Abstract
Functional magnetic resonance imaging (fMRI) was used to investigate the neural processing characteristics associated with word retrieval abilities after a phonologically-based treatment for anomia in two stroke patients with aphasia. Neural activity associated with a phonological and a semantic task was compared before and after treatment with fMRI. In addition to the two patients who received treatment, two patients with aphasia who did not receive treatment and 10 healthy controls were also scanned twice. In the two patients who received treatment, both of whose naming improved after treatment, results showed that activation patterns changed after treatment on the semantic task in areas that would have been expected (e.g., left hemisphere frontal and temporal areas). For one control patient, there were no significant changes in brain activation at the second scan; a second control patient showed changes in brain activation at the second scan, on the semantic task, however, these changes were not accompanied with improved performance in naming. In addition, there appeared to be bilateral, or even more right than left hemisphere brain areas activated in this patient than in the treated patients. The healthy control group showed no changes in activation at the second scan. These findings are discussed with reference to the literature on the neural underpinnings of recovery after treatment for anomia in aphasia.
Keywords: Aphasia, Anomia, Treatment, Neuroimaging, fMRI
1. Introduction
The use of neuroimaging techniques to study the neural underpinnings of recovery of language abilities following stroke has recently come to the forefront. As Pizzamiglio, Galati, and Committeri (2001) note in their review, many studies to date have focused on the neural processing characteristics associated with recovery from aphasia (i.e., in the absence of treatment). Evidence of both homologousright hemisphere (RH) adaptationand increased left hemisphere (LH) perilesional activity has been found (e.g., Calvert et al., 2000; Cherney & Small, 2006; Fernandez et al., 2004; Heiss, Kessler, Thiel, Ghaemi, & Karbe, 1999; Jodzio, Drumm, Nyka, Lass, & Gasecki, 2005; Rosen, 2000; Saur et al., 2006; Szekeres, Ylvisaker,& Cohen, 1987). The respective roles of the right and left hemispheres continue to be debated with regards to the question of the effects of neuroplasticity in recovery from aphasia, however Crosson et al. (2007) point out that the most fruitful approach to this question is not whether one or the other hemisphere plays a role in recovery, but rather, when and under what circumstances each hemisphere contributes to recovery.
An emerging area of enquiry is the investigation of the neural underpinnings of recovery following therapy for aphasia. Rijntjes and Weiller (2002) raise the important question of whether an observed cortical reorganization following treatment is responsible for a measurable behavioral change. Improved understanding at this level could potentially better inform theoretically motivated treatment approaches. The potential to identify therapy-induced areas of activation is encouraging based upon the studies conducted to date (e.g., Belin et al., 1996; Breier, Maher, Schmadeke, Hasan, & Papanicolaou, 2007; Cornelissen et al., 2003; Farias, Davis, & Harrington, 2006; Léger et al., 2002; Meinzer, Wienbruch, Djundja, Barthel, & Rockstroh, 2004; Musso et al., 1999; Pulvermüller, Hauk, Zohsel, Neininger, & Mohr, 2005; Richter, Miltner, & Straube, 2008; Small, Flores, & Noll, 1998; Wierenga et al., 2006). For example, Meinzer et al. (2004), using magnetoencephalography (MEG), found evidence for changes in perilesional activity, which was correlated with the amount of change in language functions after treatment in a large group of patients with chronic aphasia.
Recently, some studies have investigated neural activation patterns following treatment that was specifically aimed at improving anomia (i.e., word naming). For example, Léger et al. (2002) used functional magnetic resonance imaging (fMRI) to explore areas of activation for a picture naming task pre- and post-therapy in an individual with aphasia who had a naming deficit. They found that the pattern of activation post-therapy more closely mirrored that of healthy controls, with greater activation in the LH language areas surrounding the lesion and, in particular, in the left inferior frontal gyrus. Interestingly, they also found continued RH activation post-therapy, as well as activation of the left supra-marginal gyrus. They noted that the left supra-marginal gyrus is not typically associated with naming and suggested that it might represent a compensatory strategy induced by the therapy – specifically a greater attention to phonological features. A similar finding was found by Cornelissen et al. (2003) using MEG. They investigated the neural processing characteristics associated with a naming task in three individuals with a moderate anomia due to phonological output deficits pre- and post-therapy. For all three patients, naming improved post-therapy and was associated with greater activation in the left inferior parietal lobe. The authors attributed this to improved phonological encoding as a function of the therapy. Using time-resolved fMRI, Peck and colleagues demonstrated a homologous right hemisphere shift as a function of improved verbal response in one study (Peck et al., 2004), but not a subsequent one (Crosson et al., 2005). Davis, Harrington, and Baynes (2006) delivered an intensive semantic treatment to improve naming in one patient. The patient demonstrated improvements in both single word naming and noun production in connected speech after therapy, and fMRI showed increased activation of the left inferior frontal cortex and the right inferior posterior temporal cortex after therapy. Fridriksson and colleagues (Fridriksson, Morrow-Odom, Moser, Fridriksson, & Baylis, 2006; Fridriksson et al., 2007) have conducted two studies. In one (Fridriksson et al., 2006), three participants underwent three fMRI sessions both before and after therapy. In the two participants who benefited from the treatment, changes in perilesional activity in the left hemisphere as well as right hemisphere activation were noted. These included changes in the left temporal and the right posterior inferior parietal areas (Patient 1); and the frontal poles, the anterior cingulate gyrus and the left posterior supra-marginal gyrus (Patient 3). In a second study, Fridriksson et al. (2007) found increased activity bilaterally in the precuneus in two nonfluent patients who responded well to a combined semantic-phonological approach to naming treatment. Meinzer and colleagues (Meinzer, Obleser, Flaisch, Eulitz, & Rockstroh, 2007; Meinzer et al., 2006; Meinzer et al., 2008) have conducted both fMRI and MEG studies to investigate neuroplastic changes on naming abilities after Constraint-Induced Aphasia Therapy (CIAT). Meinzer et al. (2006) showed that correct word retrieval after treatment was associated with increased activation in the right inferior frontal gyrus (IFG) in one patient, but more bilaterally (in frontotemporal areas) in another patient (Meinzer et al., 2007). In their most recent study Meinzer et al. (2008) have used MEG in addition to fMRI to show that improved naming abilities in a group of eleven patients with chronic aphasia were correlated with increased activation within LH perilesional areas.
Based upon current theoretical models (e.g., Foygel & Dell, 2000), and as is evident from several of the studies reviewed above, of particular relevance to the study of naming difficulties in patients with aphasia are the domains of semantic and phonological processing. The results of recent investigations into these two domains in healthy participants have converged upon a consensus of brain areas involved. With regard to semantic processing, numerous studies undertaken with a variety of neuroimaging techniques (e.g., fMRI, MEG, positron emission tomography (PET)) and tasks (e.g., word fluency, category judgment) have consistently identified two particular areas of high importance – the left inferior frontal gyrus (LIFG), often the anterior portion, and the left middle temporal gyrus (Baxter et al., 2003; Binder et al., 1997; Calvert et al., 2000; McDermott, Petersen, Watson, & Ojemann, 2003; Perani et al., 2003; Roskies, Fiez, Balota, Raichle, & Petersen, 2001; Whatmough & Chertkow, 2002). With regard to phonological processing, the LIFG (often the posterior portion) has been identified as a critical area of activation (McDermott et al., 2003, Paulesu et al., 1997; Perani et al., 2003). In addition, activation of the left inferior parietal gyrus, including the supra-marginal gyrus, has been implicated in a number of phonological tasks including letter word fluency (Perani et al., 2003), rhyming (Kareken, Lowe, Chen, Lurito, & Mathews, 2000; Léger et al., 2002; Lurito, Kareken, Lowe, Chen, & Mathews, 2000) and naming (Cornelissen et al., 2003). Specifically in relation to picture naming, areas identified as being preferentially activated overlap with the above-mentioned areas for semantic and phonological processing. In healthy participants, picture naming has been shown to activate a large bilateral network (see Murtha, Chertkow, Beauregard, & Evans, 1999; Price, Devlin, Moore, Morton, & Laird, 2005).
In summary, studies that have investigated the neural underpinnings of recovery following naming therapy in particular, have generally found activation post-therapy in areas that have been linked to semantic and/or phonological processing in healthy participants, with the exception of Fridriksson et al. (2007) who also found post-treatment changes in areas not typically associated with language processing. In addition, some have reported increased LH compared to RH activation after therapy (Cornelissen et al., 2003; Meinzer et al., 2004; Meinzer et al., 2007); others have found increased RH activation after therapy (Meinzer et al., 2006; Peck et al., 2004); while still others have reported bilateral activation after therapy (Fridriksson et al., 2006; Léger et al., 2002; Meinzer et al., 2007). Patterns of activation have also been reported to be more similar to controls’ after therapy in one study (Léger et al., 2002), but not similar to controls’ in another (Fridriksson et al., 2007).
These studies are notable in their attempts to correlate therapyinduced improvements in naming performance with neural reorganization. They do, however, suffer from some methodological limitations. For instance, most studies do not include either a healthy control group tested at two time points or an untreated aphasic group, making it difficult to rule out potential test–retest effects (Carel et al., 2000) and effects of maturation (or time). In addition, with some notable exceptions (e.g., Cornelissen et al., 2003; Fridriksson et al., 2007; Léger et al., 2002), most treatment approaches were not specifically designed to treat word finding impairments, making it uncertain whether the activation findings reflect changes in word production per se or language processing more broadly.
In the current investigation we used fMRI to investigate the neural processing characteristics associated with word retrieval abilities after treatment for anomia. Incorporating appropriate control groups, we compared performance of individuals with aphasia on language tasks before and after a therapy program specifically targeted at increasing the awareness of the phonological aspects of words (Leonard, Rochon, & Laird, 2008). Participants from three groups (age-matched healthy controls, patients with aphasia who received treatment, patients with aphasia who did not receive treatment), were scanned twice, thereby avoiding possible confounds related to test–retest effects and maturation. The time period between scans for the healthy control group and the untreated aphasic participants was approximately of the same length as that of the treated group. This design also allows us to compare our activation findings to those for healthy control participants on the same tasks. Second, the activation tasks used during scanning did not include a naming task, but rather included a rhyme judgment task (to tap phonological processing) and a semantic judgment task. Since naming tasks arguably require the activation of both semantic and phonological information of a word, we chose to use the judgment tasks in an attempt to isolate semantic processing from phonological processing (similar to McDermott et al., 2003). The aim was to enable us to better examine independent effects of phonological therapy on these two processes and their associated neural mechanisms while addressing the point raised by Rijntjes and Weiller (2002) of investigating the relationship between cortical reorganization and behavioural change.
