Abstract
Purpose/Objectives
To identify situations and thoughts that may precipitate or protect against cancer patients’ loneliness.
Research Approach
Qualitative.
Setting
University outpatient oncology center.
Participants
Purposive sample of 15 patients (47% female) undergoing treatment for multiple myeloma or non-Hodgkin’s lymphoma.
Methodologic Approach
Individual, semi-structured qualitative interviews were conducted. Theoretical thematic analysis was used to analyze interview data.
Findings
Factors that appeared to precipitate loneliness included several situations (e.g., physical isolation, social constraints such as criticism) as well as thoughts (e.g., unmet expectations for visits or questions about their health, beliefs that others do not understand their cancer experience). Factors that appeared to protect against loneliness included several situations (e.g., social support, maintaining a normal routine) as well as thoughts (e.g., beliefs that time alone is desirable and others’ discomfort with cancer-related discussions is normative). Certain social situations were loneliness-inducing for some patients and not others, suggesting that patients’ thoughts about their situations, rather than the situations themselves, have the greatest impact on their loneliness.
Conclusions
The current study fills gaps in loneliness theory by identifying cancer-related situations and thoughts that patients associate with their loneliness. Consistent with theory, patients reported feeling lonely when they had negative thoughts about their social situations.
Interpretation
Findings inform nursing assessment and intervention strategies to incorporate into care plans. For instance, when conducting assessments, nurses should be more attentive to patients’ satisfaction with their social environment than actual characteristics of the environment. Normalizing patients’ experiences and encouraging positive thoughts about others’ behavior may reduce patients’ loneliness.
Knowledge Translation
Patients’ thoughts about their social situations, rather than the situations themselves, appeared to have the greatest impact on loneliness.
Patients with negative explanations for others’ behavior towards them and negative social expectations endorsed loneliness.
Findings point to the potential importance of targeting social cognitions, such as explanations for others’ behavior, in future interventions to reduce cancer patients’ loneliness.
Keywords: loneliness, cancer, qualitative, cognitions, social support, social constraints
Feeling socially connected is a critical aspect of well-being; in the absence of social connection, we experience loneliness. Theorists have defined loneliness as the perception of social isolation and dissatisfaction with the quality of relationships (Cacioppo et al., 2006; Peplau & Perlman, 1982). Loneliness is a known risk factor for a number of poor physical and mental health outcomes in the general population (e.g., Cacioppo & Hawkley, 2009; Hawkley & Cacioppo, 2003), and preliminary research suggests that loneliness is also associated with poor health outcomes in cancer patients (Drageset, Eide, Kirkevold, & Ranhoff, 2013; Jaremka et al., 2014; Jaremka, Fagundes, Glaser, et al., 2013; Nausheen et al., 2010). For instance, higher levels of loneliness have predicted worse immune functioning and greater depressive symptoms, fatigue, pain, and all-cause mortality in cancer patients (e.g., Drageset et al., 2013; Jaremka et al., 2014; Jaremka, Fagundes, Glaser, et al., 2013; Nausheen et al., 2010).
According to a recent meta-analysis, cancer patients experience moderate levels of loneliness on average, and few predictors of their loneliness have been identified (Deckx, van den Akker, & Buntinx, 2014). Specifically, loneliness is more common in unmarried patients and tends to increase as more time elapses since the cancer diagnosis. In addition, social support has consistently shown negative associations with cancer patients’ loneliness (Deckx et al., 2014).
Other social predictors of cancer patients’ loneliness have rarely been examined. One study found that greater social constraints, such as others’ avoidance and discomfort with cancer-related discussions, were associated with more incomplete cognitive processing (i.e., intrusive thoughts about the illness and avoidance of these thoughts) and greater loneliness (Mosher et al., 2012). In turn, more incomplete cognitive processing and greater loneliness were associated with greater psychological distress (Mosher et al., 2012). This finding is consistent with social cognitive processing theory suggesting that constraints on disclosure discourage cognitive processing of stressful events with others and lead people to feel misunderstood and alienated (Lepore & Revenson, 2007).
Although literature on loneliness in cancer patients is growing (Deckx et al., 2014; Wells & Kelly, 2008), little is known about aspects of the cancer experience that patients perceive as loneliness-inducing. In one qualitative study, post-treatment breast cancer patients described their experiences of loneliness, including heightened existential concerns (e.g., fear of death) during and after cancer treatment that others did not appear to understand (Rosedale, 2009). Additionally, patients reported withholding illness-related fears from others in order to protect them, which decreased social connection.
