Summary
Dietary interventions have not been effective in the treatment of multiple sclerosis (MS). Here we show that periodic 3 day cycles of a fasting mimicking diet (FMD) are effective in ameliorating demyelination and symptoms in a murine experimental autoimmune encephalomyelitis (EAE) model. The FMD reduced clinical severity in all mice, and completely reversed symptoms in 20% of the animals. These improvements were associated with increased corticosterone levels and Treg cell number, reduced levels of pro-inflammatory cytokines, TH1 and TH17 cells, and antigen presenting cells (APCs). Moreover, the FMD promoted oligodendrocyte precursor cell regeneration and remyelination in axons in response to both EAE and cuprizone MS models, supporting its effects on both suppression of autoimmunity and remyelination. We also report preliminary data suggesting that a FMD or a chronic ketogenic diet are safe, feasible and potentially effective in the treatment of relapsing remitting multiple sclerosis (RRMS) patients (NCT01538355).
Introduction
Multiple sclerosis (MS) is an autoimmune disorder characterized by T cell-mediated demyelination and neurodegeneration in the central nervous system (CNS) (Friese and Fugger, 2005; Pender and Greer, 2007; Rasmussen et al., 2007; Sospedra and Martin, 2005). In experimental autoimmune encephalomyelitis (EAE), an animal model for MS, activated myelin-specific TH1 and TH17 cells cross the blood brain barrier and migrate into the CNS, where they are activated by local antigen presenting cells (APCs) and promote inflammation (Dhib-Jalbut, 2007; Fletcher et al., 2010; Goverman, 2009; Hemmer et al., 2002). This inflammatory process leads to oligodendrocyte death, demyelination and axonal damage, which eventually cause neurological damage (Lucchinetti et al., 1999; Raine and Wu, 1993). Although oligodendrocyte precursor cells (OPCs) can migrate to the sites of MS lesions, they often fail to differentiate into functional oligodendrocytes (Chang et al., 2002; Wolswijk, 1998). Several MS treatment drugs have been effective in reducing immune responses, but their impact on long-term disease progression, accrual of irreversible neurological disability, and the function of the immune system remains largely unclear, underlining the need for novel therapeutic strategies (Wingerchuk and Carter, 2014). Therefore, effective treatments for MS may require not only the mitigation of autoimmunity, but also the stimulation of oligodendrocyte regeneration and the restoration of a functional myelin sheath. Periodic cycles of prolonged fasting (PF) or of a fasting mimicking diet (FMD) lasting 2 or more days can increase protection of multiple systems against a variety of chemotherapy drugs in mice and possibly humans. Moreover, PF or FMD reverse the immunosuppression or immunosenescence of either chemotherapy or aging through hematopoietic stem cell-based regeneration (Brandhorst et al., 2015; Cheng et al., 2014; Fontana et al., 2010; Guevara-Aguirre et al., 2011; Lee et al., 2010; Longo and Mattson, 2014). Chronic caloric restriction, a ketogenic diet (KD), and intermittent fasting have been shown to prevent EAE by reducing inflammation and enhance neuroprotection when administered prior to disease induction or signs (Esquifino et al., 2007; Kafami et al., 2010; Kim do et al., 2012; Piccio et al., 2008) but dietary interventions have not been reported as a therapy for EAE or MS or to promote myelin regeneration.
Here we report on the effects of low calorie and low protein FMD cycles as a treatment of MS mouse models, and investigate the mechanisms involved. Furthermore, we report preliminary results on the safety and feasibility of a FMD and a KD in patients with relapsing-remitting MS (RRMS).
Results
The FMD cycles reduce disease severity in the MOG35-55-induced EAE model
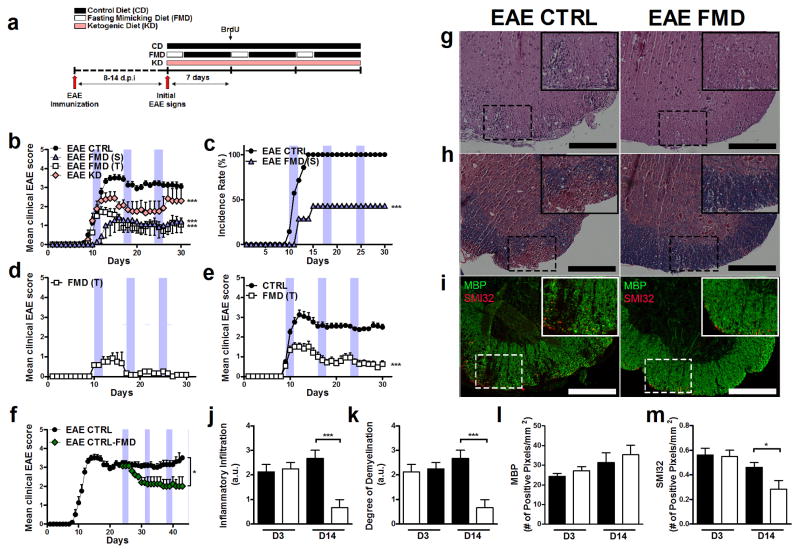
We examined the effects of periodic cycles of a very low calorie and low protein fasting mimicking diet (FMD) lasting 3 days every 7 days (3 cycles) or a ketogenic diet (KD) continued throughout the 30 days on EAE model induced with active immunization with myelin oligodendrocyte glycoprotein 35-55 (MOG35-55) (Fig. 1a). Groups of mice were treated both semi-therapeutically -EAE FMD (S); in which FMD treatment started after 10% of the immunized population showed EAE signs- or therapeutically -EAE FMD (T), in which FMD treatment started after all of the immunized population showed EAE signs. FMD and KD treatment decreased the disease severity compared to the control (Fig. 1b); however, the FMD reduced the mean severity score to approximately 1, whereas the KD group reduced the severity score to approximately 2 at the later stages (Fig. 1b). In the EAE FMD (S) group, FMD treatment not only delayed the onset of disease but also lowered the incidence rate (100% vs. 45.6%; Fig. 1c). In the EAE FMD (T) group, FMD cycles completely reversed the severity score to 0 in 21.7% of the cohort (no observable signs; Fig. 1d), and reduced the severity score to below 0.5 in over 50% of the mice (12 out of 23 mice; Fig. 1e). To address whether the FMD cycles also have beneficial effects on the chronic EAE models that have established disease, we initiated FMD treatment two weeks after initial EAE signs (EAE CTRL-FMD). Prior to the treatment, both the EAE CTRL and EAE CTRL-FMD cohorts had similar severity scores (3.19 ± 0.52 vs. 3.30 ± 0.27; Day 24). After three FMD cycles, we observed a significant reduction of severity score in the EAE CTRL-FMD cohort compared to the EAE CTRL cohort (3.3 ± 0.57 vs. 2.1 ± 0.89; Day 42; p < 0.05; Fig. 1f). As infiltration of immune cells and demyelination are histopathological hallmarks of EAE and MS, spinal cord sections were stained with hematoxylin and eosin to visualize infiltrating immune cells (H&E; Fig. 1g) or solochrome cyanine to visualize myelin (Fig. 1 h). To assess demyelination and axonal damage, immunohistochemistry was performed using antibodies against myelin basic protein (MBP) or dephosphorylated neurofilaments (SMI-32; Fig. 1i). At D3, the level of infiltrating immune cells and demyelination were similar in the EAE CTRL and EAE FMD groups (Fig. 1j; Supplemental Fig. 1h). At D14, sections of EAE CTRL mice displayed severe immune cell infiltration corresponding with demyelinated lesions, reduced MBP expression and increased SMI-32 expression (Fig. 1j–m). By contrast, sections of EAE FMD mice at D14 displayed significantly reduced immune cell infiltration and demyelination (Fig. 1j–m). Although MBP staining showed no significant difference between EAE CTRL and EAE FMD at D14 (Fig. 1l), neurofilament dephosphorylation in the EAE FMD mice was reduced compared to the EAE CTRL group (Fig. 1m). Overall, these results suggest that FMD cycles reduce EAE disease severity in part by reducing inflammation, and preventing demyelination and axonal damage.
