Abstract
Background: In the recent years, using health technologies to diagnose and treat diseases has had a considerable and accelerated growth. The proper use of these technologies may considerably help in the diagnosis and treatment of different diseases. On the other hand, unlimited and unrestricted entry of these technologies may result in induced demand by service providers. The aim of this study was to determine the appropriate criteria used in health technologies priority-setting models in the world.
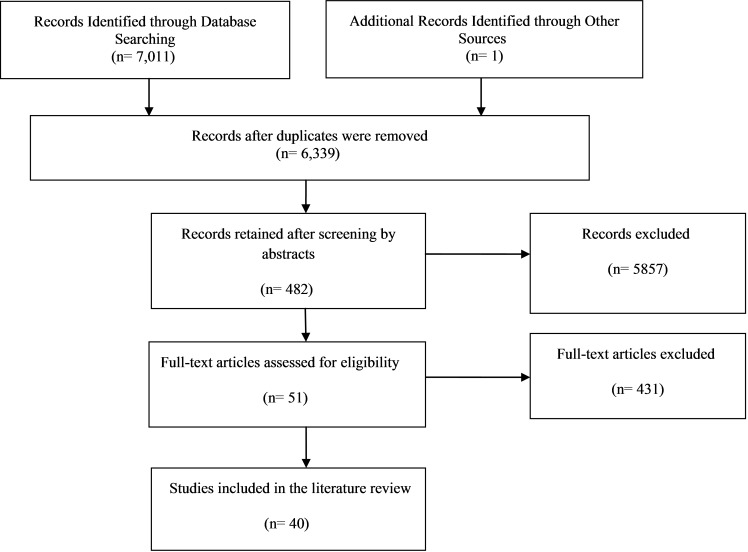
Methods: Using MESH and free text, we sought and retrieved the relevant articles from the most appropriate medical databases (the Cochrane Library, PubMed and Scopus) through three separate search strategies up to March 2015. The inclusion criteria were as follows: 1) Studies with specific criteria; 2) Articles written in English; 3) Those articles conducted in compliance with priority setting of health technologies. Data were analyzed qualitatively using a thematic synthesis technique.
Results: After screening the retrieved papers via PRISMA framework, from the 7,012 papers, 40 studies were included in the final phase. Criteria for selecting health technologies (in pre assessment and in the assessment phase) were categorized into six main themes: 1) Health outcomes; 2) Disease and target population; 3) Technology alternatives; 4) Economic aspects; 5) Evidence; 6) and other factors. "Health effects/benefits" had the maximum frequency in health outcomes (8 studies); "disease severity" had the maximum frequency in disease and target population (12 studies); "the number of alternatives" had the maximum frequency in alternatives (2 studies); "cost-effectiveness" had the maximum frequency in economic aspects (15 studies); "quality of evidence" had the maximum frequency in evidence (4 studies); and "issues concerning the health system" had the maximum frequency in other factors (10 studies).
Conclusion: The results revealed an increase in the number of studies on health technologies priority setting around the world, and emphasized the necessity of application of a multi- criteria approach for appropriate decision making about healthcare technologies in the health systems.
Keywords: Priority Setting, Priority Setting Criteria, Health Technology, Health Systems, Health Technology Assessment
Introduction
Acceptance of health technologies in the health systems within the last decades has experienced some intensive changes. The belief in abiding with the acceptance of health technologies within 1960s and 1970s gradually was replaced by an increasing suspicion of society towards the credibility of advanced health technologies. Nowadays, politicians and the public have an ambiguous opinion about the use of a new health technology (1).
Within the recent years, the use of health technologies for diagnosis and treatment of diseases experienced considerable and accelerated growth. The proper use of these technologies may considerably help in the diagnosis and treatment of diseases. On the other hand, unlimited and unrestricted entry of these technologies may result in induced demand by service providers (2).
Although the number of health technologies, which required assessment, was more than the available resources, all the Health Technology Assessment Organizations prioritized their research projects (3). Various studies have been applied for this purpose worldwide until now such as Canadian Drug and Health Technologies Organization (CADTH), which utilized the analytical hierarchy process (AHP) for priority setting of health technologies (4). Another existing model in relation to priority and selection of health technologies was EVIDEM (Evidence and Value: Impact on Decision Making) model in Canada (5). Nonetheless, there is no consensus on appropriate priority setting between the Health Technology Assessment Organizations (3). The main goal of this study was to identify the most appropriate health technologies priority setting criteria (in pre-assessment and in the assessment phase) and their applications through a systematic review.
Methods
We sought and retrieved the relevant articles based on three separate strategies from the most appropriate medical databases (the Cochrane Library, Pub Med and Scopus) up to March 2015, using MESH and free text (Appendix 1). We retrieved 2,072 articles from Cochrane, 3,733 articles from Pub Med and 1,207 articles from Scopus. In order to find the theses related to the subject, ProQuest database was searched; however, none was found. In addition, in order to find related studies, which might have not been found in the search via the main databases, Google scholar was also searched and one relevant study was found. In order to extract the data for this research, the articles were reviewed by an independent reviewer and double-checked by another one. A self-made data extraction form was used to extract the data from the selected articles. The inclusion criteria were as follows: Papers and academic theses which included specified qualitative and quantitative criteria; 2) Articles written in English; 3) Fall in line with priority setting of health technologies. The majority of the included studies were empirical studies in terms of the application of Multi- Criteria Decision analysis (MCDA) in the health scope, but for these types of studies, authors could not find the proper quality appraisal checklist because quality appraisal was not performed in this research. The findings of the studies were analyzed qualitatively using a thematic synthesis technique. Criteria and sub- criteria were categorized via a classification system from the EVIDEM (5) and Noorani et al. (3) framework and their number of occurrence among the included studies were calculated. In this study, three search strategies were used separately (Appendix 1).