Since the groups of healthy controls and untreated patients with aphasia served as control groups for this investigation, patterns of activation were expected to remain relatively unchanged in these groups between the two scans. Based on the literature to date, it was hypothesized that post-therapy for the treated patients with aphasia, when performing the rhyme judgment task, there would be greater LH than RH activation and more LH perilesional activation associated with improved performance in naming. Moreover, because the therapy specifically targets phonological processing, activation in the left supra-marginal gyrus post-therapy was expected (Cornelissen et al., 2003; Léger et al., 2002). Activation by treated patients in the LIFG and middle temporal areas, as well as increased left hemisphere activation post-therapy, during the semantic judgment task will provide evidence of the influence of a phonologically based therapy on semantic processing.
2. Method
2.1. Participants
2.1.1. Participants with aphasia
Six individuals with aphasia participated in this investigation. Three of the individuals received treatment (ATr). Three served as untreated control patients with aphasia (AUn). One participant in the ATr group and one in the AUn group were each subsequently excluded from this study due to either motion artefact in the data (ATr participant) or premature termination of the scan at the patient’s request (AUn participant). The two remaining treated patients included one woman (ATr1, age: 50 years; years of education: 16) and one man (ATr2, age: 73 years; years of education: 12). They were part of the larger study noted above investigating the efficacy of a phonological treatment (PCA) for improving word finding abilities in individuals with aphasia (Leonard et al., 2008).1 The untreated patients with aphasia were both men (AUn1, age: 83 years, years of education: 14; AUn2, age: 63 years, years of education:12). They were on a waiting list for the same PCA treatment that the treated participants received. The AUn participants received treatment after the final follow-up assessment in the PCA study. All participants with aphasia were recruited from aphasia centres in the Toronto area.
The patients participating in this study had experienced a single left-hemisphere cerebrovascular accident and were at least one year post-onset at the time of enrolment. ATr1’s lesion was in the left posterior frontal, temporal and parietal lobes; ATr2’s lesion was in left frontotemporal areas; AUn1’s lesion was in left temporoparietal regions, and AUn2’s lesion was in the left posterior temporal and occipital lobes. Classification of aphasia, based on the results of the Boston Diagnostic Aphasia Examination (Goodglass, Kaplan, & Barresi, 2001) revealed that ATr1 had Broca’s aphasia, ATr2 a mixed nonfluent aphasia, AUn1 Wernicke’s aphasia, and AUn2 anomic aphasia. All patients had a naming impairment defined by less than 75% accuracy on the Boston Naming Test (BNT) (Goodglass et al., 2001). All participants had visual perceptual abilities within normal limits as determined by the Minimal Feature Matching subtest of the Birmingham Object Recognition Battery (BORB) (Riddoch & Humphreys, 1993). In order to rule out the presence of apraxia of speech, all participants were administered a motor speech exam comprised of tasks which typically identify apraxia of speech such as diadokinetic rate, repetition of words of increasing length, etc. The results were reviewed by two speech-language pathologists. None of the participants was receiving formal speech-language therapy at the time of testing (see Table 1 for a summary of patient characteristics).
Table 1.
Participant characteristics and scores (percent correct) on background tests for patients with aphasia.
| Participant | ||||
|---|---|---|---|---|
|
| ||||
| ATr1 | ATr2 | AUn1 | AUn2 | |
| Background information | ||||
| Age (years) | 50 | 73 | 83 | 63 |
| Education (years) | 16 | 12 | 14 | 12 |
| Gender | F | M | M | M |
| Time post-onset (years) | 3.5 | 4 | 2.5 | 4 |
| Lesion site | Left posterior frontal, temporal & parietal | Left frontotemporal | Left temporoparietal | Left posterior temporal and occipital |
| Aphasia typea | Broca’s | Mixed nonfluent | Wernicke’s | Anomia |
| Tests [mean (S.D.), range for normative date] | ||||
| Naming severity | ||||
| BNT [94, 78.3–100]b | 13 | 40 | 33 | 40 |
| Input processing | ||||
| Pyramids and palm trees test [98–99]c | 83 | 81 | 96 | 96 |
| PALPA 47 spoken word – picture matching [98.2 (1.07), 87.5–100] | 87 | 90 | 79 | 100 |
| Output processing | ||||
| PNT [96 (7.0)] | 49 | 64 | 58 | 80 |
| PALPA 53 word repetition [99.5 (0.83)] | 88 | 93 | 53 | 100 |
| PALPA 53 oral reading [99.9 (0.19)] | 65 | 93 | 98 | 90 |
Note. nt = not tested; BNT – Boston Naming Test (Goodglass et al., 2001); PALPA – Psycholinguistic Assessments of Language Processing in Aphasia (Kay et al., 1992); Pyramids and Palm Trees (Howard & Patterson, 1992); PNT – Philadelphia Naming Test (Roach et al., 1996).
Aphasia type determined based on performance on Boston Diagnostic Aphasia Examination (BDAE; Goodglass et al., 2001).
Normative data based on the 60-item version.
Range of values is the only normative data available for this test.
2.1.2. Healthy control group
A group of twelve healthy controls (HC) was also included. The data for two HC participants were excluded due to motion artefact and vision problems, respectively. The remaining group of ten healthy controls was composed of three women and seven men (mean age: 61; mean level of education: 16 years). Individuals in the HC group were screened on a variety of tests to rule out the possibility of dementia (Mini-Mental State Examination, Folstein, Folstein, & McHugh, 1975) and naming (BNT) or visual spatial deficits (BORB).
All participants (both patient and HC) were right-handed, English-speaking individuals. For all participants with aphasia, hearing was within normal limits in at least one ear as determined by a hearing screening at less than 40 dB HL at the speech frequencies 0.5, 1 and 2 kHz (Ventry & Weinstein, 1982). For the HC group hearing was within normal limits as determined by self-report. All participants had normal or corrected to normal vision. As well, for all participants exclusionary criteria included a history of drug or alcohol abuse, a history of major psychiatric illness and/or neurological illness. For all participants, standard contraindications to MRI (e.g., metallic implants, claustrophobia, etc.) also served as exclusionary criteria for this study. All participants provided written informed consent to participate in this investigation.
2.2. Characterization of patients’ naming deficits
Naming impairments can result from impaired access to semantic, lexical, and/or phonological representations (see Martin, Fink, Renvall, & Laine, 2006; Schwartz, Dell, Martin, Gahl, & Sobel, 2006). In an effort to determine the level of impairment in the patients in this study, additional tests were administered (see Table 1). The integrity of semantic representations was assessed using the picture version of the Pyramids and Palm Trees Test (Howard & Patterson, 1992). Based on the criterion that individuals who score 90% or better do not have a clinically significant impairment, AUn1 and AUn2 can be considered to have intact semantic representations, whereas ATr1 and ATr2 appear to have at least some degree of impairment in conceptual semantics. To assess the status of lexical semantic knowledge, the spoken word-picture matching subtest of the Psycholinguistic Assessments of Language Processing in Aphasia (PALPA) (Kay, Lesser, & Coltheart, 1992) was administered.
As can be seen in the table, performance for all but one participant (AUn1) was within the range of normal for spoken word-picture matching. Based on the results of the tasks above, it would appear that all patients but AUn2 may have some degree of either conceptual and/or lexical semantic impairment, albeit mild, contributing to their word production difficulties. As can be seen in Table 1, performance on naming, as measured by both the BNT and the Philadelphia Naming Test (PNT) (Roach, Schwartz, Martin, Grewal, & Brecher, 1996) was below normal for all participants. With the exception of AUn2 on word repetition, performance on word repetition and oral word reading tasks was also below normal for all participants. To analyze patients’ performance on these tasks, we employed the coding scheme recommended for the PNT (Roach et al., 1996) which has been useful in characterizing naming deficits according to computational cognitive models (Dell, Lawler, Harris, & Gordon, 2004; Foygel & Dell, 2000). As can be seen in Table 2, ATr1 made a preponderance of semantic errors in naming, followed by ‘other’ errors which consisted mostly of picture part descriptions. This pattern of errors has been characterized as indicating difficulties in activating a lexical representation from conceptual semantics (Laine & Martin, 2006), which is consistent with ATr1’s pattern of performance on the Pyramids and Palm Trees test, mentioned above. Her errors in repetition, while few, are more phonologically based and her errors in oral reading are shared mostly between semantic and phonologically-based errors. ATr2 made a preponderance of omissions, followed by semantic errors in naming. This pattern of errors is also consistent with difficulties activating lexical representations from conceptual semantics (Laine & Martin, 2006), and, as for ATr1, is also consistent with the patient’s performance on the Pyramids and Palm Trees test. ATr2 made very few errors on the repetition task, though his errors were phonological in nature. His errors in oral reading, while few again, were not easily ascribable to either category. Based on this pattern of deficits, we cannot rule out for either of these two patients the possibility that they have difficulties with the phonological processing of words. However, a lack of phonological errors in naming in the presence of good repetition, as is found in ATr1 and ATr2 has been characterized as indicating that “output phonological processes are relatively intact” (Laine & Martin, 2006, p. 101). For both patients, this pattern of relative strengths and weaknesses suggests that with relatively mild lexical processing difficulties and relatively intact phonological processing, patients’ naming impairments appear to arise from a difficulty mapping between lexical and phonological output processing.
Table 2.
Number of error types on the naming, repetition and oral reading tasks for treated and untreated patients.
| Participant Test (n) | Error type | ||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Omissions | Formal | Semantic | Mixed | Nonwords | Unrelated | Other | |
| ATr1 | |||||||
| PNT (175) | 9 | 1 | 40 | 4 | 7 | 5 | 24 |
| PALPA 53 repetition (40) | 0 | 3 | 0 | 0 | 2 | 0 | 0 |
| PALPA 53 oral reading (40) | 2 | 5 | 4 | 0 | 1 | 1 | 1 |
| ATr2 | |||||||
| PNT (175) | 28 | 1 | 18 | 1 | 11 | 1 | 3 |
| PALPA 53 repetition (40) | 0 | 3 | 0 | 0 | 0 | 0 | 0 |
| PALPA 53 oral reading (40) | 0 | 0 | 1 | 0 | 1 | 1 | 0 |
| AUn1 | |||||||
| PNT (175) | 0 | 15 | 7 | 2 | 22 | 16 | 11 |
| PALPA 53 repetition (40) | 0 | 7 | 0 | 0 | 11 | 1 | 0 |
| PALPA 53 oral reading (40) | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| AUn2 | |||||||
| PNT (175) | 3 | 0 | 3 | 2 | 0 | 0 | 27 |
| PALPA 53 repetition (40) | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| PALPA 53 oral reading (40) | 0 | 3 | 0 | 0 | 1 | 0 | 0 |
Note. PNT – Philadelphia Naming Test (Roach et al., 1996); PALPA – Psycholinguistic Assessments of Language Processing in Aphasia (Kay et al., 1992).