Figure 1. FMD cycles decrease disease severity of the MOG35-55-induced EAE model.
(mean ± S.E.M, * p < 0.05, ** p<0.01; *** p < 0.001; t test, 1-way or 2-way ANOVA & Bonferroni Post Test; Scale bar represents 200 μm).
a. Diagram displaying the time course of the immunization and the diet interventions.
b. The EAE severity scoresof the Control Diet (EAE CTRL; n=23), ketogenic diet (EAE KD); n=13, semi-therapeutic FMD cycles (EAE FMD(S); n=7) or therapeutic FMD cycles (FMD(T); n = 23).
c. Incidence rate of the EAE CTRL and EAE FMD (S) (n=7–23).
d. EAE severity score of the EAE FMD(T) mice that completely reversed the EAE severity and scored 0, no observable disease (n=5).
e. EAE severity score of the best-performing control mice (n=12) and the FMD(T) mice (n=12).
f. EAE severity score of the EAE CTRL mice that treated with FMD upon chronic EAE development(EAE CTRL-FMD) (n=6).
g–m. Spinal cord of the EAE CTRL and the EAE FMD (T) mice with quantification of (g) H&E staining, (h) solochrome cyanine staining, and (i) MBP (Myelin Basic Protein) and SMI32 staining of spinal cord sections isolated at day 14.
The FMD cycles reduce infiltration of immune cells in the spinal cord
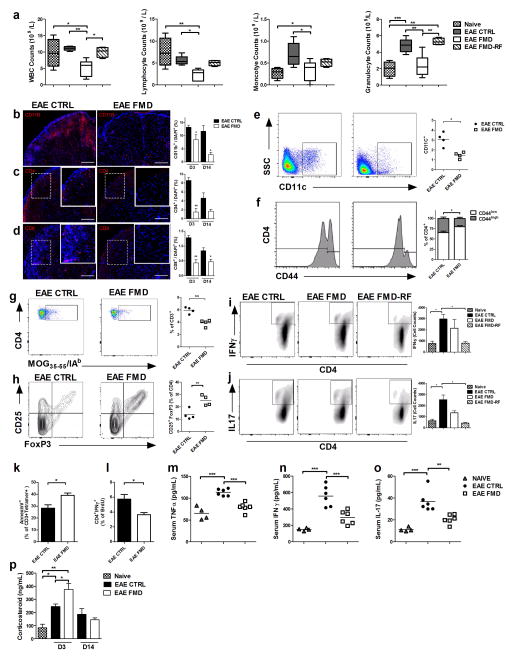
To investigate the capacity of FMD cycles to reduce potential autoimmune T-cells, we measured circulating white blood cells (WBCs), lymphocytes, monocytes and granulocytes of the naive, EAE CTRL, EAE FMD and EAE FMD:RF (measured 4 days after returning to a standard ad lib diet) groups after 3 cycles of the FMD regimen (Fig. 2a). The FMD resulted in a temporary 40–50% reduction in total WBCs, lymphocytes, monocytes and granulocytes. Upon returning to the standard ad lib diet (EAE FMD:RF), all CBC counts returned to either naive level or lower levels than those observed in the EAE CTRL with exception of granulocytes, indicating that the FMD cycles cause both white blood cell death and regeneration (Fig. 2a). Next, we measured the inflammatory markers associated with EAE pathophysiology. D3 and D14 spinal cord sections of the EAE CTRL were extensively populated with CD11b+ cells (Fig. 2b). However, at D14, the EAE FMD mice displayed a 75% reduction (p< 0.05) in spinal cord-associated CD11b+ cells compared to mice on the control diet (11.7% vs. 2.8%; Fig. 2b). Since the myelin-specific effector T cells migrate into the CNS and initiate demyelination, we investigated the accumulation of CD4+ or CD8+ T cells in the spinal cord. A large number of CD4+ T cells was detected in the white matter of the spinal cord from the control diet cohort (Fig. 2c). In contrast, the FMD treated cohort displayed an over 4-fold reduction (p< 0.01) in CD4+ T cells at D3 (8.6% vs. 1.5%; Fig. 2c) compared to the control diet cohort, which remained lower even at D14. The FMD group also had reduced CD8+ T cells (D3: 1.3% vs. 0.4%; p<0.01; Fig. 2d) compared to the control diet group. To investigate whether the FMD affects APCs, we isolated splenocytes from EAE CTRL and EAE FMD mice at D3, stained them for CD11c and F4/80 and characterized them by flow cytometry. We observed a significant decrease (p< 0.05) in CD11c+ dendritic cells in the EAE FMD cohort compared to the EAE CTRL cohort (3.08±0.70% vs. 1.46±0.31%), but did not observe any changes in the number of F4/80+ macrophage cells in the control or the FMD treated groups (Fig. 2e; Supplemental Fig. 2b). To determine the effects of the FMD treatment on T cell infiltration in the spinal cord, we measured T-cell activation levels. The number of CD4+ T cells and CD8+ T cells in the EAE CTRL and EAE FMD mice was similar (Supplemental Fig. 2c–d), but the ratio of splenic naive (CD44low) to activated (CD44High) CD4+ T cells was increased (p< 0.05) in the FMD group compared to the control group (1.95 vs. 3.67; Fig. 2f). No difference in CD8+ T cells was observed (Supplemental Fig. 2e). Moreover, the total number of effector (CD44High and CD62Llow) T cells was reduced in the FMD compared to the control group, but the ratio of effector (CD44High and CD62Llow) to memory T (CD44High and CD62LHigh) cells did not change (Supplemental Fig.2f–h). These results indicate that FMD cycles decrease dendritic cells and increases the relative number of naïve T cells which may explain the reduced autoimmunity caused by the FMD.
