Abstract
The range of implantable cardiac pacing devices has expanded, with the advances in available technology. Indications for cardiac pacing devices, that is pacemakers, implantable cardioverter defibrillators (ICDs) and cardiac resynchronisation therapy devices (CRTs), have expanded for the treatment, diagnosis and monitoring of bradycardia, tachycardia and heart failure. While the need for pacemakers is increasing, not all patients who require pacemakers are receiving them, especially in the Asia-Pacific region. There is a need to be more critical in advising the use of more expensive devices like ICDs and CRT/CRT-D devices, since most patients in the Asia-Pacific region pay out of pocket for these therapies. The AHA-ACC guidelines need not be blindly followed, since they are too wide-sweeping and are often based on the intention-to-treat basis of trials rather than on the parameters of the patients actually enrolled.
Since the introduction of clinical cardiac pacing in 1958,1 the range of implantable cardiac pacing devices has expanded, with advances in available technology. In proportion, the indications for cardiac pacing devices, that is pacemakers, implantable cardioverter defibrillators (ICDs) and cardiac resynchronisation therapy devices (CRTs), have expanded for the treatment, diagnosis and monitoring of bradycardia, tachycardia and heart failure. Often, a large number of capabilities such as bradycardia support, ventricular tachyarrhythmia therapy, biventricular stimulation, arrhythmia monitoring and recording of heart failure data, in varying degrees, are combined into a single device.2 Consequently, the indications for implantation of these devices have broadened with an increasing frequency of device utilisation over the last five decades. Presently, the broadened scope and goal of pacing therapy have been to improve survival and functional status by preservation of a heart-rate response to exercise, maintenance of atrioventricular (AV) synchrony, the preservation of atrial electrical stability and the optimisation of haemodynamics by the use of programmable and automated features.2 3
In a recent estimation, by the Heart Rhythm Society and the European Heart Rhythm Association, approximately 280 000 pacemakers and 160 000 ICDs were implanted in North America in 2006, while the corresponding numbers for the countries of Europe were 250 000 and 50 000 respectively.4 The growth in the use of pacing devices has been exponential, with the review of the United States Food and Drug Administration (US FDA) annual reports revealing a threefold increase for permanent pacemakers and a 10-fold increase for ICDs in the last decade.5 However, the results of the 2001 and the more recent 2005 World Survey on Cardiac Pacing and Implantable Cardioverter Defibrillators show that not all patients who require pacemakers are receiving them, particularly in the Asia-Pacific region. For example, the number of new implants per million population in India (seven implants per million population in the 2001 and 2005 survey) and China (eight implants per million population in the 2001 survey; 13 implants per million population in the 2005 survey) is much less than in the USA (786 implants per million population in the 2001 survey; 752 implants per million population in the 2005 survey) or Germany (837 implants per million population in the 2001 survey).6 7 The low pacemaker implant rates in Asia are due to various reasons, with economic factors being the most important by far.
Pacemakers
Indications for pacing
For the last five decades, sinus node dysfunction (SND) and atrioventricular (AV) block have been the primary indications for pacing. The more recent indications for permanent pacemakers include neurocardiogenic syncope, carotid sinus hypersensitivity, treatment of medically refractory chronic heart failure and prevention of atrial fibrillation.8 In neurocardiogenic syncope, however, pacemakers have a very limited role. They may be used for those with refractory cardioinhibitory type of response; even here they are only partly effective.9 For prevention of atrial fibrillation, different manufacturers have several algorithms. None of these, however, are very effective. They are an “add-on” feature when pacing patients with a tachy–brady syndrome, the primary indication for pacing being bradycardia.8 For carotid sinus hypersensitivity, DDDR pacing with a rate-drop response feature is advisable.10 The appropriate pacemaker, therefore, must be objectively selected on the clinical evidence of a benefit with respect to underlying rhythm disturbance of the patient and other related factors such as chronotropic response to exercise, overall physical condition, associated medical problems and exercise capacity.11
The major indication for pacemakers has been AV block in Asia, while SND has been the most frequent indication for pacing in the Western countries.6 For example, AV block alone was the indication for an average of 48% of the initial implants in the 12 Asian countries evaluated in the 2005 survey, with Bangladesh (87%), Nepal (84%) and India (60%) having the highest percentage. In comparison, AV block was the indication for an average of only 26% of the initial implants in the 16 European countries evaluated with the percentage not exceeding 36% in any of the European countries. Since the incidence of SND and AF increases with age, it is natural that this is more prevalent in the West, where the median age of the population is at least a decade higher than most Asian countries.12 Thus, it is not surprising that AV block is the commonest indication for pacing in the developing world. Since pacing therapy plays a life-saving role when indicated for bradyarrhythmias due to AV block, the optimal utilisation and increased use of pacemakers needs to be focused upon in the Asian region.
