Abstract
Objective
To characterise the risk-factor profile and treatment gaps among patients with, or at risk for, cardiovascular disease in the Middle East.
Design
Secondary analysis of a prospective observational study.
Setting
International multicentre study (Reduction of Atherothrombosis for Continued Health).
Patients
Stable outpatients with established cardiovascular disease or at least three risk factors for atherothrombosis. The present analysis was based on 840 patients from the Middle East.
Intervention
Observational study without a study-specific intervention.
Main outcome measures
A treatment gap was defined as at least one of the following: current cigarette smoking, total cholesterol ≥200 mg/dl, serum glucose ≥126 mg/dl or blood pressure of ≥140/90.
Results
The majority of Middle Eastern patients had hypertension (80.2%), more than half had a history of diabetes mellitus (52.3%), and a third had hypercholesterolaemia (34.1%). There was a high prevalence of obesity (38.6%), and nearly half the patients were former or current smokers (46%). β-Blockers and angiotensin-converting enzyme inhibitors were the most commonly prescribed antihypertensives (61.1% and 57.5%, respectively). Antiplatelet therapy (most commonly aspirin) and lipid-lowering drugs (most commonly a statin) were used in most patients (90.7% and 85.2%, respectively). Three-quarters of the participants (75.6%) had at least one uncontrolled risk factor.
Conclusion
Patients with atherothrombosis in the Middle East have a high prevalence of risk factors including alarming rates of diabetes mellitus and obesity. At least one risk factor is uncontrolled in the majority of patients, presenting a pressing need for improving the care of such patients in the Middle East.
Keywords: Cardiovascular disease, diabetes mellitus, obesity, risk factors, Middle East, diabetes
Introduction
Cardiovascular disease is the leading cause of morbidity and mortality worldwide.1 2 Over the past half century, our understanding of the epidemiology of and risk factors for cardiovascular disease has led to the development of effective measures to combat the cardiovascular epidemic, and resulted in significant improvements in patient outcomes. A substantial proportion of that improvement in cardiovascular disease outcomes was driven by implementation of primary and secondary preventive measures in stable outpatients.
To date, the vast majority of the literature on patients with, or at high risk for, cardiovascular disease comes from predominantly Western populations in affluent/industrialised countries. Non-Western and mostly developing regions of the world contribute an increasingly greater share to the global burden of cardiovascular disease, yet are greatly under-represented in the literature.3 4 In the Middle East, there is growing recognition that cardiovascular disease and its associated risk factors represent a significant public-health challenge, with some Middle Eastern countries reporting some of the highest rates of diabetes and obesity worldwide.5–9 Nonetheless, relatively few data are available on risk factors and management in patients with established cardiovascular disease in the Middle East.
The Reduction of Atherothrombosis for Continued Health (REACH) registry provides a unique opportunity to characterise the risk-factor profile, treatment gaps and outcomes in patients with cardiovascular disease or cardiovascular disease risk factors in the Middle East. In the present analysis, we characterise the risk-factor profile, management patterns and treatment gaps among stable outpatients from the Middle East with cardiovascular disease or cardiovascular disease risk factors enrolled in the REACH registry.
Methods
The REACH registry is an international, prospective, observational study of stable outpatients with or at high risk for cardiovascular disease.10 11 A detailed design and methodology have been previously published.10 12 Briefly, consecutive eligible outpatients aged 45 or older with established coronary artery disease, cerebrovascular disease or peripheral arterial disease, or with at least three atherosclerotic risk factors were enrolled in 2004. Ethics committee approval was obtained at each participating institution, and each patient gave written informed consent to participate in the registry.
The diagnosis of coronary artery disease required at least one of the following: history of stable or unstable angina with documented coronary artery disease, prior percutaneous coronary intervention or coronary artery bypass graft surgery, or previous myocardial infarction. Documented cerebrovascular disease required a hospital or neurologist report with the diagnosis of ischaemic stroke or transient ischaemic attack. Diagnosis of peripheral arterial disease required the presence of current intermittent claudication with an ankle brachial index of <0.9 or a history of intermittent claudication with a related peripheral vascular intervention (eg, angioplasty, surgical bypass graft or amputation).