Figure 2. FMD cycles decrease the number of infiltrating T cells in the Spinal Cord.
(n=4–8 / group; mean ± S.E.M, * p < 0.05, ** p<0.01; *** p < 0.001; t test, 1-way ANOVA & Bonferroni Post Test; Scale bar represents 200 μm).
a. Total white blood cells (WBC), lymphocytes, monocytes and granulocyte counts of the naïve, EAE-CTRL, EAE-FMD, and after 3 days of the re-feeding (EAE-FMD: RF) mice after 3 cycles of the FMD and matched time point for the EAE-CTRL.
b–d. Spinal cord sections (D14) and quantification at D3 and D14 post the first EAE sign for (b)CD11b+, (c) CD4+, and (d) CD8+ (at least 6 sections / mouse).
e. CD11c+ isolated from the EAE CTRL or EAE FMD mice on D3 and the quantification of cells from the total isolated splenocyte.
f. CD4+ gated for CD44L or CD44H isolated from the EAE CTRL or EAE FMD and quantification of % splenocyte of CD4+ CD44L (Inactive) or CD4+ CD44H (Active) cells.
g. CD3+ lymphocytes gated for CD4 and MOG35-55/IAb from EAE CTRL or EAE FMD and quantification of the MOG specific CD4+ cells.
h. CD4+ CD25+ FoxP3+ isolated from EAE CTRL or EAE FMD and the quantification of CD25+ FoxP3+ of CD4+ cells.
i–j. Intracellular staining for either IFNγ (i) or IL17(j) after gated for CD4+ of the naïve, EAE CTRL, EAE FMD, EAE FMD:RF and quantification of cell counts.
k. Quantification of Annex in V+ apoptotic CD3+ MOG35-55/IAb cells.
l. Quantification of CD4+IFNγ+ of BrdU+ lymphocytes.
m–o. Serum (m)TNFα, (n)IFNγ, and (o)IL-17 level (pg/mL) of the naive, EAE CTRL and EAE FMD mice on D3 post first sign of EAE.
p. Serum corticosterone level (ng/mL) of before immunization, at the time of the symptom, 3 or 14 days after initial symptom of the control or FMD.
The FMD cycles induce autoreactive lymphocytes apoptosis and increase the number of naive cells
To determine whether FMD cycles also reduce the MOG-specific antigen reactive cells, we used a MHC Tetramer (MOG35-55 /IAb) to identify antigen-reactive cells after a FMD cycle in vivo. CD4+ MOG35-55 /IAb + cells were reduced in the EAE FMD cohort compared to the EAE CTRL cohort (5.75 ± 0.51 % vs. 3.83 ± 0.66 % of lymphocytes; * p < 0.05; Fig. 2g). To determine whether the reduced active T-cells numbers are due to an increase in the number of regulatory T cells (Treg), we isolated lymphocytes from draining lymph nodes and spleens of the EAE CTRL or EAE FMD mice and analyzed for CD4+ CD25+ FoxP3+ Treg cells. The FMD cohort resulted in a two-fold increase (p<0.01) in CD25+ FoxP3+ expressing Treg cells (13.6±4.2 % vs. 25.1±4.2%; Fig. 2h). Moreover, the FMD cohort resulted in a 27.8% reduction (p<0.05) in IFN-γ expressing TH1 cells (2974.4±708.0 vs. 2148.1±1396.1; Fig. 2i) and a 46.5% reduction (p<0.05) in IL-17 expressing TH17 cells (2535.9±722.0 vs. 1357.1±256.2; Fig. 2j), both known to be central mediators of EAE. Interestingly, upon re-feeding of the control diet, the EAE FMD treatment group (EAE FMD: RF) showed a 72.9% reduction (p< 0.05) in IFN-γ expressing TH1 cells (2974.4±708.0 vs. 805.8±251.5; Fig. 2i) and 82.9% reduction (p< 0.05) in IL-17 expressing TH17 cells (2535.9±722.0 vs. 432.4±117.4; Fig. 2j), suggesting that the FMD can prevent autoimmunity in part by reducing the levels of pro-inflammatory T cells implicated in EAE.
In order to assess how the FMD cycles may reduce the number of T cells, we measured apoptosis in MOG-specific T cells (CD3+MOG35-55/IAb) in vivo. We observed a significant increase (p < 0.05) in apoptotic CD3+ MOG35-55/IAb level in the EAE FMD cohort compared to the EAE CTRL cohort (28.3 ± 4.94 % vs. 39.1 ± 4.79 %; Fig. 2k), which was consistent with the major reduction in the number of white blood cell and lymphocytes in the FMD group (Fig. 2a). To investigate whether these apoptotic cells are replaced by newly generated cells, we treated the mice with BrdU during the re-feeding period (4 injections within 48 hours, 1 mg of BrdU/injection). Splenocytes were isolated 4 days after the re-feeding of the regular diet, and stained for BrdU (Supplemental Fig. 2i). We observed no difference in levels of total BrdU+ lymphocytes (8.11 ± 1.99% vs. 12.02 ± 2.72%; Supplemental Fig. 2j), but a significantly reduced proliferation of TH1 (BrdU+ CD4+IFNγ+) (5.74 ± 1.07% vs. 3.65 ± 0.63 %; * p < 0.05; Fig. 2l), and no difference in proliferation of TH17 (BrdU+CD4+IL17+) (4.71 ± 1.53% vs. 5.01 ± 1.66 %; Supplemental Fig. 2k). Taken together, these data indicate that FMD cycles may promote apoptosis of the autoreactive T cells, leading to an increase in the proportion of naïve T cells and regulatory T cells. In addition, FMD cycles may interfere with proliferation and differentiation of TH1 cells but not TH17 cells. To investigate whether the FMD effects on CNS infiltrating immune cells are associated with suppression of TH1- and TH17-dependent cytokine production (IL-17, IFNγ, and TNF-α), we analyzed serum from the naive, EAE CTRL and EAE FMD mice (Fig. 2k–m). We observed a significant reductions in serum TNF-α (113.3±7.9 vs. 79.3±10.5 pg/mL; p<0.001; Fig. 2m), IFNγ (558.43±124.5 vs. 296.0±83.4 pg/mL; p<0.001; Fig. 2n), and IL-17 (36.8±9.67 vs. 20.75±4.2 pg/mL; p<0.01; Fig. 2o). To identify a potential mediator for the effects of FMD cycles on the suppression of autoimmune responses, we measured serum corticosterone. Corticosterone is a glucocorticoid hormone with broad anti-inflammatory and immunosuppressive effects affecting leukocyte distribution, trafficking, and death (Ashwell et al., 2000; Herold et al., 2006; Planey and Litwack, 2000; Vegiopoulos and Herzig, 2007). Serum corticosterone levels were elevated in association with the first EAE signs (EAE Day1; before the treatment). The FMD treatment caused a further increase in corticosterone levels at D3 compared to those in controls (245.9±38.8 vs. 375.0±94.1 ng/mL; p < 0.01), which returned to EAE basal levels by D14 in both groups (Fig. 2p). These results indicate that the FMD cycles reduce TH1 and TH17 effector cells and the production of pro-inflammatory cytokines. These effects of the FMD may be regulated in part by the temporary elevation of corticosterone levels, dampening of T cell activation, and reduced APCs and T cell infiltration in the spinal cord.
