Abstract
Asthmatic patients are known to have a higher risk of anxiety and depression. In the present study, we aimed to explore the association of serotonin transporter (5-HTT), brain-derived neurotrophic factor (BDNF) and neuropeptide S receptor 1 (NPSR1) gene polymorphisms with anxiety and depression in asthmatic patients. This was a cross-sectional study conducted on 143 asthmatic patients and 175 healthy volunteers. Of the asthmatic patients, 49 suffered from anxiety and 12 exhibited signs of depression. Patients with a lower level of education were more prone to depression. Both anxiety and depression were associated with poor asthma control as evaluated by the Asthma Control Test (ACT) score. The association of single nucleotide polymorphisms of BDNF, NPSR1 and 5-HTT with anxiety and depression in asthamtic patients was evaluated. The distribution of 5-HTT gene polymorphisms in the healthy group, the group with asthma but without anxiety, and the group with asthma and anxiety had significant differences. Females with asthma and anxiety were more prone to BDNF polymorphism. Also, BDNF gene distribution exhibited significant differences among those in the healthy group, the group with asthma but no depression, and the group with asthma and depression; however, NPSR1 gene distribution did not vary greatly between the groups. The anxiety score was significantly affected by the interaction between 5-HTT (LL, S+) and BDNF (A+, GG) (H=5.99, P=0.015). The depression score was significantly affected by the interaction between BDNF (A+, GG) and NPSR1 (AA, T+). We noted that both anxiety and depression led to poor asthma control. The interaction between 5-HTT (LL) and BDNF (A+) increased the risk of anxiety, and the interaction between BDNF (A+, GG) and NPSR1 (AA, T+) increased the risk of depression in asthmatic patients.
Keywords: asthmatic patients, anxiety, depression, serotonin transporter, brain-derived neurotrophic factor, neuropeptide S receptor 1, gene polymorphisms
Introduction
Bronchial asthma is a chronic inflammatory disease of the respiratory tract which is characterized by airway hyper-responsiveness and reversible airflow restriction. Currently, standardized treatment and self-management by patients have significantly reduced the incidence of acute asthmatic attacks. However, asthma remains a disease which does not yet have a complete cure (1). Psychological problems are common in asthmatic patients, even in patients who have well-controlled asthma. Valença et al (2) reported that 43.5% of patients with asthma had at least one type of psychiatric disorder. Anxiety and depression are the two most common disorders encountered in asthmatic patients, and tend to correlate with asthma control (3,4). A recent study reported that anxiety and depression occurred in 33.3 and 47.7% asthmatic patients, respectively (5).
Asthmatic patients are at a higher risk of psychiatric morbidity, with anxiety and depression being the two most common disorders in these patients (3,4,6–12). Asthma significantly affects psychological and social wellbeing due to the impact it has on routine activities, sleep and the daily life of patients (3,4,6–12). Conversely, psychological factors may be a risk factor for the exacerbation of this disorder. Another theory regarding the link between asthma and psychological factors describes asthma as a classic psychosomatic disorder caused by specific psychological conflicts (13).
The serotonin transporter (5-HTT) is known to be associated with depression and emotional stress (14). The 5′-flanking promoter region of the 5-HTT gene has a biallelic insertion/deletion (5-HTTLPR) (15). Furthermore, it has been reported that the 5-HTTLPR genotype is linked with severe depression (15); the polymorphisms within this region are associated with improved responses to treatment with selective serotonin reuptake inhibitors (16). Brain-derived neurotrophic factor (BDNF) is a growth factor which belongs to the neurotrophin family and is highly expressed in the hippocampus and amygdala of the brain (17). It regulates the pathophysiology of mood disorders, including major depressive disorder (MDD) and bipolar disorder (BD), as well as learning and memory (17,18). Patients with anxiety and BD are known to have decreased levels of BDNF (17,18). Previous studies have also implicated BDNF in the pathogenesis of asthma (19–21). Furthermore, the BDNF gene polymorphism has been reported to be associated with allergic asthma and allergic rhinitis (22).
Neuropeptide S receptor 1 (NPSR1) gene has been suggested to be a candidate gene which is associated with increased susceptibility to asthma and other atopic disorders in different populations (23). The signaling system of NPSR1 and its ligand neuropeptide S (NPS) have been implicated in various pathophysiological pathways, including regulation of the immunologic phenotype and various neurobiological phenomena such as wakefulness, arousal, anxiety, learning and memory (23).
To the best of our knowledge, the association of NPSR1, BDNF and 5-HTT gene polymorphisms with anxiety or depression in asthmatic patients has not been previously examined. Hence, this study was undertaken in order to correlate anxiety and depression with the clinical characteristics of asthmatic patients, and to explore their association with 5-HTT, BDNF and NPSR1 gene polymorphisms.
Subjects and methods
Subjects
This study was approved by the Medical Ethics Committee for Clinical Research, Zhongda Hospital Affiliated to Southeast University (Nanjing, China). Written informed consent was obtained from all subjects. The inclusion criteria were as follows: patients were of Han Chinese ethnicity aged >18 years, who had been diagnosed with bronchial asthma as per the diagnostic criteria established by the Respiratory Diseases Branch of the Chinese Medical Association (24), without mental disorders according to the diagnostic standard of the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM2-IV), and had completed at least primary education. Subjects with chronic diseases (diabetes, hypertension, coronary heart disease, chronic obstructive pulmonary disease and genetic diseases), pregnant or lactating women or individuals with a history of drug abuse were excluded from the study. The healthy controls were volunteers from Zhongda Hospital, which included hospital staff, doctors and medical students.
Assessment of asthma control, anxiety and depression
All patients completed questionnaires using the Hamilton Anxiety Rating Scale (HAMA), the Hamilton Depression Rating Scale (HAMD) and the Asthma Control Test (ACT) score (11). Asthma without anxiety was defined as a HAMA anxiety score ≤14 points; asthma with anxiety was defined as a HAMA anxiety score >14 points; asthma without depression was defined as a HAMD depression score ≤7 points; and asthma with depression was defined as a HAMD depression score >7 points.
Genomic DNA preparation
Blood for genomic studies was collected from all asthma patients and healthy controls in an ethylenediaminetetraacetic acid (EDTA) vial. The genomic DNA was extracted from 3 ml of EDTA-anticoagulated whole blood using a Blood Genomic DNA Extraction kit (cat. no. DP318; Tiangen Biotech (Beijing) Co., Ltd., Beijing, China) according to the manufacturer's instructions. The quality and quantity of genomic DNA extracted was examined with spectrophotometry (ND-1000; NanoDrop products, Thermo Fisher Scientific, Wilmington, DE, USA). All extracted DNA had an OD260/280 between 1.7 and 1.9. The purified DNA samples were stored at −80°C until further testing.