Broadly, the selection of pacemaker systems is dependent on the chamber paced: single-chamber (atria or ventricle) with or without rate modulation or dual-chamber (both). In recent years, the goal in permanent pacemaker therapy has been “physiological” pacing (rate modulation and AV synchrony).11 Consequently, the dual-chamber system has become the intuitive choice in pacemaker systems because of its ability in maintaining AV synchrony. However, the conflicting data concerning the benefits of AV sequential pacing in some patient groups and the added cost and complexity of dual-chamber systems have resulted in the continuation of the single-chamber systems as a suitable alternative.
Single-chamber pacemakers
There are essentially only two forms of single-chamber pacing: AAI and VVI, with optional rate modulation (AAIR and VVIR); the VVI/VVIR form of single-chamber pacing is more common.
AAI/AAIR pacing
AAI/AAIR pacing is indicated for patients who have isolated sinus node dysfunction and have no known or anticipated AV block. In an evaluation of the pacing mode selection across 18 studies with over 28 000 patients, AAI/AAIR pacing in patients with sinus node dysfunction resulted in prevention of ventricular dysfunction (secondary to chronic right apical pacing) and a lower rate of development of atrial fibrillation and chronic heart failure with lower mortality as compared with those with VVI pacing.8 13 However, the use of AAI/AAIR pacing is also associated with a lack of ventricular support should AV block occur and the risk of development of atrial fibrillation with slow ventricular response requiring ventricular pacing support. Consequently, this pacing mode is used rarely in the USA, where DDDR pacing (possibly with long AV delay) usually is preferred even when AV conduction is intact.14 But unnecessary RV pacing with its deleterious effects is a trade-off in many patients. Moreover, with the incidence of clinically significant AV node disease being less than 2% per year, AAI/AAIR pacing is a cost-effective alternative in patients with isolated sinus node dysfunction.15 It is crucial to understand that in a patient with SND and an intact AV node, even if AV block should occur at a later date, it is not a sudden, catastrophic event. Hence, in the rare instances of such an event, one could safely change to a dual-chamber pacemaker.
VVI/VVIR pacing
VVI/VVIR pacing is indicated for patients with chronic atrial arrhythmias that are not expected to return to sinus rhythm. While VVI/VVIR protects patients from lethal bradyarrhythmias, it does not maintain AV synchrony, which sometimes leads to “Pacemaker syndrome.”8 13
Retrospective uncontrolled studies have often indicated that atrial or dual-chambered pacing, which maintain AV synchrony, substantially reduce the stroke, atrial fibrillation, heart failure and mortality indicators as compared with VVI/VVIR pacing.15 In addition, controlled trials like the PASE (Pacemaker Selection in the Elderly) study,16 MOST (Mode Selection Trial) study17 and UK-PACE (United Kingdom Pacing and Cardiovascular Events) trial,18 have shown the relative merits of dual-chamber pacing over VVI/VVIR pacing.
However, VVI/VVIR pacemakers are still very commonly used in developing countries mainly because of the cost consideration and simplicity of implantation. Moreover, only a small percentage of patients with VVI/VVIR pacing develop LV dysfunction—the risk factors being elderly (age over 70 years) pre-existing or new CAD and pre-existing BBB or wide QRS complexes.19
Dual-chamber pacemakers
The VDD and the DDD/DDR pacing system are the two forms of dual-chamber pacing systems used in patients indicated for pacemaker therapy.