Results
Duplicated and unrelated topics were excluded, leaving 481 relevant topics. The full texts of the articles, which remained from a previous phase, were checked against the inclusion criteria, leaving 51 relevant articles. After a final cross checking against the inclusion criteria, 11 more articles were dropped from the previous list, and 40 articles were included in the final list to be analyzed. The exclusion criteria were as follows: Non-English language articles (13 cases), nonconformity to priority setting framework for health technologies (360 cases), lack of abstract and full text (8 cases), lack of specified qualitative and quantitative criteria (47 cases), articles presented in conferences (14 cases). Overall, 442 studies were excluded from the primary list of the retrieved articles (Fig. 1).
Fig. 1 .
PRISMA Diagram
Criteria for selecting health technologies (in pre-assessment and the assessment phase) were analyzed and synthesized into six main themes as follows: 1) Health outcomes; 2) Disease and target population; 3) Technology alternatives; 4) Economic aspects; 5) Evidence; 6) Other factors (Table 1, Appendix 2).
Table 1 . Definitions of the Main Themes .
| Main Themes | Definition |
| Health outcomes | This criterion was defined by such sub- criteria as health benefits and clinical benefits related to the technology. |
| Disease and target population | This criterion was defined by such sub- criteria as disease burden and disease severity related to the technology. |
| Technology alternatives | This criterion was defined by such sub- criteria as the number and availability of alternatives related to the technology. |
| Economic aspects | This criterion was defined by such sub- criteria as the cost effectiveness and budget impact status related to the technology. |
| Evidence | This criterion was defined by such sub- criteria as the quality and number of medical scientific studies related to the technology. |
| Other factors | This criterion was defined by such sub- criteria as the health system and political, social and moral issues related to the technology. |
A) Health Outcomes
A.1) Health Effects/Benefits
In Ghana, health effects were used for priority setting of health interventions (6-7). To choose new health technologies, health benefit (in population and patient level) was considered (8). To invest on health services, potential health benefit in three states of best health condition (100%), good health condition (75%) and average health condition (50%) was used (9). In Latvia, health benefit was defined as the extent to which health technology application has helped in sustaining good health, assisted in early diagnosis/treatment and reduced the rate of morbidity or mortality (10). For priority setting criteria in state health organizations in the United States, two criteria, including seriousness of the consequences and immediate benefit were applied (11). To obtain new health services, predicted benefit, including an increase of 5-year survival probability of more than 10% (reduction of absolute risk) and improvement of physical and mental performance were used (12). In Europe, “Health Effect Criterion” was defined based on the following: Does the technology have the potential of considerable health benefit for the patients? (13).
A.2) Clinical Impact
The clinical effect was defined for priority setting in terms of two questions: Potential effects of health technology compared to the existing therapies and assessment benefits for reduction of uncertainty (3). In CADTH, “the potential effects of technology on health compared to the existing therapies” was used (4). Clinical factors such as severity status or lifetime shortness were used for decision making in health technologies in Germany (14). Clinical benefit was used for the allocation of resources in the health systems (15). Clinical effect was used for reimbursement decisions about the health interventions (16). In the PATHS health technology assessment priority-setting model, clinical benefit was one of the criteria (17).
A.3) Efficacy/Effectiveness
Efficacy/effectiveness was used for the acceptance of technology in the hospital level (4). In the EVIDEM, efficiency/effectiveness improvement was considered (5). For Iranian basic health insurance package, effectiveness was applied as the priority setting criteria (18). Effectiveness of health intervention was used in Thailand (19).
A.4) Individual Health Benefits
Individual health benefit was used for priority setting (21). Individual health was defined as small: Less than five healthy life years and large: Otherwise (22-23).
A.5) Safety
One of the criteria in EVIDEM was the improvement of safety and tolerability (The minimum score was 0; namely, less than the alternative, and the maximum score was 3; namely, major improvement) (5). Safety was used as a part of therapeutic value as one of the relevant criteria in health technologies decision-making coverage in Germany (14). In addition, safety was used as one of the criteria related to health benefits for the allocation of resources in the health systems (15).
A.6) Quality of Life
Some studies have considered the quality of life and the potential to extend life with quality in priority setting (24).
A.7) Potential Changes in Health Consequences
The Spanish Health Technology Assessment Agency used the potential changes in health consequences for priority setting (25).
A.8) The Effect of Assessment on Reduction of Uncertainty
To assess the relative importance of different resources used by the Health Technology Assessment Plan of UK NHS, “the reduction of uncertainty by performing the assessment” was used as one of the main criteria to identify the potential priorities (26).
A.9) Marginal Benefit
In order to set priority to analyze horizon scanning in Denmark, marginal benefit was defined as created benefits for every patient by the new health technology (27).
A.10) Ability to Reduce Own Health Risk
To organize empirical evidence about coverage decisions, the ability to reduce own health risk was assumed as one of the main criteria of decision-making coverage in health technologies (14).
A.11) Potential to Extend Life
In the view of the Canadian people, the potential to extend life was assumed for priority setting (24).
A.12) Potential to Detect a Condition which, if Treated Early, Averts Costs in The Future
In the view of the Canadian people, the potential of technology to detect a condition, which if treated early, averts costs in the future, was assumed for priority setting (24).
B) Disease and Target Population
B.1) Disease Severity
For priority setting, the severity of disease of intervention target in two severe and non-severe states was used (6). In Ghana, the severity of the disease was defined as the preference of patients with high severity of disease is in accordance with their higher need for health care, and loss of final appropriateness of health such that health improvement of severe conditions obtains more score than the same improvement for patients with lower severity (7). Among the world horizon scanning organizations, the severity of disease was one of the criteria (8). In Thailand, severity of disease was applied considering that its society generally prioritizes the objectives with high severity of disease, due to their more need for health care (19). Severity of disease was adopted using a 4-star scale (more stars imply more severity) (21). In Nepal, severity of disease “in two non-severe states: Surviving in predicted life years of more than two years, if intervention was not available at the time of need and severe states: Otherwise” was defined (22). In Norway, severity of disease (in two non-severe states: Prediction of health more than two years without intervention, and severe state: Prediction of health lower than two years) was used (23). In EVIDEM, severity of disease was defined (5). In Ghana, severity of disease (in two states including non-severe: Surviving in predicted life years of more than five years without intervention and severe: Remaining in predicted health life years between one to five years) was defined (28). In Norway, severity of disease was used based on this question: Does intervention create a specific value in health status severity to achieve its objectives? (29). Severity of disease was used for health priority setting in developing countries (30). To assess EVIDEM framework efficiency, severity of disease was one of the main criteria in 3 states of non-severe, average severity and severe (31).