The two untreated patients show a somewhat different error profile. AUn1 made a preponderance of nonword, unrelated and formal errors in naming, with mostly nonword and formal errors in repetition and with one formal error in oral word reading. Although we cannot rule out completely the contribution of a lexical semantic deficit (based upon the auditory comprehension performance, mentioned above), this patient’s errors suggest that he has difficulty with phonological output processing, perhaps even with the internal structure of the representations (Kohn, Smith, & Alexander, 1996). However, it is important to note that he can access these representations through the graphemic route. Patient AUn2’s errors in naming consisted overwhelmingly of the ‘other’ category, which entailed mainly descriptions of the pictures or picture parts, in addition to a small number of omissions, semantic and mixed errors. His repetition was flawless and he also performed very well in oral reading, with his few errors constituting mostly formal errors. This patient had the mildest impairments of the four patients. For him, as for the others (albeit to differing degrees), better performance in repetition and/or oral reading suggests that phonological processes could be accessed better through these modalities (Raymer, Thompson, Jacobs, & Legrand, 1993). Despite some of the differences in the error patterns exhibited by all patients, and in the absence of additional data (e.g., nonword repetition, written naming), it appears that all four patients exhibit the greatest difficulty accessing output phonology via lexical semantics.
2.3. Anomia treatment and design
A phonological components analysis (PCA) treatment was employed (Leonard et al., 2008). This treatment is fashioned after the semantic feature analysis approach (Coelho, McHugh, & Boyle, 2000). The PCA treatment consisted of presenting a target picture in the centre of a chart and asking the participant to name it. Subsequently, irrespective of the patient’s ability to name the target he/she was asked to provide or choose (if necessary) five phonological components related to the target (a word that rhymes with it, the first sound, another word that starts with the same first sound, the last sound, and the number of syllables). Once this was complete the patient was asked to name the target again. Then the examiner reviewed all the phonological components and asked the patient to name the target a third time.
A single-subject multiple-baseline across behaviours design (McReynolds & Kearns, 1983) was used. Participants were shown 105 coloured photographs, which constituted the pool of all possible treatment items, and asked to name the items in three consecutive sessions. A list of 30 words was compiled, with input from the patient, based on words that were in error at least 2 of the 3 sessions. The words were divided into three lists of 10 items each. Overlap was minimal between the pool of potential treatment stimuli (i.e., n = 105) and the items in the fMRI tasks (described below): there were three items in common with the fMRI semantic task and six items in common with items on the fMRI phonological task. One of the overlap items was the same for both the semantic and phonological tasks, resulting in a total of eight overlap items. Of these eight possible overlap items from the entire pool of 105 words, the overlap between actual treated items and the items in the fMRI tasks was negligible. For each patient, there was overlap of one treated item with the semantic task and for one of the two patients (ATr2) there was also overlap of one item with the phonological task. For information regarding the theoretical basis of the treatment and complete details regarding the protocol please see Leonard et al. (2008).
2.4. fMRI activation tasks
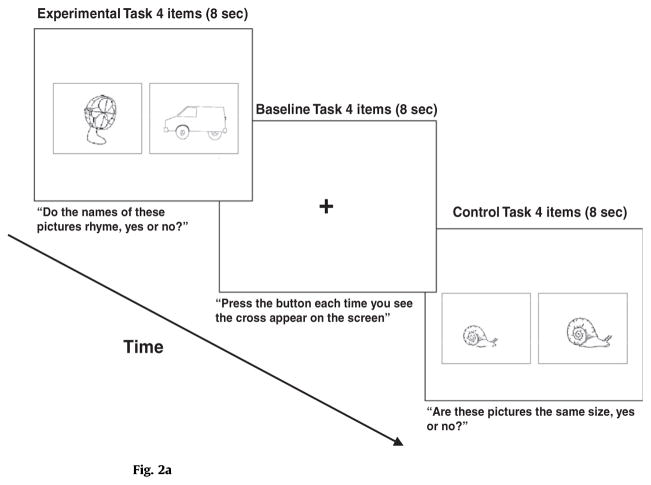
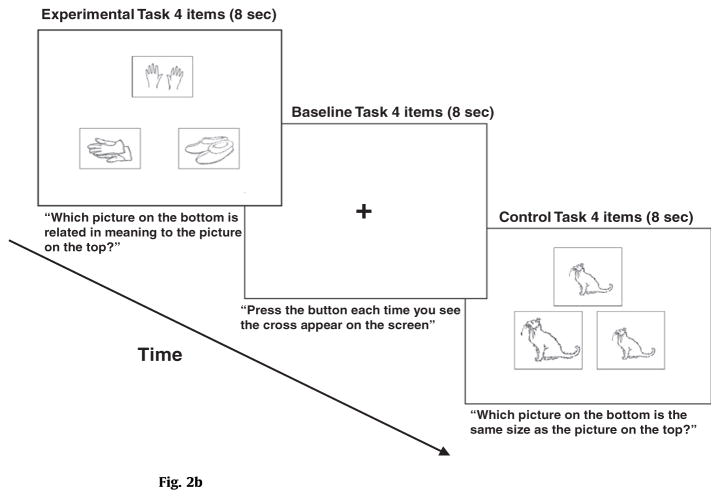
Two experimental tasks and their corresponding control tasks were used. For all four tasks, accuracy and response time were automatically recorded by the computer.
Experimental semantic task. The experimental semantic task consisted of a semantic judgement task using 24 stimuli from the Pyramids and Palm Trees Test (Howard & Patterson, 1992). Participants were presented with three pictures of objects, simultaneously, via a computer. The stimuli were oriented such that one was on top and the other two were below it, side by side. The participant’s task was to determine which of the two bottom images was related in meaning to the one on top. He/she indicated his/her choice (left or right) with a key press.
Semantic control task. The semantic control task consisted of three pictures of the same object that were presented simultaneously via the computer. The stimuli (n = 24) were oriented as above, with one on the top and two on the bottom. Of the bottom two objects, one was the same size as the object on top and one was a different size. The participant’s task was to determine which of the two objects on the bottom was the same size as the one on top. He/she indicated his/her choice (left or right) with a key press.
Experimental phonological task. The phonological experimental task consisted of a rhyme judgement task based on 24 stimuli from the PALPA 14 subtest Rhyme Judgment Requiring Picture Selection (Kay et al., 1992). Participants were presented with pictures of two objects (side by side), simultaneously, via a computer. Their task was to decide if the two words rhymed or not. The participant indicated his/her choice (yes or no) with a key press.
Phonological control task. Participants were presented with pictures (n = 24) of two objects (side by side), simultaneously, via a computer. The pictures were identical except that they differed in terms of size. The participant’s task was to decide if the objects were the same size or not. The participant indicated his/her choice (yes or no) with a key press.
Baseline task. A low-level baseline measure was also taken using a fixation task. A cross was presented in the center of the computer screen and the participant simply pressed a button in order to produce a motor response.
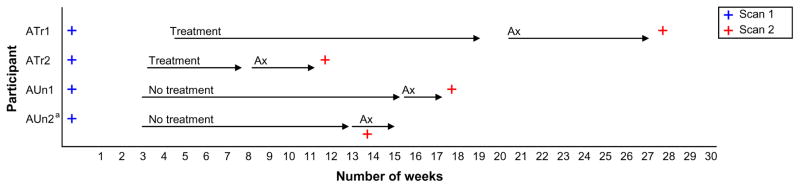
2.5. fMRI protocol
Scanning occurred 4 weeks prior to treatment for ATr1 and 3 weeks prior to treatment for ATr2. Post-treatment scans occurred 8 weeks following treatment for ATr1 (due to scheduling difficulties) and 3 weeks post-treatment for ATr2. This resulted in an interval of 7 months between scans for ATr1 and a 3-month interval for ATr2. It should be noted that in addition to scheduling difficulties, ATr1 was in treatment for 13 weeks, whereas ATr2 was in treatment for 5 weeks. The difference between the total time spent in treatment was due to the fact that ATr2 reached criterion for success more quickly than ATr1 (Leonard et al., 2008). For the untreated aphasic participants, an interval of approximately 4 months separated scans 1 and 2 (see Fig. 1). For individuals in the HC group there was a 3.5 month interval, on average, between scans 1 and 2.
Fig. 1.
Study timeline showing sequence of testing. Note. Ax = Second assessment and follow-up period. See p. 14 for explanation of differences in length of treatment for ATr1 and ATr2. aScan 2 for AUn2 occured before the end of this second assessment due to scheduled scanner maintenance.
Anatomical and functional magnetic resonance scans were obtained using a research dedicated whole-body 3.0 Tesla system (Signa Eclipse, GE Medical Systems, Milwaukee, WI) using the standard quadrature, bird-cage head coil combined with a vacuum pillow (Par Scientific Inc., Odense, Denmark) for head restraint. For each participant, we acquired a T1-weighted volumetric anatomical MRI (124 axial slices, 1.4 mm thick, FOV = 22 cm). Brain activation was assessed using the blood oxygenation level-dependent effect. For functional imaging, 26 5-mm-thick axial slices were obtained utilizing a T2-weighted pulse sequence with spiral in–out readout (TR = 2000 ms, TE = 30 ms, FOV = 20, 64 × 64 matrix).
Visual stimuli were presented to the participant during scanning using fMRI-compatible goggles (Silent Vision Avotec, Inc.) that operate at super-VGA (video graphics array) resolution and have adjustments for interpupillary distance and visual acuity to compensate for elderly participants with visual acuity reductions. Responses were recorded by key presses using an fMRI-compatible device (the Rowland USB Response Box, RURB). Stimulus delivery and recording of psychophysical responses was performed using standard software (EPrime, Psychology Software Tools, Inc.). The software delivered a trigger pulse to the MRI system to start the onset of fMRI data collection and to ensure time synchrony between stimulus delivery and fMRI. The scanner has a built-in communication system so that the examiner could communicate with the participant when necessary.
Prior to the fMRI examination, at both scan times 1 and 2, a 10–15 min training session on an fMRI simulator (Seto et al., 2001) was provided to the participant2. The simulator was used to ensure that the participants were comfortable with the fMRI environment and to ensure that head motion was minimized.
Practice on the behavioural tasks was provided on three occasions – twice while outside the scanner and once in the scanner. Four practice items were presented. These included the experimental stimuli, the control stimuli and the baseline fixation cross. Participants were allowed to practice until they felt comfortable with the task (usually within 1–2 presentations).
For the fMRI data acquisition a block design was employed. For each task, the 24 experimental stimuli were divided into 6 runs. Each run contained 3 blocks (experimental, baseline, control) with 4 trials in each block. Stimuli were presented at a rate of one per 8 s, resulting in blocks of 32 second each and runs of 96 s each. A total of 6 runs was presented, resulting in a total duration of 576 second. The six runs comprising the phonological task were presented together, followed by the six runs for the semantic task (see Figs. 2a and 2b for an example trial of each task). This order was counterbalanced across scan times 1 and 2 and across participants.
Figure 2.
Fig. 2a. Example of an experimental trial for the phonological task.
Fig. 2b. Example of an experimental trial for the semantic task.
2.6. fMRI data analysis
The fMRI images were preprocessed using the Analysis of Functional Neuroimages software (Cox, 1996) and the Statistical Parametric Mapping software (SPM99). The first 20 second of data from each scanning sequence were omitted and then each image in the time series was co-registered to the first to remove the effect of small movements. The images were then spatially normalized to a standard space using a linear transformation and interpolation and detrended to a constant reference scan. Further pre-processing was done using Independent Components Analysis (Kochiyama et al., 2005; Stone, 2002) to improve the signal to noise ratio in the image data.
