Abstract
Chronic pain is an affliction that affects a large proportion of the general population and is often accompanied by a myriad of negative emotional, cognitive, and physical effects. However, current pain adaptation paradigms do not account for the many chronic pain patients who demonstrate little or no noticeable impairment due to the effects of chronic pain. This paper offers resilience as an integrative perspective that can illuminate the traits and mechanisms underlying the sustainability of a good life and recovery from distress for individuals with chronic pain.
Keywords: Chronic pain, Resilience (psychological), Coping behavior, Stress
Introduction
Pain is an essential process that can signal injury or illness and can attract attention to areas of the body that require immediate care. However, when pain progresses from an acute to a chronic condition, it loses its usefulness as an indicator of injury and instead becomes a toxic influence unto itself. It is estimated that between 10% and 20% of the general population suffers from chronic or recurrent chronic pain [1]. Chronic pain has been associated with a variety of negative outcomes, including depression [2], and a variety of health problems, including obesity [3].
The experience of pain has been described as multimodal; that is, there are sensory, affective, and cognitive experiences of pain that can affect distinct domains of health and well-being. A number of studies have provided evidence that chronic pain adversely affects health and well-being through cognitive and affective processes such as catastrophizing [4], as well as more general passive or avoidant coping strategies [5]. There is also growing research indicating that chronic pain and accompanying cognitive-affective states can impact health and well-being through changes in physiological functioning, including activation and inflammation of the immune system [6]. Chronic high levels of pain is a prominent stressor [7] that can significantly increase the allostatic load (the strain or burden put on an individual's physiological and psychological system in order to maintain homeostasis) [8], leading to deleterious effects on health and emotional well-being [9]. Given that pain demonstrates influence that spans different systems of human functioning, it is useful to conceptualize means of coping with the deleterious effects of pain in the same way. This article proposes a multimodal paradigm for understanding pain and pain coping: the process of resilience to pain.
Issues in Defining Resilience to Pain
Themes of resilience arose in the field of child development, based on observations of many children who sustained positive functioning and development despite the presence of significant risk factors such as abuse or low socioeconomic status [10]. Although child development provides some of the most salient examples of resilience due to the often sensitive nature of children to risk factors, resilience is not a construct that is confined solely to the young. Resilience is a construct that retains its importance throughout the life span; adults, as well as children, can be considered “resilient” [11••].
In this article, resilience is considered from three different perspectives: 1) resilience as an outcome of adaptation efforts; 2) differential resilience in response to different types of stressors; and 3) the qualities of the individual and his/her social world that foster resilience. There are three primary classes of resilient outcomes: recovery, sustainability, and growth [11••]. Recovery refers to the extent to which the person regains equilibrium, following upsetting events. Recovery is particularly salient in the study of physiological systems, but also applies to “a return to normal” following cognitive and affective disturbances in homeostasis that result from stressful experiences. Sustainability refers to the perseverance of desirable actions, goal pursuits, and social engagements that are sources of positive emotion and self-esteem. Here, resilience is measured by the extent to which sources of personal and social meaning in the person's work, family, and leisure life are preserved. Growth, meanwhile, refers to the realization of greater understanding of one's capacities, and new learning that arises as a consequence of the stressful experience and outcomes of one's coping efforts. Although somewhat counterintuitive, many individuals report increases in personal growth in the face of stress; this has been shown to be especially salient in the process of benefit finding, which is discussed in greater detail later.
It is worthwhile to examine the relationship between the processes of recovery and sustainability. Also unexamined to date is how growth may relate to sustainability or recovery. It may be that those who realize some level of individual growth while in pain may also demonstrate more effective recovery as a result, or that they exhibit a more successful process of sustainability; the interrelationships of these processes will need to be borne out in future research. It is suggested here that examination of these manifestations of resilience should include factors that influence maintenance of positive functioning, as well as those factors that facilitate quicker or more effective recovery from episodic pain and other stressors that lead individuals to report long-term benefits that result from their pain.
Differences also exist in the ways that resilience is manifested in the face of various challenges that an individual may face. The degree to which an individual's response is resilient may depend on the type of challenge that he or she is facing. Those who are resilient to physiological stressors, for example, may not be as resilient in the face of toxic emotional stressors [12]. Individuals may exhibit highly effective coping in response to one type of stressor, but also exhibit very poor coping in the face of a different stressor. People are generally resilient, but few, if any, are resilient to all possible circumstances that may befall them.