B.2) Disease Burden
Burden of disease, including prevalence, incidence, and life years adjusted based on disease, predicted health years, economic burden and other indices related to burden of disease, was defined as the priority setting criteria (3). Burden of disease, including prevalence, incidence, and life years adjusted based on disease, predicted health years, economic burden and other indices related to burden of disease, was used in CADTH (4). Burden of disease, including influenced patients, was used in decision-making about health technologies in Germany (14). Burden and importance of illness was used for priority setting (25). Actual burden of disease was used in Netherlands (29). To select health technology assessment, titles and systematic review, burden of disease, including disease prevalence information, risk facing during life and health survival using rate, were assumed (32). In Korean Health Insurance Organization, burden of the condition, including population size and cost burden of services, was used (33). In Mexico, burden of disease was used as a main criterion (34).
B.3) Age of the Target Group
Age of the target group was assumed for health interventions priority setting (youth-elderly or youth-adult-elderly) (6-7,9,14,21,22,23).
B.4) Population Size
Population size was used in EVIDEM (5). Target population size (number of disabled people, number of people with cancer, number of people having mental problems, number of obese people, number of people who were asthmatic and number of people addicted to drugs) was applied for investment prioritization in health (14). Population size influenced by disease was used for decision making in Thailand (19). Prevalence of health status or problem was assumed for setting health priorities (25).
B.5) Number of Potential Beneficiaries
The number of potential beneficiaries in two small and large scales was used as one of the main criteria in health interventions priority setting (21). In Norway, the number of potential beneficiaries (less state: Lower than 100,000 and much state: More than 100,000) was defined as one of the priority setting criteria of the health care (23). To determine health priorities in Ghana, the number of potential beneficiaries was defined in three scales: Less (lower than 100,000, average: 100,000-1,000,000 and much: More than 1,000,000 (28).
B.6) Social Characteristics of Intervention Target Groups
In Norway, the characteristics of the target social groups of intervention, including socioeconomic status, living zone, gender, race, ethnicity, religion and sexual orientation, were used (29). In EVIDEM evaluation framework, the characteristics of target social groups of the intervention were used (31).
B.7) Number of Patients
In the Horizon Scanning Organization, number of patients was used (8). In Netherlands, number of target patients of technology (annual total number) was used (35).
B.8) Effect of Technology on Reduction of Disease Prevalence and Incidence and Reduction of Mortality
In Netherlands, the effect of assessed technology on reduction of disease prevalence and incidence and reduction of mortality was used (36).
B.9) Disease Impacts
Disease impact, including severity of disease, disease-determining characteristics, burden of disease and epidemiology, was assumed for the allocation of resources in the health system (15).
B.10) Effect on the Targeted Group
Two criteria of effect on targeted groups and effect on audiences and local people were used in state health organizations in the United States (16).
B.11) Vulnerable Population Size
Vulnerable population size in four ranges, including lack of specific vulnerable population, children younger than five years of age, and women in fertility ages and elders over 65, was used in Ghana (28).
C) Status of Criteria Related to Alternatives in Included Studies
C.1) Number of Alternatives
Technology alternatives was defined as the number of current and future technologies replaced in order to asses technology for the treatment of a target condition (3-4).
C.2) Availability of Alternatives
Availability of treatment alternatives was used for decision making in Germany (14).
C.3) Limitations of Comparative Interventions
In EVIDEM, limitations of compared interventions were assumed in two levels: Low limitation and major limitation (5).
C.4) Lack of Alternative
Criterion related to lack of a suitable alternative was used for priority setting in the viewpoint of the citizens (24).
D) Status of Criteria Related to Economic Aspects in Included Studies
D.1) Cost -Effectiveness
In EVIDEM, one economic aspect was cost effectiveness (in two states: Without cost effectiveness and very cost effective) (5). To set the priority of health interventions, cost effectiveness (in two states: Without cost effectiveness and cost effectiveness) was used (6-8,12,15,16,18,21,34,37). To set the priority of health interventions, cost effectiveness (in two states: Cost effectiveness: Incremental cost effectiveness ratio lower than one and more than GDP per capita and without cost effectiveness: Incremental cost effectiveness ratio more than one and more than GDP per capita) was defined (19). Cost effectiveness (without cost effectiveness: Cost per DALY 3 times more than GDP per capita, average effective cost: Cost per Daly within 1-3 times more than GDP per capita, cost effectiveness: Cost per DALY lower than 1 and more than GDP per capita) was used for priority setting in Nepal (22). In Norway, cost effectiveness (in two states: Without cost effectiveness: Cost per DALY more than 1 of GDP per capita, and cost effectiveness: Cost per DALY lower than one time and more than GDP per capita) was defined for health care priority setting (23). In Ghana, cost effectiveness (without cost effectiveness: Cost per for DALY more than 3 times and more than GDP per capita, average cost effective: Cost per DALY within 1-3 times more than GDP per capita, cost effective: Cost per DALY lower than 1 and more than GDP per capita) was used (28).