The image data for patients (both treated and untreated) were analyzed individually; whereas for the healthy controls a group analysis was conducted. For all analyses Partial Least Squares (PLS; McIntosh, Bookstein, Haxby, & Grady, 1996; McIntosh, Chau, & Protzner, 2004) was used. PLS has typically been used with group data, but recently has been adapted for use with single subject data (McIntosh & Lobaugh, 2004). The advantage of PLS is that, as a multivariate technique it is more sensitive to lower signals than univariate analyses. This is important for patient data analysis. PLS identifies a group of brain regions that together covary across the experimental conditions. It is based on the assumption that cognition is the result of the integrated activity of dynamic brain networks rather than the action of any single region acting independently. This method examines the covariance between activity in all brain voxels and the experimental conditions, and provides sets of mutually independent spatial patterns depicting the brain regions that show the strongest relation to (i.e., are covariant with) the contrasts across tasks. PLS analysis produces a set of latent variables (LVs) which reflect cohesive patterns of neural activity associated with task demands (with the LV accounting for the most covariance extracted first). The significance for each LV as a whole was determined by using a permutation test (McIntosh et al., 1996). As 500 permutations were used, the smallest p value obtainable for each LV was p < 0.002. In addition to the permutation test, a second and independent step was to determine the reliability of the saliences for the brain voxels characterizing each pattern identified by the LVs. To do this, all saliences were submitted to a bootstrap estimation of the standard errors (SE, Efron & Tibshirani, 1986). Reliability for each voxel was determined from the ratio of its salience value to the SE for that voxel.
3. Results
3.1. Treatment
A complete presentation of treatment results for ATr1 and ATr2 is available in Leonard et al. (2008). To summarize, both ATr1 and ATr2 demonstrated robust treatment effects. For both patients, mean effect sizes across lists were found to be large, at 3.00 and 3.47, respectively (Busk & Serlin, 1992). Results also indicated that treatment gains were maintained at a follow-up assessment administered 4 weeks after the termination of the treatment protocol for both patients on two of the three treated word lists (see Leonard et al., 2008). Performance of all participants with aphasia was also assessed on the entire pool of possible treatment stimuli (n = 105) before the administration of both scans (i.e., for treated patients this included words that were included in their treatment lists as well as control words that were not treated; control patients were not treated on any word lists). Naming performance on the word list comparing Time 1 (averaged across the three baselines) and Time 2 was compared individually for each participant using the Wilcoxon signed rank test. Results indicated that there was no change in naming performance in the interval between the two scans for either of the two untreated patients (AUn1, p = .67; AUn2, p = .40), whereas there was a significant change for ATr1 (p < .05) and a marginally significant change for ATr2 (p < .07) on these items.
3.2. Behavioural performance in the scanner
3.2.1. Healthy control group
Table 3 shows the reaction time (RT) and accuracy data for healthy control participants and all patient groups on the experimental phonological and semantic tasks. Paired samples t-tests were used to examine the differences in RTs between Scans 1 and 2 on both the phonological and semantic tasks for the healthy controls. Neither of the two comparisons was significant. Accuracy data for controls show that there was no difference in performance between Scan 1 and Scan 2 on either of the two tasks, though the phonological task was more difficult for participants than the semantic task, with a mean percent correct of 76% versus 93% correct, respectively.
Table 3.
Accuracy and reaction time (RT; msec.) data for all participants on the phonological and semantic tasks at scans 1 and 2.
| Phonological experimental task | Semantic experimental task | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| SCAN 1 | SCAN 2 | SCAN 1 | SCAN 2 | |||||
|
|
|
|
|
|||||
| RT | Accuracy | RT | Accuracy | RT | Accuracy | RT | Accuracy | |
| Treated patients | ||||||||
| ATr1 | 3768.00 | 0.50 | 4353.00 | 0.46 | 3308.00 | 0.88 | 3892.00 | 0.91 |
| ATr2 | 3653.00 | 0.67 | 3930.00 | 0.58 | 3928.00 | 0.42 | 4607.00* | 0.50 |
| Mean (SD) | 3710.50 (81.32) | 0.585 (0.12) | 4141.5 (299.11) | 0.52 (0.08) | 3618.00 (438.41) | 0.65 (0.33) | 4249.50 (505.58) | 0.71 (0.29) |
| Untreated patients | ||||||||
| AUn1 | 5367.00 | 0.65 | 5560.00 | 0.65 | 3972.00 | 0.92 | 3672.00 | 1.00 |
| AUn2 | 5203.00 | 0.68 | 5035.00 | 0.63 | 4758.00 | 0.88 | 4865.00 | 0.92 |
| Mean (SD) | 5285.00 (115.97) | 0.665 (0.02) | 5297.5 (371.23) | 0.64 (0.01) | 4365.00 (555.79) | 0.90 (0.03) | 4268.50 (843.58) | 0.96 (0.06) |
| Healthy controls | ||||||||
| Mean (SD) | 3165.15 (546.24) | 0.76 (0.15) | 3337.75 (687.73) | 0.76 (0.11) | 3335.61 (675.37) | 0.93 (0.07) | 3173.32 (957.77) | 0.93 (0.06) |
Note. msec = millisecond;
p < .001.
3.2.2. Participants with aphasia
The McNemar change test was used to assess the difference in accuracy between Scans 1 and 2 on both the phonological and semantic tasks for all four patients. The Wilcoxon test was used to examine the differences in reaction times between Scans 1 and 2 on both the phonological and semantic tasks for all four patients.
3.2.3. Treated patients
Analysis of the accuracy data revealed no significant differences for either ATr1 or ATr2, indicating that patients’ accuracy in responding in both tasks did not differ at Scan 1 and Scan 2. With respect to the reaction time analysis only one comparison was significant, that for ATr2 [Z = −3.29, p < .001] on the semantic task, however this difference was in the opposite direction to what would have been expected, with RTs being slower at Scan 2 than at Scan 1.
3.2.4. Untreated patients
As for the treated patients, analysis of the accuracy data revealed no significant differences for either patient. Regarding the analysis of the reaction time data, no comparisons were significant.
3.3. fMRI Results
Participants’ performance on the phonological and semantic tasks was of primary interest in this study. As a result, only analyses comparing these conditions will be presented in this paper. As mentioned, the PLS approach used for the fMRI analyses in the present study identifies patterns of activity across the brain that covary with aspects of the experimental tasks (McIntosh et al., 1996). As such, the approach does not specify the task contrasts; instead it reveals the contrasts that account for the most covariance between the tasks and the brain activity. As mentioned, the algorithm extracts a set of latent variables (LVs) explaining the covariance between conditions and brain activity in order of the amount of covariance explained (with the LV accounting for the most covariance extracted first). As such, the LVs reflect cohesive patterns of neural activity associated with task demands. PLS analyses were carried out on the imaging data from the normal control group and then separately for the individual patients, both treated and control.
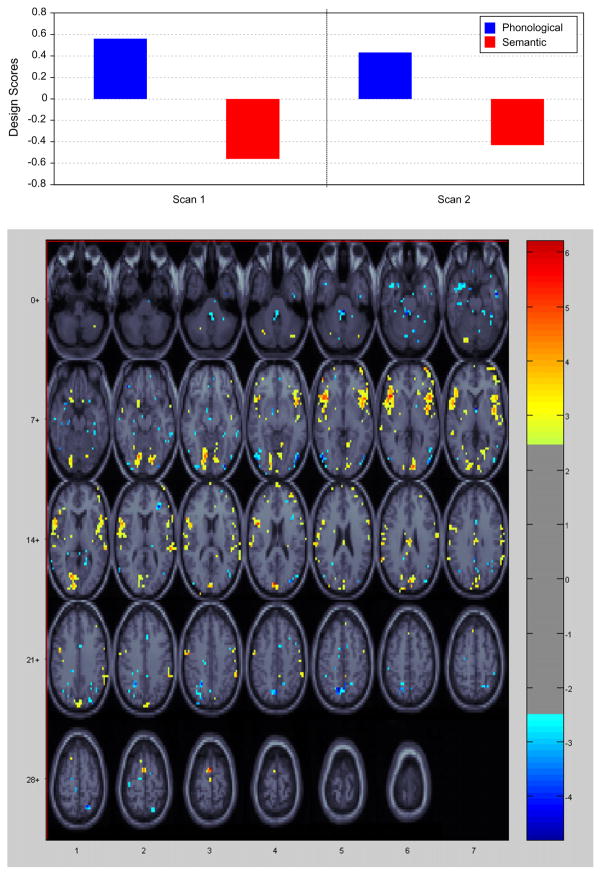
3.3.1. Healthy control group
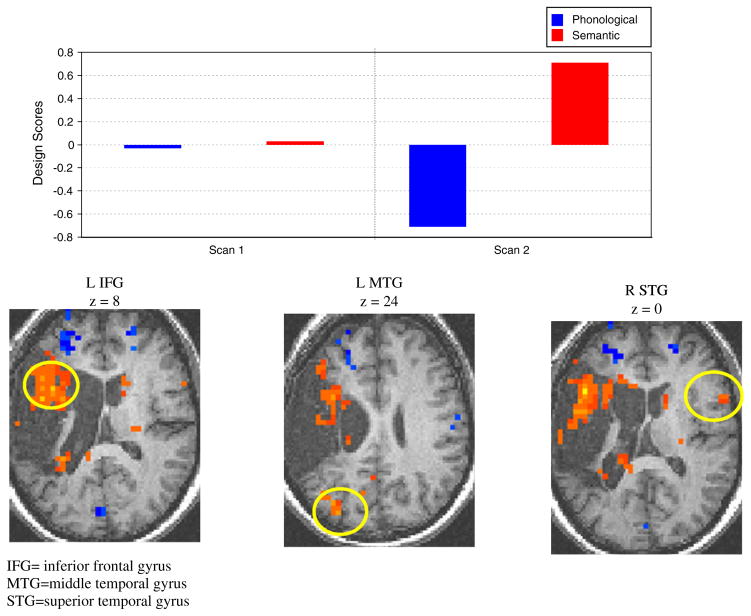
PLS analysis performed on the phonological and semantic tasks revealed a latent variable (LV1) that accounted for 58% of the variance (p < .02), which distinguished the two tasks from each other at both Scan 1 and Scan 2. Fig. 3 shows the design scores and areas of activation for this analysis and Table 4 shows the significant areas of cortical activation for both tasks.
Fig. 3.
Healthy control subject activation during the phonological and semantic tasks. Activations denoted in yellow/red represent brain regions that positively correlate with the phonological task and negatively with the semantic task. Activations denoted in blue represent brain regions that positively correlate with the semantic task and negatively with the phonological task. The images show the active areas on a standard MRI scan in which the right side of the brain is shown on the right side of the image.
Table 4.