Polymerase chain reaction (PCR) amplification and genotyping
Genotyping of BDNF, NPSR1 and 5-HTT was performed using the PCR-restriction fragment length polymorphism (PCR-RFLP) and direct sequencing (GenScript Corp., Nanjing, China). For detecting single nucleotide polymorphisms (SNPs), 5-HTT (5-HTTLPR), BDNF (rs6265) and NPSR1 (rs324981) genes were amplified using PCR. The sequences of all primers and the conditions of PCR-RFLP analysis for the three polymorphisms (5-HTTLPR for 5-HTT, rs324981 for NPSR1 and rs6265 for BDNF) are summarized in Table I. Each SNP site for DNA sequencing was randomly selected from 10% of the samples. The sequencing was performed using the dideoxynucleotide termination method.
Table I.
Characterization of PCR reaction conditions for the analyzed single nucleotide polymorphisms.
| Target | Primer sequence (5′→3′) | Tm (°C) | Restriction enzyme | Allele sizes (bp) |
|---|---|---|---|---|
| 5-HTT | F: GGCGTTGCCGCTCTGAATGC | 59 | ||
| R: GAGGGACTGAGCTGGACAACC | ||||
| BDNF (rs6265) | F: ACTCTGGAGAGCGTGAATGG | 60 | Eco72I | A: 171 |
| R: ACTACTGAGCATCACCCTGGA | G: 99, 72 | |||
| NPSR1 (rs324981) | F: GCTTTGCATTTCCTCAGTGG | 60 | AseI | T: 471 |
| R: ATTTGTGGCTCGTTTGTGTTTTCT | A: 277, 194 |
5-HTT, serotonin transporter; Tm, annealing temperature (°C); BDNF, brain-derived neurotrophic factor (BDNF); NPSR1, neuropeptide S receptor 1; F, forward; R, reverse.
Statistical analysis
All statistical analyses were conducted using SPSS statistical analysis software (version 19.0; IBM SPSS, Chicago, IL, USA). Hardy-Weinberg equilibrium (HWE) was evaluated for each SNP in all groups. The Satterthwaite test was used to compare the differences in age between groups with and without anxiety or depression. The Chi-square test was used to compare the differences in genotypic distribution among groups. The interactive effects of different genotypes on the anxiety/depression scores were analyzed using the Scheirer-Ray-Hare test. A P-value <0.05 was considered to indicate a statistically significant difference.
Results
Baseline characteristics of subjects
The baseline characteristics of the subjects are summarized in Table II. A total of 143 (male 63, female 80) asthmatic patients were examined in this study. There were 49 patients with anxiety and 94 without anxiety. There were 12 patients with depression and 131 without depression. There were 20 males and 29 females with anxiety, and 7 males and 5 females with depression. A total of 175 (male 51, female 124) healthy controls, (mean age, 39.11±14.98 years) were included in this study. The mean age of the asthmatic patients was 50.22±12.95 years. The mean age of the patients with and without anxiety was 52.76±10.13 and 48.9±14.08 years, respectively, with no significant difference in age between the two groups (t=−1.88, P=0.063). Similarly, no significant difference was observed between the mean ages of patients with and without depression [54.08±8.21 and 49.87±13.27 years, respectively (t=−1.08, P=0.283)]. These results suggest that the occurrence of both anxiety and depression in asthmatic patients is not associated with age. Both age and gender were significantly different in the group with asthma and the group with asthma and anxiety (age, F=25.74, P<0.0001; gender, χ2=7.95, P=0.019), when compared with healthy controls.
Table II.
Baseline characteristics of study subjects.
| Variable | Healthy | Asthma | Asthma without anxiety | Asthma with anxiety | Statistics | Asthma without depression | Asthma with depression | Statistics |
|---|---|---|---|---|---|---|---|---|
| Total | 175 | 143 | 94 | 49 | 131 | 12 | ||
| Age (years) | 39.11±14.98 | 50.22±12.95 | 48.9±14.08 | 52.76±10.13 | t=−1.88, P=0.063 |
49.87±13.27 | 54.08±8.21 | t=−1.08, P=0.283 F=25.74, P<0.0001 |
| Gender | ||||||||
| Male | 51 | 63 | 43 | 20 | 56 | 7 | χ2=7.95, | |
| Female | 124 | 80 | 51 | 29 | 75 | 5 | P=0.019 | |
| Education | ||||||||
| 1 | 4 (4.35) | 2 (4.08) | χ2=0.29, | 5 (3.88) | 1 (8.33) | χ2=5.70, | ||
| 2 | 22 (23.91) | 14 (28.57) | P=0.59 | 29 (22.48) | 7 (58.33) | P=0.017 | ||
| 3 | 34 (36.96) | 18 (36.73) | 50 (38.76) | 2 (16.67) | ||||
| 4 | 32 (4.78) | 15 (30.61) | 45 (34.88) | 2 (16.67) | ||||
| ACT score | N/A | 18.49±4.51 | 19.77±4 | 16.04±4.47 | P<0.05 | 18.9±4.37 | 14±3.67 | t=0.76, P=0.0002 |
ACT, Asthma Control Test. Education was graded as follows: 1, primary school; 2, junior high school; 3, senior high school and technical secondary school; 4, college and university.
In the present study, patients who were less educated were more likely to suffer from depression (χ2 =5.70, P=0.017) rather than anxiety (χ2=0.29, P=0.59). Our results suggest a negative correlation between depression and education levels, possibly due to the educated patients having a better understanding of asthma and other diseases. Upon evaluation of the ACT score, we noted that asthma patients with anxiety and depression had lower scores as compared to those without any psychiatric illness (anxiety, 16.04±4.47; P<0.05 and depression, 14±3.67; P=0.0002). These findings suggest a negative correlation of the ACT score with both anxiety and depression in asthmatic patients.
Association of 5-HTT gene polymorphisms with anxiety and depression in asthmatic patients
To examine the association of 5-HTT gene polymorphisms with anxiety and depression in asthmatic patients, we analyzed the frequency of 5-HTT genotypes in the healthy control group, the groups with asthma but without anxiety/depression, and the groups with asthma and anxiety/depression (Table III and Fig. 1). In addition, 5-HTT gene polymorphisms were not detected in 6 healthy subjects. Therefore, there were data from 169 healthy subjects shown in Table III.