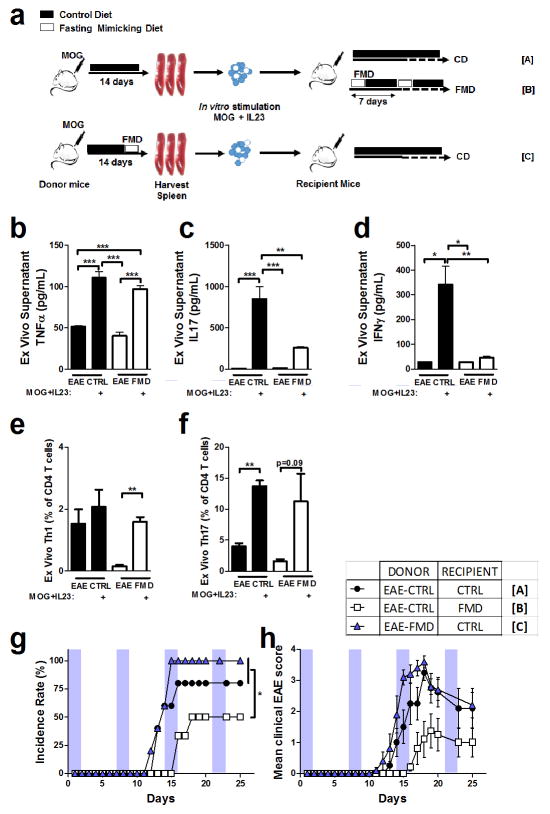
FMD reverses EAE symptoms by reducing the levels/reactivity of established autoimmune cells
To determine how FMD affects the initiation of EAE, splenocytes were isolated from EAE CTRL and EAE FMD, re-activated with MOG35-55 peptide and IL-23 ex-vivo and transferred into naïve recipient mice to induce EAE. Then the mice were subjected to either the control diet or FMD cycles (Fig. 3a). The supernatant from ex-vivo splenocyte cultures derived from the EAE FMD showed no difference in TNFα level (110.8±14.9 pg/mL vs. 97.1±8.4 pg/mL; Fig. 3b) but showed a major reduction (p< 0.01) in IFNγ (342.0±29.8 pg/mL vs. 46.6±16.6 pg/mL Fig. 3c) and IL-17 (850.5±442.0 pg/mL vs. 257.4±36.4 pg/mL; Fig. 3d). Interestingly, upon in vitro reactivation, both EAE CTRL and EAE FMD had similar levels of TH1 and TH17 differentiated cells (Fig. 3e–f). To determine whether the immune cells from EAE CTRL and EAE FMD mice have similar encephalitogenic effects, we transferred splenocytes from either donor group (EAE CTRL or EAE FMD) into naive recipients -[A; EAE CTRL donor to control diet recipient] and [C; EAE FMD donor to control diet recipient]. This resulted in a similar disease incidence rate (Fig. 3g), and an equally severe EAE disease severity by day 20 (2.38±0.48 vs. 2.70±0.75; Fig. 3h), indicating that the FMD did not affect the development and function of reactive immune cells in vivo or ex vivo. However, when the FMD treatment initiated after transfer of control donor splenocytes [B; EAE CTRL donor to naïve mice with FMD treatment], the recipient mice displayed a delayed disease onset (Day 12 vs. Day 16 post-transfer; Fig. 3g) and a major reduction in EAE severity scores compared to the control (2.38±0.48 vs. 0.75±0.87; Fig. 3h). Taken together, these results suggest that T-cell priming in response to myelin antigen occurred normally in EAE CTRL and EAE FMD groups.
Figure 3. Antigen activated splenocytes from the EAE-CTRL and the EAE-FMD mice had similar encephalitogenic effects.
(n=5–6 / group; mean ± S.E.M, * p < 0.05, ** p<0.01; *** p < 0.001; t test, 1-way ANOVA & Bonferroni Post Test).
a. Diagram for the adoptive transfer EAE model.
b–d. Quantification of the (b) TNFα, (c) IFNγ, and (d)IL-17 (pg/mL) of the supernatant from ex-vivo culture of splenocytes from naïve, EAE CTRL, and EAE FMD either with or without MOG35-55 and IL-23 re-activation
e–f. Quantification of TH1 or TH17 (represented by % of CD4+) from lymphocytes culture of EAE CTRL and EAE FMD with or without MOG35-55 and IL-23 re-activation
g. Incidence rate of adoptive transfer EAE groups.
h. EAE severity score of adoptive transfer EAE groups.