D.2) Costs
In EVIDEM, one of the economic criteria was the effect of intervention on other health expenditures (5). To select new health technology, technology utilization cost for society and patient was used (8). In investment on health service innovation, taxpayers’ cost was assumed (9). Cost saving was used in the form of the following question in Europe: Does a potential considerable cost have an impact on the case of extensive utilization of technology? (13). Intervention cost was used for reimbursement decisions in health (16). In health and clinical services, cost for status management and potential costs changes were assumed (25). In Denmark, direct marginal costs of health care arising from the new technology were used (27). In Netherlands, reduction in cost of the health care, related to the technology, was one of the criteria (28). In Netherlands, direct intervention cost for each patient was used (29). In PATHS (The Health Technology Assessment Priority Setting) in UK, cost saving factor was used (34). In health care priority setting, economic criteria included the following items: What are predicted costs of the third party payer? How the costs are affected by employment? Does new technology provide predicted increase or decrease in health care costs to the society over a long period of time? Assuming that other costs exist, have they been compensated by potential benefits? (38).
D.3) Budget Impact
Budget impact was used as one of the main priority setting criteria in the World Health Technology Assessment Organization (3). Economic impact due to technology utilization was an important factor in CADTH (4). To use EVIDEM, one of the economic criteria was budget impact (5). For setting priorities in Ghana, the budget impact (an intervention has a high budget impact that covers more than 10% of the public annual health expenditures) was used (6,7). Budget impact and budget increase for the third party payer was one of the main factors of decision making in Germany (14). To determine priority-setting criteria in the State Health Organizations in the United States, availability of funds was used (16). Budget impact was used for health interventions priorities in Thailand (19). In Denmark, predicted budget impact due to technology utilization, was used (27). To assess the efficiency of EVIDEM framework, budget impact was used (31).
D.4) Economic Impact
In the World Health Technology Assessment Systems, economic impact (including direct technology costs, potential technology cost effectiveness and potential assessment cost effectiveness) was used (3). Economic impact (impact on the health system, government and society expenditures) was used in CADTH (4). Economic considerations were considered for decision making in health technologies in Germany (14). Economic impacts were used as one of the main criteria for allocating resources (15). Economic impact on household expenditure for prevention of exorbitant health costs was used (19). In technology acceptance in the hospital level, economic value creation was assumed (20).
D.5) Poverty Reduction
Poverty reduction in two states of neutral and positive was defined for health interventions priority setting (6,21). In Ghana, poverty reduction was used based on the following reason: Societies sought to provide therapeutic methods to that part of the society that benefits less than the other parts (7). In Nepal, poverty reduction in two states of neutral (when disease is not prevalent among the poor) and positive (when disease is highly prevalent among the poor) was defined (22).
D.6) Value for Money
To identify the potential priorities to assess the Health Technology Assessment Plan of UK NHS, the following question was used: "Does assessment most probably deal with providing value for money?" (26). To assess EVIDEM framework efficiency, value for money of intervention was used (31).
D.7) Financial Opportunity/Consequence
To set priorities in health, financial opportunity was assumed (25). In Netherlands, financial consequences of intervention over time were used (35).
D.8) Economic Productivity
In Norway, economic productivity criterion was defined as upraise of economic productivity through establishing extra non-health welfare benefits for all via tax system or other transfer methods (29). In developing countries, economic efficiency was used as one of the nonmedical elements (30).
D.9) Financial Protection
Financial protection against the costs of ill health was used in Norway (29).
D.10) Willingness to Pay Subside
In Norway, willingness to pay subsidies was in two ranges: More than 70% of the total health costs and less than 70% of the total health costs. This criterion was used to reduce poverty as defined (23).
D.11) Society Interests and Demand
In Korean Health Insurance Organization, society profit and demand implied that beneficiaries (patients, providers, insurers, policy makers or governments) sought for a specified service and there was a demand for improving quality (33).
D.12) Price and Sales Volume
Technology price and sales volume were used for decision making in Germany (14).
E) Status of Criteria Related to Evidence in Included Studies
E.1) Quality of Evidence
Quality of evidence related to health technology assessment, economic assessment and systematic review was used in CADTH (4). Quality of effectiveness and economic evidence was used for decision making concerning health technologies (14). For allocation of resources in health, quality of evidence was defined as the number of available evidence, evidence power and evidence relevance, characteristics of evidence, research ethics and requirements of evidence (15). Quality of evidence was used for priority setting in Iranian basic health insurance package (18).
E.2) Number of Evidence
Number of evidence was used in the World Health Technology Assessment Systems (3). In Latvia, adequacy of evidence about technology was used (18). Criterion related to completeness of side effects data in connection to technology was one of the priority setting criteria from the viewpoint of the citizens (24).
E.3) Relevance and Validity of Evidence
In EVIDEM, relevance and validity of evidence, with respect to the need for decision- making, was used (5).
E.4) Power of Evidences
To determine priority-setting criteria in State Health Organizations in the United States power of evidence was used (16).
E.5) Completeness and Consistency of Reporting Evidence
In EVIDEM, one of the criteria related to evidences was completeness and consistency in reporting evidence (5).
E.6) Adherence to Requirements of Decision making body
In EVIDEM, one of the criteria related to evidences was adherence of evidence to requirements of decision-making body (5).
F) Status of Other Criteria Related to Priority Setting in Included Studies
F.1) Issues Related to Health System
Variation of technology utilization in targeted clinical conditions was assumed in the Health Technology Assessment Organizations CADTH (3-4). System capacity and appropriate use of intervention was used in EVIDEM (5). For priority setting model in Europe, the following questions were considered: “Is there any inappropriate technology utilization potential?” and “Does technology utilization need to reorganize the organizational structure, purchase equipment or personnel training?” (13). Tasks, requirements, and health system capacity were used for allocation of resources in health systems (15). Feasibility of intervention acceptance in health system was used for reimbursement decisions in the health systems (16). For compiling priorities in health and clinical services research, variation of service use and the potential of interpreting the new knowledge were used (25). In Denmark, the criteria affecting health policies related to new technology was used (27). Potential benefits of the research projects and their potential impact on health care were used in Netherlands (30). To identify various criteria to determine health interventions priority, health system purposes and their constituents were used (34). In Netherlands, impact on health policies was used as one of the main criteria (35).