Several gaps in our understanding of cancer patients’ loneliness warrant investigation. First, loneliness is theorized to be sustained by negative social cognitions, such as negative social expectations (Cacioppo & Hawkley, 2009), but little research has examined these cognitions in cancer patients. Second, situational factors contributing to loneliness in cancer patients warrant further study. Specifically, theory suggests that social conditions (e.g., whether people choose to form connections with a lonely individual) impact the persistence of loneliness and negative social cognitions (Cacioppo & Hawkley, 2009), but these conditions have rarely been studied among cancer patients. Third, although greater social support appears to be a protective factor for loneliness in cancer patients (Deckx et al., 2014), other thoughts and situations that protect against patients’ feelings of loneliness have yet to be examined. Identifying experiences and thoughts that lead to loneliness could help nurses address this important problem experienced by cancer patients.
To address these gaps in the literature, the aims of the present study were to identify: (1) cancer-related situations that may precipitate or protect against patients’ loneliness, and (2) thoughts that may precipitate or protect against patients’ loneliness. Qualitative interviews were used to capture the range and complexity of loneliness-related situations and thoughts. Patients undergoing treatment for multiple myeloma or non-Hodgkin’s lymphoma were interviewed, as many receive hematopoietic stem cell transplantation (HSCT), which involves prolonged isolation. In addition, others’ limited understanding of these less prevalent cancers may contribute to patients’ feelings of loneliness.
Methods
Participants and Procedure
Following institutional review board approval, cancer patients were recruited from the hematology/oncology clinic at the Indiana University Simon Cancer Center (IUSCC). Eligible patients were English-speaking adults (≥18 years of age) who were undergoing curative or palliative treatment for multiple myeloma or non-Hodgkin’s lymphoma. Eligibility status was determined by medical chart review and consultation with oncologists. We used purposive sampling (Berg, 2004) based on patient gender and age (≥65 years vs. <65 years) to ensure approximately equal numbers of demographic subgroups.
Following a written consent process, participants first completed a brief demographic questionnaire in clinic. Subsequently, participants completed an audiotaped, semi-structured interview in a private area of the clinic. Interviews ranged from 10 to 30 minutes in length and were conducted by an advanced clinical psychology doctoral student. First, participants were provided with the following definition of loneliness: “loneliness means feeling isolated or disconnected from others around you. It isn’t about how much time you spend with others or how many friends you have, but more about how connected you feel with others overall.” Then participants were asked to describe any experiences of loneliness since their cancer diagnosis. The interviewer probed for any situations precipitating their loneliness and thoughts experienced while feeling lonely. The interviewer also asked for descriptions of situations and thoughts that protected against feelings of loneliness. Throughout the interview, the interviewer asked follow-up questions to obtain a detailed narrative. All participants received a standard brochure outlining available psychosocial services (e.g., social work, support groups) at IUSCC. Patients were given a $25 gift card for their participation. Medical characteristics were collected via medical records.
Data Analysis
Descriptive statistics were used to characterize participants’ demographic and medical information. Interviews were transcribed verbatim and transferred to Atlas.ti for thematic analysis, defined as “a method for identifying, analysing, and reporting patterns (themes) within data” (Braun & Clarke, 2006, p. 6). A theoretical thematic analysis was conducted rather than an inductive one. Specifically, the analysis was guided by loneliness theory (Cacioppo & Hawkley, 2009; Cacioppo et al., 2006; Peplau & Perlman, 1982) such that the analytic goal was to identify situations and thoughts that either precipitated or protected against loneliness. An iterative sampling process was used; thus, two coders (a clinical psychologist and an advanced clinical psychology doctoral student who both specialize in psycho-oncology) generated codes independently and met on a regular basis to discuss them (i.e., after the first 3 interviews and then after every 4 interviews). Discrepancies between coders were discussed and reconciled. Data collection was complete when the coders agreed that saturation had been achieved. Prior research suggests that saturation generally occurs after data from 12 participants have been analyzed (Guest, Bunce, & Johnson, 2006). Next, the researchers categorized the codes into broader themes. The themes were checked to ensure that they were internally consistent and distinguishable from one another.