In the absence of established cardiovascular disease, eligible patients had to have at least three risk factors for cardiovascular disease either documented in the medical record or for which they were receiving treatment. The qualifying risk factors were: treated diabetes mellitus, diabetic nephropathy (microalbuminuria ≥30 μg/ml), asymptomatic ankle brachial index of <0.9 or asymptomatic carotid stenosis of 70% or higher, at least one carotid plaque as evidenced by intima-media thickness exceeding twice that of neighbouring sites, systolic blood pressure of ≥150 mm Hg despite therapy for at least 3 months, hypercholesterolaemia currently treated with medication, current smoking (>15 cigarettes per day), or age ≥65 years for a male, and ≥70 years for a female.
Data were entered on standardised international case report forms completed at the study sites and then collected centrally. Baseline measurements included height, weight, waist circumference, seated systolic and diastolic blood pressure, and fasting glucose and total cholesterol levels. Body mass index (BMI) was defined as weight in kilograms divided by the square of height in metres. Obesity was defined as a BMI of 30 or higher or a waist circumference of 40 inches (102 cm) or larger in men or 35 inches (88 cm) or larger in women. Participants were considered overweight if they had a BMI of 25 to <30. Smoking was defined as at least five cigarettes per day on average, and was considered current if continued within the last month before study entry or former if discontinued more than 1 month before study entry. A treatment gap was defined as the presence of at least one of the following: current cigarette smoking, total cholesterol ≥200 mg/dl, serum glucose ≥126 mg/dl or a blood pressure of ≥140/90.
Statistical methods
Data are summarised as medians with 25th and 75th percentiles for continuous variables, and proportions for categorical variables. Continuous variables were compared using the Wilcoxon rank sum test or the Kruskal–Wallis test. Categorical variables were compared with the χ2 test. The association between the presence of a treatment gap and 1 year outcomes was examined using logistic regression adjusting for age and gender, and quantified with the OR with 95% confidence limits. A p value of <0.05 was considered statistically significant. Analyses were performed with the SAS 9.1 statistical package (SAS Institute).
Results
The REACH registry enrolled more than 68 000 patients from 44 countries. The present analysis is based on 840 patients enrolled from four Middle Eastern countries: Israel (374 patients), Lebanon (120 patients), Saudi Arabia (196 patients) and United Arab Emirates (150 patients). The baseline characteristics are listed in table 1. The median age was 67.6 years (58.0–74.1), and nearly three-quarters of the participants were male (71.6%). There was a regional variation in the age of participants, ranging from 60.2 (52.8–68.2) in Saudi Arabia to 71.5 (65.0–76.4) in Israel (p<0.0001). The majority of patients had hypertension (80.2%), more than one-half had a history of diabetes mellitus (52.3%), and one-third had hypercholesterolaemia (34.1%). There was a high prevalence of obesity (38.6%), and nearly half the patients were either former or current smokers (46%). Most of the participants had established cardiovascular disease (85%), most commonly coronary artery disease (54.7%) (figure 1). Only a small proportion of the patients with established cardiovascular disease had documented disease in more than one vascular bed (15.1% in two locations and 1.7% in three locations). The majority of patients were cared for by a general practitioner/internist (50%) or a cardiologist (40%).
Table 1.
Baseline demographics of Middle Eastern patients in the Reduction of Atherothrombosis for Continued Health registry
| All (n=840) | Established (n=713) | Risk factor only (n=127) | |
| Age | 67.6 (58.0–74.1) | 67.1 (57.8–74.1) | 69.0 (58.6–75.4) |
| Male | 71.6 | 73.5 | 61.1 |
| Diabetes mellitus | 52.3 | 48.7 | 72.4 |
| Hypertension | 80.2 | 78.1 | 92.1 |
| Hypercholesterolaemia | 34.1 | 29.6 | 58.0 |
| Obesity | 38.6 | 37.2 | 46.5 |
| Body mass index | |||
| (<25 kg/m2) | 24.0 | 24.3 | 22.6 |
| (25 to <30 kg/m2) | 46.1 | 46.7 | 42.7 |
| (30 to <35 kg/m2) | 21.6 | 20.4 | 28.3 |
| (≥35 kg/m2) | 8.3 | 8.6 | 6.5 |
| Smoker | |||
| Current | 14.8 | 13.9 | 20.0 |
| Former | 31.2 | 32.8 | 22.4 |
Figure 1.
Middle Eastern population in Reduction of Atherothrombosis for Continued Health by disease category. CAD, coronary artery disease; CVD, cerebrovascular disease; PAD, peripheral artery disease.