F.2) Sporadic Sub Criteria
Timeliness of health technologies assessment was used in CADTH (4). Service use time and its proper application were used in the priority-setting model of investment on health service innovation, using public preferences (9). Conditions arising from public health value, issues related to uncertainty, methodological issues and number of targeted indications of technology were used for decision-making coverage in health technologies in Germany (14). Need, as one of the criteria, was used for allocation of resources in the health system (15). The followings were all used to determine the priority setting criteria in State Health Organizations in the United States: Level of compulsion of service; seriousness; recommendation by other suppliers; conformity to instruction and federal priorities; previous allocation and its results; prevention and protection; instability; effect on personnel; maximization of Dollar rate for other plans; emergency issues; coordination with strategic plan; effectiveness on technical expert capacity; improvement tools; society interests; population orientation; new or extending plan against maintaining action; and social benefits (16). Timeliness and usefulness of health technology assessment were used in Latvia (18). To set the priority of health interventions in Thailand, variation in clinical practice was used (19). Knowledge creation was used for formulation of technology acceptance at the hospital level (20). To assess the Health Technology Assessment Plan of UK NHS to identify the potential priorities, the following questions were defined: “How long may benefits identification last?”, “How important is the initial assessment?”, “Are there any factors related to technology that can affect the importance of assessment use?” (26). In the health technology assessment priority setting model in Netherlands, experience and specialty availability and access to excellent research environment and its expansion were used (36). Experiences of world countries for priority setting were inputs, appropriate principles and effectiveness on politics (40).
F.3) Political, Social and Moral Issues
The controversial nature, psychosocial and moral considerations were used in health technology assessment organizations and CADTH (3-4). In EVIDEM, one of the criteria was moral framework, which included appropriateness of health goals (5). Consistency to moral and social values was one of the criteria for reimbursement decisions (11). Political profits were used for priority setting in State Health Organizations in the United States (16). Social, legal and moral concepts were used for priority setting in Latvia (18). To formulate priority setting of technology in a hospital, social value creation was used (20). Informing the potential on moral, legal, social and political profit issues was one of the criteria for priority setting (25). In priority setting in the health interventions in the developing countries, moral reasons and political conditions were used (37). Political considerations and society expectations were assumed about health technology decision making (39).
F.4) Benefits of Beneficiaries
Predicted demand range was used as one of the main priority setting criteria in Health Technology Assessment Organizations (3-4,18). In EVIDEM, one of the criteria was stakeholders' pressures (5). Benefits of beneficiaries and their pressures were used as one of the main criteria for allocation of resources in the health system (15). Criteria related to beneficiaries included this question: How are the viewpoints of all beneficiary groups indicated appropriately in a unit value criterion? (38).
F.5) Issues Related to Patients
A series of criteria were set for health technology decision making, and patients care improvement was one of them (14). Family or patient satisfaction was used in formulating technology priority setting model at the hospital level (20). Responding to patients’ legitimate non-health expectations was used for setting priorities of health interventions in social protection system in Mexico (34). Conditions arising from patients’ behavior were used for decision-making coverage in health technologies in Germany (39). To select health technology assessment titles and systematic review, patients/users’ concerns, information taken by users/patients, unmet information needs, attractive subjects for reading and what experts believe about users/patients’ needs or wants were used (41).
F.6) Issues Related to Decision Making Conditions
In EVIDEM, political and historical conditions were used (5). The magnitude of the problem was used for priority setting in state health organizations in the United States (16). The potential of informing the need for identifying the problem was used in health and clinical services research (25). In Korean health insurance organization, acceptability and qualitative of feasibility assessment were used (33). Six qualitative factors were used for priority setting: Institutions that made health-related decisions, people who made decision, factors taken into consideration, decision-making arguments, decision-making process and mechanism of challenging the decisions (42).
F.7) Fairness and Equity
Equity in access to health services, which was made possible by utilization of technology, was assumed as the priority setting criteria (5,15,27,39).
Discussion
The findings of the present study revealed that 25 out of 40 studies included in this research dealt with “Health outcome”, as the main criteria in priority setting of health technology assessment. The maximum frequency in this theme was “health effects/benefits” (8 studies). In the disease and target population, 24 studies dealt with this criterion, with “disease severity” having the maximum frequency in this theme (12 studies). Alternatively, five studies dealt with this criterion, with “the number of alternatives” having the maximum frequency in this theme (2 studies). With respect to the economic aspect, 35 studies dealt with this criterion, with “cost-effectiveness” having the maximum frequency in this theme (15 studies). Evidently, nine studies dealt with this criterion, with “quality of evidence” having the maximum frequency (4 studies). In other factors, 28 studies dealt with this criterion, with “issues concerning health system” having the maximum frequency (10 studies). The result of this study is comparable to that of the study by Guindo et al. (15) who found that the priority setting criteria frequencies in relevant studies included equity/fairness (32 times), efficacy/effectiveness (29), stakeholder interests and pressures (28), cost-effectiveness (23), strength of evidence (20), safety (19), mission and mandate of health system (19), organizational requirements and capacity (17), patient-reported outcomes (17) and need (16).
Conclusion
The results revealed an increasing demand for health technologies priority setting around the world and stressed on the necessity of application of a multi- criteria approach for appropriate decision making about healthcare technologies in health- related areas.
Acknowledgement
This study was part of a PhD dissertation, which was supported by Science and Research branch of Islamic Azad University, Tehran, Iran.
Limitations
During the performance of this research, there was no access to the Web of Science (WOS) database in Iran.
