Abstract
Objective
The purpose of this study was to determine whether high-sensitivity C-reactive protein (hsCRP) levels differ among patients with acute aortic syndromes (AAS) and if hsCRP could predict their long-term outcomes.
Design
Retrospective observational study.
Setting
Cleveland Clinic Hospital, Cleveland, Ohio.
Patients
115 consecutive patients with AAS admitted to the cardiac intensive care unit.
Interventions
HsCRP and other laboratory data were measured within 24 h of admission. Demographic, imaging and laboratory data were obtained at the time of presentation. For the long-term survival analysis, the social security death index was used to determine all-cause mortality.
Main outcome measures
HsCRP levels among AAS patients.
Results
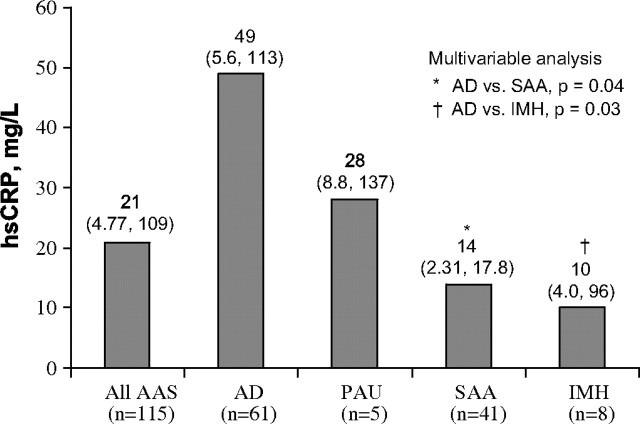
Hospital mortality was 4.3% for AAS patients. HsCRP levels differed significantly among AAS; the median hsCRP was higher in the aortic dissection group (49 mg/l) than in those with penetrating aortic ulcer (28 mg/l), symptomatic aortic aneurysm (14 mg/l), and intramural haematoma (10 mg/l); (p=0.02). In multivariable analysis, aortic dissection patients had higher hsCRP levels than intramural haematoma (p=0.03) and symptomatic aortic aneurysm (p=0.04) patients, after adjusting for age and gender. Multivariable Cox regression analyses showed that elevated hsCRP levels at presentation were associated with a higher long-term mortality (p=0.007).
Conclusions
Among patients with AAS, those with aortic dissection have the highest hsCRP levels at presentation. Elevated hsCRP independently predicted a higher long-term mortality in AAS patients.
Keywords: C Reactive protein, aortic diseases, aneurysm, dissecting, inflammation, aortic root disease, biochemical markers, cytokines, outcomes, vascular heart disease
Acute aortic syndromes (AAS), defined as aortic dissection (AD), intramural haematoma (IMH), penetrating aortic ulcer (PAU) and symptomatic aortic aneurysm (SAA), are acute processes which disrupt the aortic wall and carry the consequent risk of aortic rupture. Despite recent advances in more rapid and accurate diagnostic imaging techniques, these entities are associated with a poor prognosis unless rapid intervention occurs. There is increasing evidence that tissue-level inflammatory processes contribute to the development and progression of aortic diseases,1–3 and that circulating inflammatory markers are elevated in patients with aneurysmal diseases.3 4 Recent data have established an association between systemic inflammation, evident by high-sensitivity C-reactive protein (hsCRP) levels, and aortic atheromatous disease5 as well as asymptomatic aortic aneurysm.3 There is also evidence that elevated hsCRP levels at admission in patients with AAS may be associated with poor short-term prognosis.6 7 However, the role and extent of inflammation among the different AAS and its effect on long-term prognosis are not completely known. Therefore, the objective of the present study was to examine the diagnostic and long-term prognostic value of hsCRP in patients presenting with various types of AAS.
Methods
One hundred and fifteen consecutive patients with AAS admitted to the cardiac intensive care unit at Cleveland Clinic Hospital, Cleveland, Ohio between January 2001 and December 2003 were retrospectively identified. The primary condition of these patients included AD (n=61), SAA (n=41), IMH (n=8) and PAU (n=5). The diagnosis of AAS was ascertained based on clinical history, imaging modalities and direct surgical inspection. Imaging modalities included transoesophageal echocardiography, computed tomographic scanning, contrast angiography and magnetic resonance angiography. The aortic disease was classified according to the Stanford classification system based on either ascending or descending aortic involvement.
