Abstract
Background
Although associations between risk factors such as hypertension and hypercholesterolaemia, and cardiovascular disease (CVD) are well-established it is not known to what extent these associations are similar in people from different ethnicities or regions. This study aims to measure the contributions of systolic blood pressure (SBP) and total cholesterol (TC) to ischaemic heart disease (IHD) and stroke in the Thai population.
Methods and results
Data from a Thai cohort study were used for analyses. Participants were 2702 males and 797 females aged between 35 and 54 years at the start of study in 1985. Cox Proportional Hazards Models were used to assess RRs of IHD or stroke associated with SBP or TC stratified by age at the time of an event of 30–44, 45–59, and 60–69 years. During the 17 years of follow-up, 96 IHD (40 non-fatal, 56 fatal), 69 strokes (32 non-fatal and 37 fatal) occurred. Each 1 mmol/l increase in TC was associated with a fivefold increase in IHD risk in people aged 30–44 years, but not with significant increase in stroke risk in any age group. The RRs (95% CIs) of IHD per 10 mm Hg increase in SBP were 1.31 (1.04 to 1.64) and 1.46 (1.15 to 1.87), and of stroke, 1.40 (1.10 to 1.79) and 1.85 (1.40 to 2.45) in people aged 45–59 and 60–69 years, respectively.
Conclusions
Increases in IHD and stroke risks associated with these two risk factors observed in Thailand are comparable with those in the Asia Pacific and western populations.
Keywords: Blood pressure, cholesterol, ischaemic heart disease, stroke, cardiovascular disease
Introduction
The associations between a range of risk factors such as high blood pressure, high cholesterol, smoking, insufficient physical activity, and overweight and cardiovascular disease (CVD) are well-established.1–7 Cohort studies based mainly in industrialised countries have indicated that a reduction in serum cholesterol of 0.6 mmol/l reduced the incidence of ischaemic heart disease by 54%, 39%, 27%, 20%, and 19% at age 35–44, 45–54, 55–64, 65–74, 75–84 years, respectively.8 In the Asia-Pacific region each 1 mmol/l higher level of total cholesterol was associated with 35% increased risk of coronary death, 25% increased risk of fatal or non-fatal ischaemic stroke, and 20% decreased risk of fatal haemorrhagic stroke.1 In China and Japan, each 5 mmHg decrease in diastolic blood pressure was associated with 39% lower risk of non-haemorrhagic stroke and 46% lower risk of haemorrhagic stroke.9 In the US, high-normal blood pressure, as compared with optimal blood pressure, was associated with a risk-factor–adjusted HR for cardiovascular disease of 2.5 (95% CI 1.6 to 4.1) in women and 1.6 (95% CI 1.1 to 2.2) in men among 6859 participants in the Framingham Heart Study who were initially free of hypertension and cardiovascular disease.10 However, it is not known to what extent these associations are similar in people from different ethnicities and levels of socio-economic development. Though several studies reported these associations, the results cannot be compared directly because of differences in the adjustment for other covariates and the use of usual versus baseline blood pressure or cholesterol.11
The comparative assessment of associations between a disease and various risk factors in different regions is warranted because the information can aid in more accurate comparisons of population health problems between different parts of a country or regions of the world.12 Consequently, it can help to assess the potential health gains from interventions that reduce exposure to risk factors.13 For example, WHO used the associations between cholesterol and ischaemic heart disease or stroke from specific regions in the assessment of the global and regional burden of high cholesterol for all regions of the world for the year 2000.8 14 In Thailand, the same framework was used to estimate the burden attributable to high blood pressure, high cholesterol and other risk factors in 1999. It was found that non-optimal blood pressure accounted for 5% and non-optimal cholesterol for 2% of the total burden of disease in the country.15 However, these estimates remain somewhat uncertain until the disease burden has been assessed based on local data on the associations of risk factors with disease outcomes.
This study assessed the RRs of ischaemic heart disease or stroke associated with blood pressure or cholesterol in a sample of the Thai population, and investigated whether the associations differ between Thailand and other areas.
Methods
Cohort
The Electricity Generating Authority of Thailand (EGAT) cohort study followed the EGAT employees over 17 years for the occurrence of health outcomes including ischaemic heart disease and stroke. The methodology used has previously been described.16 In brief, participants were aged between 35 and 54 years at baseline (1985) with 2702 males and 797 females. Assessments including physical examinations and laboratory tests were performed in 1985 and 1997.