The qualities of the person and the social environment that lead to resilient outcomes take many forms. One useful distinction may be made between resilience resources, and mechanisms by which a person exhibits resilience. Resilience resources refer to stable personal characteristics, such as extraversion and optimism, and beneficial social situations, such as strong positive family ties, that increase the likelihood of resilience outcomes of recovery, sustainability, and/or growth. These resilience resources influence resilient responses to stress through their promotion of beneficial resilience mechanisms. Resilience mechanisms refer to cognitions, affects, and behaviors employed at the time of the stressor that sustain well-being, aid recovery, and promote new learning/growth [13•]. Figure 1 describes the conceptual relationship between pain, resilience resources, mechanisms, and outcomes.
Fig. 1. Pathways to resilience for those in chronic pain. All items listed below the pathways are examples.
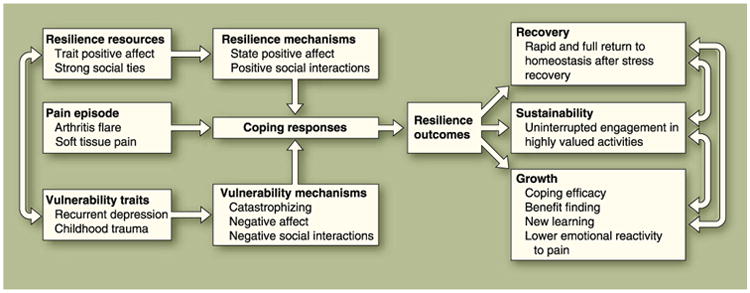
As shown in Fig. 1, resilience mechanisms modify the relationship between pain and outcome through strengthening coping responses to pain. In this way, resilience mechanisms may be thought of as moderators of these interrelationships involving pain and outcomes related to health and well-being [13•]. In order to effectively define resilience to pain, it is therefore important to consider prominent aspects of both the mechanisms of resilience and of resilience resources.
Sources of resilience are often treated as opposites of risk factors and vulnerabilities [14••], but it is most useful to consider them separate constructs. We have included vulnerability and risk in our overall model as distinct influences inversely correlated with resilience resources, because they are also important in the charting of pain adaptation success and failure. The focus of this article is on factors that increase the likelihood of resilience, and little attention is given to sources of vulnerability and risk. There is no lack of attention to those sources of failure of adaptation in the current literature on chronic pain.
The remainder of this article examines key resilience resources and mechanisms that span various systems of human functioning and that are likely to play a prominent role in adaptive coping responses to chronic pain; it also provides an examination of possible methodological and conceptual issues that may arise in defining resilience to pain.
Key Personality Resources
Smith and Zautra [14••] enumerated various “positive characteristics” that can be considered resilience resources in individuals with chronic pain: optimism, purpose in life, and pain acceptance. The trait of dispositional optimism has been increasingly studied as a source of individual resilience, and it appears that optimism may play a role in effective coping with pain through increased healthy behaviors and decreased unhealthy behaviors that lead to better physical functioning for those in chronic pain [15•]. Dispositional optimism has been broadly defined as a tendency to consistently hold positive expectations for the future, even in the face of uncertainty, and has been theorized to be a key mechanism in maintaining active engagement in attempts to accomplish one's goals despite adversity [16]. Evidence has demonstrated a positive association of optimism and healthy aging behaviors, such as moderate alcohol use and less smoking [17], and habituation to a cold pressor pain induction task [15•], and has been found to be a partial mediator of the relationship between pain and life satisfaction [18]. Furthermore, higher levels of optimism have been found to be related to lower rates of pain intensity and depressive symptoms in people in the early and intermediate stages of rheumatoid arthritis [19].
Lightsey [20] suggests that the definition of well-being as an individual outcome should take into account factors that are less hedonic in nature and relate more to self-actualization and the meaning of one's life. With this in mind, another resilience resource of note is the belief that one's life has meaning and purpose. “Purpose in Life” is a construct that refers to the extent to which individuals understand the purpose and direction of their current and past lives, have goals and beliefs that give their lives meaning, and demonstrate a high level of intention toward pursuing their goals [21]. Those individuals that express a stronger belief that their lives have purpose have demonstrated a higher tolerance to pain on both cold pressor and heat-based pain induction procedures [15•]. Furthermore, those that score high on the “Purpose in Life” scale have demonstrated faster recovery times from knee replacement surgery [22]. This resource may be especially valuable to sustainability in the face of episodic pain.