Findings
Sample
Seventeen patients were approached regarding this study. All were eligible, and 15 agreed to participate in the study (an 88% response rate). Reasons for patient refusal included discomfort being audiotaped and having insufficient time to complete the interview. Participant characteristics are found in Table 1.
Table 1.
Sample Characteristics (N = 15)
| Characteristic | N (%) | M (SD) | Range |
|---|---|---|---|
| Average age | 62.6 (11.9) | 43.0–77.0 | |
| Female gender | 7 (46.7) | ||
| Marital status | |||
| Never married | 2 (13.3) | ||
| Married/living with partner | 10 (66.6) | ||
| Divorced or widowed | 3 (20.0) | ||
| Race/ethnicity | |||
| White | 14 (93.3) | ||
| African American | 1 (6.7) | ||
| Education level | |||
| Some high school | 1 (6.7) | ||
| High school graduate | 4 (26.7) | ||
| Some college or technical school | 3 (20.0) | ||
| College graduate | 7 (46.7) | ||
| Employment status | |||
| Employed full or part-time | 6 (40.0) | ||
| Retired | 6 (40.0) | ||
| Unemployed due to disability | 2 (13.3) | ||
| Student | 1 (6.7) | ||
| Cancer type | |||
| Multiple myeloma | 8 (53.3) | ||
| Non-Hodgkin’s lymphoma | 7 (46.7) | ||
| Cancer stage | |||
| Early stage | 5 (33.3) | ||
| Late stage | 10 (66.7) | ||
| Years since diagnosis | 2.9 (3.2) | 0.2–9.4 | |
| Treatments received | |||
| Chemotherapy | 14 (93.3) | ||
| Autologous stem cell transplant | 7 (46.7) | ||
| Targeted therapy | 6 (40.0) | ||
| Bisphosphonate | 4 (26.7) | ||
| Other surgery | 1 (6.7) | ||
| Radiation | 1 (6.7) |
Note. M = mean; SD = standard deviation.
Situations Associated with Loneliness
Isolation
Several participants said they felt lonely during periods of physical isolation. For example, the lengthy hospitalization phase of HSCT was described as isolating, especially when visits from family and friends were infrequent. One HSCT survivor expressed this perspective:
I was in the hospital for 37 days and there were certain periods when people couldn’t be there…They lived almost 2 hours away…so they couldn’t always come down and…just being in the hospital by oneself is lonely.
Other situations that limited social contact, such as lack of employment and singleness, were also identified as precipitants of loneliness. Many of these situations were attributed to changes in functional status and physical symptoms. One patient noted how her symptom burden resulted in social isolation:
I haven’t been out much in the last year…so I have been kind of isolated at home…before I had the medicine, I…didn’t feel like [going out] much…because I didn’t feel good.
Others’ socially constraining behavior
Another precipitant of loneliness was the socially constraining behavior of family and friends. For example, many participants stated that family and friends acted in a nervous or uncomfortable manner around them, especially when discussing their cancer. As one woman said,
My husband and kids, after hearing about [the cancer], would sometimes feel awkward around me and that would make me feel lonely…kind of left out.
Other socially constraining behaviors of loved ones included criticism or blaming the patient for the cancer diagnosis. Following criticism, participants often avoided sharing their feelings about the cancer with loved ones, which heightened feelings of loneliness. For example, one woman reported avoidance of cancer-related discussions with her husband and feelings of isolation after a hurtful encounter:
After my first [cancer] treatment last month, I was still…weak…and [my husband] just approached me outside and screamed at me that he blamed [me]– it’s 100% my fault I had cancer.
Withholding medical information from others
Some participants did not inform others of their cancer diagnosis or treatment, which led to feelings of isolation. A lack of cancer-related disclosure was often motivated by a desire to protect others from distress, as illustrated by the following statement:
[My husband] gets real depressed, so I…don’t share too much of the information with him…from these scans, year over year, they seem to get worse every time…But I can’t share that with him because he’s going to be really upset if I told him…It’d be better if I did have somebody to share it with…I don’t [think] I can do that.
Thoughts Associated with Loneliness
Others do not visit or ask questions as often as I expect
Many participants had unmet expectations for visits and calls from family and friends, which resulted in feelings of loneliness. Perceiving a lack of care and concern from others during conversations also contributed to loneliness. As one woman stated,
My children haven’t asked me any questions [about the cancer]…they just…change the subject. I don’t know if they just don’t want to talk about it. It does cross my mind, “Why aren’t they asking any questions?”