HsCRP and other laboratory data were measured at the time of presentation within 24 h of admission. HsCRP concentrations were assayed by immunonephelometry by the BNII analyser protocol (Dade Behring, Deerfield, Illinois) and determined with a typical detection limit of 0.175 mg/l (ultrasensitive CRP). Complete in-hospital follow-up was available for all patients. Demographic, clinical, laboratory, echocardiographic, radiographic and surgical data were obtained by database review or from the patients' medical records. All patients had a definitive diagnosis by at least one diagnostic imaging modality. Exclusion criteria included recent infection, vasculitis, malignancy, traumatic aortic disease and recent surgery. Study approval was obtained from the Cleveland Clinic institutional review board.
Statistical analysis
Continuous data are expressed as mean±SD and medians, 15th and 85th percentile values. Kruskal–Wallis non-parametric analysis of variance tests were used to analyse group differences for the continuous data. Categorical data are displayed as frequencies and percentages, and group comparisons were made using χ2 tests or Fisher exact tests where appropriate. Multivariable linear regression was used to determine factors associated with hsCRP and predictors of hospital length of stay. Logistic regression analysis was used to find possible associations of risk factors of hospital mortality. Various cutpoints of hsCRP were evaluated for the predictive ability of hsCRP within the four AAS groups. Threshold values of hsCRP were investigated to determine the accuracy in predicting AD versus the other three AAS. C-statistics, sensitivity, specificity, positive predictive values and negative predictive values are provided for tested cutpoints. The social security death index was used to determine all-cause mortality for the analysis of survival. Non-parametric survival estimates were obtained using the Kaplan–Meier method.8 Multivariable Cox regression analysis9 was used to find the effect of hsCRP on all-cause mortality.
In all analyses, variables were selected using a backward approach and a criterion of p<0.05 for retention in the final multivariable models. For further adjustment, age and gender were added to the models. Because the distributions for the measurements of hsCRP were skewed, natural log transformations were used in the analysis. Statistical analyses were performed using SAS version 9.1.
Results
Multiple modalities were used in the diagnosis of AAS (computed tomographic scanning 88%, MRI 7%, transesophageal echocardiography 3% and angiography 2%). Table 1 summarises the baseline characteristics for all AAS patients. The four groups were similar with respect to baseline characteristics with the exception of gender, and the distribution of ascending and descending thoracic aorta involvement.
Table 1.
Baseline patient characteristics
| Acute aortic syndromes | Aortic dissection | Penetrating aortic ulcer | Intramural haematoma | Symptomatic aortic aneurysm | ||
|---|---|---|---|---|---|---|
| Variable | n=115 | n=61 | n=5 | n=8 | n=41 | p Value |
| Age, median | 72 | 70 | 70 | 78 | 71 | 0.37 |
| Female | 53 (46%) | 29 (48%) | 3 (60%) | 7 (88%) | 14 (34%) | 0.04 |
| Hypertension | 93 (81%) | 49 (80%) | 5 (100%) | 7 (88%) | 32 (78%) | 0.65 |
| Coronary disease | 50 (44%) | 24 (40%) | 2 (40%) | 2 (25%) | 22 (55%) | 0.31 |
| Median ejection fraction (%) | 55 | 55 | 55 | 60 | 55 | 0.03 |
| Diabetes mellitus | 20 (17%) | 11 (18%) | 1 (20%) | 3 (38%) | 5 (12%) | 0.38 |
| Hyperlipidaemia | 42 (37%) | 17 (28%) | 2 (40%) | 5 (63%) | 18 (44%) | 0.15 |
| Ascending thoracic aorta involvement | 34 (30%) | 24 (39%) | 2 (40%) | 1 (13%) | 7 (17%) | 0.07 |
| Descending thoracic aorta involvement | 76 (66%) | 44 (72%) | 3 (60%) | 7 (88%) | 22 (54%) | 0.14 |
| Median creatinine | 1.05 | 1.1 | 1.0 | 0.8 | 1.1 | 0.34 |
| Median white blood cell count | 9.6 | 9.4 | 11.7 | 12.7 | 8.9 | 0.31 |
| Median troponin | 0.01 | 0.01 | 0.01 | 0.01 | 0.01 | 0.80 |
Treatment modalities included surgical, endovascular or medical, as depicted in table 2. The in-hospital complications among the various AAS are shown in table 3. An hsCRP value >20 mg/l was significantly associated with in-hospital complications (table 4).
