogatis LR. The Brief Symptom Inventory-18 (BSI-18): Administration, Scoring and Procedures Manual. Minneapolis, MN: National Computer Systems; 2000. [Google Scholar]
- 24.Stewart AL, Ware JE, Sherbourne CD, et al. In: Psychological distress/well-being and cognitive functioning measures in Measuring Functioning and Well-being: the Medical Outcomes Study Approach. Stewart AL, Ware JE, editors. Durham, NC: Duke University Press; 1992. pp. 102–142. [Google Scholar]
- 25.Carlson EB, Palmieri PA, Ruzek JI, et al. Development and validation of a brief self-report measure of trauma exposure: the Trauma History Screen. Psychol Assess. 2011;23:463–477. doi: 10.1037/a0022294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morrow-Howell N, Hinterlong J, Rozario PA, et al. Effects of volunteering on the well-being of older adults. J Gerontol B Psychol Sci Soc Sci. 2003;58:S137–S145. doi: 10.1093/geronb/58.3.s137. [DOI] [PubMed] [Google Scholar]
- 27.Erikson E. In: Eight ages of man, in Readings in the psychology of adjustment. Gorlow L, Katovsky W, editors. New York, NY: McGraw Hill; [Google Scholar]
- 28.Monin JK, Levy BR, Pietrzak RH. From serving in the military to serving loved ones: Unique experiences of older veteran caregivers. Am J Geriatr Psychiatry. 2014;22:570–579. doi: 10.1016/j.jagp.2012.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fox KR. The influence of physical activity on mental well-being. Public Health Nutr. 1999;2:411–418. doi: 10.1017/s1368980099000567. [DOI] [PubMed] [Google Scholar]
- 30.Arent SM, Landers DM, Etnier JL. The Effects of exercise on mood in older adults: A meta-analytic review. J Aging Phys Act. 2000;8:407–430. [Google Scholar]
- 31.Oxman TE, Berkman LF, Kasl S, et al. Social support and depressive symptoms in the elderly. Am J Epidemiol. 1992;135:356–368. doi: 10.1093/oxfordjournals.aje.a116297. [DOI] [PubMed] [Google Scholar]
- 32.Friedman MJ. Posttraumatic stress disorder among military returnees from Afghanistan and Iraq. Am J Psychiatry. 2006;163:586–593. doi: 10.1176/ajp.2006.163.4.586. [DOI] [PubMed] [Google Scholar]
- 33.Adler RP, Goggin J. What Do We Mean By “Civic Engagement”? J Transform Educ. 2005;3:236–253. [Google Scholar]
- 34.Magruder KM, Frueh BC, Johnson MR, et al. PTSD symptoms, demographic characteristics, and functional status among veterans treated in VA primary care clinics. J Trauma Stress. 2004;17:293–301. doi: 10.1023/B:JOTS.0000038477.47249.c8. [DOI] [PubMed] [Google Scholar]
- 35.Whitbourne SK, Meeks S. In: Psychopathology, bereavement, and aging, in Handbook of the psychology of aging. Schaie KW, Willis SL, editors. Burlington, MA: Elsevier Academic Press; 2011. pp. 311–323. [Google Scholar]
- 36.Friedman MJ, Schnurr PP, McDonagh-Coyle A. Post-traumatic stress disorder in the military veteran. Psychiatr Clin North Am. 1994;17:265–277. [PubMed] [Google Scholar]
- 37.Dalgard OS, Bjoork S, Tambs K. Social support, negative life events and mental health. Br J Psychiatry. 1995;166:29–34. doi: 10.1192/bjp.166.1.29. [DOI] [PubMed] [Google Scholar]
- 38.Jette AM, Davies AR, Cleary PD, et al. The functional status questionnaire. J Gen Intern Med. 1986;1:143–149. doi: 10.1007/BF02602324. [DOI] [PubMed] [Google Scholar]
- 39.Litz BT. Research on the impact of military trauma: Current status and future directions. Mil Psychol. 2007;19:217–238. [Google Scholar]
- 40.Peterson AL, Luethcke CA, Borah EV, et al. Assessment and treatment of combat-Related PTSD in returning war veterans. J Clin Psychol Med Settings. 2011;18:164–175. doi: 10.1007/s10880-011-9238-3. [DOI] [PubMed] [Google Scholar]
- 41.Spiro A, Schnurr PP, Aldwin CM. Combat-related posttraumatic stress disorder symptoms in older men. Psychol Aging. 1994;9:17–26. doi: 10.1037//0882-7974.9.1.17. [DOI] [PubMed] [Google Scholar]
- 42.Löckenhoff CE, Carstensen LL. Socioemotional selectivity theory, aging, and health: the increasingly delicate balance between regulating emotions and making tough choices. J Pers. 2004;72:1395–1424. doi: 10.1111/j.1467-6494.2004.00301.x. [DOI] [PubMed] [Google Scholar]
- 43.Killgore WD, Cotting DI, Thomas JL, et al. Post-combat invincibility: violent combat experiences are associated with increased risk-taking propensity following deployment. J Psychiatr Res. 2008;42:1112–1121. doi: 10.1016/j.jpsychires.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 44.Riggs DS, Byrne CA, Weathers FW, et al. The quality of the intimate relationships of male Vietnam veterans: Problems associated with posttraumatic stress disorder. J Trauma Stress. 1998;11:87–101. doi: 10.1023/A:1024409200155. [DOI] [PubMed] [Google Scholar]