Table III.
Genotype distributions and allele frequencies of 5-HTT polymorphisms for asthmatic patients vs. control group.
| Subject | Genotype
|
Total | Statistics | ||
|---|---|---|---|---|---|
| LL | LS | SS | |||
| Healthy | 6 (3.55) | 63 (37.28) | 100 (59.17) | 169 | |
| Male | 3 (6.12) | 17 (34.69) | 29 (59.18) | 49 | |
| Female | 3 (2.50) | 46 (38.33) | 71 (59.17) | 120 | |
| Asthma without anxiety | 10 (11.11) | 42 (56.67) | 38 (42.22) | 90 | |
| Male | 4 (9.76) | 20 (48.78) | 17 (41.46) | 41 | |
| Female | 6 (12.24) | 22 (44.90) | 21 (42.86) | 49 | |
| Asthma with anxiety | 3 (6.38) | 21 (44.68) | 23 (48.94) | 47 | χ2=10.18, P=0.038 |
| Male | 3 (15.79) | 7 (36.84) | 9 (47.37) | 19 | χ2=4.02, P=0.43 |
| Female | 0 (0.00) | 14 (50.00) | 14 (50.00) | 28 | χ2=10.97, P=0.027 |
| Asthma without depression | 12 (9.52) | 59 (46.83) | 55 (43.65) | 126 | |
| Male | 6 (11.32) | 24 (45.28) | 23 (43.40) | 53 | |
| Female | 6 (8.22) | 35 (47.95) | 32 (43.84) | 73 | |
| Asthma with depression | 1 (9.09) | 4 (36.36) | 6 (54.55) | 11 | χ2=9.34, P=0.053 |
| Male | 1 (14.29) | 3 (42.86) | 3 (42.86) | 7 | χ2=3.04, P=0.55 |
| Female | 0 (0.00) | 1 (25.00) | 3 (75.00) | 4 | χ2=7.09, P=0.13 |
5-HTT, serotonin transporter.
Figure 1.
Genotyping single nucleotide polymorphism (SNP) (5-HTTLPR) in the serotonin transporter (5-HTT) gene. (A) PCR products were resolved in 3% agarose gel. Lanes 1, 3, 5, 6, 2 and 4: LL, homozygous; lanes 7 and 8: SS, homozygous; and lane 9: SL, heterozygous. (B) Representative sequence of 5-HTTLPR.
The majority of healthy individuals had the SS (59.17%) genotype. However, in the group with asthma but without anxiety, the majority had the LS (56.67%) genotype, followed by SS (42.22%) and LL (11.11%) genotypes. In the group with asthma and anxiety, the LS and SS genotypes accounted for 44.68 and 48.94%, respectively, whereas LL accounted for only 6.38%. None of the females had the LL genotype in this group. There were significant differences in the distribution of 5-HTT genotypes in the group with asthma but without anxiety, and the group with asthma and anxiety, when compared with the healthy controls (χ2=10.18, P=0.038). Furthermore, there were significant differences in the distribution of 5-HTT genotypes among female patients (χ2=10.97, P=0.027) with asthma and anxiety when compared with healthy females. However, similar results were not noted for males. These findings suggest an association between the 5-HTT gene polymorphisms and female asthmatic patients with anxiety.
In the group with asthma without depression, the LS and SS genotypes accounted for 46.83 and 43.65%, respectively; LL accounted for only 9.52%. In the group with asthma and depression, LS and SS accounted for 36.36 and 54.55%, respectively, whereas LL accounted for only 9.09%. It is important to note that none of the females had the LL genotype. The Chi-square test showed that 5-HTT gene distributions in the healthy group, and in asthma patients with or without depression group were similar (χ2=9.34, P=0.053). Also, there was no gender bias between the three groups. These findings suggest that there is no association between 5-HTT gene polymorphisms and asthmatic patients with depression.
Association of BDNF gene polymorphisms with anxiety and depression
The frequency of BDNF gene polymorphisms in the healthy controls, asthmatic patients without anxiety/depression, and groups with asthma and anxiety/depression was also examined (Table IV and Fig. 2). In addition, BDNF gene polymorphisms were not detected in 4 healthy subjects. Therefore, there were data from 171 healthy subjects shown in Table IV. We noted that 52.63% of healthy individuals had the AG genotype. In the group with asthma but not anxiety, the major genotype of BNDF was AA (40.66%), followed by AG (32.97%) and GG (26.37%). In the group with asthma and anxiety, the major genotype of BNDF was AA (44.44%), followed by AG (31.11%) and GG (24.44%). BDNF genotype distributions in the group with asthma but not anxiety, and the group with asthma and anxiety (χ2=24.72, P<0.0001) were significantly different when compared with the control group. Furthermore, there were significant differences in the distribution of the BNDF genotype among the female asthmatic patients with anxiety when compared with healthy females (χ2=19.35, P=0.0007). A corresponding association was not observed in male patients. These findings suggest an association between BDNF gene polymorphisms and female asthmatic patients with anxiety.
Table IV.
Genotype distribution and allele frequencies of BDNF polymorphisms in asthmatic patients vs. controls.
| Subject | Genotype
|
Total | Statistics | ||
|---|---|---|---|---|---|
| AA | AG | GG | |||
| Healthy | 69 (40.35) | 90 (52.63) | 12 (7.02) | 171 | |
| Male | 22 (43.14) | 27 (52.94) | 2 (3.92) | 51 | |
| Female | 47 (39.17) | 63 (52.50) | 10 (8.33) | 120 | |
| Asthma without anxiety | 37 (40.66) | 30 (32.97) | 24 (26.37) | 91 | |
| Male | 17 (40.48) | 17 (40.48) | 8 (19.05) | 42 | |
| Female | 20 (40.82) | 13 (26.53) | 16 (32.65) | 49 | |
| Asthma with anxiety | 20 (44.44) | 14 (31.11) | 11 (24.44) | 45 | χ2=24.72, P<0.0001 |
| Male | 9 (47.37) | 5 (26.32) | 5 (26.32) | 19 | χ2=9.34, P=0.053 |
| Female | 11 (42.31) | 9 (34.62) | 6 (23.08) | 26 | χ2=19.35, P=0.0007 |
| Asthma without depression | 52 (41.6) | 42 (33.6) | 31 (24.8) | 125 | |
| Male | 22 (40.74) | 21 (38.89) | 11 (20.37) | 54 | |
| Female | 30 (42.25) | 21 (29.58) | 20 (28.17) | 71 | |
| Asthma with depression | 5 (45.45) | 2 (18.18) | 4 (36.36) | 11 | χ2=26.40, P<0.0001 |
| Male | 4 (57.14) | 1 (14.29) | 2 (28.57) | 7 | χ2=10.82, P=0.029 |
| Female | 1 (25.00) | 1 (25.00) | 2 (50.00) | 4 | χ2=18.92, P=0.0008 |
BDNF, brain-derived neurotrophic factor.