Others do not understand my cancer-related experiences
Participants reported feeling misunderstood by others during times of loneliness. Specifically, some patients felt that others could not understand various cancer-related experiences, such as the process of undergoing cancer treatment and its physical side effects. One patient who underwent two HSCTs described this experience:
Sometimes you are misunderstood. People don’t know. They don’t understand my cancer…people come up to you and say, “You don’t look sick.” I’ll tell you, only after my second transplant did I really look sick, because…I lost tons of weight. That is a question where you sit there and think, “I don’t know quite what I am supposed to say to that.” Or people who don’t understand the cancer and think you had this transplant and now I’m well. Well, you don’t want to dwell on it and say, “It doesn’t go away. I’m not going to get better.”
My time might be limited
Some participants reported a new awareness of their mortality following their cancer diagnosis. Existential questions such as “Why me?” and “How much longer do I have to live?” led to feelings of disconnection from others who did not face the same challenges. Although this existential awareness increased some patients’ desire to spend time with family and friends, others felt that they did not have time for certain relationships. One man described his withdrawal from others:
I’ve chosen…to be isolated…I have…isolated myself more and more from people I know…It’s almost like I have the feeling that I just don’t have time…to maintain these relationships…Of course, when you’re sixty and you have cancer…your own mortality becomes a significant issue…I just don’t have…time, however long I’ll live…The cancer does play a role, because it becomes a limiting factor…again, the cancer has put an exclamation point on that eventuality, that we’re all going to die, right?…It’s really put an exclamation point on that for me.
Situations Protective Against Loneliness
Social support
The most common protective situations with respect to loneliness were supportive experiences with family and friends, some of whom were cancer survivors. One participant noted the increased support and expressions of care since his diagnosis:
They show such interest, and want to know, “anything I can do to help you?” Anything. They want you to get over this…They’ve changed. Nurturing me and coming to me. And my sister even came closer…I am just really surprised by the whole thing…I thought I was just in my own area, but no, it’s different. I do not feel lonely.
Withholding medical information from others
In contrast to participants who found withholding diagnostic or treatment information from others to be isolating, some participants thought that withholding this information prevented feelings of disconnection or other unwanted changes in their relationships. One woman noted the social advantages of withholding diagnostic information from her friends:
I don’t want to share it [the cancer diagnosis] with people. But my church friends and my friends know I am having a problem. I’ve told them this is not cancerous but I am getting antibiotic treatment - so they don’t know that I’m getting treated for cancer…I want my relationships with everybody to go on as it has…I started worrying if I told them, they would start treating me different and…I want to be treated just like I always have been treated, not any different than anyone else. Is that wrong?…I’m always needed because they don’t know I have cancer.
Maintaining normalcy
A number of participants reported that maintaining a normal routine, including work and social activities, served to distract them from feelings of loneliness. One woman expressed this viewpoint:
My mind feels occupied…and I’m not sitting around being depressed or morbid about things…I never feel alone because I tend to…work on projects.
Thoughts Protective Against Loneliness
Time alone is desirable
Some participants found time alone to be desirable rather than loneliness-inducing. One woman described her acceptance of solitude:
I don’t have a ton of friends. I tend to be very comfortable on my own, and not [feeling] alone. I don’t look at it that way. Just by myself. Doing my own thing…I tend to be very comfortable doing that.
Discomfort with cancer-related discussions is normative
Some participants characterized others’ discomfort with cancer-related discussions and avoidance of these discussions as normative. Rather than inferring that others do not care about them, some participants provided alternative explanations for socially constraining behavior, which appeared to protect against feelings of loneliness. As one woman said,
A lot of people know I have it [cancer]…and they don’t bring it up. They don’t ask about it…I just understand…people feel uncomfortable asking that…Because they don’t understand the medical terms, and they don’t want to make me upset or make me sad. So I think they just don’t know what to say.
Experiences with cancer are common
Participants who characterized cancer as a common experience in their family or social network denied feeling misunderstood by others. Viewing cancer as normative appeared to protect against loneliness, as illustrated by the following statement:
People around me have either experienced cancer or certainly have had friends of theirs who have cancer so I don’t feel left out. Somebody in a different situation could certainly feel that way [lonely]…I think the older you get, frankly, the more you realize a lot of [your] friends have had cancer or [are] going through treatment. So, I don’t feel I have to have a big support system.