Data used in this analysis were based on 17 years of follow-up between 1985 and 2002. Consent and ethical approval were obtained.16
Risk factors
Risk factors considered in the analyses were systolic blood pressure (SBP) (in mmHg) and total cholesterol (TC) (in mmol/l). Blood pressure was measured after 5 min rest, using a calibrated mercury sphygmomanometer with systolic blood pressure (SBP) and diastolic blood pressure (DBP) recorded as the first and fifth Korotkoff sounds respectively. Blood samples were obtained after a 12 h overnight fast. Serum total cholesterol was measured using enzymatic calorimetric assays (Boehringer Mannheim, Mannheim, Germany).16
Endpoints
Ischaemic heart disease encompassed fatal and non-fatal myocardial infarction, surgical revascularisation and silent myocardial infarction. Stroke included fatal and non-fatal ischaemic or haemorrhagic subtypes. These outcomes were ascertained by physical examinations and reviewing detailed medical treatment history during the follow-up in 1997 by three cardiologists, one neurologist and one gastroenterologist. Fatal CVD cases were confirmed by an independent adjudication committee of two cardiologists, one neurologist, one gastroenterologist and one internist, based upon all available evidence and using international criteria. Information about the likely cause of death was sought through a review of information obtained from interviews with relatives and colleagues, medical notes, medical insurance reimbursement claims, records of hospital admissions and death certificates.16
Statistical analysis
Cox Proportional Hazard Models were used to determine the RR of each risk factor individually for IHD and stroke outcomes with total cholesterol, SBP and smoking as covariates, in a similar manner to the Asia Pacific Cohort Studies Collaboration (APCSC) and Law et al studies that served as inputs to the WHO Comparative Risk Assessment (CRA).8 14 Age was used as a time-dependent variable in order to assess changes in hazards as individuals' age increases.17 18 We excluded one case above these age ranges (aged 70+ years) from the analyses and presented the results for three age groups at which the events occurred (30–44, 45–59 and 60–69 years). The most recent pre-event measurement was used to determine the risk factor exposure in the EGAT study. All analyses were undertaken using the STATA8 software package (Stata Corp LP, College Station, Texas).
Regression dilution bias
In general, baseline blood pressure or cholesterol measures are subject to random fluctuation over time because of measurement error or intraindividual variation. Measurement error occurs as a result of imperfect instruments or observer bias. Intraindividual variation, such as in blood pressure, is due to diet, ambient temperature, or the patient's position before the measurement.19 Measurement error results in an underestimation of RRs. This error is called ‘regression dilution bias.’ Studies reported that the associations (regression coefficients) were underestimated by approximately 70–80%14 20 and 60–70%19 20 when only one measurement of SBP and TC was used, respectively. The bias can be prevented by repeating the measurements at a later point in time. This is expensive and impractical. Alternatively, the bias can be reduced by using attenuation factors obtained in previous studies that did have repeated measurements. In this analysis, an attenuation factor of 1.84 was used for the adjustment of the regression coefficients between SBP and IHD or stroke,18 1.61 for TC and IHD, and 1.8 for TC and stroke.17 The adjusted RR of IHD or stroke associated with SBP or TC is calculated with the following equation:
Results
Baseline characteristics of the cohort
Compared with no IHD, participants with IHD were older at baseline, had higher prevalence of diabetes mellitus and smoking, and had higher levels of systolic and diastolic blood pressure and total cholesterol. Similarly, participants with stroke had higher levels of systolic and diastolic blood pressure, and a higher prevalence of smoking and diabetes mellitus than participants without stroke. However, patients with stroke did not have a higher level of total cholesterol than people without stroke. People who later developed IHD or stroke did not differ in alcohol consumption from people who remained free of these two conditions (table 1). During the 17 years of follow-up, there were 96 ischaemic and 69 stroke cases in the EGAT cohort. The majority of events occurred at ages 45–59 years (table 2).
Table 1.