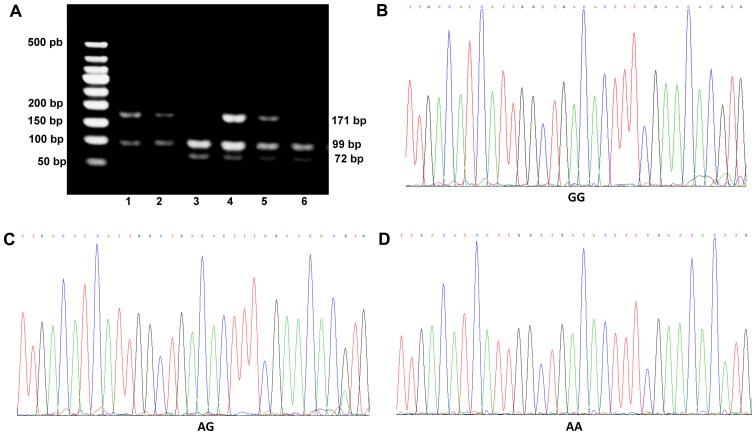
Figure 2.
Genotyping single nucleotide polymorphism (SNP) (rs6265) in the brain-derived neurotrophic factor (BDNF) gene. (A) PCR products were digested with Eco72I and resolved in 3% agarose gel. Lanes 1 and 2: AA, homozygous; lanes 4 and 5: AG, heterozygous; and lanes 3 and 6: GG, homozygous. (B–D) Representative sequences of GG, AG and AA, respectively.
In the group of asthmatic patients without depression AA, AG and GG genotypes of BNDF accounted for 41.6, 33.6 and 24.8%, respectively. In the group with asthma and depression, AA, AG and GG genotypes accounted for 45.45, 18.18 and 36.36%, respectively. In this group, AA, AG and GG genotypes were present in 57.14, 14.29 and 28.57% of males, respectively, and 25.00, 25.00 and 50.00% of females, respectively. There were significant differences in the distribution of BDNF genotypes in the asthmatic patients with and without depression (χ2=26.40, P<0.0001), when compared with the healthy controls. Further analysis revealed significant differences in the distribution of BNDF genotypes among both male (χ2=10.82, P=0.029) and female patients (χ2=18.92, P=0.0008) with asthma and depression, when compared with healthy males and females, respectively. These findings suggest an association between BDNF gene polymorphisms and asthmatic patients with depression regardless of gender.
Association of NPSR1 gene polymorphisms with anxiety and depression
To examine the association between NPSR1 gene polymorphisms and both anxiety and depression in asthmatic patients, we analyzed the frequencies of NPSR1 genotypes in the healthy control group, the groups with asthma but without anxiety/depression, and the groups with asthma and anxiety/depression (Table V and Fig. 3). In addition, NPSR1 gene polymorphisms were not detected in 4 healthy subjects. Therefore, there were data from 171 healthy subjects shown in Table V.
Table V.
Genotype distribution and allele frequencies of NPSR1 polymorphisms in asthmatic patients vs. controls.
| Subject | Genotype
|
Total | Statistics | ||
|---|---|---|---|---|---|
| TT | AT | AA | |||
| Healthy | 59 (34.50) | 79 (46.20) | 33 (19.30) | 171 | |
| Male | 19 (37.25) | 26 (50.98) | 6 (11.76) | 51 | |
| Female | 40 (33.33) | 53 (44.17) | 27 (22.50) | 120 | |
| Asthma without anxiety | 26 (28.57) | 49 (53.85) | 16 (17.58) | 91 | |
| Male | 13 (30.95) | 23 (54.76) | 6 (14.29) | 42 | |
| Female | 13 (26.53) | 26 (53.06) | 10 (20.41) | 49 | |
| Asthma with anxiety | 16 (34.78) | 20 (43.48) | 10 (21.74) | 46 | χ2=1.94, P=0.75 |
| Male | 7 (36.84) | 8 (42.11) | 4 (21.05) | 19 | χ2=1.53, P=0.82 |
| Female | 9 (33.33) | 12 (44.44) | 6 (22.22) | 27 | χ2=1.23, P=0.87 |
| Asthma without depression | 40 (31.75) | 62 (49.21) | 24 (19.05) | 126 | |
| Male | 19 (35.19) | 26 (48.15) | 9 (16.67) | 54 | |
| Female | 21 (29.17) | 36 (50.00) | 15 (20.83) | 72 | |
| Asthma with depression | 2 (18.18) | 7 (63.64) | 2 (18.18) | 11 | χ2=1.72, P=0.79 |
| Male | 1 (14.29) | 5 (71.43) | 1 (14.29) | 7 | χ2=2.22, P=0.70 |
| Female | 1 (25.00) | 2 (50.00) | 1 (25.00) | 4 | χ2=0.72, P=0.95 |
NPSR1, neuropeptide S receptor 1.
Figure 3.
Genotyping single nucleotide polymorphism (SNP) (rs324981) in the neuropeptide S receptor 1 (NPSR1) gene. (A) PCR products were digested with AseI and resolved in 3% agarose gel. Lane 1: TT, homozygous; lanes 2, 4 and 6: AT, heterozygous; and lanes 3 and 5: AA, homozygous. (B–D) Representative sequence of AA, AT and TT, respectively.
In the healthy controls, NPSR1 genotypes AT, TT and AA accounted for 46.20, 34.50 and 19.30%, respectively. Among the asthmatic patients, AT was the most common genotype that accounted for 53.85, 43.48, 49.21 and 63.64%, in asthma without anxiety, asthma with anxiety, asthma without depression, and asthma with depression, respectively; followed by TT (28.57, 34.78, 31.75 and 18.18%, respectively); and AA (17.58, 21.74, 19.05 and 18.18%, respectively). NPSR1 genotype distribution in the asthma without anxiety group, and the asthma with anxiety group (χ2=1.94, P=0.75) were not found to be significantly different when compared with healthy controls. Furthermore, there were no significant differences in genotype distribution among male (χ2=1.53, P=0.82) and female patients (χ2=1.23, P=0.87) in the asthma with anxiety group, when compared with healthy males and females, respectively. These findings suggest a lack of association between NPSR1 gene polymorphisms (both overall and gender related) and asthmatic patients with anxiety.