Activations for healthy controls on the semantic and phonological tasks.
| Task (hemisphere) | Region | BA | MNI Coordinates | Ratio | ||
|---|---|---|---|---|---|---|
|
| ||||||
| X (mm) | Y (mm) | Z (mm) | ||||
| Phonological | ||||||
| (left hemisphere) | Inferior frontal gyrus – temporal pole | 47 | −48 | 20 | −4 | 5.66 |
| Superior temporal gyrus – temporal pole | 38 | |||||
| Superior temporal gyrus | 22,42 | −64 | −28 | 16 | 4.23 | |
| Middle occipital gyrus | 18,19 | −8 | −88 | 16 | 6.03 | |
| Inferior frontal gyrus | 44,45 | −48 | 8 | 16 | 5.75 | |
| (right hemisphere) | Inferior frontal gyrus – temporal pole | 47 | 52 | 16 | −8 | 5.10 |
| Superior temporal gyrus – temporal pole | 38 | |||||
| Lingual gyrus | 17,18 | 8 | −92 | −4 | 5.00 | |
| Superior temporal gyrus | 22,42 | 60 | −32 | 8 | 4.86 | |
| Inferior parietal lobule | 40 | 60 | −40 | 40 | 4.23 | |
| Cuneus | 18 | 0 | −84 | 24 | 5.09 | |
| Semantic | ||||||
| (left hemisphere) | Inferior occipital gyrus | 18,19 | −52 | −80 | −8 | −4.29 |
| Precuneus | 7 | −12 | −68 | 48 | −4.80 | |
| (right hemisphere) | Inferior occipital gyrus | 18,19 | 48 | −80 | −12 | −4.07 |
| Middle frontal gyrus | 10 | 32 | 36 | 8 | −4.35 | |
Note. BA = Brodmann Area; MNI = Montreal Neurological Institute. All regions are reliable at p < 0.005. Positive ratios correspond to regions with positive salience on the LV.
Negative ratios correspond to regions with negative salience on the LVs. X (right/left): Negative values are in the left hemisphere; Y (anterior/posterior): negative values are posterior to the zero point (located at the anterior commissure); Z (superior/inferior): negative values are inferior to the plane defined by the anterior and posterior commissures. Ratio, salience/S.E. ratio from the bootstrap analysis, which is a measure of each voxel’s reliability.
3.3.2. Participants with aphasia
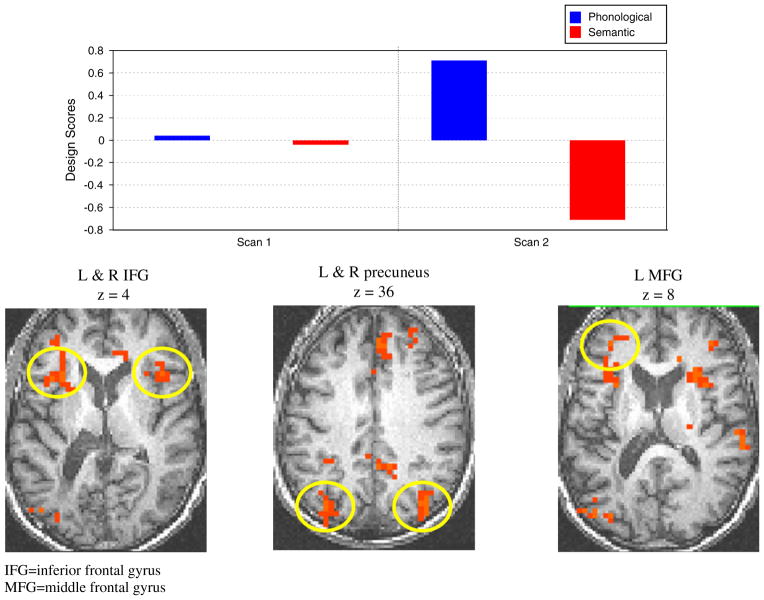
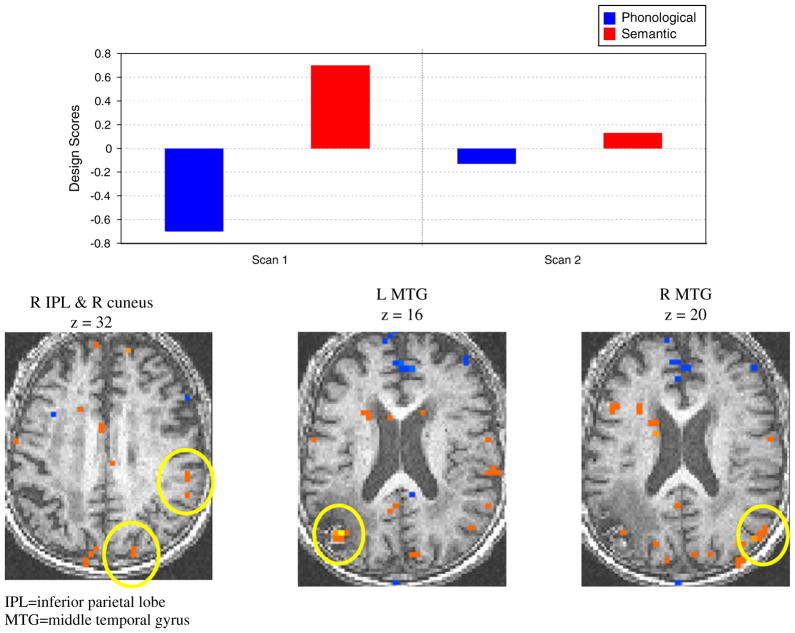
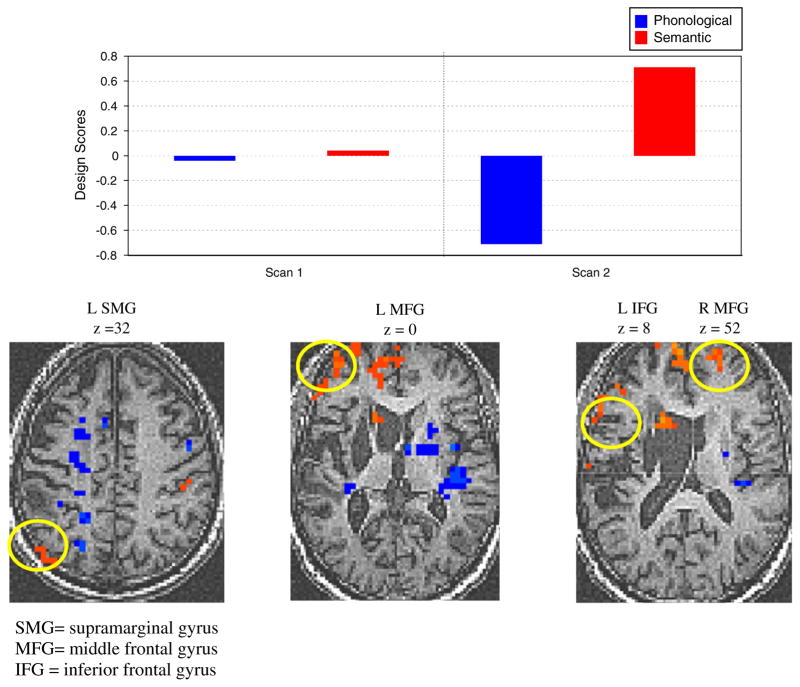
For all patients, when PLS analysis was performed on the phonological and semantic tasks, one significant LV emerged, distinguishing the semantic from the phonological tasks (p < .01) and accounting for 56–74% of the variance. Figs. 4–7 show the design scores for each patient for this analysis with representative cortical activity maps. Table 5 shows the significant areas of cortical activation on the semantic task.
Fig. 4.
Results of the analysis comparing activations in the phonological and semantic tasks for scans 1 and 2 for ATr1 with representative areas of activation on the semantic task.
Fig. 7.
Results of the analysis comparing activations in the phonological and semantic tasks for scans 1 and 2 for AUn2 with representative areas of activation on the semantic task.
Table 5.
Activations for patients with aphasia on the semantic task.
| Participant (hemisphere) | Region | BA | MNI Coordinates | Ratio | ||
|---|---|---|---|---|---|---|
|
| ||||||
| X (mm) | Y (mm) | Z (mm) | ||||
| ATr1 | ||||||
| (left hemisphere) | Inferior frontal gyrus | 45 | −48 | 20 | 8 | 24.23 |
| Middle temporal gyrus | 39 | −36 | −76 | 24 | 11.44 | |
| Superior frontal gyrus | 6 | −8 | −12 | 64 | 8.73 | |
| Cuneus | 19 | −8 | −76 | 36 | 7.51 | |
| Cerebellum | −12 | −48 | −16 | 5.08 | ||
| Cingulate gyrus | 31 | |||||
| (right hemisphere) | Precuneus | 7 | 12 | −64 | 52 | 9.01 |
| Superior temporal gyrus | 22 | 56 | 8 | 0 | 8.24 | |
| Precuneus | 23 | 4 | −60 | 20 | 4.94 | |
| ATr2 | ||||||
| (left hemisphere) | Caudate nucleus | −16 | 20 | 8 | 11.78 | |
| Superior frontal gyrus | 10 | −8 | 72 | 8 | 10.93 | |
| Inferior temporal gyrus | 20 | −52 | −12 | −32 | 8.74 | |
| Inferior frontal gyrus | 46 | −56 | 36 | 8 | 8.01 | |
| Precentral gyrus | 6 | −64 | 4 | 16 | 7.63 | |
| Supra-marginal gyrus | 39 | −60 | −68 | 32 | 7.13 | |
| Inferior parietal lobule | 40 | −48 | −40 | 56 | 7.00 | |
| Middle frontal gyrus | 10 | −44 | 60 | 0 | 6.60 | |
| Superior temporal gyrus | 38 | −36 | 20 | −28 | 6.08 | |
| (right hemisphere) | Inferior parietal lobule | 40 | 44 | −40 | 56 | 9.67 |
| Middle frontal gyrus | 10 | 24 | 64 | 8 | 8.60 | |
| Precentral gyrus | 4 | 64 | −8 | 28 | 5.06 | |
| Middle frontal gyrus | 6 | 24 | 20 | 52 | 5.05 | |
| AUn1 | ||||||
| (left hemisphere) | Middle temporal gyrus | 39 | −44 | −72 | 16 | 14.53 |
| Thalamus | −4 | −16 | 4 | 7.02 | ||
| (right hemisphere) | Superior temporal gyrus | 22 | 64 | −4 | 0 | 9.06 |
| Cingulate gyrus | 31 | 4 | −44 | 40 | 8.31 | |
| Middle temporal gyrus | 19 | 52 | −76 | 20 | 6.04 | |
| Middle temporal gyrus | 39 | 44 | −72 | 12 | 5.27 | |
| Inferior parietal lobule | 40 | 60 | −32 | 32 | 5.05 | |
| Inferior temporal gyrus | 20 | 52 | −28 | −20 | 4.30 | |
| Cuneus | 19 | 20 | −88 | 32 | 4.19 | |
| Anterior cingulate gyrus | 25 | 0 | 12 | −8 | 4.00 | |
| AUn2 | ||||||
| (left hemisphere) | Inferior frontal gyrus | 45 | −40 | 20 | 4 | −11.10 |
| Precuneus | 31 | −12 | −44 | 32 | −8.94 | |
| Middle frontal gyrus | 10 | −36 | 48 | 8 | −8.07 | |
| Angular gyrus | 39 | −36 | −76 | 32 | −8.03 | |
| Middle occipital gyrus | 19 | −48 | −84 | 8 | −7.49 | |
| Middle frontal gyrus | 10 | −36 | 48 | 8 | −8.07 | |
| Superior frontal gyrus | 10 | −24 | 68 | 12 | −6.55 | |
| (right hemisphere) | Precuneus | 19 | 36 | −84 | 40 | −13.00 |
| Precentral gyrus | 6 | 48 | −8 | 56 | −12.07 | |
| Medial frontal gyrus | 8 | 4 | 40 | 40 | −12.00 | |
| Superior frontal gyrus | 8 | 28 | 44 | 40 | −10.51 | |
| Thalamus | 20 | −12 | 16 | −9.72 | ||
| Anterior cingulate gyrus | 32 | 16 | 28 | 24 | −8.05 | |
| Inferior frontal gyrus | 45 | 44 | 24 | 4 | −7.85 | |
| Middle frontal gyrus | 9 | 40 | 44 | 28 | −6.18 | |
| Middle frontal gyrus | 10 | 28 | 48 | −4 | −5.83 | |
| Cingulate gyrus | 31 | 0 | −60 | 24 | −5.96 | |
Note. BA = Brodmann Area; MNI = Montreal Neurological Institute. All regions are reliable at p < 0.005. Positive ratios correspond to regions with positive salience on the LV.