Table 2 lists the treatment patterns for all patients and by group type (established disease and risk factors only). Almost all patients with diagnosed hypertension were on at least one antihypertensive medication. β-Blockers and angiotensin-converting enzyme inhibitors were the most commonly prescribed antihypertensives, followed by diuretics and calcium-channel blockers. Among patients with diabetes mellitus, the vast majority were on at least one antidiabetic medication, most commonly a biguanide or a sulfonylurea. Nearly a quarter of the patients with diabetes were on insulin, and a small proportion of patients were on a thiazolidinedione. Antiplatelet therapy (most commonly aspirin) and lipid-lowering drugs (most commonly a statin) were used in most patients (90.7% and 85.2%, respectively).
Table 2.
Prescribed medications among Middle Eastern patients in the Reduction of Atherothrombosis for Continued Health registry
| All (n=840) | Established (n=713) | Risk factor only (n=127) | |
| No of patients with diagnosed hypertension of elevated blood pressure at initial examination | 687 | 569 | 118 |
| At least one antihypertensive | 98.8 | 98.6 | 100 |
| β-Blockers | 61.1 | 65.2 | 41.5 |
| Angiotensin-converting enzyme inhibitors | 57.5 | 56.8 | 61.0 |
| Diuretics | 46.2 | 45.8 | 47.9 |
| Calcium-channel blockers | 42.5 | 41.8 | 45.8 |
| Angiotensin II receptor blockers | 21.2 | 21.3 | 20.7 |
| Other antihypertensives | 14.5 | 14.7 | 13.7 |
| No of patients with history of diabetes or elevated blood glucose at initial examination | 463 | 369 | 94 |
| At least one antidiabetic medication | 88.1 | 86.5 | 94.7 |
| Sulfonylureas | 49.5 | 49.2 | 50.6 |
| Biguanides | 55.0 | 52.6 | 64.8 |
| Insulin | 23.6 | 24.9 | 18.5 |
| Thiazolidinediones | 5.7 | 6.3 | 3.3 |
| Other diabetes medications | 7.3 | 6.0 | 12.4 |
| Antiplatelet therapy | |||
| At least one antiplatelet agent | 90.7 | 95.1 | 66.1 |
| Acetylsalicylic acid | 83.6 | 86.8 | 65.4 |
| Other antiplatelet agent | 25.1 | 29.1 | 2.4 |
| Any two antiplatelet agents | 17.8 | 20.8 | 1.6 |
| Lipid-lowering therapy | |||
| At least one agent | 85.2 | 85.8 | 81.9 |
| Statin | 82.5 | 74.8 | 83.9 |
| Other lipid-lowering agent | 7.5 | 7.3 | 8.7 |
| Nitrates | 31.5 | 36.8 | 1.6 |
| Non-steroidal anti-inflammatory drugs | 8.2 | 8.6 | 5.6 |
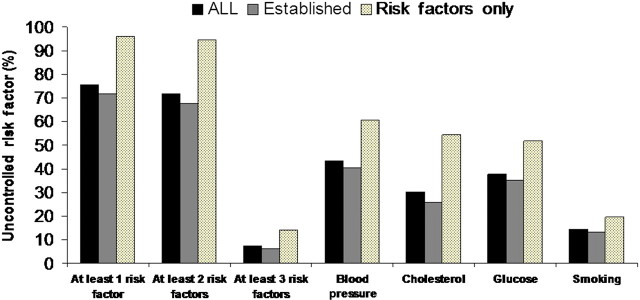
Figure 2 displays the prevalence of uncontrolled risk factors among all patients and by group type. Many patients had a total cholesterol of ≥200 mg/dl (30.2%), a blood pressure of ≥140/90 mm Hg (43.5%) or a serum glucose of ≥126 mg/dl (37.6%). Overall, three-quarters of the participants (75.6%) had at least one uncontrolled risk factor. Patients without symptomatic disease (risk factors only group) were more likely to have an uncontrolled risk factor than patients with symptomatic disease (figure 2). Nearly all patients without symptomatic disease (96.1%) had at least one uncontrolled risk factor.
Figure 2.
Treatment gaps among Middle Eastern patients in Reduction of Atherothrombosis for Continued Health. A treatment gap was defined as the presence of at least one of the following: current cigarette smoking, total cholesterol of ≥200 mg/dl, serum glucose of ≥126 mg/dl or blood pressure of ≥140/90.
Table 3 lists the 1-year event rates for all patients and by group type (established disease and risk factors only). No fatal events occurred in the group with risk factors only, but the 1-year mortality in the group with established cardiovascular disease was nearly 3%.
Table 3.