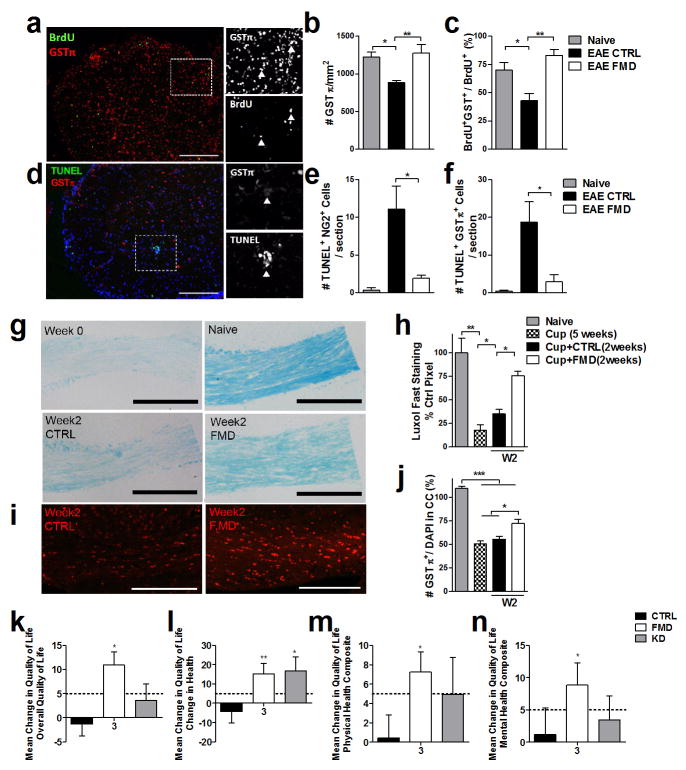
The FMD cycles stimulate remyelination by promoting oligodendrocyte regeneration
To investigate whether the reduced demyelination in FMD mice may also be related to enhanced oligodendrocyte regeneration, we first carried out a quantitative image analysis of NG2+ (oligodendrocyte progenitor cells marker; OPC) and GST- π+ (mature oligodendrocyte marker) in the spinal cord sections from the control or FMD mice (Fig. 4a). We observed no difference in the number of NG2+ OPC in the sections from EAE CTRL and EAE FMD group (Supplemental Fig. 3a). However, at D14, the number of GST- π+ oligodendrocytes was reduced in the EAE CTRL group but not in the EAE FMD group (886.7±41.6 vs. 1273±200.3; cells/ spinal cord section area; p < 0.01; Fig. 4b). To assess whether the normal levels of mature oligodendrocytes in the EAE FMD group were due to enhanced regeneration and/or differentiation, EAE CTRL or EAE FMD mice were injected with BrdU at the time of re-feeding (Day10). We observed a major increase (p< 0.01) in the percentage of cells that are double positive for BrdU+ and GSTπ+ in the EAE FMD group compared to the EAE CTRL (42.9±11.2% vs. 83.0±13.2%; p < 0.01) suggesting that the FMD promotes oligodendrocyte differentiation from precursor cells (Fig. 4c). To assess the effects of the FMD on either OPC or mature oligodendrocytes, sections were stained with TUNEL, an apoptotic marker, and GST- π+ or NG2+ (Fig. 4d). We observed a significant increase in TUNEL+ NG2+ (11.2±12.2 vs. 1.9±1.4 cells/section) cells and TUNEL+ GST- π+ (18.8±15.2 vs. 2.9±5.3 cells/section) in the control group compared to FMD group (p < 0.05; Fig. 4e–f). Taken together, these results indicate that the FMD not only stimulates regeneration and differentiation of oligodendrocytes but also protects OPC and mature oligodendrocytes from apoptosis.
Figure 4. The FMD cycles protect the spinal cord from loss of oligodendrocyte precursor cells and oligodendrocytes and enhances remyelination in the cuprizone model.
(At least 12 sections/ mouse were used for quantification; n=4; mean ± S.E.M, * p < 0.05, ** p<0.01; *** p < 0.001; 1-way ANOVA & Bonferroni Post Test).
a – c. Spinal cord sections isolated at Day 14 and quantification for (a) GST-π (mature oligodendrocyte) and BrdU, for (b) TUNEL and NG2 (oligodendrocyte precursor cells), and for (c) TUNEL and GST-π of the naive, EAE-CTRL or EAE-FMD.
f–h. Sections from the corpus callosum region and quantification of cuprizone treated brains, stained with Luxol Fast Blue of the naïve control, end of 5 weeks of cuprizone diet (week 0), cuprizone (5 weeks) + regular chow (2 weeks), cuprzione (5 weeks) + FMD cycle (2 weeks).
i–j. Section from the corpus callosum region and its quantification of the cuprizone treated brains stained with GST-π+ of cuprizone (5 weeks) + regular chow (2 weeks), cuprzione (5 weeks) + FMD (2 weeks). Quantification is normalized to % of the naïve GST-π+ level.
k–m. Change in the quality of life at 3 month of (k) overall quality of life, (l) change in health, (m) physical health composite, and (n) mental health composite. The dotted line represents a threshold that is thought to be clinically important (≥ 5 points) (mean ± SED; * p<0.05; Mann-Whitney-U test. Increase of ≥ 5 points are considered as clinically important).
To investigate whether the FMD-dependent stimulation of oligodendrocyte differentiation and remyelination can occur independent of the observed effects on T-cell number and activity, we used the cuprizone-induced demyelinating mouse model (Ransohoff, 2012; Torkildsen et al., 2008). Addition of 0.2% (w/w) cuprizone to the regular mouse diet for 5–6 weeks results in demyelination in the corpus callosum followed by spontaneous remyelination upon re-feeding with regular chow. After 5 weeks of cuprizone treatment, mice were switched to either the control diet or FMD cycles for 5 weeks and some were euthanized weekly to assess the degree of myelination by Luxol Fast staining and GST- π+ (Fig. 4g, i). As expected, after 5 weeks of the cuprizone diet, a significant reduction in myelin staining was observed in the corpus callosum compared to the naive controls (Fig. 4h, j). After 2 cycles, the FMD-treated group displayed increased myelin staining and in the number of GST- π+ oligodendrocytes compared to the control diet group (Fig. 4h, j). However, at later time points, we did not observe differences between spontaneous re-myelination of the control diet cohort and FMD cohort, since it is well established that cuprizone-dependent myelin damage can be fully reversed after removal of the toxin (Supplemental Fig. 3 c, d). These results indicate that the FMD promotes OPC-dependent regeneration and accelerates OPC-differentiation into oligodendrocytes while enhancing remyelination independently of its modulation of the inflammatory response.
A randomized pilot trial to test the effects of a FMD or KD in relapsing-remitting MS patients: evidence for safety and feasibility
A randomized parallel-group 3 arm pilot trial (NCT01538355) was conducted to assess the safety and feasibility of FMD or KD treatment on health-related quality of life (HRQOL) in relapsing-remitting MS patients. 60 patients were randomly assigned to: control diet (CD n=20), KD for 6 months (n=20) or a single cycle of modified human FMD for 7 days (n=20) followed by a Mediterranean diet for 6 months (Supplemental Fig. 4). Baseline characteristics were balanced between the 3 groups (Supplemental Tab. 1 and Supplemental Tab. 2). The FMD and KD cohorts displayed clinically meaningful improvements in the HRQOL summary scales at 3 months which included the overall quality of life (Fig. 4k) change in health (Fig. 4l), physical health composite (Fig. 4m), and mental health composite (Fig. 4n). Also, similar changes were observed in the total HRQOL scales at different time points (Supplemental Fig. 5). Adverse events (AEs) and serious adverse events [SAEs] were reported for 92% [8%] of CD cohort individuals, 78% [16%] of FMD cohort individuals, and 78% [11%] of KD cohort individuals (Supplemental Tab. 5). The most common AEs was airways infection (common adverse events) and the most frequent SAE was lower urinary tract infection (serious adverse events). No indication of increase in liver enzymes exceeding the normal range was observed in any of the three treatment groups. Also, the interventions were well tolerated, as evident from high compliance rates (CD: 60%; KD: 90%; FMD: 100%). During the 6-month study period we observed a total of 8 relapses: 4 in the CD, 1 in the KD, and 3 in the FMD group. In addition to increased β-hydroxybutyrate levels in plasma, we observed a slight reduction in lymphocytes and white blood cell counts and we detected a mild reduction in EDSS scores in the FMD and KD groups (measured on Day 7 for FMD and Day 30 for KD; Supplemental Tab. 4 and Supplemental Tab. 6). Thus, there was an inverse association between EDSS and HRQOL scores (Supplemental. Tab. 7). Overall, our study indicates that the administration of FMD and KD is safe, feasible and potentially effective, but further studies including analyses such as MRI, blinded clinical assessments, an appropriate control diet, and immune assays are required to determine efficacy.