Negative ratios correspond to regions with negative salience on the LVs. X (right/left): negative values are in the left hemisphere; Y (anterior/posterior): negative values are posterior to the zero point (located at the anterior commissure); Z (superior/inferior): negative values are inferior to the plane defined by the anterior and posterior commissures. Ratio, salience/S.E. ratio from the bootstrap analysis, which is a measure of each voxel’s reliability.
As can be seen in Figs. 4–7 and Table 5, significant areas of activation in the semantic task at Scan 2 for ATr1 (Fig. 4) included expected cortical areas such as inferior frontal gyrus (IFG) and the middle temporal gyrus of the left hemisphere (LH). The left cuneus and right precuneus were also activated in this task. For ATr2 areas of activation included frontal (IFG and others) temporal and parietal (i.e., supra-marginal gyrus) regions in the LH as well as the inferior parietal lobe bilaterally. Note that for both these treated patients, there are a greater number of significant activations in the LH than the RH and that these emerged at the second scan. Untreated patient AUn2 (Fig. 7) also demonstrated significant activation changes at Scan 2 and these changes also occurred on the semantic task. Areas of activation included bilateral frontal and occipital regions. Interestingly, unlike the treated patients, AUn2 had an equivalent number of LH and RH areas activated at Scan 2. AUn1 (Fig. 6), on the other hand, showed differences in cortical activation between the two tasks, which was greater at Scan 1, including bilateral temporal regions and the right inferior parietal lobe, and the right cuneus. This control patient showed more RH than LH areas of activation. Note that we have highlighted representative areas of activation for the semantic task since this is where the changes were evident at Scan 2 for ATr1, ATr2 and AUn2. Areas of activation on the phonological task are shown in Appendix A.
Fig. 6.
Results of the analysis comparing activations in the phonological and semantic tasks for scans 1 and 2 for AUn1 with representative areas of activation on the semantic task.
Appendix A.
Activations for patients with aphasia on the phonological task.
| Participant (hemisphere) | Region | BA | MNI Coordinates | Ratio | ||
|---|---|---|---|---|---|---|
|
| ||||||
| X (mm) | Y (mm) | Z (mm) | ||||
| ATr1 | ||||||
| (left hemisphere) | Cerebellum | −44 | −76 | −24 | −13.82 | |
| Middle frontal gyrus | 10 | −28 | 60 | 20 | −12.31 | |
| Supramarginal gyrus | 40 | −64 | −48 | 40 | −8.08 | |
| Inferior temporal gyrus | 20 | −56 | −20 | −20 | −7.59 | |
| (right hemisphere) | Middle frontal gyrus | 10 | 24 | 44 | 12 | −10.59 |
| Cerebellum | 44 | −48 | −32 | −8.86 | ||
| Middle frontal gyrus | 11 | 28 | 36 | −12 | −6.52 | |
| Lingual gyrus | 18 | 12 | −96 | −4 | −5.71 | |
| ATr2 | ||||||
| (left hemisphere) | Middle temporal gyrus | 21 | −48 | 4 | −24 | −26.68 |
| Uncus (hipp.gyrus) | −20 | 0 | −28 | −17.87 | ||
| Precentral gyrus | 6 | −44 | −4 | 20 | −9.13 | |
| Superior temporal gyrus | 42 | −52 | −28 | 12 | −7.59 | |
| Inferior temporal gyrus | 20 | −48 | −20 | −16 | −7.53 | |
| Precuneus | 7 | −24 | −72 | 40 | −7.26 | |
| Superior frontal gyrus | 11 | −24 | 56 | −20 | −6.93 | |
| Cingulate gyrus | 32 | −8 | 16 | 40 | −6.11 | |
| Inferior parietal lobule | 40 | −56 | −32 | 48 | −5.94 | |
| (right hemisphere) | Lentiform nucleus (BG) | 16 | 0 | −4 | −12.57 | |
| Insula | 13 | 40 | 0 | 0 | −11.97 | |
| Uncus (hipp.gyrus) | 20 | 0 | −28 | −8.35 | ||
| AUn1 | ||||||
| (left hemisphere) | Middle frontal gyrus | 11 | −44 | 36 | −12 | −7.74 |
| Precuneus | 19 | −28 | −68 | 44 | −7.69 | |
| Middle frontal gyrus | 10 | −28 | 44 | 24 | −6.07 | |
| Superior temporal gyrus | 38 | −56 | 16 | −8 | −3.98 | |
| (right hemisphere) | Precuneus | 7 | 24 | −72 | 56 | −4.31 |
| Medial frontal gyrus | 9 | 0 | 52 | 16 | −7.11 | |
| AUn2 | No signicant activations on phonological task | |||||
Note. BA = Brodmann Area; MNI = Montreal Neurological Institute. All regions are reliable at p < 0.005. Positive ratios correspond to regions with positive salience on the LV.
Negative ratios correspond to regions with negative salience on the LVs. X (right/left): negative values are in the left hemisphere; Y (anterior/posterior): negative values are posterior to the zero point (located at the anterior commissure); Z (superior/inferior): negative values are inferior to the plane defined by the anterior and posterior commissures. Ratio, salience/S.E. ratio from the bootstrap analysis, which is a measure of each voxel’s reliability.
4. Discussion
The purpose of this research was to examine changes in cortical activity associated with a phonologically-based naming treatment (Leonard et al., 2008) in two patients with aphasia whose naming improved after the treatment. In addition, we sought to compare the changes in the treated patients to cortical activations across time in two patients with aphasia who had not received treatment and in a group of healthy, older controls. In an attempt to isolate phonological and semantic processing, the fMRI tasks did not entail overt naming, but rather a phonological and semantic judgment task, respectively. The results showed performance of the healthy control participants was stable across time. Results also showed that after treatment changes in patterns of cortical activation in the treated patients were especially evident in the semantic task. Performance of the two untreated patients with aphasia was less stable, but each showed their own unique pattern of performance, which was different from the treated patients’. Several issues related to these findings will be discussed in turn below, beginning with the performance of the healthy control participants.
As expected, administration of the two experimental tasks in the older healthy control group produced stable patterns of activation across the three and a half-month interval separating the scans, establishing the reproducibility of the fMRI results using our experimental tasks. Acknowledging the instability of performance associated with processing in a damaged brain, nonetheless the reproducibility of the results found in the healthy participants suggests that changes found in the patient scans after treatment are most likely not simply attributable to effects of time or test–retest.
When areas of activation were compared for the phonological and semantic judgment tasks in the healthy control group (i.e., as shown in Fig. 3 and Table 4), both tasks were found to activate bilateral regions, with the phonological task activating expected areas such as inferior frontal and inferior parietal areas. Although the semantic task was expected to activate temporal areas, in comparison to the phonological task, these areas were more activated in the phonological than the semantic task, leaving significant activations mostly in occipital areas in this latter task in the healthy controls. These occipital areas have been associated with the low level perceptual processing necessary for object naming and semantic judgments (Murtha et al., 1999), however it is surprising that temporal regions, usually associated with processing semantic representations, were differentially activated in the phonological but not the semantic task. Another possibility that cannot be ruled out is that the items in the phonological task may have stimulated semantic processing since pictures of objects were used.3 It must be noted that the behavioral data show that the phonological task was more difficult (for participants in all groups) than the semantic task. Unfortunately, this means that the two tasks were not equated for difficulty. As a result, it is possible that when the two were compared to each other, most of the variance associated with performance was absorbed by the phonological task.
Areas of activation for ATr1 and ATr2 were consistent with areas that have been identified in other studies following treatment for anomia in aphasia. These include frontal and temporal regions in particular, as well as the supra-marginal gyrus and inferior parietal regions. In addition, areas not traditionally thought of as related to semantic or phonological processing, but that have been identified in other studies, such as the precuneus (Fridrikson et al., 2006) and the anterior cingulate gyrus (Fridriksson et al., 2007) were also found to be activated in this study. Regarding the question of hemispheric involvement, our findings are in keeping with other studies (Cornelissen et al., 2003; Meinzer et al., 2004; Meinzer et al., 2007; Meinzer et al., 2008) that have found greater left than right hemisphere processing after treatment. This was evident when comparing significant activations for the treated patients to both of the control patients. After treatment in which naming performance was improved, there were more significant areas of activation in the fMRI semantic task for both treated patients in the left hemisphere than the right. Although there were also changes in the fMRI semantic task for untreated patient AUn2 at Scan 2, this patient’ s naming performance did not change in the interval between the two scans and he had a nearly equivalent number of left and right hemisphere areas activated. Untreated patient AUn1, whose naming performance did not change at Scan 2 had more right than left hemisphere areas activated (the same pattern is evident on the fMRI phonological task across patients, see Appendix). Together, these findings suggest that behavioral improvement must be accompanied by greater left than right hemisphere processing. Also consistent with previous findings (e.g., Fridriksson et al., 2006; Léger et al., 2002; Meinzer et al., 2008), improved naming at Scan 2 was associated with greater perilesional activity. This was more evident for ATr1 than ATr2, who additionally showed activation in the lesioned area.