I focus on the here and now
A number of participants said that living in the present moment distracted them from negative thoughts and feelings. One man noticed how a focus on daily tasks prevented feelings of loneliness:
I was just taking it one day at a time getting through…But I…didn’t dwell on being alone or being isolated or anything like that…I just didn’t. I couldn’t. I had to focus on what was in front of me which was my illness.
Discussion
This study is among the first to identify thoughts and situations related to cancer patients’ loneliness. Results suggest that thoughts, including attributions for others’ behavior and social expectations, may have a greater impact on patients’ degree of loneliness than their actual social environment (see Figure 1 for a visual representation). Regarding attributions, some patients thought that others’ avoidance of cancer-related discussions showed a lack of compassion, whereas other patients made more positive attributions (e.g., others were protecting them from distressing conversations). Patients reporting positive attributions tended to feel less lonely under those circumstances. Regarding social expectations, some patients felt that others could never understand their experiences with cancer, whereas other patients believed their cancer experiences to be common and therefore understood by many people. Patients who felt understood by others also reported feeling less isolated from their social network. Thus, patients’ interpretation of events appeared to impact their loneliness, consistent with theory linking negative social cognitions to greater loneliness (Cacioppo & Hawkley, 2009). In addition, findings fill gaps in existing theory by suggesting specific cancer-related thoughts that may lead to more negative social interactions and isolation and, in turn, sustain feelings of loneliness.
Figure 1.
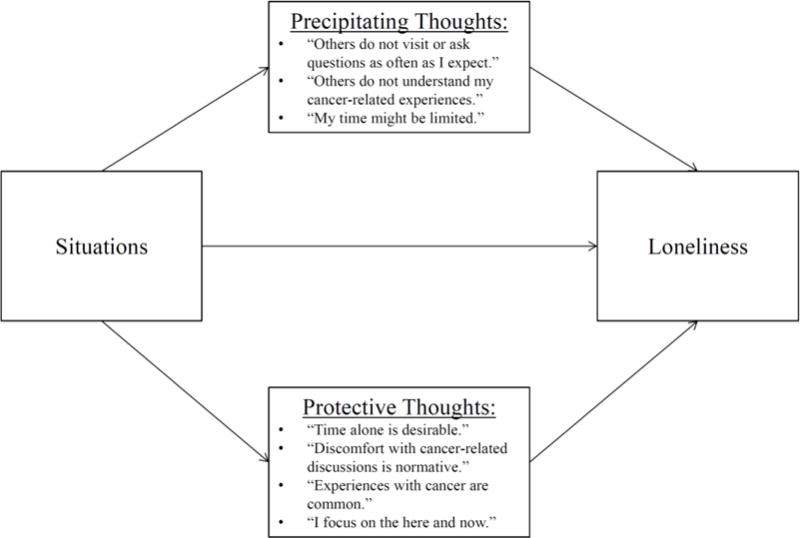
Conceptual model of cancer patients’ loneliness
Existential thoughts also appeared to contribute to cancer patients’ loneliness. Specifically, some patients said they felt alone in their newfound awareness of their mortality and unpredictable future. These findings are comparable to those of a qualitative study of post-treatment breast cancer patients (Rosedale, 2009) and suggest that some patients undergoing treatment for primarily late-stage cancers experience similar feelings. Furthermore, a novel finding of the current study was that thoughts about mortality may contribute to loneliness by decreasing interest in maintaining relationships. Specifically, some patients prioritized other activities over certain relationships when they perceived their time as limited, which led to feelings of isolation.
Situational precipitants of loneliness also were explored. First, we found that physical isolation led to heightened loneliness for some patients, whereas others enjoyed time to themselves to focus on tasks. This finding is consistent with loneliness theory suggesting that the perception of social isolation underlies loneliness rather than actual isolation (Cacioppo et al., 2006; Peplau & Perlman, 1982). This result also may be understood within a cognitive theoretical framework for depression, which posits that people’s interpretations of their environment impact their mood (Beck, 2011). Also consistent with theory (Lepore, 2001; Lepore & Revenson, 2007), patients who felt supported by others did not endorse loneliness, whereas those experiencing social constraints (e.g., criticism, avoidance) often reported loneliness. These findings converge with meta-analytic evidence supporting a negative relationship between social support and loneliness in cancer patients (Deckx et al., 2014) as well as results of one quantitative study of HSCT survivors indicating a positive relationship between social constraints and loneliness (Mosher et al., 2012). Further research is needed to understand the social factors that have the greatest impact on cancer patients’ loneliness. For example, examining the relative influence of positive versus negative social exchanges with close others on loneliness may contribute to theory and intervention development.