Discussion
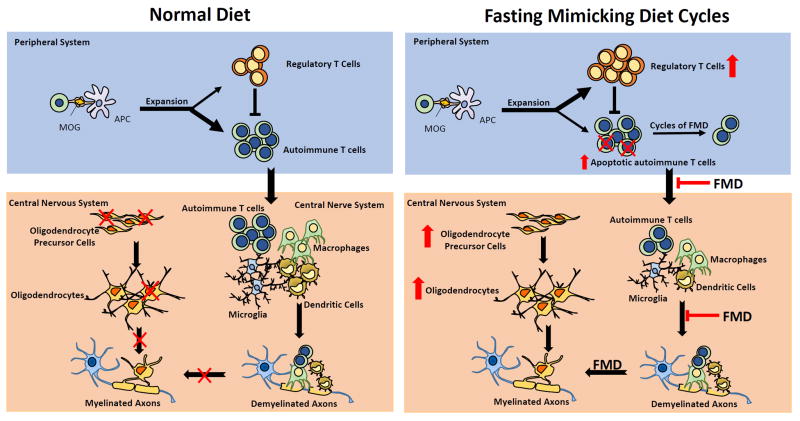
A FMD administered every week was effective in ameliorating EAE symptoms in all mice and completely reversed disease progression a portion of animals after the onset of EAE signs. By contrast, the KD had more modest effects and did not reverse EAE progression in mice. FMD cycles appear to be effective in the treatment of EAE in mice by: (1) promoting oligodendrocyte precursor-dependent regeneration, and 2) reducing the levels of microglia/monocytes and of T cells contributing to the autoimmunity and encephalomyelitis. Our results support a FMD-mediated anti-inflammatory effects possibly involving the up-regulation of AMPK or down-regulation of mTORC1, which sense nutrient availability and dictate cell fate (Laplante and Sabatini, 2012). It was shown that mTORC1 couples the immune signals and the metabolic programming to establish Treg-cell function (Zeng et al., 2013). In fact, treatment with the mTORC1 inhibitor rapamycin or AMPK activator metformin attenuates EAE symptoms by modulating effector and regulatory T cells and restricting the infiltrating mononuclear cells into the CNS (Esposito et al., 2010; Nath et al., 2009; Zeng et al., 2013). Therefore, the FMD treatment could interfere with T-cell proliferation, differentiation, and with recruitment of other immune cells, resulting in a decreased recruitment at the lesion sites (Fig. 5). Some of these effects of the FMD may be triggered by an endogenous glucocorticoid production. Glucocorticoids are used to treat MS relapses, but are generally administered in short bursts since they can cause adverse effects including osteoporosis, and metabolic syndrome (Brusaferri and Candelise, 2000; Ce et al., 2006; Roth et al., 2010; Uttner et al., 2005). The FMD may avoid these adverse effects by promoting additional and coordinated endogenous responses. Importantly, FMD cycles also activated oligodendrocyte precursor cells resulting in myelin regeneration, as demonstrated by accelerated remyelination rate in the cuprizone model (Fig. 5). Notably, because it is the alternation of FMD cycles and re-feeding and not the FMD alone that promotes both the regeneration and the replacement of autoimmune cells with naïve cells, the use of chronic restriction may not be effective or as effective in the treatment of EAE/MS.
Figure 5. A simplified model of FMD-mediated effects on glucocorticoid, immune suppression & oligodendrocyte regeneration and differentiation in MS.
The FMD treatment promotes endogenous glucocorticoid production, increases Treg cell numbers, blocks T-cell activation and promotes T-cell death. In the lesion area. FMD treatment reduces autoimmune T-cell and microglia infiltration, promotes oligodendrocyte precursor dependent regeneration and the differentiation of myelinating oligodendrocyte which engage with demyelinated axons to promote the formation of myelin sheaths.
Finally, we report that the administration of the FMD and KD in MS patients was safe, well tolerated and resulted in high compliance. We observed potentially positive effects of FMD cycles or KD treatment in RRMS based on changes in self-reported HRQOL, and a mild improvement in EDSS (Supplemental Tab. 6). However, the lack of a proper Mediterranean diet control makes it difficult to establish whether the FMD cycles alone are sufficient for these effects. In addition, MRI analyses and an adequately blinded clinical assessments (EDSS, MSFC) and of immune function analyses, would greatly enhance the strength of the clinical findings. Because, unlike for the mouse experiments, the FMD was only administered to patients once, it will be important to test the effects of multiple FMD cycles on MS patients in larger, randomized and controlled trials.
Materials and Methods
EAE model
C57Bl/6 (10-week-old female) mice were purchased from The Jackson Laboratory, immunized subcutaneously with 200 μg myelin oligodendrocyte glycoprotein peptide (MOG35-55; GenScript) mixed 1:1 with supplemented complete Freund’s Adjuvant followed by 200 ng of mouse pertussis toxin (PTX; List Biological Laboratories) i.p. at day 0 and day 2. For adoptive transfer, spleens from active immunized mice were isolated and RBC were lysed. Spleen cells were cultured in presence of MOG35-55 (20 μg/mL) with rmIL-23 (20 ng/mL) for 48 hours. Cells were collected and re-suspended in PBS and 15 million cells were injected intravenous. See supplemental material and methods for detailed description of disease severity scoring. All experiments were performed in accordance with approved Institutional Animal Care and Use Committee (IACUC) protocols of University of Southern California
Fasting Mimicking Diet (Mouse)
Mice were fed ad lib with irradiated TD.7912 rodent chow (Harlan Teklad), containing 15.69 kJ/g of digestible energy (animal-based protein 3.92 kJ/g, carbohydrate 9.1 kJ/g, fat 2.67 kJ/g). The experimental FMD is based on a nutritional screen that identified ingredients which allow high nourishment during periods of low calorie consumption. The FMD diet consists of two different components designated as day 1 diet and day 2–3 diet that were fed in this order respectively. See supplemental material and methods for detailed explanation of the FMD. Mice consumed all the supplied food on each day of the FMD regimen and showed no signs of food aversion. After the end of FMD, we supplied TD.7912 chow ad lib for 4 days before starting another FMD cycle. Prior to supplying the FMD, animals were transferred into fresh cages to avoid feeding on residual chow and coprophagy.