One variable that has been increasingly studied in recent years that may play a prominent role in resilience to pain is pain acceptance. Pain acceptance refers to a general willingness to experience pain and its associated cognitive and emotional consequences as a means of fostering a greater sense of personal engagement and well-being by not relying on avoidant or control-based coping [23]. It has been suggested that pain acceptance can be a particularly useful coping strategy for individuals suffering from chronic pain because it frees up cognitive and affective resources from worrying about the pain itself (which is, in essence, an unchangeable condition and thus makes such attempts counterproductive) to focus on external stressors or concerns that actually can be changed [24]. Higher acceptance scores have been found to be predictive of lower levels of pain catastrophizing [25], better cognitive, emotional, social, and occupational functioning [23], and has been shown to play a prominent role in mental- and health-related quality of life [26]. Kratz et al. [27], for example, found that pain acceptance levels were directly related to the level of positive affect experienced by an individual, which also buffered the positive association between pain intensity and negative affect.
In the broadest sense, resilience mechanisms relevant to pain identify the processes through which individuals quickly recover from pain flares, sustain a satisfying level of positive functioning, and perhaps also find they have “grown” from the experience. Questions remain, however, about precisely which mechanisms best characterize these processes. It appears that a useful chart of resilient processes should encompass different domains of functioning, including emotions, social interactions, cognitions, and behaviors.
Emotional Aspects of Resilience to Pain
One key resource that aids individuals in resisting the deleterious effects of pain in their everyday functioning, as well as in the recovery from pain-related deficits in functioning, is high average levels of positive emotion, usually measured as elevations in positive affect. Positive affect has been associated with a wide range of benefits: it has been associated with lower negative affect and pain from week to week [28], and those who have higher average levels of positive affect have been found to have more responsive immune systems [29] and, more specifically, those with higher levels of positive emotionality have demonstrated lower reported rates of viruses such as rhinovirus and influenza [30].
The experience of positive emotions can strengthen personal efforts to cope with a present stressor; this is referred to as the “broaden-and-build theory of positive emotions” [31]. In this way, positive affect can be used to cope with current stressors, but it can also aid in the recovery from negative experiences. The dynamic model of affect (DMA) suggests that positive and negative affects become more negatively associated under conditions of stress (and, by extension, pain) [32]. Stressors such as pain narrow the “affective space,” such that the experience of negative emotions reduces the likelihood of experience of positive emotions.
Recent evidence indicates that those individuals who are higher in resilience resources show lower daily levels of trait catastrophizing and more experiences of positive emotions than those who are low in trait resilience, and that positive emotions mediate the process of recovery from catastrophizing for people who are psychologically resilient [33]. People who typically report high levels of positive emotion can sustain those feelings in the face of negative affects, showing greater emotional complexity, better stress adaptation, and quicker recovery [34]. When people experience greater than usual positive affects, pain does not elevate their negative emotions to the same degree [35]. Those who are more able to experience both positive and negative emotions during a stressful episode are also said to exhibit higher affective complexity [32], a potential resource in sustainability and growth for those with chronic pain.
Two other traits appear to be related to higher individual levels of affective complexity, and may therefore be viewed as emotion-specific resilience resources: discrete emotional knowledge and self-focused attention. Discrete emotional knowledge is a construct that refers to the ability of an individual who can identify the object of the emotion, its context, associated bodily sensations, rules for expression, and actions that are appropriate to take in response to the emotion. Individuals who have higher discrete emotional knowledge are able to more effectively differentiate between emotions [36]. Those who demonstrate a greater level of attention to their own moods may have the capacity to use their emotional reactions as a means of coping with stress [37]. Given that both discrete emotional knowledge and self-focused attention can play a prominent role in the regulation of positive and negative affect, they can also be considered resources for recovery, sustainability, and growth, although studies that might test these relationships have not been performed as yet.
Cognitive-Behavioral Aspects of Resilience to Pain
Another key variable that plays a prominent role in resilience to pain is active coping. Active coping refers to directed actions by an individual in pain to control their own pain and to function in spite of any pain that they are experiencing [38]. Active coping has been associated with physical activity levels [38], higher levels of social interaction [39], and lower levels of depression [25]. Higher pain acceptance scores have also been found to predict higher rates of active coping [25]. We would caution, however, that active coping is vague and could encompass behaviors that are not adaptive, such as attempts to control pain episodes that are uncontrollable or to repeatedly seek social support from those unwilling to provide it [39]. Further, meditative methods of emotion regulation may be mistakenly classified as passive means of coping, when using an active versus passive language to describe coping efforts. A more useful term is “approach” coping, which refers to the person's cognitive and behavioral orientation to chronic pain. Approach coping encompasses all direct efforts to solve the problem of pain, and stands in sharp contrast with mechanisms of avoidance.