An interesting social factor that warrants further study in relation to loneliness is cancer patients’ degree of illness-related disclosure. In the current study, patients who refrained from disclosing information about their diagnosis and treatments to family or friends did not invariably report feeling lonely. In fact, some patients said that this decision prevented unwanted relationship changes, such as being treated differently. Conversely, some patients felt disconnected from others when they failed to discuss cancer-related concerns. Both findings may be understood within the framework of social cognitive processing theory (Lepore, 2001). Unwanted relationship changes, such as avoidance, criticism, and discomfort during conversations, may be avoided if patients do not disclose their cancer diagnosis. By avoiding others’ socially constraining behaviors, patients may experience less distress and loneliness. However, non-disclosing patients do not have the opportunity to process cancer-related information with others, which has been found to facilitate psychological adjustment (Lepore & Helgeson, 1998; Manne et al., 2004; Mosher et al., 2012). Overall, findings suggest that cognitive and situational precipitants of loneliness vary substantially across individuals. Thus, future research should examine moderators of the impact of cognitive and contextual variables on loneliness, including demographic (e.g., gender, age), medical, and personality characteristics (e.g., introversion) and level of psychopathology.
Limitations
Limitations of this study should be noted. Although the sample was diverse with respect to a number of demographic factors, participants were primarily Caucasian patients from one institution in the Midwest. Exploring precipitants of loneliness in diverse cultural groups is an important direction for future research. In addition, loneliness has been found to be greater at some points in the cancer trajectory than others (Deckx et al., 2014), and retrospective reporting may not fully capture these changes in loneliness and its precipitants. Furthermore, interviews were relatively brief because they were completed in a busy clinic setting. Longitudinal data collection using in-depth interviews would allow us to gather more detailed information about loneliness experiences over different phases of the disease trajectory.
Implications for Future Research
Findings point to the potential importance of targeting social cognitions, such as attributions for others’ behavior, in future interventions to reduce cancer patients’ loneliness. To date, the limited intervention research to address cancer patients’ loneliness has not adopted this approach (Fukui, Koike, Ooba, & Uchitomi, 2003; Masi, Chen, Hawkley, & Cacioppo, 2010). Cognitive therapy, which involves teaching patients to challenge and replace negative thoughts, has reduced loneliness in non-cancer populations (Hopps, Pépin, & Boisvert, 2003; Tatlilioğlu, 2013; Theeke & Mallow, 2015), but this approach has yet to be tailored to cancer patients’ loneliness experiences.
Another finding with implications for intervention is that patients felt less isolated when they focused on the present moment. If further research supports this finding, therapeutic techniques that foster attention to the present moment (i.e., mindfulness approaches) may also reduce cancer patients’ loneliness. In fact, one study found that a mindfulness-based therapy approach reduced healthy older adults’ loneliness (Creswell et al., 2012). Both mindfulness interventions and cognitive therapy have led to better mental health outcomes in cancer patients (Shennan, Payne, & Fenlon, 2011; Tatrow & Montgomery, 2006), but additional research is needed to examine whether these interventions may be modified to reduce cancer patients’ loneliness.
Implications for Nursing Practice
Results of this study have implications for loneliness assessment and intervention strategies that nurses should consider when developing cancer patients’ care plans. First, results suggest that nurses should be most attentive to patients’ satisfaction with their social environment rather than the quantity of social support when conducting assessments, as this may have the greatest impact on loneliness. Second, nurses can teach patients skills for communicating with providers or family members and refer them to available support services. Third, nurses may reduce patients’ loneliness by normalizing their experiences, as lonely patients in this study often reported feeling misunderstood. Fourth, nurses may help patients generate alternate explanations for others’ behaviors that are less loneliness-inducing. For instance, if friends rarely call a patient, he or she may attribute this behavior to a lack of caring, whereas an alternate explanation is that friends are worried about disturbing the patient’s sleep. Thus, through assessment, intervention, and referral, nurses may play a key role in reducing cancer patients’ loneliness.