Table 2.
Management strategy of acute aortic syndrome patients
| Aortic dissection | Penetrating aortic ulcer | Intramural haematoma | Symptomatic aortic aneurysm | |
|---|---|---|---|---|
| Type of management | n=61 | n=5 | n=8 | n=41 |
| Surgical | 29 (48%) | 3 (60%) | 2 (25%) | 21 (51%) |
| Aortic surgery with CABG and AVR | 6 (10%) | 0 (0%) | 0 (0%) | 1 (2.4%) |
| Aortic surgery with CABG | 4 (6.6%) | 0 (0%) | 0 (0%) | 5 (12%) |
| Aortic surgery with AVR | 8 (13%) | 0 (0%) | 0 (0%) | 1 (2.4%) |
| Aortic surgery, isolated | 7 (11%) | 0 (0%) | 1 (13%) | 10 (25%) |
| Endovascular stent | 4 (6.6%) | 3 (60%) | 1 (13%) | 4 (10%) |
| Endovascular stent (no surgery) | 1 (0.5%) | 0 (0%) | 0 (0%) | 2 (4.9%) |
| Medical therapy | 32 (52%) | 2 (40%) | 6 (75%) | 20 (49%) |
AVR, aortic valve replacement; CABG, coronary artery bypass grafts.
Table 3.
In-hospital complications of acute aortic syndrome patients
| Aortic dissection | Penetrating aortic ulcer | Intramural haematoma | Symptomatic aortic aneurysm | Total | ||
|---|---|---|---|---|---|---|
| Complication | n=61 | n=5 | n=8 | n=41 | n=115 | p Value |
| Haemodynamic shock | 5 (8.2%) | 1 (20%) | 1 (13%) | 4 (9.8%) | 11 (9.6%) | 0.84 |
| Renal failure | 9 (14%) | 0 (0%) | 1 (13%) | 3 (7%) | 13 (11%) | 0.52 |
| Stroke | 2 (3.3%) | 0 (0%) | 1 (13%) | 1 (2.4%) | 4 (3.5%) | 0.52 |
| Myocardial infarction | 5 (8.2%) | 0 (0%) | 0 (0%) | 6 (15%) | 11 (9.6%) | 0.44 |
| Limb ischaemia | 2 (3.3%) | 0 (0%) | 0 (0%) | 1 (2.4%) | 3 (2.6%) | 0.93 |
| In-hospital mortality | 4 (6.6%) | 0 (0%) | 0 (0%) | 1 (2.4%) | 5 (4.3%) | 0.64 |
Table 4.
In-hospital complications of acute aortic syndrome stratified by high-sensitivity C-reactive protein (hsCRP)
| hsCRP ≤20 mg/l | hsCRP >20 mg/l | ||
|---|---|---|---|
| Complication | n=55 | n=60 | p Value |
| Haemodynamic shock | 4 (7.3%) | 7 (11.7%) | 0.42 |
| Stroke | 1 (1.8%) | 3 (5.0%) | 0.35 |
| Myocardial infarction | 4 (7.3%) | 7 (11.7%) | 0.42 |
| Limb ischaemia | 1 (1.8%) | 2 (3.3%) | 0.62 |
| Any complication* | 10 (18%) | 19 (32%) | 0.048 |
| In-hospital mortality | 2 (3.6%) | 3 (5.0%) | 0.72 |
*Any complication includes a combination of haemodynamic shock, stroke, myocardial infarction and limb ischaemia.
HsCRP level in AAS
The median hsCRP for patients with AD (49 mg/l) was higher than in those with PAU (28 mg/l), SAA (14 mg/l) and IMH (10 mg/l) (figure 1). A non-parametric Kruskal–Wallis test showed differences among the four groups (p=0.02). In multivariable linear regression, IMH (p=0.03) and SAA (p=0.04) had lower hsCRP levels compared with AD cases, even after adjusting for age and gender. There was no significant difference between the PAU and AD groups (p=0.8). Among patients with AD, hsCRP levels were similar for those with involvement of the ascending aorta versus the descending aorta (59±49 mg/l vs 59±59 mg/l, respectively; p=0.87).