Baseline characteristics of the cohort by incident ischaemic heart disease (IHD) and stroke
| IHD | Stroke | |||||
|---|---|---|---|---|---|---|
| Characteristic | New IHD | No IHD | p Value | New stroke | No stroke | p Value |
| n | 96 | 3400 | 69 | 3429 | ||
| Sex (percentage men) | 90.6 | 76.9 | <0.001 | 87.1 | 77.1 | 0.013 |
| Age (years) | 46.1 (0.58) | 42.9 (0.09) | <0.001 | 45.4 (0.61) | 43.0 (0.09) | <0.001 |
| Systolic blood pressure (mmHg) | 129.6 (2.11) | 120.5 (0.28) | <0.001 | 132.0 (2.49) | 120.5 (0.28) | <0.001 |
| Diastolic blood pressure (mmHg) | 81.0 (1.35) | 75.1 (0.19) | <0.001 | 83.2 (1.83) | 75.1 (0.19) | <0.001 |
| Total cholesterol (mmol/l) | 6.11 (0.13) | 5.75 (0.02) | 0.006 | 5.71 (0.13) | 5.78 (0.02) | 0.65 |
| Diabetes mellitus (%) | 21.9 | 6.4 | <0.001 | 14.3 | 6.7 | 0.013 |
| Current smokers (%) | 55.2 | 43 | 0.02 | 58.6 | 43 | 0.009 |
| Current alcohol drinker (%) | 56.3 | 65.5 | 0.06 | 70 | 65.1 | 0.41 |
Data are percentages or means±SD. Total n=3499. p Values for dichotomous outcomes were based on Pearson χ2; p values for continuous outcomes were based on an F test.
Table 2.
Number of ischaemic heart disease (IHD) and stroke cases by age at event
| IHD | Stroke | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | All IHD | Male | Female | All stroke | |||||
| Age (years) | Non-fatal | Fatal | Non-fatal | Fatal | Non-fatal | Fatal | Non-fatal | Fatal | ||
| 30–44 | 0 | 3 | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 |
| 45–59 | 23 | 28 | 3 | 4 | 58 | 20 | 19 | 5 | 2 | 46 |
| 60–69 | 12 | 20 | 2 | 0 | 34 | 6 | 15 | 1 | 1 | 23 |
| 70 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Total | 35 | 52 | 5 | 4 | 96 | 26 | 34 | 6 | 3 | 69 |
Associations between risk factors and cardiovascular diseases
There were significant associations between systolic blood pressure and ischaemic heart disease in Thai people aged 45–49 and 60–69 years, but not in those aged 30–44 years. The associations were strongest in the oldest age group. The risk of stroke rose with systolic blood pressure in both age groups 45–59 and 60–69 years. The RRs of stroke associated with changes in blood pressure could not be estimated for the youngest age group because there were too few stroke events (table 3).
Table 3.
RR of ischaemic heart disease and stroke per 10 mmHg increase in systolic blood pressure by age at event
| Ischaemic heart disease | Stroke | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age group (years) | RR* | LL | UL | RR† | LL | UL | RR* | LL | UL | RR† | LL | UL |
| 30–44 | 1.23 | 0.56 | 2.69 | 1.45 | 0.34 | 6.19 | NA | NA | NA | NA | NA | NA |
| 45–59 | 1.16 | 1.02 | 1.31 | 1.31 | 1.04 | 1.64 | 1.2 | 1.05 | 1.37 | 1.4 | 1.1 | 1.79 |
| 60–69 | 1.23 | 1.08 | 1.41 | 1.46 | 1.15 | 1.87 | 1.4 | 1.2 | 1.63 | 1.85 | 1.4 | 2.45 |
*Adjusted for smoking and total cholesterol.
†Adjusted for smoking and total cholesterol and corrected for regression dilution bias.
LL, lower limit of 95% CI; UL, upper limit of 95% CI.
The RR per 1 mmol/l increase in total cholesterol for IHD in the EGAT cohort was 6.3 (95% CI 1.6 to 25.0) for age group 30–44 years. This was a significant association. However, the associations of IHD and total cholesterol at older ages were not statistically significant. There were too few stroke cases for the estimation of the RRs of stroke associated with changes in total cholesterol in age group 30–44 years. At older ages, total cholesterol was not significantly associated with all stroke combined (table 4).
Table 4.
RR of ischaemic heart disease and stroke per 1 mmol/l increase in total cholesterol by age at event
| Ischaemic heart disease | Stroke | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age group | RR* | LL | UL | RR† | LL | UL | RR* | LL | UL | RR† | LL | UL |
| 30–44 | 3.14 | 1.33 | 7.38 | 6.3 | 1.59 | 24.99 | NA | NA | NA | NA | NA | NA |
| 45–59 | 1.09 | 0.87 | 1.36 | 1.15 | 0.8 | 1.64 | 0.91 | 0.7 | 1.17 | 0.84 | 0.53 | 1.34 |
| 60–69 | 1.05 | 0.87 | 1.36 | 1.08 | 0.8 | 1.64 | 0.78 | 0.52 | 1.18 | 0.64 | 0.3 | 1.35 |
*Adjusted for smoking and systolic blood pressure.