VDD pacing
The VDD pacing system is indicated in patients with intact sinus node function and AV block (acquired, congenital or postoperative) with near-normal structure of the heart. For patients with the above indications, the cardiologist has to choose between the VDD and DDD/DDR system. In an evaluation of the two pacing modalities, Wiegand et al had shown the VDD systems have a significantly shorter implantation time as compared with DDD systems (44 min versus 74 min, p<0.001), with lesser early and long-term complications and significantly lower overall costs.17 Thus, VDD pacing is indicated as a cost-effective alternative in patients with intact sinus node function and AV block (acquired, congenital or postoperative) with near-normal structure of the heart. One must realise that atrial sensing is rarely optimal with a single VDD lead. To improve atrial sensing, a VDD pacemaker can be used with two separate atrial and ventricular leads.
DDD/DDDR pacing
DDD/DDDR pacing is the obvious preferred option in patients with AV block. Several of these patients have sinus node dysfunction (intrinsic or drug-induced), and so a rate-responsive DDDR option is superior. Moreover, some patients may go on to develop SND later on as they age, and a DDDR pacing is of advantage in the long run.
However, a DDD/DDDR pacing also necessitates careful monitoring during both the implant procedure and follow-up, as it is associated with a higher rate of complications, atrial lead dislodgement and problems with ventricular leads. Also, as suggested by the MOST trial, the right ventricular apical pacing by the DDDR pacing contributes to ventricular dyssynchrony which often masks the advantage of AV synchrony provided by it, affecting the benefit in the primary outcome rates for DDD pacing versus VVI pacing modes.20 Placing a screw-in RV lead in the mid-high interventricular septum logically is better physiologically than RV apical pacing. While this practice is being followed in many centres, proof of concrete benefit is awaited. Optimisation of the mode-switching feature is of importance in DDD/DDDR pacing, as in the MOST trial, the incidence of heart failure in DDD pacing was closely related to the percentage of ventricular paced beats.20
Selection of the appropriate pacemaker
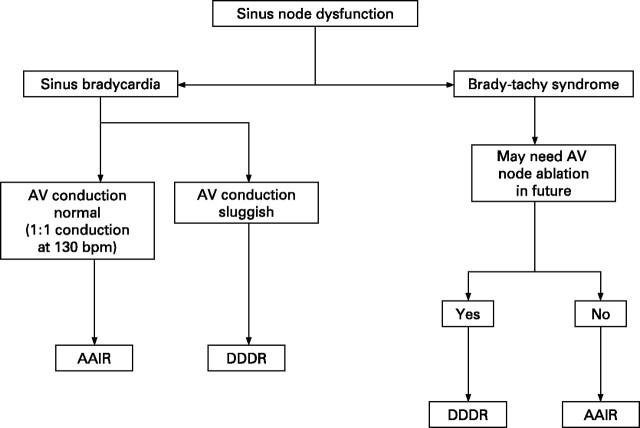
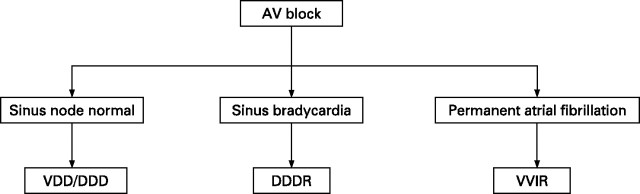
From the various pacing modes available, the selection of the pacing mode should be based on an individual approach that takes into consideration the patient's quality of life, potential clinical outcome and the complication rates of the procedure. Choosing the appropriate pacemaker with relation to electrical considerations must take into account the atrial rhythm status, status of AV conduction and presence of chronotropic competence.21 An indicative algorithm (figs 1, 2) categorising the various patient subgroups could be useful in objectively selecting the appropriate pacemaker.
Figure 1.
Selection of the pacemaker mode in sinus node dysfunction. AV, atrioventricular.
Figure 2.
Selection of the pacemaker mode in atrioventricular (AV) block.