Appendix 1
1 . Search Strategy for the Cochrane Library .
| #1/health near/1 intervention*/1500 |
| #2/health near/1 technolog* /24380 |
| #3/health technology assessment /26301 |
| #4/HTA/ 16360 |
| #5/MeSH descriptor health technology assessment explode all trees /476 |
| #6/ (#1 or #2 or #3 or #4 or #5) /28142 |
| #7/priority near/1 setting /90 |
| #8/priorit* /42946 |
| #9/decision near/1 making/6730 |
| #10/MeSH descriptor priority setting explode all trees/201 |
| #11/MeSH descriptor decision making explode all trees /617 |
| #12/ (#7 or #8 or #9 or #10 or #11) /49167 |
| #13/ (#6 and #12) /2072 |
2 . Search Strategy for Pub Med .
| "#1/ health intervention*/7134 |
| "#2/ health technolog*/5560 |
| "#3/ health technology assessment/19722 |
| "#4/ HTA/2991 |
| "#5/ health technology assessment [MeSH Terms]/0 |
| "#6/ ((#1 or #2 or #3 or #4 or #5))/29983 |
| "#7/ priority setting/3751 |
| "#8/ priorit*/75538 |
| "#9/ decision making/192582 |
| "#10/ priority setting [MeSH Terms]/0 |
| "#11/ decision making [MeSH Terms]/124769 |
| "#12/ ((#7 or #8 or #9 or #10 or #11))/263325 |
| "#13/ ((#6 and #12))/3733 |
2. Search Strategy for Scopus .
| ((("health intervention*" OR "health technolog*" OR "health technology assessment" OR HTA)) AND (("priority setting"))) AND ( LIMIT-TO(SUBJAREA,"MEDI" ) OR LIMIT-TO(SUBJAREA,"BIOC" ) OR LIMIT-TO(SUBJAREA,"HEAL" ) OR LIMIT-TO(SUBJAREA,"NURS" ) ) AND ( LIMIT-TO(DOCTYPE,"ar" ) OR LIMIT-TO(DOCTYPE,"re" ) ) AND ( LIMIT-TO(LANGUAGE,"English" ) ) / 1207 |
Appendix 2 . Classification of Main Criteria and Sub Criteria based on Frequency in reviewed Studies (in pre-Assessment and also in Assessment phase) .
| Main Criteria | Health Outcomes | Disease and Target Population | Alternatives | Economic Aspects | Evidence | Other Factors | ||||||
| Sub criteria | Frequency | Sub criteria | Frequency | Sub criteria | Frequency | Sub criteria | Frequency | Sub criteria | Frequency | Sub criteria | Frequency | |
| 1 |
Health effects/benefits (6-13) |
8 |
Disease severity (6-8,19,21-23,28-31) |
12 |
Number of alternatives (3-4) |
2 |
Cost-effectiveness (5-8,12,15-16,18-19,21-23,28,34,37) |
15 |
Quality of evidence (4,14-15,18) |
4 |
Issues related to health system (3-5,13,15-16,25,27,30,34-35) |
11 |
| 2 |
Clinical effects/benefits (3-4,14-17) |
7 |
Disease burden (3-4,14,25,29,32-34) |
8 |
Availability of alternative (14) |
1 |
Costs (8-9,13,25,27-29,34,38) |
11 |
Number of evidence (3,18,24) |
3 |
Sporadic sub criteria (4,9,14-16,18-20,26,36,40) |
11 |
| 3 |
Efficacy/effectiveness (4-5,18-19) |
4 |
Target population age (6-7,9,14,21-23) |
7 |
Limitations of comparative interventions (5) |
1 |
Budget impact (3-7,14,16,19,27) |
10 |
Evidence relevance and validity (5) |
1 |
Political, social and moral issues (3-5,11,16,18,20,25,37,39) |
10 |
| 4 |
Individual health benefits (21-23) |
3 |
Population size (5,14,19,25) |
3 |
Lack of alternatives (24) |
1 |
Economic impact (3-4,14-15,19-20) |
6 |
Power of evidence (16) |
1 |
Benefits of beneficiaries (3-5,15,18,38) |
6 |
| 5 |
Safety (5,14-15) |
3 |
Number of potential beneficiaries (21,23,28) |
3 | - | - |
Poverty Reduction (6-7,21-22) |
4 |
Completeness and consistency of reporting evidence (5) |
1 |
Issues related to patients (14,20,34,39,41) |
5 |
| 6 |
Quality of life (24) |
1 |
Characteristics of target social groups for intervention (29,31) |
2 | - | - |
Value for money (26,31) |
2 |
Adherence to requirements of decision making body (5) |
1 |
Issues related to decision-making conditions (5,16,25,33,42) |
5 |
| 7 |
Potential changes in health consequences (25) |
1 |
Number of patients (8,35) |
2 | - | - |
Financial opportunity/consequences (25,35) |
2 | - | - |
Fairness and equity (5,15,27,39) |
4 |
| 8 |
The effect of assessment on reduction of uncertainty (26) |
1 |
Effect of technology on reduction of disease prevalence and incidence (36) |
1 | - | - |
Economic productivity (29-30) |
2 | - | - | - | - |
| 9 |
Marginal benefits (27) |
1 |
Disease impacts (15) |
1 | - | - |
Financial protection (29) |
1 | - | - | - | - |
| 10 |
Ability to reduce own health risk (14) |
1 |
Effect on targeted groups (16) |
1 | - | - |
Subsidized Payment (23) |
1 | - | - | ||
| 11 | Potential to extend life (24) | 1 |
Size of vulnerable population (28) |
1 | - | - |
Society interest and demand (33) |
1 | - | - | - | - |
| 12 | Potential to detect a condition which, if treated early, averts costs in the future | 1 | - | - | - | - |
Technology price and sale volume |
1 | - | - | - | - |
Cite this article as: Mobinizadeh M, Raeissi P, Nasiripour AA, Olyaeemanesh A, Tabibi SJ. The health systems' priority setting criteria for selecting health technologies: A systematic review of the current evidence. Med J Islam Repub Iran 2016 (16 February). Vol. 30:329.