Karoly and Ruehlman [40] have developed a definition of resilience that characterizes individuals as resilient if they experience high levels of pain severity, but low levels of emotional burden and pain-related dysfunction. The researchers determined that individuals with chronic pain who fit this definition of resilience showed significantly better functioning across various cognitive and behavioral domains (including pain coping strategies, attitudes toward pain, and health care and medication utilization) than a similar, “non-resilient” group, who demonstrated similar levels of pain severity, but higher levels of functional interference and emotional burden. Similarly, those who are high in trait resilience also demonstrate lower levels of cortisol secretion in anticipation of a stressful event [41]. Furthermore, it has been suggested that individuals who demonstrate a higher belief in their own ability to cope with pain (pain coping efficacy) tend to expend more effort in coping with their own pain [42]. These self-efficacious beliefs appear to be closely related conceptually to the “approach” behaviors set out by Smith and Zautra [14••], which share prominent features of behavioral activation and motivation.
Another cognitive process that has been linked more specifically to perceptions of growth is benefit finding. Benefit finding refers to cognitive restructuring that a person does to recast an inherently negative event such as pain into a beneficial outcome: the proverbial “blessing in disguise” [43]. This process has been theorized to lead to a state of “enhanced allostasis” that leads an individual to react to a stressor in more efficient ways, such as lower physiological arousal and inflammatory response that may lead to better physical health outcomes in the future [43].
Identifying the “Trait and State” Components of Resilience Processes
The model proposed in this article suggests that for certain broad constructs such as pain acceptance and benefit finding, it may be possible to “deconstruct” these concepts into state and trait components, which can have wide-reaching implications for building theories and interventions related to these constructs. The conceptual model in Fig. 1 suggests that an intervention that specifically targets benefit finding may increase the average (trait) level of benefit finding in an individual. This trait-level increase may then impact the level of day-to-day benefit finding that an individual attempts, thereby fostering better outcomes in the future. That is, the model provides a clearer hypothesis about how interventions designed to change mean levels of a given behavior or reaction can actually impact the day-to-day resilient responses of a person in pain. The model is a conceptual framework that provides a detailed explanation of the processes that may be involved in how an individual can be “resilient” to pain. It delineates “higher-order” resilience resources that may serve as points of intervention (eg, trait positive affect and pain acceptance), as well as “state” resilience mechanisms that may have a more immediate impact on the day-to-day adaptation to chronic pain (eg, the number of positive social interactions experienced, or daily fluctuations in positive affect). Consideration of whether a given intervention targets resilience mechanisms or resilience resources may help to clarify the domains in which the intervention is intended to effect change, as well as the extent of this intervention's effect in other areas (eg, does an intervention intended to increase an average level of positive social engagement also lead to changes in trait or state levels of positive affect?).
Although a great deal of refining remains to be done in order to more precisely describe the processes involved in resilience, there is little doubt that many of these processes are interrelated. Some aspects (eg, positive affect and active coping) may be considered both predictors and outcomes of successful resilience to pain. Given the bidirectional nature of the influence of constructs such as positive affect and coping behavior, it appears that the process by which individuals maintain homeostasis is integrative, and the individuals who cope most effectively with chronic pain are those who show the greatest propensity for conserving their internal resources and more efficiently maintaining homeostatic function during a painful episode. As a result of this “enhanced allostasis,” they are better able to resist or recover from the physical, cognitive, and emotional drains that a recurrent stressor such as pain can present.
Social Resilience Resources and Mechanisms
Resilience has also been used to refer to a capacity by families, work teams, neighborhoods, and communities when interactions between individuals serve to bolster personal and community resources in the face of adversity [44]. It is important to consider the potentially powerful role that social interaction can play in coping with chronic pain. Social engagement, as well as the cognitive appraisal of secure attachment, can have a substantial benefit on the ability of individuals suffering from chronic pain to cope with their pain and stress. Conversely, social stressors such as interpersonal conflict have been associated with higher negative affect [28] and with lower levels of perceived social support and social support coping [45], which suggests a “social vulnerability” for many individuals with pain that can also lead to higher rates of avoidant coping.
The relationship between social interactions and affect in pain patients is more complex than it might first appear. Recent evidence suggests that resilient individuals may also bolster their positive emotions through positive social interactions, so it may be assumed that those that are more proactive in seeking such events may demonstrate an even higher level of resilience to pain [14••]. This is further illustrated by evidence that positive social engagements are effective in promoting resilience and reports of lower pain at a later time [28]. The personality trait of extraversion may also play a prominent role in resilience by increasing the frequency of beneficial social interactions [46]. What may be most important, however, is that the occurrence of positive social interactions does not seem to be tied very closely to fluctuations in pain or disease behavior; instead, social engagement appears more to be a function of personal characteristics and social opportunity that may potentially be improved through psychological and social intervention [47]. Thus, those individuals who learn to sustain positive social relationships and secure social support seem to demonstrate a higher level of adaptation to pain.