Cardiac resynchronisation therapy (CRT) or biventricular pacing
The term “cardiac resynchronisation” was first used in 1994 when Cazeau and colleagues used epicardial leads on all four cardiac chambers to modify the ventricular activation sequence and improve haemodynamic performance in heart failure due to dilated cardiomyopathy accompanied by LBBB.22
Presently, CRT or biventricular pacing therapy is indicated for Class 3 or 4 patients with dilated cardiomyopathy and left ventricular dyssynchrony caused by left bundle branch block.
Various selection criteria have been evaluated to determine the patient subgroups which will respond the most to CRT. These criteria include QRS duration, advanced heart failure symptoms, non-ischaemic cardiomyopathy or permanent atrial fibrillation.23 24 The determinant of the improvements obtained with CRT in these studies has been the improvement in ventricular dyssynchrony. In patients with wide QRS complexes, approximately 70% show haemodynamic improvement with CRT.24 Also, patients with more advanced heart failure symptoms as compared with patients with less severe symptoms, patients with non-ischaemic cardiomyopathy as compared with patients with ischaemic cardiomyopathy and patients with LBBB as compared with patients with RBBB respond more consistently to CRT.24 25
Implantable cardioverter defibrillator (ICD)
ICDs provide immediate cardioversion/defibrillation in patients who have not yet experienced life-threatening ventricular tachyarrhythmias (primary prevention) but have a high risk for sudden cardiac death (SCD) and in patients who have already experienced a life-threatening ventricular tachyarrhythmia (secondary prevention). In the 2008 ACC/AHA “Guidelines for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices,” ICD therapy is mainly recommended in:15
survivors of cardiac arrest due to ventricular fibrillation or haemodynamically unstable sustained VT after evaluation to define the cause of the event and to exclude any completely reversible causes;
structural heart disease and spontaneous sustained VT, whether haemodynamically stable or unstable;
syncope of undetermined origin with clinically relevant, haemodynamically significant sustained VT or ventricular fibrillation induced at electrophysiological study;
LVEF less than 35% due to prior myocardial infarction who are at least 40 days postmyocardial infarction or with non-ischaemic dilated cardiomyopathy and are in NYHA functional Class II or III;
LV dysfunction due to prior myocardial infarction who are at least 40 days postmyocardial infarction, have an LVEF less than 30% and are in NYHA functional Class I;
non-sustained VT due to prior myocardial infarction, LVEF less than 40%, and inducible ventricular fibrillation or sustained VT at electrophysiological study.
Automated ICDs can also induce a high-rate, overdrive antitachycardia pacing (ATP) which effectively terminates ventricular tachycardia. For patients with haemodynamically tolerated ventricular tachycardia (generally <200 bpm), ATP is the preferred choice for initial therapy because it has a success rate greater than 90% in terminating ventricular tachycardia.26
However, from the perspective of developing countries, the above indications are highly unrealistic. Even several developed countries do not follow these sweeping indications, especially for primary prevention. There have also been several criticisms of using ICDs as per the MADIT-II guideline. For instance, a vast majority of the patients who received an ICD “prophylactically” after a large MI never utilised these devices.27 28 Moreover, 10% of these patients received unnecessary, inappropriate, highly disturbing shocks from the ICD. Using solely the LVEF as a guide is fraught with fallacies. Who measured the EF? How was it measured? When was it measured? What about other parameters—the clinical class, the QRS width, the LV volume over time, etc? It would be more prudent to identify the high-risk patients and weed out the low-risk subgroup. Modalities such as Holter (showing NSVT),29 microvolt T wave alternans,30 signal-averaged ECG31 and EP study32 are of some utility for these purposes. Personally we do not advocate ICDs for primary prevention of SCD in the post-MI group.
Koller et al followed up 442 patients postimplant for 7 years. Only 52% of patients received appropriate ICD therapy.33 The cost-effectiveness of the ICD would be greatly enhanced if patients highly unlikely to receive life-saving device therapy could be accurately screened out before implantation.