It must also be mentioned that there was a disparity for the treated patients between performance on the naming tasks used in treatment and the experimental semantic and phonological tasks used in the fMRI protocol (which did not involve naming). Specifically, the naming performance of the treated patients improved on items trained in therapy after treatment; however, patients’ performance did not change significantly on either the phonological or semantic fMRI tasks at Scan 2. Stability would have been expected of the untreated patients, but we might have expected the treated patients’ performance to have improved in a manner similar to their improvement on the treatment stimuli. Generalization has often been difficult to demonstrate in aphasia treatment studies. The two fMRI tasks were chosen to reflect two of the purported underlying components of picture naming; however, it may be that both the nature of the stimuli and the tasks were too different from the treatment task to obtain generalized improvement in the treated patients.
In addition, while it is true that changes in brain activations were obtained in the absence of behavioral changes on the fMRI tasks, similar findings have been found in aging studies where, while no differences are found behaviorally between younger and older adults, differences in activation patterns have been identified (Grady, McIntosh, & Craik, 2003; McIntosh et al., 1999). With respect to the patients, it might be that their performance may be attributed to strategy use.
We are left to speculate about what effect our phonologically-based treatment was exerting in the fMRI semantic task in the treated patients. The activation of ‘phonological’ areas in the semantic task, such as the left supra-marginal gyrus in ATr2, suggests that the treated patients may have been attempting to apply phonology (e.g., pronouncing the word subvocally) to the drawings they were viewing and making judgments about. Based upon the characterization of the patients’ deficits, which situated their difficulties in naming in the connections between lexical and phonological processing, this view is consistent with the possibility that treatment strengthened the connections between the two levels in order for naming performance to be improved. This view is also consistent with the possibility that although our treatment focused on the phonological aspects of words to be named, semantic processing and representations were also activated since (a) we used pictures to represent the stimuli and (b) the (correct) production of a word requires the activation of both semantics and phonology.
Before concluding, some limitations of the current study should be noted. First, while patient numbers are comparable to many in the literature it will be important to replicate these findings with a larger sample size. Secondly, since the fMRI tasks chosen were unfortunately not equated on difficulty, this may have had a bearing on the results. In addition, although we chose the tasks to presumably isolate semantic and phonological processing, it is acknowledged that both tasks potentially recruit both types of processing. In future studies we will use an overt naming task. It will also be important in future studies to control for type of aphasia and lesion site to better delineate the neural underpinnings of our PCA treatment.
In conclusion, this investigation was important for its potential to inform our PCA treatment for anomia and to contribute to the understanding of neural reorganization as a function of therapy. Unlike most studies in the literature, ours included both a healthy control group and untreated patients as controls, which strengthened the findings. We will continue to build upon these findings in future studies.
Fig. 5.
Results of the analysis comparing activations in the phonological and semantic tasks for scans 1 and 2 for ATr2 with representative areas of activation on the semantic task.
Acknowledgments
This research was supported by the Heart and Stroke Foundation of Canada (Grant #s 5379 and 6092). The authors also acknowledge the support of Toronto Rehabilitation Institute, which receives funding under the Provincial Rehabilitation Research Program from the Ministry of Health and Long-Term Care in Ontario. We thank the MRI technologists and Caron Murray at Sunnybrook Health Sciences Centre for assistance with this experiment. Lauren Reznick provided valuable assistance on this project. We especially thank the participants for their patience and perseverance, and we thank the referring clinicians at the Aphasia Institute and the York-Durham Aphasia Centre. Portions of this work were presented at the Organization for Human Brain Mapping meeting in Florence, 2006; the Academy of Aphasia meeting in Victoria, 2006; the Rotman Research Conference meeting in Toronto, 2006; and the 1st Canadian Stroke Congress in Quebec, 2010.
Footnotes
In Leonard et al. (2008) P5 and P6 correspond, respectively, to ATr1 and ATr2 of the present article.
Due to technical difficulties 3 individuals from the HC group did not participate in this training session.
We thank an anonymous reviewer for pointing this out.
References
- Baxter LC, Syakin AJ, Flashman LA, Johnson SC, Guerin SJ, Babcock DR, et al. Sex differences in semantic language processing: A functional MRI study. Brain and Language. 2003;84:264–272. doi: 10.1016/s0093-934x(02)00549-7. [DOI] [PubMed] [Google Scholar]
- Belin P, Van Eeckhout P, Zilbovicius M, Remy P, François C, Guillaum S, et al. Recovery from nonfluent aphasia after melodic intonation therapy: A PET study. Neurology. 1996;47:1504–1511. doi: 10.1212/wnl.47.6.1504. [DOI] [PubMed] [Google Scholar]
- Binder JR, Frost J, Hammeke T, Cox R, Rao S, Prieto T. Human brain language areas identified by functional magnetic resonance imaging. Journal of Neuroscience. 1997;17:353–362. doi: 10.1523/JNEUROSCI.17-01-00353.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breier JI, Maher LM, Schmadeke S, Hasan KM, Papanicolaou AC. Changes in language-specific brain activation after therapy for aphasia using magnetoencephalography: A case study. Neurocase. 2007;13(3):169–177. doi: 10.1080/13554790701448200. [DOI] [PubMed] [Google Scholar]
- Busk PL, Serlin R. Meta-analysis for single case research. In: Kratochwill TR, Levin JR, editors. Single-case research design and analysis: New directions for psychology and education. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992. [Google Scholar]
- Calvert GA, Brammer MJ, Morris RG, Williams SR, King N, Matthews PM. Using fMRI to study recovery from acquired dysphasia. Brain and Language. 2000;71:391–399. doi: 10.1006/brln.1999.2272. [DOI] [PubMed] [Google Scholar]
- Carel C, Loubinoux I, Boulanuar K, Manelfe C, Rascol O, Celsis P, et al. Neural substrate for the effects of passive training on sensory motor cortical representation: A study with functional magnetic resonance imaging in healthy subjects. Journal of Cerebral Blood Flow and Metabolism. 2000;20:478–484. doi: 10.1097/00004647-200003000-00006. [DOI] [PubMed] [Google Scholar]
- Cherney LR, Small SL. Task-dependent changes in brain activation following therapy for nonfluent aphasia: Discussion of two individual cases. Journal of the International Neuropsychological Society. 2006;12(6):828–842. doi: 10.1017/S1355617706061017. [DOI] [PubMed] [Google Scholar]
- Coelho CA, McHugh RE, Boyle M. Semantic feature analysis as a treatment for aphasic dysnomia: A replication. Aphasiology. 2000;14(2):133–142. [Google Scholar]
- Cornelissen K, Laine M, Tarkiainen A, Jarvensivu T, Martin N, Salmelin R. Adult brain plasticity elicited by anomia treatment. Journal of Cognitive Neuroscience. 2003;15(3):444–461. doi: 10.1162/089892903321593153. [DOI] [PubMed] [Google Scholar]
- Cox RW. AFNI: Software for analysis and visualization of functional magnetic resonance neuroimages. Computers and Biomedical Research. 1996;29:162–173. doi: 10.1006/cbmr.1996.0014. [DOI] [PubMed] [Google Scholar]
- Crosson B, McGregor K, Gopinath KS, Conway TW, Benjamin M, Chang Y, et al. Functional MRI of language in aphasia: A review of the literature and the methodological challenges. Neuropsychology Review. 2007;17(2):157–177. doi: 10.1007/s11065-007-9024-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crosson B, Moore AB, Gopinath K, White KD, Wierenga CE, Gaiefsky ME, et al. Role of the right and left hemispheres in recovery of function during treatment of intention in aphasia. Journal of Cognitive Neuroscience. 2005;17(3):392–406. doi: 10.1162/0898929053279487. [DOI] [PubMed] [Google Scholar]
- Davis CH, Harrington G, Baynes K. Intensive semantic intervention in fluent aphasia: A pilot study with fMRI. Aphasiology. 2006;20(1):59–83. [Google Scholar]
- Dell GS, Lawler EN, Harris HD, Gordon JK. Models of errors of omission in aphasic naming. Cognitive Neuropsychology. 2004;21(2):125–145. doi: 10.1080/02643290342000320. [DOI] [PubMed] [Google Scholar]
- Efron B, Tibshirani R. Bootstrap methods for standard errors, confidence intervals and other measures of statistical accuracy. Statistical Science. 1986;1:54–77. [Google Scholar]
- Farias D, Davis C, Harrington G. Drawing: Its contribution to naming in aphasia. Brain and Language. 2006;97(1):53–63. doi: 10.1016/j.bandl.2005.07.074. [DOI] [PubMed] [Google Scholar]
- Fernandez B, Cardebat D, Démonet JF, Joseph P, Mazaux JM, Barat M, et al. Functional MRI follow-up study of language processes in healthy subjects and during recovery in a case of aphasia. Stroke. 2004;35:2171–2176. doi: 10.1161/01.STR.0000139323.76769.b0. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Foygel D, Dell GS. Models of impaired lexical access in speech production. Journal of Memory and Language. 2000;43(2):182–216. [Google Scholar]
- Fridriksson J, Morrow-Odom L, Moser D, Fridriksson A, Baylis G. Neural recruitment associated with anomia treatment in aphasia. NeuroImage. 2006;32(3):1403–1412. doi: 10.1016/j.neuroimage.2006.04.194. [DOI] [PubMed] [Google Scholar]
- Fridriksson J, Moser D, Bonilha L, Morrow-Odom KL, Shaw H, Fridriksson A, et al. Neural correlates of phonological and semantic-based anomia treatment in aphasia. Neuropsychologia. 2007;45(8):1812–1822. doi: 10.1016/j.neuropsychologia.2006.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodglass H, Kaplan E, Barresi B. Boston diagnostic aphasia examination (BDAE) Baltimore, MD: Lippincott Williams & Wilkins; 2001. [Google Scholar]
- Grady CL, McIntosh AR, Craik FIM. Age-related differences in the functional connectivity of the hippocampus during memory encoding. Hippocampus. 2003;13:572–586. doi: 10.1002/hipo.10114. [DOI] [PubMed] [Google Scholar]