References
- 1. Carlsson P. Health technology assessment and priority setting for health policy in Sweden. International journal of technology assessment in health care. 2004;20(01):44–54. doi: 10.1017/s0266462304000777. [DOI] [PubMed] [Google Scholar]
- 2.Bridges JF, Jones C. Patient-based health technology assessment: a vision of the future. Int J Technol Assess Health Care. 2007;23(1):30–5. doi: 10.1017/S0266462307051549. [DOI] [PubMed] [Google Scholar]
- 3.Noorani HZ, Husereau DR, Boudreau R, Skidmore B. Priority setting for health technology assessments: a systematic review of current practical approaches. International journal of technology assessment in health care. 2007;23(03):310–315. doi: 10.1017/s026646230707050x. [DOI] [PubMed] [Google Scholar]
- 4.Husereau D, Boucher M, Noorani H. Priority setting for health technology assessment at CADTH. International journal of technology assessment in health care. 2010;26(3):341–347. doi: 10.1017/S0266462310000383. [DOI] [PubMed] [Google Scholar]
- 5.Goetghebeur MM, Wagner M, Khoury H, Rindress D, Grégoire JP, Deal C. Combining multicriteria decision analysis, ethics and health technology assessment: applying the EVIDEM decision making framework to growth hormone for Turner syndrome patients. Cost Eff Resour Alloc. 2010;8(1):4. doi: 10.1186/1478-7547-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baltussen R. Priority setting of public spending in developing countries: do not try to do everything for everybody. Health Policy. 2006;78(2):149–156. doi: 10.1016/j.healthpol.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 7.Baltussen R, Stolk E, Chisholm D, Aikins M. Towards a multi‐criteria approach for priority setting: an application to Ghana. Health economics. 2006;15(7):689–696. doi: 10.1002/hec.1092. [DOI] [PubMed] [Google Scholar]
- 8.Douw K, Vondeling H. Selection of new health technologies for assessment aimed at informing decision making: A survey among horizon scanning systems. International journal of technology assessment in health care. 2006;22(02):177–183. doi: 10.1017/S0266462306050999. [DOI] [PubMed] [Google Scholar]
- 9.Erdem S, Thompson C. Prioritizing health service innovation investments using public preferences: a discrete choice experiment. BMC health services research. 2014;14(1):360. doi: 10.1186/1472-6963-14-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jankauskiene D, Petronyte G. A Model for HTI Priority Setting: Experience In Lithuania. International journal of technology assessment in health care. 2013;29(04):450–455. doi: 10.1017/S0266462313000470. [DOI] [PubMed] [Google Scholar]
- 11.Leider JP, Resnick B, Kass N, Sellers K, Young J, Bernet P. et al. Budget-and Priority-Setting Criteria at State Health Agencies in Times of Austerity: A Mixed-Methods Study. American journal of public health. 2014;104(6):1092–1099. doi: 10.2105/AJPH.2013.301732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Norheim OF, Ekeberg Ø, Evensen SA, Halvorsen M, Kvernebo K. Adoption of new health care services in Norway (1993–1997): specialists’ self-assessment according to national criteria for priority setting. Health Policy. 2001;56(1):65–79. doi: 10.1016/s0168-8510(00)00135-4. [DOI] [PubMed] [Google Scholar]
- 13.Wild C, Simpson S, Douw K, Geiger-Gritsch S, Mathis S, Langer T. Information service on new and emerging health technologies: Identification and prioritization processes for a European Union–wide newsletter. International journal of technology assessment in health care. 2009;25(S2):48–55. doi: 10.1017/S0266462309990687. [DOI] [PubMed] [Google Scholar]
- 14.Fischer KE. A systematic review of coverage decision-making on health technologies—Evidence from the real world. Health Policy. 2012;107(2):218–230. doi: 10.1016/j.healthpol.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Guindo LA, Wagner M, Baltussen R, Rindress D, van Til J, Kind P, Goetghebeur MM. From efficacy to equity: Literature review of decision criteria for resource allocation and healthcare decision making. Cost Eff Resour Alloc. 2012;10(9):10–1186. doi: 10.1186/1478-7547-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diaby V, Goeree R. How to use multi-criteria decision analysis methods for reimbursement decision-making in healthcare: a step-by-step guide. Expert review of pharmacoeconomics & outcomes research. 2014;14(1):81–99. doi: 10.1586/14737167.2014.859525. [DOI] [PubMed] [Google Scholar]
- 17.Townsend J, Buxton M, Harper G. Prioritisation of health technology assessment The PATHS model: methods and case studies. National Coordinating Centre for Health Technology Assessment. 2003 doi: 10.3310/hta7200. [DOI] [PubMed] [Google Scholar]
- 18.Dehnavieh R, Rashidian A, Maleki M, Tabibi SA, Ibrahimi H, Pour SNH. Criteria for Priority-setting in Iran Basic Health Insurance Package: Exploring the Perceptions of Health Insurance Experts. HealthMED. 2010;7(2):1542. [Google Scholar]
- 19.Youngkong S, Baltussen R, Tantivess S, Mohara A, Teerawattananon Y. Multicriteria decision analysis for including health interventions in the universal health coverage benefit package in Thailand. Value in Health. 2012;15(6):961–970. doi: 10.1016/j.jval.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Lettieri E, Masella Masella, C C. Priority setting for technology adoption at a hospital level: Relevant issues from the literature. Health policy. 2009;90(1):81–88. doi: 10.1016/j.healthpol.2008.07.007. [DOI] [PubMed] [Google Scholar]
- 21.Baltussen R, Niessen L. Priority setting of health interventions: the need for multi-criteria decision analysis. Cost Effectiveness and Resource Allocation. 2006;4(1):14. doi: 10.1186/1478-7547-4-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baltussen RMPM, Ten Asbroek AHA, Koolman X, Shrestha N, Bhattarai P, Niessen LW. Priority setting using multiple criteria: should a lung health programme be implemented in Nepal? Health Policy and Planning. 2007;22(3):178–185. doi: 10.1093/heapol/czm010. [DOI] [PubMed] [Google Scholar]