Combination of cardiac resynchronisation and defibrillation therapy (CRT-D)
The proportion of CRTs and ICDs in the total number of implantable cardiac devices utilised has increased exponentially over the years with their increasing capabilities and defined target population. In addition, the overall therapeutic and mortality benefits of CRT has been widened when used along with ICD therapy (CRT-D). Three studies of CRT-ICDs involving more than 2500 patients, the MIRACLE CD, CONTAK CD and COMPANION trials, have evaluated various endpoints of CRT-D therapy in different patient subgroups.34–36 The COMPANION trial, in particular, used CRT with and without prophylactic ICD backup in 1520 patients with advanced heart failure and bundle branch block in addition to optimised medical therapy and found a significant reduction in total mortality in heart failure recipients of CRT-ICDs.35
These studies confirm that while ICD and CRT have their individual merits, the quality of life and functional status of patients with an EF≤35%, a QRS width of ≥120 ms and NYHA class III or IV symptoms refractory to optimal medical therapy are remarkably improved when given a CRT combined with a defibrillator backup.36
However, one needs to be critical in analysing the basis for these recommendations. Though the recommendation is for LVEF<35%, the mean LVEF of the patients actually included in the trials was much lower (eg, 23 (SD 6.9)% in the CRT-D group and 22 (6.8)% in the CRT group in the COMPANION trial).35 Also, the QRS width of the patients in the trials was much higher (eg, 159 (24) ms in the CRT-D group and 159 (25) ms in the CRT group in the COMPANION trial).35 Moreover, an overwhelming majority had LBBB. Thus, the recommendations are not accurately commensurate with the facts.
Conclusion
While the need for pacemakers is increasing, not all patients who require pacemakers are receiving them, especially in the Asia-Pacific region. The precise indication is not the only factor which is associated with the selection of pacemaker type; age and economic resources play a significant role.
The current pacemaker guidelines for mode selection are to preserve AV synchrony with atrial or AV sequential pacing in the absence of permanent atrial fibrillation. In developing countries, with limited healthcare resources, ventricular pacing devices may be used as a cost-effective alternative.
There is an underutilisation of the excellent AAIR pacing mode for symptomatic SND. Evidence-based practice now supports the fact that atrial-based pacing reduces the incidence of atrial fibrillation and that continuous right ventricular pacing increases the risk of heart-failure progression.37 Therefore, all attempts to avoid unnecessary right ventricular pacing by implementing strategies to preserve normal ventricular activation are recommended.
The selection and use of the pacing devices will also be influenced by the improvement in technology resulting in new stratifications of the target patient population and cost reductions in the simpler pacing devices, which will increase the number of target patients receiving pacemakers.
We need to be more critical in advising the use of more expensive devices like ICDs and CRT/CRT-D devices, since most patients in the Asia-Pacific region pay out of pocket for these therapies. In this context, the AHA-ACC guidelines need not be blindly followed, since they are too wide-sweeping. They are based often on the intention-to-treat basis of trials rather than on the parameters of the patients actually enrolled.
Footnotes
Competing interests: None.