NPSR1 genotype distribution was not found to be significantly different in the asthma without depression group, and the asthma with depression group (χ2=1.72, P=0.79), when compared with healthy controls. Furthermore, there were no significant differences in genotype distribution among male (χ2=2.22, P=0.70) and female asthmatic patients (χ2=0.72, P=0.95) with depression, when compared with healthy males and females, respectively. These findings also indicate a lack of association between NPSR1 gene polymorphisms (both overall and gender related) and depression in asthmatic patients.
Allele frequencies of 5-HTT, BDNF and NPSR1 in asthma patients with and without anxiety or depression
We analyzed the allele frequencies of 5-HTT, BDNF and NPSR1 in the asthmatic patients with and without anxiety or depression (Table VI). The majority of patients with asthma had the S+ allele in the 5-HTT gene, A+ in the BDNF gene and T+ in the NPSR1 gene. The frequency of the S+ allele in the 5-HTT gene was 89.36% (without anxiety), 93.88% (with anxiety), 90.84% (without depression) and 91.67% (with depression). LL only accounted for 10.64, 6.12, 9.16 and 8.33%, respectively. The frequency of the A+ allele in the BDNF gene was 74.47% (without anxiety), 77.55% (with anxiety), 76.34% (without depression) and 66.67% (with depression); GG accounted for 25.53, 22.45, 23.66 and 33.33%, respectively. The frequency of the T+ allele in the NPSR1 gene was 82.98% (without anxiety), 79.59% (with anxiety), 81.68% (without depression), and 83.33% (with depression); and AA accounted for 17.02, 20.41, 18.32 and 16.67%, respectively.
Table VI.
Genotype distributions of 5-HTT and BDNF and NPSR1 polymorphisms in asthmatic patients with and without anxiety or depression.
| 5-HTT
|
BDNF
|
NPSR1
|
||||
|---|---|---|---|---|---|---|
| S+ | LL | A+ | GG | T+ | AA | |
| Asthma without anxiety | 84 (89.36) | 10 (10.64) | 70 (74.47) | 24 (25.53) | 78 (82.98) | 16 (17.02) |
| Asthma with anxiety | 46 (93.88) | 3 (6.12) | 38 (77.55) | 11 (22.45) | 39 (79.59) | 10 (20.41) |
| Asthma without depression | 119 (90.84) | 12 (9.16) | 100 (76.34) | 31 (23.66) | 107 (81.68) | 24 (18.32) |
| Asthma with depression | 11 (91.67) | 1 (8.33) | 8 (66.67) | 4 (33.33) | 10 (83.33) | 2 (16.67) |
5-HTT, serotonin-transporter; BDNF, brain-derived neurotrophic factor; NPSR1, neuropeptide S receptor 1.
Correlation of 5-HTT, BDNF and NPSR1 gene polymorphisms with anxiety/depression scores
When the alleles were LL (5-HTT) and A+ (BDNF), the anxiety score had the highest median value. Scheirer-Ray-Hare analysis demonstrated that the anxiety score was significantly affected by the interactions between 5-HTT (LL, S+) and BDNF (A+, GG) (H=5.99, P=0.015), as shown in Table VII. In addition, BDNF gene polymorphisms were not detected in 1 patient. Therefore, there were data from 142 patients shown in Table VII. This suggests a synergistic effect of the interaction between 5-HTT and BDNF on the anxiety score. When the alleles were GG (BDNF) and AA (NPSR1), the depression score had the maximum median value. Scheirer-Ray-Hare analysis showed that the depression score was significantly affected by the interactions between BDNF (A+, GG) and NPSR1 (AA, T+) (H=4.22, P=0.04), as shown in Table VIII. The results suggest that the interaction between BDNF and NPSR1 had a synergistic effect on the depression score.
Table VII.
Interaction between 5-HTT and BDNF polymorphisms and its affect on the anxiety score of asthmatic patients.
| BDNF | 5-HTT | Frequency | Anxiety score
|
Statistics | |
|---|---|---|---|---|---|
| Median | Quartile | ||||
| A+ | S+ | 97 | 11 | 9 | H=5.99, |
| GG | S+ | 33 | 8 | 8 | P=0.015 |
| A+ | LL | 10 | 82 | 6 | |
| GG | LL | 2 | 20 | 12 | |
5-HTT, serotonin transporter; BDNF, brain-derived neurotrophic factor.
Table VIII.
Interaction between BDNF and NPSR1 polymorphisms and its affect on the depression score of asthmatic patients.
| BDNF | NPSR1 | Frequency | Depression score
|
Statistics | |
|---|---|---|---|---|---|
| Median | Quartile | ||||
| A+ | T+ | 87 | 6 | 6 | H=4.22, |
| A+ | AA | 21 | 3 | 6 | P=0.04 |
| GG | T+ | 30 | 4.5 | 7 | |
| GG | AA | 5 | 8 | 7 | |
BDNF, brain-derived neurotrophic factor; NPSR1, neuropeptide S receptor 1.
Discussion
Asthmatic patients are known to have a higher risk of developing mental disorders (25). The interactions between behavioral, neural, endocrine and immune processes have been studied in asthmatic patients and it has been noted that a major role is played by psychological factors in the development of asthma (26). The higher risk of anxiety and depression in asthmatic patients is also well documented (5,12,27–29). Furthermore, anxiety and depression are closely associated with poor asthma control and aggravated symptomatology (2,3,30). Genetic polymorphisms may predispose asthmatic patients to anxiety or depression. In this study, we sought to examine the correlation between both anxiety and depression and the clinical characteristics of asthmatic patients, and we explored the association between NPSR1, BDNF and 5-HTT gene polymorphisms and anxiety and depression in these patients. We found no evidence of any association between age or education level and the occurrence of anxiety. However, depression was associated with a lower level of education, but not age. Both anxiety and depression negatively correlated with the ACT score.
Genetic factors are thought to influence the susceptibility of asthmatic patients to anxiety or depression. We noted that the interaction between 5-HTT (LL) and BDNF (A+) exerted a synergistic effect to increase the anxiety score in the asthmatic patients whereas the interaction between BDNF (A+, GG) and NPSR1 (AA, T+) exerted a synergistic effect to increase the depression score in asthmatic patients.