The literature on pain and adaptation has centered on the qualities of the person to define those who are most likely to be resilient. Equal weight needs to be given to the person's social world in identifying factors that promote resilience. Environments that reward efforts aimed at recovery, sustainability, and growth foster resilience in important ways, and individuals differ in the resourcefulness of the environments in which they live. Although the patient is at the center of attention in clinical work, there is much benefit when the social environment is also examined for its responsiveness to the patient's capacities for positive adaptation, and the patient is guided to favor interactions in those social realms most likely to reinforce resilient action.
Methodological Concerns
The term “chronic pain” is used to subsume a wide variety of disorders involving pain, including joint pain, muscle pain, neurological pain, pain from autoimmune system dysfunction, and pain resulting from terminal diseases such as cancer. Both localized pain (such as lower back pain) and widespread bodily pain may be part of the clinical picture. Thus, the subjective experience of pain may be qualitatively different, both across disorders and across individuals. For instance, it appears that individuals suffering from fibromyalgia seem to experience a greater degree of emotional distress than those individuals who suffer from osteoarthritis, although both disorders involve a similar degree of widespread bodily pain. These differences may be borne out through differential neurophysiological processes, or it may be manifested in a difference in a behavior, coping, or cognitive reaction to the pain itself. These considerations can have far-reaching implications toward the direction of future research on a given disorder, as well as on the development of a syndrome-or disease-specific treatment for pain.
Similarly, consideration should be given to demographic factors that may impact the overall nature of an individual's chronic pain experience and their subsequent reaction to it. Steptoe et al. [17] posit that age is a significant consideration when conceptualizing healthy behavior, because such behaviors can often be confounded by higher rates of disability and chronic illness. The same can be said of socioeconomic status (SES), because those individuals who report a lower SES may have fewer material or personal resources to contribute to maintaining or increasing healthy behavior. Another consideration that is closely related with SES is that of race and ethnicity. Despite evidence of fewer health care resources and the presence of risk factors such as discrimination and acculturation, there is evidence of better physical and emotional outcomes among the African-American [48] and Latin American communities [49] than Caucasians. What may explain this difference? It has been suggested that the presence of culture- or ethnicity-specific protective factors such as racial identification [48] and allocentrism [49], and/or higher rates of protective factors such as familial cohesion, religiosity, and spirituality may lead to significantly better resilience among different ethnic subgroups [48, 49]. As a result, it cannot be assumed that the nature of pain and pain coping are the same for different ethnicities.
There may also be significant gender differences to consider when examining the process of resilience to pain. Evidence suggests that there are significant psychosocial differences in how men and women respond to the same type of pain [50]. These differences may lead to differential rates of disability, activity level, and social interactions [50], all of which may impact the overall health status of an individual with chronic pain. Future research should serve to illuminate the influences of gender, race, ethnicity, culture, and socioeconomic differences.
Conclusions
Instead of focusing on deficits and vulnerabilities exclusively, this paper encourages that researchers and clinicians give more attention to how chronic pain patients may be resilient. One useful way of conceptualizing resilience to pain is to change one's perspective from looking for vulnerabilities to identifying one or more strengths that can foster resilient outcomes for people in pain. It is important to note that both stable personal characteristics (resilience resources) and more dynamic processes (resilience mechanisms) can play a prominent role in determining the effectiveness of individual pain adaptation. Those individuals that we may consider to be resilient to pain are those who adopt more adaptive coping strategies to pain (including adaptive seeking of social support and positive interactions, consistent exercise, less substance use, and/or consistent utilization of health care services), possess a greater belief that they can effectively control their pain, and thus expend more effort when implementing these coping strategies. Resilient individuals possess greater emotional knowledge and direct more attention within in order to evaluate their current emotional state, and thus may seek to bolster their own positive affect as a means of reducing the control that their current pain has over their emotions. They may demonstrate a more optimistic outlook on their lives, express a greater belief that their lives have meaning, and demonstrate a willingness to accept pain and its consequences as a means of fostering a greater sense of engagement in their lives overall. When they do experience pain and associated negative emotions, resilient individuals demonstrate more emotional complexity and, in the case of negative emotions, may also use information associated with these emotions in order to return to their normal levels of positive affect more quickly, thus aiding in the process of recovery from pain. Individuals who are more resilient may exhibit less intense negative emotions that subside more rapidly, quicker recovery from a pain episode, and this experience may be reflected physiologically, through a less severe inflammatory response from the immune system and/or lower levels of cortisol secretion.