References
- 1.Furman S, Robinson G. Use of an intracardiac pacemaker in the correction of total heart block. Surg Forum 1958;9:245–8. [PubMed] [Google Scholar]
- 2.Altemose GT, Groh WJ. Assessment of electrical devices for arrhythmia control and prevention: past and future. ACC Curr J Rev 1999;8:47–50. [Google Scholar]
- 3.Charles RG. Prospective randomized trials on pacing mode: What have we learned? Am J Cardiol 2000;86(Suppl):116–118K. [DOI] [PubMed] [Google Scholar]
- 4.Wilkoff BL, Auricchio A, Brugada J, et al. HRS/EHRA expert consensus on the monitoring of cardiovascular implantable electronic devices (CIEDs): description of techniques, indications, personnel, frequency and ethical considerations. Heart Rhythm 2008;5:907–25. [DOI] [PubMed] [Google Scholar]
- 5.Maisel WH, Moynahan M, Zuckerman BD, et al. Pacemaker and ICD generator malfunctions: analysis of Food and Drug Administration annual reports. JAMA 2006;295:1901–6. [DOI] [PubMed] [Google Scholar]
- 6.Mond HG, Irwin M, Ector H, et al. The world survey of cardiac pacing and cardioverter-defibrillators: calendar year 2005 an International Cardiac Pacing and Electrophysiology Society (ICPES) project. Pacing Clin Electrophysiol 2008;31:1202–12. [DOI] [PubMed] [Google Scholar]
- 7.Mond HG, Irwin M, Morillo C, et al. The world survey of cardiac pacing and cardioverter defibrillators: calendar year 2001. Pacing Clin Electrophysiol 2004;27:955–64. [DOI] [PubMed] [Google Scholar]
- 8.Glikson M, Hayes DL. Cardiac pacing: a review. Med Clin N Am 2001;85:369–421. [DOI] [PubMed] [Google Scholar]
- 9.Raj SR, Sheldon RS. Role of pacemakers in treating neurocardiogenic syncope. Curr Opin Cardiol 2003;18:47–52. [DOI] [PubMed] [Google Scholar]
- 10.Brignole M, Sartore B, Barra M, et al. Is DDD superior to VVI pacing in mixed carotid sinus syndrome? An acute and medium-term study. Pacing Clin Electrophysiol 1988;11(11 Pt 2):1902–10. [DOI] [PubMed] [Google Scholar]
- 11.Lamas GA, Ellenbogen KA, Hennekens CH, et al. Evidence base for pacemaker mode selection from physiology and randomized trials. Circulation 2004;109:443–51. [DOI] [PubMed] [Google Scholar]
- 12. Central Intelligence Agency. The 2008 World Fact Book. Central Intelligence Agency Web site. https://www.cia.gov/library/publications/the-world-factbook/ (accessed 3 Dec 2008). [Google Scholar]
- 13.Tang CY, Kerr CR, Connally SJ. Clinical trials of pacing mode selection. Cardiol Clin 2000;18:1–23. [DOI] [PubMed] [Google Scholar]
- 14.Bemstein AD, Parsonnet V. Survey of cardiac pacing and defilbrillation in the United States in 1993. Am J Cardiol 1996;78:187. [PubMed] [Google Scholar]
- 15.Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Circulation 2008;117:2820–40. [DOI] [PubMed] [Google Scholar]
- 16.Lamas GA, Orav EJ, Stambler BS, et al. Quality of life and clinical outcomes in elderly patients treated with ventricular pacing as compared with dual-chamber pacing. Pacemaker Selection in the Elderly Investigators. New Engl J Med 1998;338:1097. [DOI] [PubMed] [Google Scholar]
- 17.Wiegand UK, Potratz J, Bode F, et al. Cost-effectiveness of dual chamber pacemaker therapy: does single lead VDD pacing reduce treatment costs of atrioventricular block? Eur Heart J 2001;22:174–80. [DOI] [PubMed] [Google Scholar]
- 18.Castelnuovo E, Stein K, Pitt M, et al. The effectiveness and cost-effectiveness of dual-chamber pacemakers compared with single-chamber pacemakers for bradycardia due to atrioventricular block or sick sinus syndrome: systematic review and economic evaluation. Health Technol Assess 2005;9:iii, xi–xiii, 1–246. [DOI] [PubMed] [Google Scholar]
- 19.Sweeney MO, Prinzen FW. A new paradigm for physiologic ventricular pacing. J Am Coll Cardiol 2006;47:282–8. [DOI] [PubMed] [Google Scholar]
- 20.Sweeney MO, Hellkamp AS, Ellenbogen KA, et al. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation 2003;107:2932–7. [DOI] [PubMed] [Google Scholar]