To explore a potential association between anxiety/depression and the demographic and clinical characteristics of the patients, we disaggregated the study subjects by age, gender, educational level and ACT scores. Consistent with a previous study (31), the incidence of asthma correlated with age and gender. However, significant differences in asthmatic patients with or without anxiety and with or without depression were not noted with respect to age or gender. The incidence of anxiety or depression was similar between males and females, as well as with respect to age. The results of our study differ from some earlier studies in this respect (32,33). For example, in a study by Fernandes et al (33), the risk of anxiety was noted as being directly proportional to age, and inversely proportional to the socioeconomic level, particularly in women. Notably, we found that depression rather than anxiety was associated with a lower level of education. Consistent with the findings of previous studies (2,3,5,7,10,34), both anxiety and depression were associated with poor asthma control, as evaluated by the ACT score in our study. Amelink et al (7) reported that patients with severe prednisone-dependent asthma were at a higher risk of emotional distress than those with severe non-prednisone dependent asthma, or those with mild to moderate asthma. Thus, co-existing anxiety and/or depression may be a major determinant of treatment outcomes in asthmatic patients. These findings underline the importance of screening asthmatic patients for anxiety and depression, as part of the routine management of these patients. Furthermore, adjunctive behavioral therapy or psychiatric intervention should be considered for these patients.
Our study also assessed the role of genetic factors in contributing to the increased risk of anxiety or depression in asthmatic patients. We explored the association between SNPs of 5-HTT, BDNF and NPSR1 genes and anxiety or depression in asthmatic patients. Our results demonstrated an association between 5-HTT gene polymorphisms and anxiety in female asthmatic patients. To the best of our knowledge, this is the first report linking 5-HTT gene polymorphisms with anxiety in asthmatic patients. Caspi et al (35) reported an association between polymorphisms in the promoter region of the 5-HTT gene and the influence of stressful life events on depression. However, a meta-analysis of 14 independent studies (14) did not support this conclusion. This previous analysis showed that the 5-HTT polymorphism was not associated with an increased risk of depression in males alone, females alone or both males and females (14). BDNF is a neurotrophic factor which plays a critical role in maintaining the function of the neurons (21). It has also been reported to play a pivotal role in the pathogenesis of major depression and other mood disorders (21,36). In addition to being highly expressed in the brain, it is also expressed in the lungs (37). Braun et al (38) suggested a link between BDNF and allergic bronchial asthma. Genetic variants of BDNF have been implicated in the causation of allergic asthma in various populations (19,22,39–41). However, whether polymorphisms of the BDNF gene predispose asthmatic patients to be affected by mood disorders has not yet been established. In the present study, gene polymorphisms in BDNF were not only associated with anxiety in female asthmatic patients, but were also linked with depression in the asthmatic population regardless of gender. These results suggest that BDNF genetic variants play an important role in the pathogenesis of anxiety and depression in asthmatic patients.
The NPS receptor signaling pathway is involved in the pathogenesis of asthma and allergies (42). It also regulates anxiety and arousal in rodents (43). Donner et al (22) suggested that the NPS and NPSR1 signaling pathway is involved in regulating human susceptibility to anxiety disorders. The NPSR1 gene has been linked with asthma, high serum total IgE levels and other atopic diseases (44). By contrast, the present study showed that NPSR1 gene polymorphisms were not associated with either anxiety or depression in asthmatic patients.
Furthermore, we found that the S+ (5-HTT), A+ (BDNF) and T+ (NPSR1) alleles had the highest frequency in the asthmatic patients regardless of anxiety or depression. More importantly, the risk and severity of anxiety or depression appeared to be influenced by the interaction between gene-gene polymorphisms. Asthmatic patients carrying both risk alleles 5-HTT (LL) and BDNF (A+) had enhanced anxiety scores, and those carrying risk alleles BDNF (A+, GG) and NPSR1 (AA, T+) had increased depression scores. A previous study demonstrated that the NPSR1 polymorphism in AA carriers was linked to increased anxiety scores. However, the fear-potentiated startle is affected by the interaction between 5-HTT and NPSR1 polymorphisms (45). In our study, there was no evidence to suggest that the interaction between 5-HTT and NPSR1 polymorphisms plays a role in inducing anxiety or depression in asthmatic patients. Our findings suggest that anxiety and depression in asthmatic patients are influenced not only by polymorphisms of individual genes, but also by interactions between different gene polymorphisms.
It is necessary to acknowledge some limitations of our study. In the present study, the assessment of anxiety and depression was undertaken using a simple questionnaire, without conducting a structured interview. Another limitation is the cross-sectional study design, due to which the results may not be consistent over time. The third possible limitation is the existence of selection bias in the study, as all the patients were enrolled from a single hospital.
In conclusion, the present study demonstrates differences in the risk factors for anxiety and depression in asthmatic patients. Depression was negatively associated with the level of education. There was a correlation between both anxiety and depression and poor asthma control. The interaction between 5-HTT (LL) and BDNF (A+) appeared to increase the risk of anxiety, whereas the interaction between BDNF (A+, GG) and NPSR1 (AA, T+) appeared to increase the risk of depression in asthmatic patients.
Acknowledgments
We would like to thank Dr Xiaojin Yu and his research team at the Southeast University School of Public Health for assistance with statistical analysis. We would like to thank Professor Ran Liu at the Southeast University School of Public Health for assistance in genetic testing.