One-year event rates among Middle Eastern patients in Reduction of Atherothrombosis for Continued Health
| All (n=840) | Established (n=713) | Risk factor only (n=127) | |
| Combined endpoint of cardiovascular death (including fatal MI/stroke and other cardiovascular death), non-fatal MI/stroke, vascular interventions and hospitalisations for atherothrombotic events | 19.88 | 22.02 | 7.87 |
| All-cause mortality | 2.51 | 2.95 | 0 |
| Cardiovascular death | 2.14 | 2.52 | 0 |
| Cardiovascular death/MI/stroke | 6.91 | 7.85 | 1.58 |
| Fatal MI | 0.48 | 0.56 | 0 |
| Non-fatal MI | 2.98 | 3.37 | 0.79 |
| Fatal stroke | 0.60 | 0.70 | 0 |
| Non-fatal stroke | 1.79 | 1.96 | 0.79 |
| Percutaneous coronary intervention | 4.46 | 5.19 | 1.57 |
| Coronary artery bypass graft | 2.26 | 2.52 | 0.79 |
| Congestive heart failure | 5.0 | 5.61 | 1.57 |
| Unstable angina | 8.21 | 9.26 | 2.36 |
MI, myocardial infarction.
Discussion
We present a unique description of the risk-factor profile, treatment patterns and gaps and 1-year outcomes in Middle Eastern outpatients with established cardiovascular disease or multiple cardiovascular risk factors. The most striking features of this population are the high prevalence of diabetes (nearly half of the patients with established cardiovascular disease) and obesity (nearly three-quarters were either obese or overweight). While most patients were prescribed medications to control risk factors and prevent cardiovascular events, treatment gaps were prevalent, with three-quarters of these high-risk patients having at least one treatment gap.
The high prevalence of diabetes mellitus and obesity in the present analysis is consistent with previous observations from the Middle East.13 14 In the Gulf Registry of Acute Coronary Events (Gulf RACE), a multinational registry of more than 8000 patients admitted with acute coronary syndromes in six Middle Eastern countries, 40% of the patients had a history of diabetes, and 67% were overweight or obese.15 Patients with diabetes in Gulf RACE tended to have worse in-hospital outcomes. Another distinctive feature of patients with cardiovascular disease in the Middle East is the relatively younger age compared with their Western counterparts. In Gulf RACE, patients with ACS were a decade or two younger than what had been observed in international or American registries. The mean age among participants from Saudi Arabia in REACH was nearly a decade younger than the mean age in the entire REACH cohort. The younger age among patients with both acute and non-acute cardiovascular disease in some Middle Eastern countries may reflect the relatively younger populations of these countries but may also reflect premature disease mediated by the high prevalence of diabetes, obesity and genetic predisposition.16
The significant gaps in attaining treatment goals represent a substantial opportunity to improve the care of patients with, or at high risk for, cardiovascular disease in the Middle East. These gaps were observed despite the fact that 40% of the participants were cared for by cardiologists. The suboptimal achievement of prevention goals in ambulatory practice has been described in other regions of the world, and in patients with and without established cardiovascular disease. While physicians may prescribe the appropriate therapies, treatment goals may not be achieved because of a lack of familiarity with such goals, inappropriate follow-up and patient non-compliance with, or intolerance of, medications. A major factor in using preventive measures is the physician's perception of the patient's risk. While current prevention guidelines advocate the concept of cardiovascular ‘risk equivalence,’ this notion may not have been adequately disseminated among physicians. For example, nearly three-quarters of the ‘risk-factors only’ group had diabetes mellitus, a coronary artery disease risk equivalent, yet almost all patients (96.1%) had at least one uncontrolled risk factor. The present study highlights the prevalence of uncontrolled risk factors, and future work should focus on identifying the barriers to risk-factor control and how to overcome them. Particularly alarming is the high prevalence of diabetes and obesity in the Middle East emphasising the need for greater education and awareness campaigns for healthcare providers and the public.
Several limitations to the present analysis are worth noting. The findings represent the practice and patient characteristics of the four Middle Eastern countries in REACH, and may not reflect trends in other parts of the Middle East. The estimates on 1-year outcomes and treatment gaps from REACH may not accurately reflect national trends within the respective countries, since they represent practice patterns in select centres that participate in multinational registries, and in which a large proportion of the patients are cared for by cardiologists. Therefore, it is likely that the figures obtained here regarding poorly controlled risk factors are underestimates.