It is important to keep in mind the different ways that a person in pain may show resilience. The effect of resilience may be manifested in quicker recovery from the negative effects of pain, through the effective sustaining of positive functioning despite the presence of pain, and even through the realization of personal growth due to the presence of pain. It should be noted that individual differences are unquestionably present in the process of resilience to pain, both in recovery of homeostasis following upset and sustainability of positive engagements. The nature of an individual's experience of pain may vary across different disorders and based on demographic variables such as age and gender. The responsiveness of the person's social world is a key factor in activation of resilient resources. In the absence of social interactions that reinforce resilient ways of thinking and behaving, the capacity that many people have to resolve their difficulties with chronic pain might otherwise remain dormant. Future research is needed to further illuminate the degree of the many forms that resilience can take. Nevertheless, the adoption of a strength-based view of those coping with chronic pain promises to greatly enhance our understanding of how people can adapt successfully, and provide important guidance to pain management programs.
Acknowledgments
The two authors contributed equally to this work. They wish to thank Billie Sandberg and members of the Resilience Solutions Group (RSG). The members of the RSG, in addition to the authors of this article, are, in alphabetical order: Leona Aiken, Felipe Castro, Mary Davis, John Hall, Roger Hughes, Martha Kent, Rick Knopf, Kathy Lemery, Linda Luecken, Kate Murray, Morris Okun, and John Reich. This work is supported in part by a grant from the National Institute on Aging (R01 AG 026006), Alex Zautra (PI), John Hall (Co-PI). In addition, the authors are grateful to St. Luke's Charitable Trust and the Arizona State University Office of the Vice President for Research for invaluable support of the RSG.
Footnotes
Disclosure No potential conflicts of interest relevant to this article were reported.
Contributor Information
John A. Sturgeon, Email: jasturge@asu.edu.
Alex J. Zautra, Email: atajz@asu.edu.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Gatchel RJ, Peng YB, Peters ML, et al. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133:581–624. doi: 10.1037/0033-2909.133.4.581. [DOI] [PubMed] [Google Scholar]
- 2.Brown GK, Nicassio PM, Wallston KA. Pain coping strategies and depression in rheumatoid arthritis. J Consult Clin Psychol. 1989;57:652–657. doi: 10.1037//0022-006x.57.5.652. [DOI] [PubMed] [Google Scholar]
- 3.Marks R. Obesity profiles with knee osteoarthritis: correlation with pain, disability, disease progression. Obesity (Silver Spring) 2007;15:1867–1874. doi: 10.1038/oby.2007.221. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7:524–532. [Google Scholar]
- 5.Zautra AJ, Hamilton NA, Burke HM. Comparison of stress responses in women with two types of chronic pain: fibromyalgia and osteoarthritis. Cognit Ther Res. 1999;23:209–230. [Google Scholar]
- 6.Zautra AJ, Yocum DC, Villanueva I, et al. Immune activation and depression in women with rheumatoid arthritis. J Rheumatol. 2004;31:457–463. [PubMed] [Google Scholar]
- 7.Carr DB, Goudas LC. Acute pain. Lancet. 1999;353:2051–2058. doi: 10.1016/S0140-6736(99)03313-9. [DOI] [PubMed] [Google Scholar]
- 8.Charney DS. Psychobiological mechanisms of resilience and vulnerability: implications for successful adaptation to extreme stress. Am J Psychiatry. 2004;161:195–216. doi: 10.1176/appi.ajp.161.2.195. [DOI] [PubMed] [Google Scholar]
- 9.McEwen BS, Stellar E. Stress and the individual: mechanisms leading to disease. Arch Intern Med. 1993:2093–2101. [PubMed] [Google Scholar]
- 10.Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 2000;71:543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11••.Reich JW, Zautra AJ, Hall JS, editors. Handbook of Adult Resilience. New York: Guilford Press; 2010. This book provides an updated and comprehensive overview of the construct of resilience and proposes a 3-factor model of resilience, including recovery, sustainability, and growth. [Google Scholar]
- 12.Rutter M. Psychosocial resilience and protective mechanisms. Amer J Orthopsychiatry. 1987;57:316–331. doi: 10.1111/j.1939-0025.1987.tb03541.x. [DOI] [PubMed] [Google Scholar]