Figure 1.
Median high-sensitivity C-reactive protein (hsCRP) (15th, 85th percentile) values according to acute aortic syndrome (AAS). AD, aortic dissection; IMH, intramural haematoma; PAU, penetrating aortic ulcer; SAA, symptomatic aortic aneurysm.
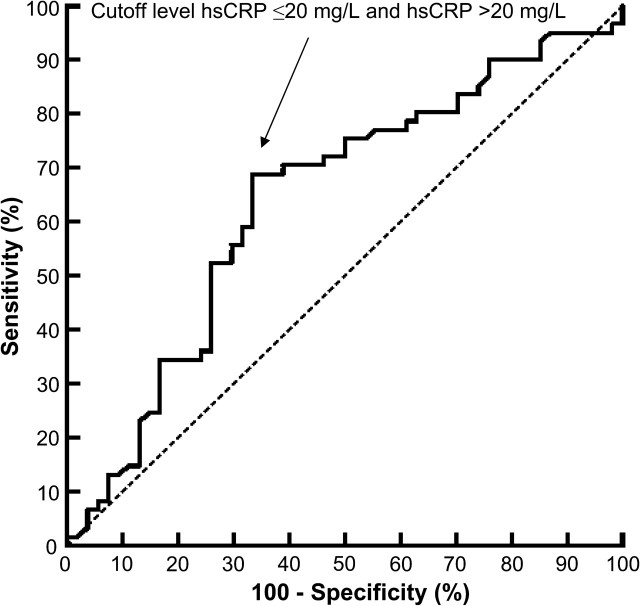
HsCRP levels greater than 20 mg/l seemed to have the best diagnostic accuracy at separating the AD group from the other AAS groups, yielding predictability with an area under the receiver-operating characteristics curve of 0.68 (figure 2). The position of this cut-off level (hsCRP≤20 and hsCRP>20 mg/l) yielded a sensitivity of 0.69 and a specificity of 0.67, with a positive predictive value of 0.70 and negative predictive value of 0.65.
Figure 2.
Receiver-operating characteristic curve showing the accuracy of high-sensitivity C-reactive protein (hsCRP) in the diagnosis of aortic dissection versus the other acute aortic syndromes. The area under the curve for hsCRP was 0.68. A cut-off level of hsCRP >20 mg/l yielded a sensitivity of 69% and specificity of 67%.
Duration of hospital stay, in-hospital and long-term survival
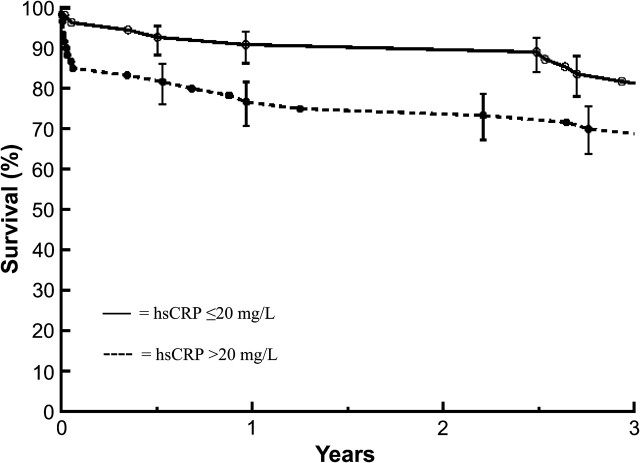
The median number of in-hospital days for this population was 10 days. Patient hsCRP levels were not associated with in-hospital length of stay. Creatinine levels upon presentation (p<0.007) and involvement of the ascending thoracic aorta (p=0.01) were the only factors related to increased hospital stay. There were five in-hospital deaths. HsCRP was not associated with in-hospital mortality. Only increased age was associated with in-hospital death (p=0.05) in AAS patients. Adjusting the model for age showed no association between hsCRP level and in-hospital mortality (OR 1.34, 95% CI 0.65 to 2.73, p=0.43, for one unit increase in log(hsCRP)). Overall unadjusted survival at 1 month, 6 months, 1 year, 2 years and 3 years was 90%, 88%, 83%, 82%, and 75%, respectively. There was a significant difference in unadjusted survival among the groups (logrank p=0.03); the 1-year survival was 85% in the AD group and 80% in the SAA group.