In conclusion, patients with a documented, or high risk for, cardiovascular disease in the Middle East have a high prevalence of risk factors including alarming rates of diabetes mellitus and obesity. At least one risk factor is uncontrolled in the majority of patients. This represents a pressing opportunity for improving the care of such patients in the Middle East.
Acknowledgments
The REACH Registry is endorsed by the World Heart Federation. A complete list of REACH investigators is accessible online at http://www.reachregistry.org.
Footnotes
Funding: The Reduction of Atherothrombosis for Continued Health Registry is sponsored in the Middle East countries by Sanofi-Aventis.
Competing interests: DLB discloses the following relationships: institutional research grants from Astra Zeneca, Bristol-Myers Squibb, Eisai, Ethicon, Heartscape, Sanofi Aventis and The Medicines Company. HM is employed by Sanofi-Aventis.
Patient consent: Obtained.
Ethics approval: Ethics approvals were obtained from the institutional review board in each country according to local requirements and signed informed consent was obtained for all patients.
Contributors: The first draft was written by AAA-A. AAA-A had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Analysis and interpretation of data: AAA-A, WAA-M. Drafting of the manuscript: AAA-A. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: AAA-A.
Provenance and peer review: Not commissioned; not externally peer reviewed.
References
- 1.Lopez AD, Murray CC. The global burden of disease, 1990–2020. Nat Med 1998;4:1241–3. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization fact sheet. http://www.who.int/mediacentre/factsheets/fs317/en/print.html (accessed 14 Sep 2010).
- 3.Reddy KS, Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation 1998;97:596–601. [DOI] [PubMed] [Google Scholar]
- 4.Reddy KS. Cardiovascular disease in non-Western countries. N Engl J Med 2004;350:2438–40. [DOI] [PubMed] [Google Scholar]
- 5.Saadi H, Carruthers SG, Nagelkerke N, et al. Prevalence of diabetes mellitus and its complications in a population-based sample in Al Ain, United Arab Emirates. Diabetes Res Clin Pract 2007;78:369–77. [DOI] [PubMed] [Google Scholar]
- 6.Malik M, Razig SA, Malik M, et al. The prevalence of the metabolic syndrome among the multiethnic population of the United Arab Emirates: a report of a national survey. Metab Syndr Relat Disord 2008;6:177–86. [DOI] [PubMed] [Google Scholar]
- 7.Hirbli KI, Jambeine MA, Slim HB, et al. Prevalence of diabetes in greater Beirut. Diabetes Care 2005;28:1262. [DOI] [PubMed] [Google Scholar]
- 8.Harzallah F, Alberti H, Ben Khalifa F, et al. The metabolic syndrome in an Arab population: a first look at the new International Diabetes Federation criteria. Diabet Med 2006;23:441–4. [DOI] [PubMed] [Google Scholar]
- 9.Al-Mahroos F, McKeigue PM. High prevalence of diabetes in Bahrainis. Associations with ethnicity and raised plasma cholesterol. Diabetes Care 1998;21:936–42. [DOI] [PubMed] [Google Scholar]
- 10.Bhatt DL, Steg PG, Ohman EM, et al. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA 2006;295:180–9. [DOI] [PubMed] [Google Scholar]
- 11.Steg PG, Bhatt DL, Wilson PW, et al. One-year cardiovascular event rates in outpatients with atherothrombosis. JAMA 2007;297:1191–206. [DOI] [PubMed] [Google Scholar]
- 12.Ohman EM, Bhatt DL, Steg PG, et al. The REduction of Atherothrombosis for Continued Health (REACH) Registry: an international, prospective, observational investigation in subjects at risk for atherothrombotic events—study design. Am Heart J 2006;151:786.e1–10. [DOI] [PubMed] [Google Scholar]
- 13.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care 1998;21:1414–31. [DOI] [PubMed] [Google Scholar]
- 14.Balkau B, Deanfield JE, Despres JP, et al. International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation 2007;116:1942–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zubaid M, Rashed WA, Almahmeed W, et al. Management and outcomes of Middle Eastern patients admitted with acute coronary syndromes in the Gulf Registry of Acute Coronary Events (Gulf RACE). Acta Cardiol 2009;64:439–46. [DOI] [PubMed] [Google Scholar]
- 16.El-Menyar A, Amin H, Rashdan I, et al. Ankle-brachial index and extent of atherosclerosis in patients from the Middle East (the AGATHA-ME study): a cross-sectional multicenter study. Angiology 2009;60:329–34. [DOI] [PubMed] [Google Scholar]