- Heiss WD, Kessler J, Thiel A, Ghaemi M, Karbe H. Differential capacity of left and right hemispheric areas of compensation of poststroke aphasia. Annals of Neurology. 1999;45:430–438. doi: 10.1002/1531-8249(199904)45:4<430::aid-ana3>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Howard D, Patterson K. The pyramids and palm trees test. Suffolk, U.K: Thames Valley Test Company; 1992. [Google Scholar]
- Jodzio K, Drumm DA, Nyka WM, Lass P, Gasecki D. The contribution of the left and right hemispheres in early recovery from aphasia: A SPECT prospective study. Neuropsychological Rehabilitation. 2005;15(5):588–604. doi: 10.1080/09602010443000137. [DOI] [PubMed] [Google Scholar]
- Kareken DA, Lowe M, Chen SH, Lurito J, Mathews V. Word rhyming as a probe of hemisphereic language dominance with functional magnetic resonance imaging. Neurophsychiatry, Neuropsychology, Behavioural Neurology. 2000;13:264–270. [PubMed] [Google Scholar]
- Kay J, Lesser R, Coltheart M. Psycholinguistic assessments of language processing in aphasia (PALPA) East Sussex, UK: Erlbaum; 1992. [Google Scholar]
- Kochiyama T, Morita T, Okada T, Yonekura Y, Matsumara M, Sadato N. Removing the effects of task-related motion using independent-component analysis. Neuroimage. 2005;25(3):802–814. doi: 10.1016/j.neuroimage.2004.12.027. [DOI] [PubMed] [Google Scholar]
- Kohn SE, Smith KL, Alexander MP. Differential recovery from impairments to the phonological lexicon. Brain and Language. 1996;52:129–149. doi: 10.1006/brln.1996.0007. [DOI] [PubMed] [Google Scholar]
- Laine M, Martin N. Anomia: Theoretical and clinical aspects. New York, NY: Psychology Press; 2006. [Google Scholar]
- Léger A, Démonet JF, Ruff S, Aithamon B, Touyeras B, Puel M, et al. Neural substrates of spoken language rehabilitation in an aphasic patient: an fMRI study. NeuroImage. 2002;17:174–183. doi: 10.1006/nimg.2002.1238. [DOI] [PubMed] [Google Scholar]
- Leonard C, Rochon E, Laird L. Treating naming impairments in aphasia: Findings from a phonological components analysis treatment. Aphasiology. 2008;22(9):923–947. [Google Scholar]
- Lurito JT, Kareken DA, Lowe MJ, Chen SH, Mathews VP. Comparison of rhyming and word generation with FMRI. Human Brain Mapping. 2000;10:99–106. doi: 10.1002/1097-0193(200007)10:3<99::AID-HBM10>3.0.CO;2-Q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin N, Fink RB, Renvall K, Laine M. Effectiveness of contextual repetition priming treatments for anomia depends on intact access to semantics. Journal of the International Neuropsychological Society. 2006;12(6):853–866. doi: 10.1017/S1355617706061030. [DOI] [PubMed] [Google Scholar]
- McDermott KB, Petersen SE, Watson JM, Ojemann JG. A procedure for identifying regions preferentially activated by attention to semantic and phonological relations using functional magnetic resonance imaging. Neuropsychologia. 2003;41:293–303. doi: 10.1016/s0028-3932(02)00162-8. [DOI] [PubMed] [Google Scholar]
- McIntosh AR, Lobaugh NJ. Partial least squares analysis of neuroimaging data: Applications ans advances. NeuroImage. 2004;23(Supplement 1):S250–S263. doi: 10.1016/j.neuroimage.2004.07.020. [DOI] [PubMed] [Google Scholar]
- McIntosh AR, Bookstein FL, Haxby JV, Grady CL. Spatial pattern analysis of functional brain images using partial least squares. NeuroImage. 1996;3(3):143–157. doi: 10.1006/nimg.1996.0016. [DOI] [PubMed] [Google Scholar]
- McIntosh AR, Chau WK, Protzner AB. Spatiotemporal analysis of event-related fMRI data using partial least squares. Neuroimage. 2004;23(2):764–775. doi: 10.1016/j.neuroimage.2004.05.018. [DOI] [PubMed] [Google Scholar]
- McIntosh AR, Sekuler AB, Penpeci C, Rajah MN, Grady CL, Sekuler R, et al. Recruitment of unique neural systems to support visual memory in normal aging. Current Biology. 1999;9:1275–1278. doi: 10.1016/s0960-9822(99)80512-0. [DOI] [PubMed] [Google Scholar]
- McReynolds LV, Kearns KP. Single-subject experimental design in communicative disorders. Baltimore, MD: University Park Press; 1983. [Google Scholar]
- Meinzer M, Flaisch T, Obleser J, Assadollahi R, Djundja D, Barthel G, et al. Brain regions essential for improved lexical access in an aged aphasic patient: A case report. BMC Neurology. 2006;6(28) doi: 10.1186/1472-2377-6-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer M, Flaisch T, Beitnstein C, Wienbruch C, Elbert T, Rockstroh B. Functional re-recruitment of dysfunctional brain areas predicts language recovery in chronic aphasia. NeuroImage. 2008;39:2038–2046. doi: 10.1016/j.neuroimage.2007.10.008. [DOI] [PubMed] [Google Scholar]
- Meinzer M, Obleser J, Flaisch T, Eulitz C, Rockstroh B. Recovery from aphasia as a function of language therapy in an early bilingual patient demonstrated by fMRI. Neuropsychologia. 2007;45(6):1247–1256. doi: 10.1016/j.neuropsychologia.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Meinzer MET, Wienbruch C, Djundja D, Barthel G, Rockstroh B. Intensive language training enhances brain plasticity in chronic aphasia. BMC Biology. 2004;2(20):1–9. doi: 10.1186/1741-7007-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murtha S, Chertkow H, Beauregard M, Evans A. The neural substrate of picture naming. Journal of Cognitive Neuroscience. 1999;11(4):399–423. doi: 10.1162/089892999563508. [DOI] [PubMed] [Google Scholar]
- Musso M, Weiller C, Kiebel S, Muller SO, Bulau P, Rijntjes M. Training-induced brain plasticity in Aphasia. Brain. 1999;122:1781–1790. doi: 10.1093/brain/122.9.1781. [DOI] [PubMed] [Google Scholar]
- Paulesu E, Goldacre B, Scifo P, Cappa SF, Gilardi MC, Castiglioni I, et al. Functional heterogeneity of left inferior frontal cortex as revealed by fMRI. NeuroReport. 1997;8:2011–2016. doi: 10.1097/00001756-199705260-00042. [DOI] [PubMed] [Google Scholar]
- Peck K, Moore A, Crosson B, Gaiefsky M, Gopinath K, White K, et al. Functional magnetic resonance imaging before and after aphasia therapy: Shifts in hemodynamic time to peak during an overt language task. Stroke. 2004;35:554–559. doi: 10.1161/01.STR.0000110983.50753.9D. [DOI] [PubMed] [Google Scholar]
- Perani D, Cappa SF, Tettamanti M, Rosa M, Scifo P, Miozzo A, et al. A fMRI study of word retrieval in aphasia. Brain and Language. 2003;85:357–368. doi: 10.1016/s0093-934x(02)00561-8. [DOI] [PubMed] [Google Scholar]
- Pizzamiglio L, Galati G, Committeri G. The contribution of functional neuroimaging to recovery after brain damage: A review. Cortex. 2001;37(1):1–31. doi: 10.1016/s0010-9452(08)70555-0. [DOI] [PubMed] [Google Scholar]
- Price CJ, Devlin JT, Moore CJ, Morton C, Laird AR. Meta-analyses of object naming: Effect of baseline. Human Brain Mapping Special Issue: Meta-Analysis in Functional Brain Mapping. 2005;25(1):70–82. doi: 10.1002/hbm.20132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulvermüller F, Hauk O, Zohsel K, Neininger B, Mohr B. Therapyrelated reorganization of language in both hemispheres of patients with chronic aphasia. NeuroImage. 2005;28(2):481–489. doi: 10.1016/j.neuroimage.2005.06.038. [DOI] [PubMed] [Google Scholar]
- Raymer AM, Thompson CK, Jacobs B, Legrand HR. Phonological treatment of naming deficits in aphasia – Model-based generalization analysis. Aphasiology. 1993;7(1):27–53. [Google Scholar]
- Richter M, Miltner W, Straube T. Association between therapy outcome and right-hemisphere activation in chronic aphasia. Brain: A Journal of Neurology. 2008;131(5):1391–1401. doi: 10.1093/brain/awn043. [DOI] [PubMed] [Google Scholar]
- Riddoch MJ, Humphreys GW. Birmingham object recognition battery. Hove, UK: Lawrence Erlbaum Associates Ltd., Publishers; 1993. [Google Scholar]
- Rijntjes M, Weiller C. Recovery of motor and language abilities after stroke: The contribution of functional imaging. Press in Neurobiology. 2002;66:109–122. doi: 10.1016/s0301-0082(01)00027-2. [DOI] [PubMed] [Google Scholar]
- Roach A, Schwartz MF, Martin N, Grewal RS, Brecher A. The Philadelphia naming test: Scoring and rationale. Clinical Aphasiology. 1996;24:121–133. [Google Scholar]
- Rosen HJ. Neural correlates of recovery from aphasia after damage to left inferior frontal cortex. Neurology. 2000;55:1883–1894. doi: 10.1212/wnl.55.12.1883. [DOI] [PubMed] [Google Scholar]
- Roskies AL, Fiez JA, Balota DA, Raichle ME, Petersen SE. Task-dependent modulation of regions in the left inferior frontal cortex during semantic processing. Journal of Cognitive Neuroscience. 2001;13:829–843. doi: 10.1162/08989290152541485. [DOI] [PubMed] [Google Scholar]
- Saur D, Lange R, Baumgaertner A, Schraknepper V, Willmes K, Rijntjes M, et al. Dynamics of language reorganization after stroke. Brain: A Journal of Neurology. 2006;129(6):1371–1384. doi: 10.1093/brain/awl090. [DOI] [PubMed] [Google Scholar]
- Schwartz MF, Dell GS, Martin N, Gahl S, Sobel P. A case-series test of the interactive two-step model of lexical access: Evidence from picture naming. Journal of Memory and Language. 2006;54(2):228–264. doi: 10.1016/j.jml.2006.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seto G, Sela WE, McIlroy SE, Black WR, Staines MJ, Bronskill AR. Quantifying head motion associated with motor tasks used in fMRI. NeuroImage. 2001;14(2):284–297. doi: 10.1006/nimg.2001.0829. [DOI] [PubMed] [Google Scholar]
- Small LS, Flores DK, Noll DC. Different neural circuits subserve reading before and after therapy for acquired dyslexia. Brain and Language. 1998;62:298–308. doi: 10.1006/brln.1998.1951. [DOI] [PubMed] [Google Scholar]
- Stone JV. Independent component analysis: An introduction. Trends Cognitive Science. 2002;6(2):59–64. doi: 10.1016/s1364-6613(00)01813-1. [DOI] [PubMed] [Google Scholar]
- Szekeres SF, Ylvisaker M, Cohen SB. A framework for cognitive rehabilitation therapy. In: Ylvisaker M, Gobble EM, editors. Community re-entry for head injured adults. Austin, TX: PRO-ED; 1987. pp. 87–136. [Google Scholar]
- Ventry IM, Weinstein BE. The hearing handicap inventory for the elderly: A new tool. Ear and Hearing. 1982;3:128–134. doi: 10.1097/00003446-198205000-00006. [DOI] [PubMed] [Google Scholar]
- Whatmough C, Chertkow H. Neuroanatomical aspects of naming. In: Hillis AE, editor. The handbook of adult language disorders. New York: Psychology Press; 2002. pp. 143–161. [Google Scholar]
- Wierenga CE, Maher LM, Moore AB, White KD, McGregor K, Soltysik DA, et al. Neural substrates of syntactic mapping treatment: An fMRI study of two cases. Journal of the International Neuropsychological Society. 2006;12(1):132–146. doi: 10.1017/S135561770606019X. [DOI] [PubMed] [Google Scholar]