In a multivariate Cox regression model, adjusted for age (p<0.0001), gender (p=0.1), type of AAS (p=0.02) and white blood cell count (p<0.004), elevated hsCRP was associated with a higher long-term mortality (OR 1.57, 95% CI 1.13 to 2.18, p=0.007, for one unit increase in log (hsCRP)) (figure 3). In this non-linear transformation, there was a higher HR for death at higher levels of hsCRP.
Figure 3.
Long-term survival of acute aortic syndromes stratified by C-reactive protein (hsCRP) levels.
Discussion
AAS are relatively uncommon conditions but often lead to catastrophic outcomes. Early and accurate diagnosis and treatment are essential to preserve life in these patients. Additional diagnostic tools that are rapid and widely available can heighten the index of suspicion and could play a significant role in detecting these conditions in an early stage at presentation. Moreover, tests that can add prognostic information are of major utility in stratifying the risk of long-term adverse outcome in this often high-risk group of patients.
Our study demonstrated that hsCRP levels differed among AAS patients, with significantly higher median hsCRP levels in AD patients compared with those with PAU, SAA and IMH. We found hsCRP levels to be potentially useful as a diagnostic marker for AD versus other AAS with a cut-off level of 20 mg/l yielding an area under the curve of 0.68, with a positive predictive value of 0.70. Thus, hsCRP levels may provide incremental value in the evaluation of acute aortic diseases and act as a corroborative test for ruling in AD. As a prognostic tool, elevated hsCRP at presentation was independently associated with worse long-term survival. Accordingly, hsCRP may serve as a biomarker to help stratify patients who are high-risk versus low-risk in the post-AAS setting. Once identified, high-risk AAS patients may warrant more aggressive therapies and closer clinical and imaging surveillance, though further prospective study is needed to validate such an approach.
Previous studies have reported positive associations between baseline CRP levels and increased mortality in patients undergoing elective abdominal aortic aneurysm repair.10 Significant progressive elevation of CRP levels was noted in patients with asymptomatic, symptomatic and ruptured aortic aneurysm.1 Prior reports showed that elevated admission CRP values among patients with symptomatic aortic aneurysm or dissection were independently associated with greater short-term mortality.6 In the present study, hsCRP failed to discriminate in-hospital survival but independently predicted long-term mortality in a wide spectrum of AAS patients. The long-term predictive value of hsCRP in this study may highlight patients who have a magnified inflammatory response and in turn may be at greater risk of later aortic-vascular events.11
Although the majority of circulating CRP in AAS patients is derived from the liver, it is believed that other sources such as vascular cells and adipose tissue can contribute.12 In some patients, CRP is produced by aneurysmal tissue,3 coronary13 and carotid atheromatous plaque.14 In animal models during abdominal aortic aneurysm formation, increased hsCRP levels stem from aneurysmal arteries with degenerating elastic lamina, a process mediated by mechanical stretch.15 In our AAS cohort, hsCRP was high, but not different, in patients with PAU and AD, which may indicate that, at least in this population, the atherosclerotic burden, local tissue release from the aortic wall and/or systemic response was greatest in these two conditions. Patients with SAA and IMH had significantly lower hsCRP levels than patients with AD and PAU. Whether this reflects a lesser role of arterial wall inflammation or a lower atherosclerotic burden in these patients is not known. Regardless, these results underscore the importance of inflammation in AAS.
Study limitations
The study's major limitation rests in the relatively small sample size. Overall the cohort size of AAS is substantial, but the individual aortic disease states are small, making the analysis to discriminate between AAS types less accurate. Prudence should be used when interpreting hs-CRP levels in these acute chest pain syndromes. Our patient sample consisted of already-diagnosed AAS, an inherent bias, and thus extending our study results on hsCRP usage to a variety of chest pain patients with non-aortic diseases is not recommended. While it would be of interest to know the cause of mortality in the patients with hsCRP elevation, we did not have any specific causes of death. Finally, measurement of hsCRP was obtained within 24 h of hospital admission, although the time from symptom onset to presentation is unknown. It is not clear if hsCRP levels would provide similar utility and prognostic value if collected within the first 24 h of symptom onset.