- 21.Lamas GA, Ellenbogen KA, Hennekens CH, et al. Evidence base for pacemaker mode selection from physiology and randomized trials. Circulation 2004;109:443–51. [DOI] [PubMed] [Google Scholar]
- 22.Cazeau S, Ritter P, Bakdach S, et al. Four chamber pacing in dilated cardiomyopathy. Pacing Clin Electrophysiol 1994;17:1974–9. [DOI] [PubMed] [Google Scholar]
- 23.Kadhiresan V, Vogt J, Auricchio A, et al. Sensitivity and specificity of QRS duration to predict acute benefit in heart failure patients with cardiac resynchronization [Abstract]. Pacing Clin Electrophysiol 2000;23(II):555. [Google Scholar]
- 24.Abraham WT, Fisher WG, Smith AL, et al. Cardiac resynchronization in chronic heart failure. New Engl J Med 2002;346:1845–53. [DOI] [PubMed] [Google Scholar]
- 25.Higgins SL, Hummel JD, Niazi IK, et al. Cardiac resynchronization therapy for the treatment of heart failure and intraventricular conduction delay and malignant ventricular tachyarrhythmia. J Am Coll Cardiol 2003;42:1454–9. [DOI] [PubMed] [Google Scholar]
- 26.Newman D, Dorian P, Hardy J. Randomized controlled comparison of antitachycardia pacing algorithms for termination of ventricular tachycardia. J Am Coll Cardiol 1993;21:1413–18. [DOI] [PubMed] [Google Scholar]
- 27.Hohnloser SH. Don't rush to implant ICDs after MI in high-risk patients. J Watch Cardiol 2005. http://cardiology.jwatch.org/cgi/content/citation/2005/128/3 (accessed 9 Oct 2008). [Google Scholar]
- 28.Gillis AM. Prophylactic implantable cardioverter-defibrillators after myocardial infarction—not for everyone. New Engl J Med 2004;351:2540–2. [DOI] [PubMed] [Google Scholar]
- 29.Stein KM.Noninvasive risk stratification for sudden death: signal-averaged electrocardiography, nonsustained ventricular tachycardia, heart rate variability, baroreflex sensitivity, and QRS duration. Prog Cardiovasc Dis 2008;51:106–17. [DOI] [PubMed] [Google Scholar]
- 30.Chow T, Kereiakes DJ, Bartone C, et al. Microvolt T-wave alternans identifies patients with ischemic cardiomyopathy who benefit from implantable cardioverter-defibrillator therapy. J Am Coll Cardiol 2007;49:50–8. [DOI] [PubMed] [Google Scholar]
- 31.Odemuyiwa O, Malik M, Poloniecki J, et al. Frequency versus time domain analysis of signal-averaged electrocardiograms: III. Stratification of postinfarction patients for arrhythmic events. J Am Coll Cardiol 1992;20:144–50. [DOI] [PubMed] [Google Scholar]
- 32.Mittal S, Iwai S, Stein KM, et al. Long-term outcome of patients with unexplained syncope treated with an electrophysiologic-guided approach in the implantable cardioverter–defibrillator era. J Am Coll Cardiol 1999;34:1082–9. [DOI] [PubMed] [Google Scholar]
- 33.Koller MT, Schaer B, Wolbers M, et al. Death without prior appropriate implantable cardioverter-defibrillator therapy: a competing risk study. Circulation 2008;117:1918–26. [DOI] [PubMed] [Google Scholar]
- 34.Young JB, Abraham WT, Smith AL, et al. Combined cardiac resynchronization and implantable cardioversion defibrillation in advanced chronic heart failure: the MIRACLE ICD Trial. JAMA 2003;289:2685–94. [DOI] [PubMed] [Google Scholar]
- 35.Bristow MR, Saxon LA, Boehmer J, et al. Cardiac-resynchronization therapy with or without an implantable defibrillator in advanced chronic heart failure. New Engl J Med 2004;350:2140–50. [DOI] [PubMed] [Google Scholar]
- 36.Al-Khatib SM, Sanders GD, Mark DB, et al. Implantable cardioverter defibrillators and cardiac resynchronization therapy in patients with left ventricular dysfunction: Randomized trial evidence through 2004. Am Heart J 2005;149:1020–34. [DOI] [PubMed] [Google Scholar]
- 37.Sweeney M. Minimizing right ventricular pacing: A new paradigm for cardiac pacing in sinus node dysfunction. Am Heart J 2007;153(4 Suppl):34–43S. [DOI] [PubMed] [Google Scholar]