Conclusions
Loneliness is a significant risk factor for poor mental and physical health outcomes in cancer patients (Drageset et al., 2013; Jaremka et al., 2014; Jaremka, Fagundes, Peng, et al., 2013; Nausheen et al., 2010), yet little is known about factors contributing to cancer patients’ loneliness experiences. The current study identified situations and thoughts that might precipitate or protect against cancer patients’ loneliness. In general, patients’ perceptions of their social situations, rather than the situations themselves, appeared to have the greatest impact on their loneliness, supporting the theoretical notion that negative cognitions sustain loneliness (Cacioppo & Hawkley, 2009). If cognitions identified in the current research are found to predict cancer patients’ loneliness in future studies, then interventions may be developed to address these cognitions and ultimately improve the health and well-being of cancer patients.
Acknowledgments
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number K05CA175048. Rebecca Adams’s work was supported by R25CA117865 (V. Champion, PI) from the National Cancer Institute. Catherine Mosher’s work was supported by K07CA168883 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Contributor Information
Rebecca N. Adams, Doctoral student in the Department of Psychology at Indiana University-Purdue University Indianapolis
Catherine E. Mosher, Assistant Professor in the Department of Psychology at Indiana University-Purdue University Indianapolis
Rafat Abonour, Professor of Medicine at the Indiana University School of Medicine, Indianapolis, IN
Michael J. Robertson, Professor of Medicine at the Indiana University School of Medicine, Indianapolis, IN
Victoria L. Champion, Mary Margaret Walther Distinguished Professor at the Indiana University School of Nursing, Indianapolis, IN
Kurt Kroenke, Professor of Medicine at the Indiana University School of Medicine, Indianapolis, IN Research Scientist at the Regenstrief Institute, Inc. and the VA HSR&D Center for Health Information and Communication, Indianapolis, IN.
References
- Beck J. Cognitive behavior therapy: Basics and beyond. 2nd. Guilford Press; 2011. [Google Scholar]
- Berg BL. Qualitative research methods for the social sciences. Vol. 5. Boston: Pearson; 2004. [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Research in Psychology. 2006;3:77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends in Cognitive Sciences. 2009;13:447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, Spiegel D. Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality. 2006;40:1054–1085. doi: 10.1016/j.jrp.2005.11.007. [DOI] [Google Scholar]
- Creswell JD, Irwin MR, Burklund LJ, Lieberman MD, Arevalo JM, Ma J, Cole SW. Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: A small randomized controlled trial. Brain, Behavior, and Immunity. 2012;26:1095–1101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deckx L, van den Akker M, Buntinx F. Risk factors for loneliness in patients with cancer: A systematic literature review and meta-analysis. European Journal of Oncology Nursing. 2014;18:466–477. doi: 10.1016/j.ejon.2014.05.002. [DOI] [PubMed] [Google Scholar]
- Drageset J, Eide GE, Kirkevold M, Ranhoff AH. Emotional loneliness is associated with mortality among mentally intact nursing home residents with and without cancer: A five-year follow-up study. Journal of Clinical Nursing. 2013;22:106–114. doi: 10.1111/j.1365-2702.2012.04209.x. [DOI] [PubMed] [Google Scholar]
- Fukui S, Koike M, Ooba A, Uchitomi Y. The effect of a psychosocial group intervention on loneliness and social support for Japanese women with primary breast cancer. Oncology Nursing Forum. 2003;30:823–830. doi: 10.1188/03.ONF.823-830. [DOI] [PubMed] [Google Scholar]
- Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18:59–82. doi: 10.1177/1525822X05279903. [DOI] [Google Scholar]
- Hawkley LC, Cacioppo JT. Loneliness and pathways to disease. Brain, Behavior, and Immunity. 2003;17:98–105. doi: 10.1016/S0889-1591(02)00073-9. [DOI] [PubMed] [Google Scholar]