†Adjusted for smoking and systolic blood pressure and corrected for regression dilution bias.
LL, lower limit of 95% CI; UL, upper limit of 95% CI.
Discussion
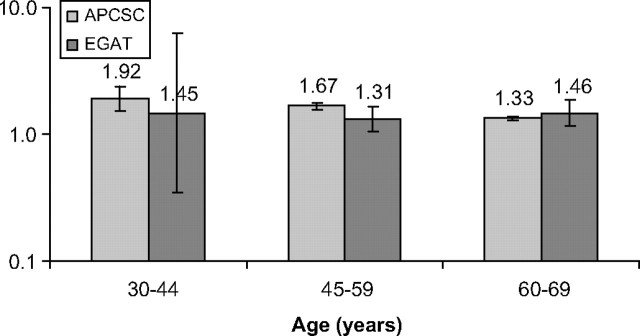
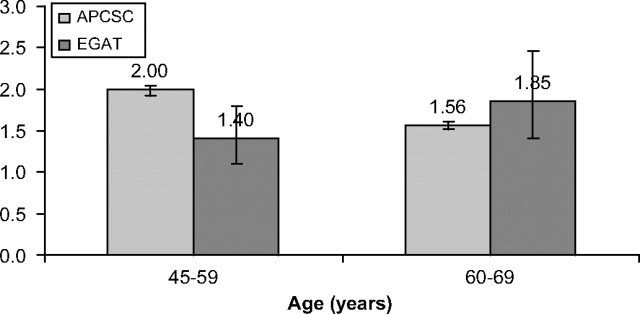
Overall, the RR estimates are similar across risks factors and outcomes between Thailand and the Asia Pacific region18 or western countries.17 The strengths of the associations between SBP and IHD were similar to those in the APCSC study, as all 95% CIs of RRs overlap between the two studies in all three age groups. Risk of stroke associated with systolic blood pressure was comparable with that reported in the APCSC study for age group 60–69 years with a somewhat weaker association in age group 45–59 years18 (see appendix, table 1 and figures 1, 2).
Figure 1.
Comparison of the relative risks of ischemic heart disease associated with increase in systolic blood pressure between the Asia Pacific Cohort Study Collaboration study and the Electricity Generating Authority of Thailand study.
Figure 2.
Comparison of the relative risks of stroke associated with increase in systolic blood pressure between the Asia Pacific Cohort Study Collaboration study and the Electricity Generating Authority of Thailand study.
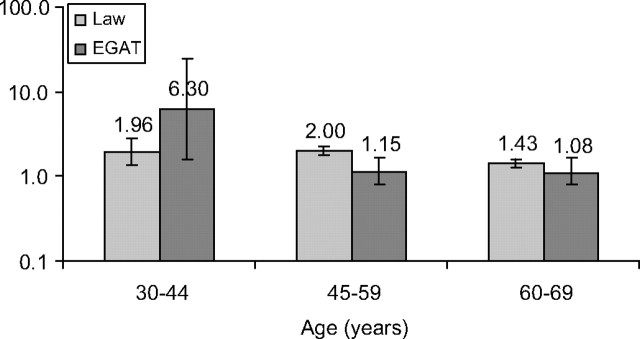
Similarly, the RR for TC in association with IHD was significantly lower in the EGAT than in the CRA study for the 45–59 year age group17 (see appendix, table 1 and figure 3). These differences may be due to chance because the number of the events was small, and the RRs in age group 60–69 years did not differ between the two studies.
Figure 3.
Comparison of the relative risks of ischemic heart disease associated with increase in total cholesterol between the Law et al. study and the Electricity Generating Authority of Thailand study.
No comparisons were made between APCSC and EGAT for the RRs of stroke associated with TC because it was not possible to distinguish between ischaemic and haemorrhagic subtypes in the EGAT study. However, the absence of a significant association between total cholesterol and all stroke in the Thai cohort may be due to the higher proportion of haemorrhagic stroke subtype compared with the Western populations.21 This may be a result of high alcohol consumption,22 especially among Thai men,23 as the risks of haemorrhagic stroke more than double for light drinkers and nearly triple for heavy drinkers compared with non-drinkers.24
A greater proportion of haemorrhagic strokes dilutes the association between total cholesterol and total stroke; the association between serum cholesterol and ischaemic stroke is positive, whereas haemorrhagic stroke is not associated with total cholesterol25 (and may even be inversely related to cholesterol).1 It is also likely that high sodium salt consumption through the use of food condiments such as fish or soy sauce plays a major role in the higher proportion of haemorrhagic stroke in Thai people.9
Limitations
In the EGAT study, it was not possible to look at ischaemic versus haemorrhagic stroke outcomes separately because a large proportion of strokes were of an undetermined type. The EGAT study represents only the upper middle class population; this group of people may not be representative of all Thais. Moreover, the analysis is dominated by male participants because of the small number of female employees in the EGAT study. In addition to these problems of representativeness, the EGAT study suffers from a small number of CVD events. This results in wide CIs around the RRs.