Clinical Trial Design
This study was a three-armed parallel grouped, single center, controlled and randomized clinical pilot trial to assess the effects of dietary interventions on HRQOL in RRMS patients. The permuted-block randomization was generated online at the website randomization.com. An investigator blind to the randomization plan determined the patients’ randomization number before they underwent the randomization step. This study is registered with ClicalTrials.gov. NCT01538355. See supplemental material and methods for detailed descriptions of the clinical trial and the diet compositions.
Supplementary Material
Acknowledgments
We thank Dr. Stephen Hauser for insightful comments. We thank Dr. Pinchas Cohen for assistance with fluorescent microscopy. We thank Nadine Krueger and Gabi Rahn for the technical assistance. Dr. Laura Piccio is a Harry Weaver Neuroscience Scholar of the National Multiple Sclerosis Society (NMSS, JF 2144A2/1) and is funded by Fondazione Italiana Sclerosi Multipla (FISM; 2014/R/15) and the Office of the Assistant Secretary of Defense for Health Affairs, through the Multiple Sclerosis Research Program under Award No. W81XWH-14-1-0156 (opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the Department of Defense). The mouse study was funded by NIH/NIA grants AG034906 to VDL. The human study was funded by Meylin Projekt e.V. and Familie Ernst Wendt Stiftung Stadt Koeln, which were not involved in any decision making process relating the study or its participants. The work of FP is supported by Deutsche Forschungsgemeinschaft (DFG Exc 257). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Aging or the National Institutes of Health. The University of Southern California has licensed intellectual property to L-Nutra that is under study in this research. As part of this license agreement, the University has the potential to receive royalty payments from L-Nutra. VDL has equity interest in L-Nutra, a company that develops medical food.
Footnotes
Author Contributions: I.C., L.P., M.W., and V.D.L designed mouse experiments. I.C., S.B. and P.C performed the mouse experiment. I.C, L.P., P.C., B.B. and A.G performed and processed immunohistochemistry. I.C., L.P. and B.B. performed qualitative and quantitative analysis. I.C. and J.S. performed FACS analysis. I.C. processed cytokine assay. AM, FP, and MB designed the human study; MB acquired human clinical data; AM, FP and MB, analyzed and interpreted data; MB performed, interpreted, and presented the statistical analysis. A.M., F.P., M.B., A.H.C., T.E.M., M.W., and V.D.L. were involved in discussing the results and editorial support. I.C., M.B., and V.D.L. wrote the paper. I.C. and L.P. contributed equally to this work. M.B. and V.D.L. contributed equally to this work. All authors discussed the results and commented on the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ashwell JD, Lu FW, Vacchio MS. Glucocorticoids in T cell development and function*. Annual review of immunology. 2000;18:309–345. doi: 10.1146/annurev.immunol.18.1.309. [DOI] [PubMed] [Google Scholar]
- Brandhorst S, Choi IY, Wei M, Cheng CW, Sedrakyan S, Navarrete G, Dubeau L, Yap LP, Park R, Vinciguerra M, et al. A Periodic Diet that Mimics Fasting Promotes Multi-System Regeneration, Enhanced Cognitive Performance, and Healthspan. Cell metabolism. 2015;22:86–99. doi: 10.1016/j.cmet.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brusaferri F, Candelise L. Steroids for multiple sclerosis and optic neuritis: a meta-analysis of randomized controlled clinical trials. Journal of neurology. 2000;247:435–442. doi: 10.1007/s004150070172. [DOI] [PubMed] [Google Scholar]
- Ce P, Gedizlioglu M, Gelal F, Coban P, Ozbek G. Avascular necrosis of the bones: an overlooked complication of pulse steroid treatment of multiple sclerosis. European journal of neurology : the official journal of the European Federation of Neurological Societies. 2006;13:857–861. doi: 10.1111/j.1468-1331.2006.01375.x. [DOI] [PubMed] [Google Scholar]
- Chang A, Tourtellotte WW, Rudick R, Trapp BD. Premyelinating oligodendrocytes in chronic lesions of multiple sclerosis. The New England journal of medicine. 2002;346:165–173. doi: 10.1056/NEJMoa010994. [DOI] [PubMed] [Google Scholar]
- Cheng CW, Adams GB, Perin L, Wei M, Zhou X, Lam BS, Da Sacco S, Mirisola M, Quinn DI, Dorff TB, et al. Prolonged fasting reduces IGF-1/PKA to promote hematopoietic-stem-cellbased regeneration and reverse immunosuppression. Cell stem cell. 2014;14:810–823. doi: 10.1016/j.stem.2014.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhib-Jalbut S. Pathogenesis of myelin/oligodendrocyte damage in multiple sclerosis. Neurology. 2007;68:S13–21. doi: 10.1212/01.wnl.0000275228.13012.7b. discussion S43–54. [DOI] [PubMed] [Google Scholar]
- Esposito M, Ruffini F, Bellone M, Gagliani N, Battaglia M, Martino G, Furlan R. Rapamycin inhibits relapsing experimental autoimmune encephalomyelitis by both effector and regulatory T cells modulation. Journal of neuroimmunology. 2010;220:52–63. doi: 10.1016/j.jneuroim.2010.01.001. [DOI] [PubMed] [Google Scholar]
- Esquifino AI, Cano P, Jimenez-Ortega V, Fernandez-Mateos MP, Cardinali DP. Immune response after experimental allergic encephalomyelitis in rats subjected to calorie restriction. Journal of neuroinflammation. 2007;4:6. doi: 10.1186/1742-2094-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher JM, Lalor SJ, Sweeney CM, Tubridy N, Mills KH. T cells in multiple sclerosis and experimental autoimmune encephalomyelitis. Clinical and experimental immunology. 2010;162:1–11. doi: 10.1111/j.1365-2249.2010.04143.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontana L, Partridge L, Longo VD. Extending healthy life span--from yeast to humans. Science. 2010;328:321–326. doi: 10.1126/science.1172539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friese MA, Fugger L. Autoreactive CD8+ T cells in multiple sclerosis: a new target for therapy? Brain : a journal of neurology. 2005;128:1747–1763. doi: 10.1093/brain/awh578. [DOI] [PubMed] [Google Scholar]