- 23.Defechereux T, Paolucci F, Mirelman A, Youngkong S, Botten G, Hagen TP. et al. Health care priority setting in Norway a multicriteria decision analysis. BMC health services research. 2012;12(1):39. doi: 10.1186/1472-6963-12-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Menon D, Stafinski T. Engaging the public in priority‐setting for health technology assessment: findings from a citizens’ jury. Health Expectations. 2008;11(3):282–293. doi: 10.1111/j.1369-7625.2008.00501.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berra S, Sánchez E, Pons J, Tebé C, Alonso J, Aymerich M. Setting priorities in clinical and health services research: properties of an adapted and updated method. International journal of technology assessment in health care. 2010;26(02):217–224. doi: 10.1017/S0266462310000012. [DOI] [PubMed] [Google Scholar]
- 26.Chase D, Milne R, Stein K, Stevens A. What are the relative merits of the sources used to identify potential research priorities for the NHS HTA programme? International journal of technology assessment in health care. 2000;16(03):743–750. doi: 10.1017/s0266462300102028. [DOI] [PubMed] [Google Scholar]
- 27.Douw K, Vondeling H, Oortwijn W. Priority setting for horizon scanning of new health technologies in Denmark: Views of health care stakeholders and health economists. Health policy. 2006;76(3):334–345. doi: 10.1016/j.healthpol.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 28.Jehu‐Appiah C, Baltussen R, Acquah C, Aikins M, d'Almeida SA, Bosu WK. et al. Balancing equity and efficiency in health priorities in Ghana: the use of multicriteria decision analysis. Value in Health. 2008;11(7):1081–1087. doi: 10.1111/j.1524-4733.2008.00392.x. [DOI] [PubMed] [Google Scholar]
- 29.Norheim OF, Baltussen R, Johri M, Chisholm D, Nord E, Brock D. et al. Guidance on priority setting in health care (GPS-Health): the inclusion of equity criteria not captured by cost-effectiveness analysis. Cost Effectiveness and Resource Allocation. 2014;12(1):18. doi: 10.1186/1478-7547-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Youngkong S, Kapiriri L, Baltussen R. Setting priorities for health interventions in developing countries: a review of empirical studies. Tropical Medicine & International Health. 2009;14(8):930–939. doi: 10.1111/j.1365-3156.2009.02311.x. [DOI] [PubMed] [Google Scholar]
- 31.Youngkong S, Tromp N, Chitama D. The EVIDEM framework and its usefulness for priority setting across a broad range of health interventions. Cost Effectiveness and Resource Allocation. 2011;9:8. doi: 10.1186/1478-7547-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bastian H, Scheibler F, Knelangen M, Zschorlich B, Nasser M, Waltering A. Choosing health technology assessment and systematic review topics: The development of priority-setting criteria for patients’ and consumers’ interests. International journal of technology assessment in health care. 2011;27(04):348–356. doi: 10.1017/S0266462311000547. [DOI] [PubMed] [Google Scholar]
- 33.Cho W, Lee S, Kang HY, Kang M. Setting national priorities for quality assessment of health care services in Korea. International Journal for Quality in Health Care. 2005;17(2):157–165. doi: 10.1093/intqhc/mzi018. [DOI] [PubMed] [Google Scholar]
- 34.González-Pier E, Gutiérrez-Delgado C, Stevens G, Barraza-Lloréns M, Porras-Condey R, Carvalho N. et al. A Priority setting for health interventions in Mexico's System of Social Protection in Health. The Lancet. 2006;368(9547):1608–1618. doi: 10.1016/S0140-6736(06)69567-6. [DOI] [PubMed] [Google Scholar]
- 35.Oortwijn WJ, Vondeling H, van Barneveld T, van Vugt C, Bouter LM. Priority setting for health technology assessment in The Netherlands: principles and practice. Health Policy. 2002;62(3):227–242. doi: 10.1016/s0168-8510(02)00037-4. [DOI] [PubMed] [Google Scholar]
- 36.Oortwijn W, Banta D, Vondeling H, Bouter L. Identification and priority setting for health technology assessment in The Netherlands: actors and activities. Health Policy. 1999;47(3):241–253. doi: 10.1016/s0168-8510(99)00020-2. [DOI] [PubMed] [Google Scholar]
- 37.Oortwijn WJ, Vondeling H, Bouter L. The use of societal criteria in priority setting for health technology assessment in The Netherlands: initial experiences and future challenges. International journal of technology assessment in health care. 1998;14(02):226–236. doi: 10.1017/s0266462300012216. [DOI] [PubMed] [Google Scholar]
- 38.Girod S, Axene DV. Prospective value-based assessment of new health care technologies and practices. Managed Care. 2000;9(8):38–40. [PubMed] [Google Scholar]
- 39.Gallego G, Fowler S, Van Gool K. Decision makers' perceptions of health technology decision making and priority setting at the institutional level. Australian Health Review. 2008;32(3):520–527. doi: 10.1071/ah080520. [DOI] [PubMed] [Google Scholar]
- 40.Sabik LM, Lie RK. Priority setting in health care: lessons from the experiences of eight countries. Int J Equity Health. 2008;7:4. doi: 10.1186/1475-9276-7-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bastian H, Scheibler F, Knelangen M, Zschorlich B, Nasser M, Waltering A. Choosing health technology assessment and systematic review topics: The development of priority-setting criteria for patients’ and consumers’ interests. International journal of technology assessment in health care. 2011;27(04):348–356. doi: 10.1017/S0266462311000547. [DOI] [PubMed] [Google Scholar]
- 42.Singer PA, Martin DK, Giacomini M, Purdy L. Priority setting for new technologies in medicine: qualitative case study. BMJ. 2000;321(7272):1316–1318. doi: 10.1136/bmj.321.7272.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]