Conclusions
The associations of cholesterol and blood pressure with IHD and stroke in Thailand are comparable with those observed in other countries in the Asia Pacific region or in the Western world. In the absence of a larger and more representative cohort study, it is reasonable to assume that the RRs of IHD and stroke used in the WHO's CRA also apply in Thailand. It is also reasonable to assume that the interventions to lower exposure to non-optimal blood pressure and cholesterol such as medications or salt intake reduction observed in other regions will have similar effects in Thailand. The information will contribute to further analyses of the cost-effectiveness of blood pressure and cholesterol-lowering interventions to prevent cardiovascular disease. This, in turn, will inform decision-making on the allocation of health sector resources.
Appendix.
Table AI.
RR of cardiovascular disease associated increase in systolic blood pressure and total cholesterol
| Ischaemic heart disease associated with 10 mmHg increase in systolic blood pressure (APCSC) | Stroke associated with 10 mmHg increase in systolic blood pressure (APCSC) | Ischaemic heart disease associated with 1 mmol/l increase in cholesterol (Law et al19) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Age group (years) | RR | LL | UL | RR | LL | UL | RR | LL | UL |
| 30–44 | 1.92 | 1.54 | 2.38 | 2.38 | 2.13 | 2.63 | 1.96 | 1.37 | 2.78 |
| 45–59 | 1.67 | 1.56 | 1.75 | 2.00 | 1.92 | 2.04 | 2.00 | 1.79 | 2.22 |
| 60–69 | 1.33 | 1.27 | 1.39 | 1.56 | 1.52 | 1.61 | 1.43 | 1.27 | 1.61 |
LL, UL, Lower and upper limits of 95% CI; APCSC, Asia Pacific Cohort Studies Collaboration.
Footnotes
Funding: Data analysis was conducted by the Setting Priorities Using Information on Cost-Effectiveness (SPICE) Project which is funded by Wellcome Trust, UK (071842/Z/03/Z) and the National Health and Medical Research Council of Australia (301199).
Competing interests: None.
Ethics approval: Ethics approval was provided by the Mahidol University of Thailand.
Contributors: This paper is the first reporting the strength of the relationship between two major risk factors, blood pressure and cholesterol, and cardiovascular disease in Thailand. It also compares the risk factor-disease relationship between Thailand and the Asia Pacific region and industrialised areas.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Zhang X, Patel A, Horibe H, et al. ; Asia Pacific Cohort Studies Collaboration. Cholesterol, coronary heart disease, and stroke in the Asia Pacific region. Int J Epidemiol 2003;32:563–72. [DOI] [PubMed] [Google Scholar]
- 2.Thrift AG, McNeil JJ, Forbes A, et al. Three important subgroups of hypertensive persons at greater risk of intracerebral hemorrhage. Hypertension 1998;31:1223–9. [DOI] [PubMed] [Google Scholar]
- 3.Woodward M, Zhang X, Barzi F, et al. ; Asia Pacific Cohort Studies Collaboration. The effects of diabetes on the risks of major cardiovascular diseases and death in the Asia-Pacific region. Diabetes Care 2003;26:360–6. [DOI] [PubMed] [Google Scholar]
- 4.Jousilahti P, Vartiainen E, Tuomilehto J, et al. Sex, age, cardiovascular risk factors, and coronary heart disease: a prospective follow-up study of 14 786 middle-aged men and women in Finland. Circulation 1999;99:1165–72. [DOI] [PubMed] [Google Scholar]
- 5.Jousilahti P, Tuomilehto J, Vartiainen E, et al. Body weight, cardiovascular risk factors, and coronary mortality: 15-year follow-up of middle-aged men and women in eastern Finland. Circulation 1996;93:1372–9. [DOI] [PubMed] [Google Scholar]
- 6.Asia Pacific Cohort Studies Collaboration. The impact of cardiovascular risk factors on the age-related excess risk of coronary heart disease. Int J Epidemiol 2006;35:1025–33. [DOI] [PubMed] [Google Scholar]
- 7.Asia Pacific Cohort Studies Collaboration. Joint effects of systolic blood pressure and serum cholesterol on cardiovascular disease in the Asia Pacific region. Circulation 2005;112:3384–90. [DOI] [PubMed] [Google Scholar]