References
- 1.Grainge C, Thomas PS, Mak JC, Benton MJ, Lim TK, Ko FW. Year in review 2015: Asthma and chronic obstructive pulmonary disease. Respirology. 2016;21:765–775. doi: 10.1111/resp.12771. [DOI] [PubMed] [Google Scholar]
- 2.Valença AM, Falcão R, Freire RC, Nascimento I, Nascentes R, Zin WA, Nardi AE. The relationship between the severity of asthma and comorbidities with anxiety and depressive disorders. Rev Bras Psiquiatr. 2006;28:206–208. doi: 10.1590/S1516-44462006005000005. [DOI] [PubMed] [Google Scholar]
- 3.Di Marco F, Verga M, Santus P, Giovannelli F, Busatto P, Neri M, Girbino G, Bonini S, Centanni S. Close correlation between anxiety, depression, and asthma control. Respir Med. 2010;104:22–28. doi: 10.1016/j.rmed.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 4.Thoren C, Petermann F. Reviewing asthma and anxiety. Respir Med. 2000;94:409–415. doi: 10.1053/rmed.1999.0757. [DOI] [PubMed] [Google Scholar]
- 5.Coban H, Aydemir Y. The relationship between allergy and asthma control, quality of life, and emotional status in patients with asthma: a cross-sectional study. Allergy Asthma Clin Immunol. 2014;10:67. doi: 10.1186/s13223-014-0067-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katon WJ, Richardson L, Lozano P, McCauley E. The relationship of asthma and anxiety disorders. Psychosom Med. 2004;66:349–355. doi: 10.1097/01.psy.0000126202.89941.ea. [DOI] [PubMed] [Google Scholar]
- 7.Amelink M, Hashimoto S, Spinhoven P, Pasma HR, Sterk PJ, Bel EH, ten Brinke A. Anxiety, depression and personality traits in severe, prednisone-dependent asthma. Respir Med. 2014;108:438–444. doi: 10.1016/j.rmed.2013.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Cheng Z, Dai LL, Li F, Liu Y, Kang Y, Chen HJ, Wang X, Zhang H, Ni R. Relationship between anxiety, depression and asthma control. Zhonghua Yi Xue Za Zhi. 2012;92:2128–2130. In Chinese. [PubMed] [Google Scholar]
- 9.Deshmukh VM, Toelle BG, Usherwood T, O'Grady B, Jenkins CR. The association of comorbid anxiety and depression with asthma-related quality of life and symptom perception in adults. Respirology. 2008;13:695–702. doi: 10.1111/j.1440-1843.2008.01310.x. [DOI] [PubMed] [Google Scholar]
- 10.Kullowatz A, Kanniess F, Dahme B, Magnussen H, Ritz T. Association of depression and anxiety with health care use and quality of life in asthma patients. Respir Med. 2007;101:638–644. doi: 10.1016/j.rmed.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Letitre SL, de Groot EP, Draaisma E, Brand PL. Anxiety, depression and self-esteem in children with well-controlled asthma: case-control study. Arch Dis Child. 2014;99:744–748. doi: 10.1136/archdischild-2013-305396. [DOI] [PubMed] [Google Scholar]
- 12.Liu S, Wu R, Li L, Liu L, Li G, Zhang X, Guo Y, Wang Y, Zhang H, Li G, Li H. The prevalence of anxiety and depression in Chinese asthma patients. PLoS One. 2014;9:e103014. doi: 10.1371/journal.pone.0103014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alvarez GG, Fitzgerald JM. A systematic review of the psychological risk factors associated with near fatal asthma or fatal asthma. Respiration. 2007;74:228–236. doi: 10.1159/000097676. [DOI] [PubMed] [Google Scholar]
- 14.Risch N, Herrell R, Lehner T, Liang KY, Eaves L, Hoh J, Griem A, Kovacs M, Ott J, Merikangas KR. Interaction between the serotonin transporter gene (5-HTTLPR), stressful life events, and risk of depression: a meta-analysis. JAMA. 2009;301:2462–2471. doi: 10.1001/jama.2009.878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mann JJ, Huang YY, Underwood MD, Kassir SA, Oppenheim S, Kelly TM, Dwork AJ, Arango V. A serotonin transporter gene promoter polymorphism (5-HTTLPR) and prefrontal cortical binding in major depression and suicide. Arch Gen Psychiatry. 2000;57:729–738. doi: 10.1001/archpsyc.57.8.729. [DOI] [PubMed] [Google Scholar]
- 16.Smeraldi E, Zanardi R, Benedetti F, Di Bella D, Perez J, Catalano M. Polymorphism within the promoter of the serotonin transporter gene and antidepressant efficacy of fluvoxamine. Mol Psychiatry. 1998;3:508–511. doi: 10.1038/sj.mp.4000425. [DOI] [PubMed] [Google Scholar]
- 17.Park MH, Chang KD, Hallmayer J, Howe ME, Kim E, Hong SC, Singh MK. Preliminary study of anxiety symptoms, family dysfunction, and the brain-derived neurotrophic factor (BDNF) Val66Met genotype in offspring of parents with bipolar disorder. J Psychiatr Res. 2015;61:81–88. doi: 10.1016/j.jpsychires.2014.11.013. [DOI] [PubMed] [Google Scholar]
- 18.Hashimoto K, Shimizu E, Iyo M. Critical role of brain-derived neurotrophic factor in mood disorders. Brain Res Brain Res Rev. 2004;45:104–114. doi: 10.1016/j.brainresrev.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Watanabe T, Fajt ML, Trudeau JB, Voraphani N, Hu H, Zhou X, Holguin F, Wenzel SE. Brain Derived Neurotrophic Factor (BDNF) Expression in Asthma. Association with Severity and Type-2 Inflammatory Processes. Am J Respir Cell Mol Biol. 2015:844–852. doi: 10.1165/rcmb.2015-0015OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ozek E, Ekici B. Asthma and suicide: possible role of brain-derived neurotrophic factor. Med Hypotheses. 2011;77:261–262. doi: 10.1016/j.mehy.2011.04.028. [DOI] [PubMed] [Google Scholar]
- 21.Tsai SJ. Asthma, major depression and brain-derived neurotrophic factor. Med Hypotheses. 2005;65:417–418. doi: 10.1016/j.mehy.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Andiappan AK, Parate PN, Anantharaman R, Suri BK, Wang Y, Chew FT. Genetic variation in BDNF is associated with allergic asthma and allergic rhinitis in an ethnic Chinese population in Singapore. Cytokine. 2011;56:218–223. doi: 10.1016/j.cyto.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 23.Donner J, Haapakoski R, Ezer S, Melén E, Pirkola S, Gratacòs M, Zucchelli M, Anedda F, Johansson LE, Söderhäll C, et al. Assessment of the neuropeptide S system in anxiety disorders. Biol Psychiatry. 2010;68:474–483. doi: 10.1016/j.biopsych.2010.05.039. [DOI] [PubMed] [Google Scholar]