- 13•.Smith BW, Dalen J, Wiggins K, et al. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15:194–200. doi: 10.1080/10705500802222972. This article identifies recovery as a key concept related to, but still independent of, the construct of resilience. The implications of differences in individual resilience for health-related outcomes are also discussed. [DOI] [PubMed] [Google Scholar]
- 14••.Smith BW, Zautra AJ. Vulnerability and resilience in women with arthritis: test of a two-factor model. J Consult Clin Psychol. 2008;76:799–810. doi: 10.1037/0022-006X.76.5.799. This article provides a delineation of the features of an affective health/resilience construct and tests resilience in a sample of chronic pain patients as a predictor of key social and emotional outcomes. [DOI] [PubMed] [Google Scholar]
- 15•.Smith BW, Tooley EM, Montague EQ, et al. The role of resilience and purpose in life in habituation to heat and cold pain. J Pain. 2009;10:493–500. doi: 10.1016/j.jpain.2008.11.007. This experimental article is among the first to test the utility of resilience as a coping mechanism to pain, and provides broader implications to the role of resilience in coping with both acute and chronic pain. [DOI] [PubMed] [Google Scholar]
- 16.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 17.Steptoe A, Wright C, Kunz-Ebrecht SR, Iliffe S. Dispositional optimism and health behavior in community-dwelling older people: associations with healthy ageing. Br J Health Psychol. 2006;11:71–84. doi: 10.1348/135910705X42850. [DOI] [PubMed] [Google Scholar]
- 18.Ferreira VM, Sherman AM. The relationship of optimism, pain and social support to well-being in older adults with osteoarthritis. Aging Ment Health. 2007;11:89–98. doi: 10.1080/13607860600736166. [DOI] [PubMed] [Google Scholar]
- 19.Treharne GJ, Kitas GD, Lyons AC, et al. Well-being in rheumatoid arthritis: the effects of disease duration and psychosocial factors. J Health Psychol. 2005;10:457–474. doi: 10.1177/1359105305051416. [DOI] [PubMed] [Google Scholar]
- 20.Lightsey OR. Resilience, meaning, and well-being. Couns Psychol. 2006;34:96–107. [Google Scholar]
- 21.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological well-being. J Pers Soc Psychol. 1989;57:1069–1081. [Google Scholar]
- 22.Smith BW, Zautra AJ. The role of purpose in life in recovery from knee surgery. Int J Behav Med. 2004;11:197–202. doi: 10.1207/s15327558ijbm1104_2. [DOI] [PubMed] [Google Scholar]
- 23.McCracken LM, Eccleston C. A prospective study of acceptance of pain and patient functioning with chronic pain. Pain. 2005;118:164–169. doi: 10.1016/j.pain.2005.08.015. [DOI] [PubMed] [Google Scholar]
- 24.McCracken LM. Learning to live with the pain: acceptance of pain predicts adjustment in persons with chronic pain. Pain. 1998;74:21–27. doi: 10.1016/S0304-3959(97)00146-2. [DOI] [PubMed] [Google Scholar]
- 25.Esteve R, Ramirez-Maestre C, Lopez-Martinez AE. Adjustment to chronic pain: the role of pain acceptance, coping strategies, and pain-related cognitions. Ann Behav Med. 2007;33:179–188. doi: 10.1007/BF02879899. [DOI] [PubMed] [Google Scholar]
- 26.Elander J, Robinson G, Mitchell K, et al. An assessment of the relative influence of pain coping, negative thoughts about pain, and pain acceptance on health-related quality of life among people with hemophilia. Pain. 2009;145:169–175. doi: 10.1016/j.pain.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Kratz AL, Davis MC, Zautra AJ. Pain acceptance moderates the relation between pain and negative affect in osteoarthritis and fibromyalgia patients. Ann Behav Med. 2007;33:291–301. doi: 10.1080/08836610701359860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zautra AJ, Johnson LM, Davis MC. Positive affect as a source of resilience for women in chronic pain. J Consult Clin Psychol. 2005;73:212–220. doi: 10.1037/0022-006X.73.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stone AA, Neale JM, Cox DS, et al. Daily events are associated with a secretory immune response to an oral antigen in men. Health Psychol. 1994;13:440–446. doi: 10.1037//0278-6133.13.5.440. [DOI] [PubMed] [Google Scholar]
- 30.Cohen S, Alper CM, Doyle WJ, et al. Positive emotional style predicts resistance to illness after experimental exposure to rhinovirus or influenza A virus. Psychosom Med. 2006;68:809–815. doi: 10.1097/01.psy.0000245867.92364.3c. [DOI] [PubMed] [Google Scholar]