- 8.Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ 1994;308:367–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anon. Blood pressure, cholesterol, and stroke in eastern Asia. Eastern Stroke and Coronary Heart Disease Collaborative Research Group. Lancet 1998;352:1801–7. [PubMed] [Google Scholar]
- 10.Vasan RS, Larson MG, Leip EP, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 2001;345:1291–7. [DOI] [PubMed] [Google Scholar]
- 11.Collins R, MacMahon S. Blood pressure, antihypertensive drug treatment and the risks of stroke and of coronary heart disease. Br Med Bull 1994;50:272–98. [DOI] [PubMed] [Google Scholar]
- 12.Ezzati M, Lopez AD, Rodgers A, et al. ; Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet 2002;360:1347–60. [DOI] [PubMed] [Google Scholar]
- 13.Ezzati M, Hoorn SV, Rodgers A, et al. Comparative Risk Assessment Collaborating Group. Estimates of global and regional potential health gains from reducing multiple major risk factors. Lancet 2003;362:271–80. [DOI] [PubMed] [Google Scholar]
- 14.Lawes CM, Rodgers A, Bennett DA, et al. ; Asia Pacific Cohort Studies Collaboration. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens 2003;21:707–16. [DOI] [PubMed] [Google Scholar]
- 15.The working group on burden of disease and injures associated with life styles and risk factors (in Thai). Burden of disease and injuries. Thailand: Ministry of Public Health, 1999. [Google Scholar]
- 16.Sritara P, Cheepudomwit S, Chapman N, et al. Twelve-year changes in vascular risk factors and their associations with mortality in a cohort of 3499 Thais: the Electricity Generating Authority of Thailand Study. Int J Epidemiol 2003;32:461–8. [DOI] [PubMed] [Google Scholar]
- 17.Lawes CMM, Vander Hoorn S, Law MR, et al. High cholesterol. In: Ezzati M, Lopez AD, Rodgers A, et al., eds. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors. Geneva: World Health Organization, 2004:391–496. [Google Scholar]
- 18.Lawes CMM, Vander Hoorn S, Law MR, et al. High blood pressure. In: Ezzati M, Lopez AD, Rodgers A, et al., eds. Comparative quantification of health risks: global and regional burden of disease attributable to selected major risk factors, Geneva: World Health Organization, 2004:281–390. [Google Scholar]
- 19.Law MR, Wald NJ, Wu T, et al. Systematic underestimation of association between serum cholesterol concentration and ischaemic heart disease in observational studies: data from the BUPA study. BMJ 1994;308:363–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Woodward M, Huxley H, Lam TH, et al. ; Asia Pacific Cohort Studies Collaboration. A comparison of the associations between risk factors and cardiovascular disease in Asia and Australasia. Eur J Cardiovasc Prev Rehabil 2005;12:484–91. [DOI] [PubMed] [Google Scholar]
- 21.Kitamura A, Nakagawa Y, Sato M, et al. Proportions of stroke subtypes among men and women >=40 years of age in an urban Japanese city in 1992, 1997, and 2002. Stroke 2006;37:1374–8. [DOI] [PubMed] [Google Scholar]
- 22.Juvela S, Hillbom M, Palomaki H. Risk factors for spontaneous intracerebral hemorrhage. Stroke 1995;26:1558–64. [DOI] [PubMed] [Google Scholar]
- 23.Aekplakorn W, Hogan MC, Tiptaradol S, et al. Tobacco and hazardous or harmful alcohol use in Thailand: joint prevalence and associations with socioeconomic factors. Addict Behav 2008;33:503–14. [DOI] [PubMed] [Google Scholar]
- 24.Donahue RP, Abbott RD, Reed DM, et al. Alcohol and hemorrhagic stroke. The Honolulu Heart Program. JAMA 1986;255:2311–14. [PubMed] [Google Scholar]
- 25.Ebrahim S, Sung J, Song YM, et al. Serum cholesterol, haemorrhagic stroke, ischaemic stroke, and myocardial infarction: Korean national health system prospective cohort study. BMJ 2006;333:22. [DOI] [PMC free article] [PubMed] [Google Scholar]