- 24.Asthma Workgroup CTS. Chinese Medical Association Guideline Chinese expert consensus on bronchial asthma control. Chin J Tuberc Respir Dis. 2008;31:177–185. In Chinese. [Google Scholar]
- 25.Feldman JM, Siddique MI, Morales E, Kaminski B, Lu SE, Lehrer PM. Psychiatric disorders and asthma outcomes among high-risk inner-city patients. Psychosom Med. 2005;67:989–996. doi: 10.1097/01.psy.0000188556.97979.13. [DOI] [PubMed] [Google Scholar]
- 26.Di Marco F, Santus P, Centanni S. Anxiety and depression in asthma. Curr Opin Pulm Med. 2011;17:39–44. doi: 10.1097/MCP.0b013e328341005f. [DOI] [PubMed] [Google Scholar]
- 27.Adams RJ, Wilson DH, Taylor AW, Daly A, Tursan d'Espaignet E, Dal Grande E, Ruffin RE. Psychological factors and asthma quality of life: a population based study. Thorax. 2004;59:930–935. doi: 10.1136/thx.2003.010256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alonso J, de Jonge P, Lim CC, Aguilar-Gaxiola S, Bruffaerts R, Caldas-de-Almeida JM, Liu Z, O'Neill S, Stein DJ, Viana MC, et al. Association between mental disorders and subsequent adult onset asthma. J Psychiatr Res. 2014;59:179–188. doi: 10.1016/j.jpsychires.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Scott KM, Von Korff M, Ormel J, Zhang MY, Bruffaerts R, Alonso J, Kessler RC, Tachimori H, Karam E, Levinson D, et al. Mental disorders among adults with asthma: results from the World Mental Health Survey. Gen Hosp Psychiatry. 2007;29:123–133. doi: 10.1016/j.genhosppsych.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leander M, Lampa E, Rask-Andersen A, Franklin K, Gislason T, Oudin A, Svanes C, Torén K, Janson C. Impact of anxiety and depression on respiratory symptoms. Respir Med. 2014;108:1594–1600. doi: 10.1016/j.rmed.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 31.de Marco R, Locatelli F, Sunyer J, Burney P. Differences in incidence of reported asthma related to age in men and women. A retrospective analysis of the data of the European Respiratory Health Survey. Am J Respir Crit Care Med. 2000;162:68–74. doi: 10.1164/ajrccm.162.1.9907008. [DOI] [PubMed] [Google Scholar]
- 32.Sundberg R, Torén K, Franklin KA, Gislason T, Omenaas E, Svanes C, Janson C. Asthma in men and women: treatment adherence, anxiety, and quality of sleep. Respir Med. 2010;104:337–344. doi: 10.1016/j.rmed.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 33.Fernandes L, Fonseca J, Martins S, Delgado L, Pereira AC, Vaz M, Branco G. Association of anxiety with asthma: subjective and objective outcome measures. Psychosomatics. 2010;51:39–46. doi: 10.1016/S0033-3182(10)70657-5. [DOI] [PubMed] [Google Scholar]
- 34.Trzcinska H, Zwierzchowska B, Kozlowski B, Derdowski S, Przybylski G. Analysis of the role of selected demographic and psychological variables (anxiety and depression) as risk factors of inadequate control of bronchial asthma. Ann Agric Environ Med. 2013;20:504–508. [PubMed] [Google Scholar]
- 35.Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- 36.Castrén E, Võikar V, Rantamäki T. Role of neurotrophic factors in depression. Curr Opin Pharmacol. 2007;7:18–21. doi: 10.1016/j.coph.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 37.Lommatzsch M, Braun A, Mannsfeldt A, Botchkarev VA, Botchkareva NV, Paus R, Fischer A, Lewin GR, Renz H. Abundant production of brain-derived neurotrophic factor by adult visceral epithelia. Implications for paracrine and target-derived Neurotrophic functions. Am J Pathol. 1999;155:1183–1193. doi: 10.1016/S0002-9440(10)65221-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Braun A, Lommatzsch M, Mannsfeldt A, Neuhaus-Steinmetz U, Fischer A, Schnoy N, Lewin GR, Renz H. Cellular sources of enhanced brain-derived neurotrophic factor production in a mouse model of allergic inflammation. Am J Respir Cell Mol Biol. 1999;21:537–546. doi: 10.1165/ajrcmb.21.4.3670. [DOI] [PubMed] [Google Scholar]
- 39.Jesenak M, Babusikova E, Evinova A, Banovcin P, Dobrota D. Val66Met polymorphism in the BDNF gene in children with bronchial asthma. Pediatr Pulmonol. 2014;50:631–637. doi: 10.1002/ppul.23065. [DOI] [PubMed] [Google Scholar]
- 40.Szczepankiewicz A, Bręborowicz A, Sobkowiak P, Popiel A. Association of BDNF gene polymorphism with asthma in Polish children. World Allergy Organ J. 2010;3:235–238. doi: 10.1097/WOX.0b013e3181eedb68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zeilinger S, Pinto LA, Nockher WA, Depner M, Klopp N, Illig T, von Mutius E, Renz H, Kabesch M. The effect of BDNF gene variants on asthma in German children. Allergy. 2009;64:1790–1794. doi: 10.1111/j.1398-9995.2009.02131.x. [DOI] [PubMed] [Google Scholar]
- 42.Ilmarinen P, James A, Moilanen E, Pulkkinen V, Daham K, Saarelainen S, Laitinen T, Dahlen SE, Kere J, Dahlen B, Kankaanranta H. Enhanced expression of neuropeptide S (NPS) receptor in eosinophils from severe asthmatics and subjects with total IgE above 100IU/ml. Peptides. 2014;51:100–109. doi: 10.1016/j.peptides.2013.10.030. [DOI] [PubMed] [Google Scholar]
- 43.Xu YL, Gall CM, Jackson VR, Civelli O, Reinscheid RK. Distribution of neuropeptide S receptor mRNA and neurochemical characteristics of neuropeptide S-expressing neurons in the rat brain. J Comp Neurol. 2007;500:84–102. doi: 10.1002/cne.21159. [DOI] [PubMed] [Google Scholar]
- 44.Bernier V, Stocco R, Bogusky MJ, Joyce JG, Parachoniak C, Grenier K, Arget M, Mathieu MC, O'Neill GP, Slipetz D, et al. Structure-function relationships in the neuropeptide S receptor: molecular consequences of the asthma-associated mutation N107I. J Biol Chem. 2006;281:24704–24712. doi: 10.1074/jbc.M603691200. [DOI] [PubMed] [Google Scholar]
- 45.Glotzbach-Schoon E, Andreatta M, Reif A, Ewald H, Tröger C, Baumann C, Deckert J, Mühlberger A, Pauli P. Contextual fear conditioning in virtual reality is affected by 5HTTLPR and NPSR1 polymorphisms: effects on fear-potentiated startle. Front Behav Neurosci. 2013;7:31. doi: 10.3389/fnbeh.2013.00031. [DOI] [PMC free article] [PubMed] [Google Scholar]