- Goverman J. Autoimmune T cell responses in the central nervous system. Nature reviews Immunology. 2009;9:393–407. doi: 10.1038/nri2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guevara-Aguirre J, Balasubramanian P, Guevara-Aguirre M, Wei M, Madia F, Cheng CW, Hwang D, Martin-Montalvo A, Saavedra J, Ingles S, et al. Growth hormone receptor deficiency is associated with a major reduction in pro-aging signaling, cancer, and diabetes in humans. Science translational medicine. 2011;3:70ra13. doi: 10.1126/scitranslmed.3001845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmer B, Archelos JJ, Hartung HP. New concepts in the immunopathogenesis of multiple sclerosis. Nature reviews Neuroscience. 2002;3:291–301. doi: 10.1038/nrn784. [DOI] [PubMed] [Google Scholar]
- Herold MJ, McPherson KG, Reichardt HM. Glucocorticoids in T cell apoptosis and function. Cellular and molecular life sciences : CMLS. 2006;63:60–72. doi: 10.1007/s00018-005-5390-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kafami L, Raza M, Razavi A, Mirshafiey A, Movahedian M, Khorramizadeh MR. Intermittent feeding attenuates clinical course of experimental autoimmune encephalomyelitis in C57BL/6 mice. Avicenna journal of medical biotechnology. 2010;2:47–52. [PMC free article] [PubMed] [Google Scholar]
- Kim do Y, Hao J, Liu R, Turner G, Shi FD, Rho JM. Inflammation-mediated memory dysfunction and effects of a ketogenic diet in a murine model of multiple sclerosis. PloS one. 2012;7:e35476. doi: 10.1371/journal.pone.0035476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell. 2012;149:274–293. doi: 10.1016/j.cell.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C, Safdie FM, Raffaghello L, Wei M, Madia F, Parrella E, Hwang D, Cohen P, Bianchi G, Longo VD. Reduced levels of IGF-I mediate differential protection of normal and cancer cells in response to fasting and improve chemotherapeutic index. Cancer research. 2010;70:1564–1572. doi: 10.1158/0008-5472.CAN-09-3228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longo VD, Mattson MP. Fasting: molecular mechanisms and clinical applications. Cell metabolism. 2014;19:181–192. doi: 10.1016/j.cmet.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucchinetti C, Bruck W, Parisi J, Scheithauer B, Rodriguez M, Lassmann H. A quantitative analysis of oligodendrocytes in multiple sclerosis lesions - A study of 113 cases. Brain : a journal of neurology. 1999;122:2279–2295. doi: 10.1093/brain/122.12.2279. [DOI] [PubMed] [Google Scholar]
- Nath N, Khan M, Paintlia MK, Singh I, Hoda MN, Giri S. Metformin attenuated the autoimmune disease of the central nervous system in animal models of multiple sclerosis. Journal of immunology. 2009;182:8005–8014. doi: 10.4049/jimmunol.0803563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pender MP, Greer JM. Immunology of multiple sclerosis. Current allergy and asthma reports. 2007;7:285–292. doi: 10.1007/s11882-007-0043-x. [DOI] [PubMed] [Google Scholar]
- Piccio L, Stark JL, Cross AH. Chronic calorie restriction attenuates experimental autoimmune encephalomyelitis. Journal of leukocyte biology. 2008;84:940–948. doi: 10.1189/jlb.0208133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Planey SL, Litwack G. Glucocorticoid-induced apoptosis in lymphocytes. Biochemical and biophysical research communications. 2000;279:307–312. doi: 10.1006/bbrc.2000.3922. [DOI] [PubMed] [Google Scholar]
- Raine CS, Wu E. Multiple-Sclerosis - Remyelination in Acute Lesions. J Neuropath Exp Neur. 1993;52:199–204. [PubMed] [Google Scholar]
- Ransohoff RM. Animal models of multiple sclerosis: the good, the bad and the bottom line. Nature neuroscience. 2012;15:1074–1077. doi: 10.1038/nn.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen S, Wang Y, Kivisakk P, Bronson RT, Meyer M, Imitola J, Khoury SJ. Persistent activation of microglia is associated with neuronal dysfunction of callosal projecting pathways and multiple sclerosis-like lesions in relapsing--remitting experimental autoimmune encephalomyelitis. Brain : a journal of neurology. 2007;130:2816–2829. doi: 10.1093/brain/awm219. [DOI] [PubMed] [Google Scholar]
- Roth P, Wick W, Weller M. Steroids in neurooncology: actions, indications, side-effects. Current opinion in neurology. 2010;23:597–602. doi: 10.1097/WCO.0b013e32833e5a5d. [DOI] [PubMed] [Google Scholar]
- Sospedra M, Martin R. Immunology of multiple sclerosis. Annual review of immunology. 2005;23:683–747. doi: 10.1146/annurev.immunol.23.021704.115707. [DOI] [PubMed] [Google Scholar]
- Torkildsen O, Brunborg LA, Myhr KM, Bo L. The cuprizone model for demyelination. Acta neurologica Scandinavica Supplementum. 2008;188:72–76. doi: 10.1111/j.1600-0404.2008.01036.x. [DOI] [PubMed] [Google Scholar]
- Uttner I, Muller S, Zinser C, Maier M, Sussmuth S, Claus A, Ostermann B, Elitok E, Ecker D, Brettschneider J, et al. Reversible impaired memory induced by pulsed methylprednisolone in patients with MS. Neurology. 2005;64:1971–1973. doi: 10.1212/01.WNL.0000163804.94163.91. [DOI] [PubMed] [Google Scholar]
- Vegiopoulos A, Herzig S. Glucocorticoids, metabolism and metabolic diseases. Molecular and cellular endocrinology. 2007;275:43–61. doi: 10.1016/j.mce.2007.05.015. [DOI] [PubMed] [Google Scholar]
- Wingerchuk DM, Carter JL. Multiple sclerosis: current and emerging disease-modifying therapies and treatment strategies. Mayo Clinic proceedings. 2014;89:225–240. doi: 10.1016/j.mayocp.2013.11.002. [DOI] [PubMed] [Google Scholar]
- Wolswijk G. Chronic stage multiple sclerosis lesions contain a relatively quiescent population of oligodendrocyte precursor cells. The Journal of neuroscience : the official journal of the Society for Neuroscience. 1998;18:601–609. doi: 10.1523/JNEUROSCI.18-02-00601.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng H, Yang K, Cloer C, Neale G, Vogel P, Chi H. mTORC1 couples immune signals and metabolic programming to establish T(reg)-cell function. Nature. 2013;499:485–490. doi: 10.1038/nature12297. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.