Acknowledgments
The authors acknowledge R Zuzek, F Al Solaiman and A Abdel Latif for their assistance in expert data extraction.
Footnotes
Funding: DLB receives research support from Astra Zeneca, Bristol-Myers Squibb, Eisai, Ethicon, Heartscape, Sanofi Aventis and The Medicines Company.
Competing interests: None.
Ethics approval: Ethics approval was provided by the Cleveland Clinic Ethics Review Board, Cleveland, Ohio.
Provenance and peer review: Not commissioned; not externally peer reviewed.
References
- 1.Domanovits H, Schillinger M, Müllner M, et al. Acute phase reactants in patients with abdominal aortic aneurysm. Atherosclerosis 2002;163:297–302. [DOI] [PubMed] [Google Scholar]
- 2.Rehm JP, Grange JJ, Baxter BT. The formation of aneurysms. Semin Vasc Surg 1998;11:193–202. [PubMed] [Google Scholar]
- 3.Vainas T, Lubbers T, Stassen FR, et al. Serum C-reactive protein level is associated with abdominal aortic aneurysm size and may be produced by aneurysmal tissue. Circulation 2003;107:1103–5. [DOI] [PubMed] [Google Scholar]
- 4.Juvonen J, Surcel HM, Satta J, et al. Elevated circulating levels of inflammatory cytokines in patients with abdominal aortic aneurysm. Arterioscler Thromb Vasc Biol 1997;17:2843–7. [DOI] [PubMed] [Google Scholar]
- 5.Agmon Y, Khandheria BK, Meissner I, et al. C-reactive protein and atherosclerosis of the thoracic aorta: a population-based transesophageal echocardiographic study. Arch Intern Med 2004;164:1781–7. [DOI] [PubMed] [Google Scholar]
- 6.Schillinger M, Domanovits H, Bayegan K, et al. C-reactive protein and mortality in patients with acute aortic disease. Intensive Care Med 2002;28:740–5. [DOI] [PubMed] [Google Scholar]
- 7.Sugano Y, Anzai T, Yoshikawa T, et al. Serum C-reactive protein elevation predicts poor clinical outcome in patients with distal type acute aortic dissection: association with the occurrence of oxygenation impairment. Int J Cardiol 2005;102:39–45. [DOI] [PubMed] [Google Scholar]
- 8.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457–81. [Google Scholar]
- 9. Cox DR, Oaks D. Analysis of Survival Data. London: Chapman & Hall, 1984. [Google Scholar]
- 10.Satta J, Immonen K, Reinilä A, et al. Outcome of elective infrarenal abdominal aortic aneurysm repair–an analysis of 174 consecutive patients. Ann Chir Gynaecol 1996;85:231–5. [PubMed] [Google Scholar]
- 11.Di Napoli M, Papa F, Bocola V. C-reactive protein in ischemic stroke: an independent prognostic factor. Stroke 2001;32:917–24. [DOI] [PubMed] [Google Scholar]
- 12.Calabro P, Chang DW, Willerson JT, et al. Release of C-reactive protein in response to inflammatory cytokines by human adipocytes: linking obesity to vascular inflammation. J Am Coll Cardiol 2005;46:1112–13. [DOI] [PubMed] [Google Scholar]
- 13.Kobayashi S, Inoue N, Ohashi Y, et al. Interaction of oxidative stress and inflammatory response in coronary plaque instability: important role of C-reactive protein. Arterioscler Thromb Vasc Biol 2003;23:1398–404. [DOI] [PubMed] [Google Scholar]
- 14.Sattler KJ, Woodrum JE, Galili O, et al. Concurrent treatment with renin–angiotensin system blockers and acetylsalicylic acid reduces nuclear factor kappaB activation and C-reactive protein expression in human carotid artery plaques. Stroke 2005;36:14–20. [DOI] [PubMed] [Google Scholar]
- 15.Huang G, Wang A, Li X, et al. Change in high-sensitive C-reactive protein during abdominal aortic aneurysm formation. J Hypertens 2009;27:1829–37. [DOI] [PubMed] [Google Scholar]