- 31.Fredrickson BL. What good are positive emotions? Rev Gen Psychol. 1998;2:300–319. doi: 10.1037/1089-2680.2.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Davis MC, Zautra AJ, Smith BW. Chronic pain, stress, and the dynamics of affective differentiation. J Pers. 2004;72:1133–1159. doi: 10.1111/j.1467-6494.2004.00293.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ong AD, Zautra AJ, Reid MC. Psychological resilience predicts decreases in pain catastrophizing through positive emotions. Psychol Aging. 2010 doi: 10.1037/a0019384. under editorial review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ong AD, Bergeman CS, Bisconti TL, Wallace KA. Psychological resilience, positive emotions, and successful adaptation to stress in later life. J Pers Soc Psychol. 2006;91:730–749. doi: 10.1037/0022-3514.91.4.730. [DOI] [PubMed] [Google Scholar]
- 35.Strand EB, Zautra AJ, Thoresen M, et al. Positive affect as a factor of resilience in the pain-negative affect relationship in patients with rheumatoid arthritis. J Psychosom Res. 2006;60:477–484. doi: 10.1016/j.jpsychores.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 36.Feldman-Barrett L, Gross J, Conner-Christensen T, et al. Knowing what you're feeling and knowing what to do about it: mapping the relation between emotion differentiation and emotion regulation. Cogn Emot. 2001;15:713–724. [Google Scholar]
- 37.McFarland C, Buehler R. The impact of negative affect on autobiographical memory: the role of self-focused attention to moods. J Pers Soc Psychol. 1998;75:1424–1440. doi: 10.1037//0022-3514.75.6.1424. [DOI] [PubMed] [Google Scholar]
- 38.Snow-Turek AL, Norris MP, Tan G. Active and passive coping strategies in chronic pain patients. Pain. 1996;64:455–462. doi: 10.1016/0304-3959(95)00190-5. [DOI] [PubMed] [Google Scholar]
- 39.Strahl C, Kleinknecht RA, Dinnel DL. The role of pain anxiety, coping, and pain self-efficacy in rheumatoid arthritis patient functioning. Behav Res Ther. 2000;38:863–873. doi: 10.1016/s0005-7967(99)00102-3. [DOI] [PubMed] [Google Scholar]
- 40.Karoly P, Ruehlman LS. Psychological “resilience” and its correlates in chronic pain: findings from a national community sample. Pain. 2006;123:90–97. doi: 10.1016/j.pain.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 41.Mikolajczak M, Roy E, Luminet O, de Timary P. Resilience and hypothalamic-pituitary-adrenal axis reactivity under acute stress in young men. Stress. 2008;11:477–482. doi: 10.1080/10253890701850262. [DOI] [PubMed] [Google Scholar]
- 42.Jensen MP, Turner JA, Romano JM. Self-efficacy and outcome expectancies: relationship to chronic pain coping strategies and adjustment. Pain. 1991;44:263–269. doi: 10.1016/0304-3959(91)90095-F. [DOI] [PubMed] [Google Scholar]
- 43.Bower JE, Moskowitz JT, Epel E. Is benefit finding good for your health? Pathways linking positive life changes after stress and physical health outcomes. Curr Dir Psychol Sci. 2009;18:337–341. [Google Scholar]
- 44.Cacioppo J, Reis H, Zautra AJ. Social resilience. Am Psychol. 2010 doi: 10.1037/a0021419. under editorial review. [DOI] [PubMed] [Google Scholar]
- 45.Davis MC, Zautra AJ, Reich JW. Vulnerability to stress among women in chronic pain from fibromyalgia and osteoarthritis. Ann Behav Med. 2001;23:215–226. doi: 10.1207/S15324796ABM2303_9. [DOI] [PubMed] [Google Scholar]
- 46.Wright LJ, Zautra AJ, Going S. Adaptation to early knee osteoarthritis: the role of risk, resilience, and disease severity on pain and physical functioning. Ann Behav Med. 2008;36:70–80. doi: 10.1007/s12160-008-9048-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Davis MC, Affleck G, Zautra AJ, Tennen H. Daily interpersonal events in pain patients: applying action theory to chronic illness. J Clin Psychol. 2006;62:1097–1113. doi: 10.1002/jclp.20297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Keyes CL. The black-white paradox in health: flourishing in the face of social inequality and discrimination. J Pers. 2009;77:1677–1706. doi: 10.1111/j.1467-6494.2009.00597.x. [DOI] [PubMed] [Google Scholar]
- 49.Gallo LC, Penedo FJ, Espinosa de los Monteros K, Arguelles W. Resilience in the face of disadvantage: do Hispanic cultural characteristics protect health outcomes? J Pers. 2009;77:1707–1746. doi: 10.1111/j.1467-6494.2009.00598.x. [DOI] [PubMed] [Google Scholar]
- 50.Sheffer CE, Cassisi JE, Ferraresi LM, et al. Sex differences in the presentation of chronic low back pain. Psychol Women Q. 2002;26:329–340. [Google Scholar]