- Hopps SL, Pépin M, Boisvert JM. The effectiveness of cognitive-behavioral group therapy for loneliness via inter relaychat among people with physical disabilities. Psychotherapy: Theory, Research, Practice, Training. 2003;40:136–147. doi: 10.1037/0033-3204.40.1/2.136. [DOI] [Google Scholar]
- Jaremka LM, Andridge RR, Fagundes CP, Alfano CM, Povoski SP, Lipari AM, Yee LD. Pain, depression, and fatigue: Loneliness as a longitudinal risk factor. Health Psychology. 2014;33:948–957. doi: 10.1037/a0034012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaremka LM, Fagundes CP, Glaser R, Bennett JM, Malarkey WB, Kiecolt-Glaser JK. Loneliness predicts pain, depression, and fatigue: Understanding the role of immune dysregulation. Psychoneuroendocrinology. 2013;38:1310–1317. doi: 10.1016/j.psyneuen.2012.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaremka LM, Fagundes CP, Peng J, Bennett JM, Glaser R, Malarkey WB, Kiecolt-Glaser JK. Loneliness promotes inflammation during acute stress. Psychological Science. 2013;24:1089–1097. doi: 10.1177/0956797612464059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lepore S. A social–cognitive processing model of emotional adjustment to cancer. In: Baum A, Andersen BL, editors. Psychosocial interventions for cancer. Washington, DC: American Psychological Association; 2001. pp. 99–118. [Google Scholar]
- Lepore S, Helgeson V. Social constraints, intrusive thoughts, and mental health after prostate cancer. Journal of Social and Clinical Psychology. 1998;17:89–106. doi: 10.1521/jscp.1998.17.1.89. [DOI] [Google Scholar]
- Lepore S, Revenson T. Social constraints on disclosure and adjustment to cancer. Social and Personality Psychology Compass. 2007;1:313–333. doi: 10.1111/j.1751-9004.2007.00013.x. [DOI] [Google Scholar]
- Manne S, Sherman M, Ross S, Ostroff J, Heyman RE, Fox K. Couples’ support-related communication, psychological distress, and relationship satisfaction among women with early stage breast cancer. Journal of Consulting and Clinical Psychology. 2004;72:660–670. doi: 10.1037/0022-006X.72.4.660. [DOI] [PubMed] [Google Scholar]
- Masi CM, Chen H-Y, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Personality and Social Psychology Review. 2010;15:219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosher CE, Lepore S, Wu L, Austin J, Valdimarsdottir H, Rowley S, Rini C. Social correlates of distress following hematopoietic stem cell transplantation: Exploring the role of loneliness and cognitive processing. Journal of Health Psychology. 2012;17:1022–1032. doi: 10.1177/1359105311432490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nausheen B, Carr NJ, Peveler RC, Moss-Morris R, Verrill C, Robbins E, Gidron Y. Relationship between loneliness and proangiogenic cytokines in newly diagnosed tumors of colon and rectum. Psychosomatic Medicine. 2010;72:912–916. doi: 10.1097/PSY.0b013e3181f0bc1c. [DOI] [PubMed] [Google Scholar]
- Peplau LA, Perlman D. Perspectives on loneliness. In: Peplau LA, Perlman D, editors. Loneliness: A sourcebook of current theory, research and therapy. New York: Wiley-Interscience; 1982. pp. 1–18. [Google Scholar]
- Rosedale M. Survivor loneliness of women following breast cancer. Oncology Nursing Forum. 2009;36:175–183. doi: 10.1188/09.ONF.175-183. [DOI] [PubMed] [Google Scholar]
- Shennan C, Payne S, Fenlon D. What is the evidence for the use of mindfulness-based interventions in cancer care? A review. Psycho-Oncology. 2011;20:681–697. doi: 10.1002/pon.1819. [DOI] [PubMed] [Google Scholar]
- Tatlilioğlu K. The effect of cognitive behavioral oriented psycho education program on dealing with loneliness: An online psychological counseling approach. Education. 2013;134:101–109. [Google Scholar]
- Tatrow K, Montgomery GH. Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: A meta-analysis. Journal of Behavioral Medicine. 2006;29:17–27. doi: 10.1007/s10865-005-9036-1. [DOI] [PubMed] [Google Scholar]
- Theeke LA, Mallow JA. The development of LISTEN: A novel intervention for loneliness. Open Journal of Nursing. 2015;5:136–143. doi: 10.4236/ojn.2015.52016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells M, Kelly D. The loneliness of cancer. European Journal of Oncology Nursing. 2008;12:410–411. doi: 10.1016/j.ejon.2008.11.003. [DOI] [PubMed] [Google Scholar]


