Abstract
Obesity in the sub-Saharan Africa region has been portrayed as a problem of affluence, partly because obesity has been found to be more common in urban areas and among the rich. Recent findings, however, reveal rising prevalence among the poor particularly the urban poor. A growing body of literature mostly in Western countries shows that obesity among the poor is partly the result of an obesogenic-built environment. Such studies are lacking in the African context. This study examines the characteristics of the local food environment in an urban poor setting in Accra, Ghana and further investigates the associated risk of obesity for residents. Data on the local food environment was collected using geographic positioning system (GPS) technology. The body mass indices (BMI) of females (15–49 years) and males (15–59 years) were calculated from measured weight and height. Data on the socio-demographic characteristics and lifestyle behaviors of respondents was also collected through a household survey. Spatial analysis tools were used to examine the characteristics of the local food environment while the influence of the food environment on BMI was examined using a two-level multilevel model. The measures of the food environment constituted the level 2 factors while individual socio-demographic characteristics and lifestyle behaviors constituted the level 1 factors. The local food environment in the study communities is suggestive of an obesogenic food environment characterized by an abundance of out-of-home cooked foods, convenience stores, and limited fruits and vegetables options. The results of the multilevel analysis reveal a 0.2 kg/m2 increase in BMI for every additional convenience store and a 0.1 kg/m2 reduction in BMI for every out-of-home cooked food place available in the study area after controlling for individual socio-demographic characteristics, lifestyle behaviors, and community characteristics. The findings of this study indicate that the local food environment in urban poor Accra is associated with increased risk of obesity through providing access to convenience stores. In order to reduce the risk of obesity in these urban poor communities, there is the need to regulate the availability of and access to convenience stores while also encouraging healthier offerings in convenience stores.
Keywords: Obesity, Urban poor, Food environment, Body mass index, Ghana
Introduction
The rise in the prevalence of obesity has become a major public health problem globally.1 Even in regions such as sub-Saharan Africa (SSA) where the prevalence is relatively low, there has been an increase in prevalence over the last three decades.2–4 While individual characteristics and behaviors such as genetic makeup, excess calorie consumption, and physical inactivity are among the factors that have been attributed to the rising prevalence of obesity, these proximal individual factors alone do not explain the rapid global increase in the prevalence of obesity over the last three decades.5–7 It is argued that the rapid increase in the prevalence of obesity is as a result of people responding normally to changes in the environment (distal factors) that encourages excess calorie consumption and sedentary lifestyles. 8,9
Obesogenic behaviors, particularly excess calorie consumption and physical inactivity become more common as countries develop and go through shifts in dietary pattern and physical activity. The nutrition transition first described by Popkin (1994)10 illustrates shifts in dietary patterns from periods of famine to periods of nutrition-related chronic diseases of lifestyle associated with the adoption of modern lifestyles that accompany socio-economic development, urbanization, and acculturation.2,11,12 Urbanization in sub-Saharan Africa has been accompanied by the availability of modern food items including sweetened carbonated soft drinks and fast foods, particularly in urban areas.2 Nutrition transition in Africa has been observed in countries such as South Africa in the Transition and Health during Urbanization of South Africans (THUSA) study. The THUSA study revealed decreased consumption of staple foods and plant-based proteins and increased consumption of energy dense snack-based foods, sweetened carbonated beverages, red meat, fast foods, and convenience foods.13 The nutrition transition in Africa is occurring along with the demographic (a shift from high mortality to improved lifestyle and health status) and epidemiologic (a change in disease pattern from infectious to chronic degenerative diseases) transitions.14 The simultaneous occurrence of the demographic and epidemiologic transitions together with the nutrition transition contributes to the increasing shift towards obesity and diet-related non-communicable diseases. 2
The increasing availability of energy dense foods has resulted in a “built environment” which has implications for obesity, physical activity, and dietary choices especially in poor areas.15,16 Research in developed countries including the USA, UK, and Canada has shown that conditions in the built environment are often associated with obesity especially in deprived and socio-economically disadvantaged areas.16–18 Such deprived areas typically lack access to healthy food options such as fresh fruits and vegetables, recreational facilities, and social structures to support a healthy and active lifestyle.16,19 Food deserts describe areas that lack access to affordable fruits, vegetables, whole grains, low fat milk, and other foods that make up a full range of a healthy diet or areas that provide an imbalance of food choices by offering less healthy foods.20 Food deserts tend to be common in socio-economically deprived areas and are often associated with poor diets, obesity, diabetes, and hypertension.18,21,22 The urban food environment is becoming more and more energy dense, offering poor and unhealthy options including fast, convenience, and processed foods. The proliferation of poor foodscapes in urban areas has resulted in the existence of “food swamps”.23 The combined existence of food deserts and food swamps is a major driver of the rising global obesity epidemic.
Research on the influence of conditions in the built environment including the food and physical activity environments is far advanced in Western countries,8 but this cannot be said of developing countries particularly in Africa. For the most part, research on obesity in sub-Saharan Africa has been primarily epidemiological,24 focusing on rates and predictors, individual characteristics and lifestyle behaviors in specific populations.25 The influence of conditions in the built environment on obesity has received limited research attention. In this paper, we examine the local food environment in an urban poor setting in Accra, Ghana and further investigate how the food environment constitutes a risk for obesity.
Methodology
Study Setting
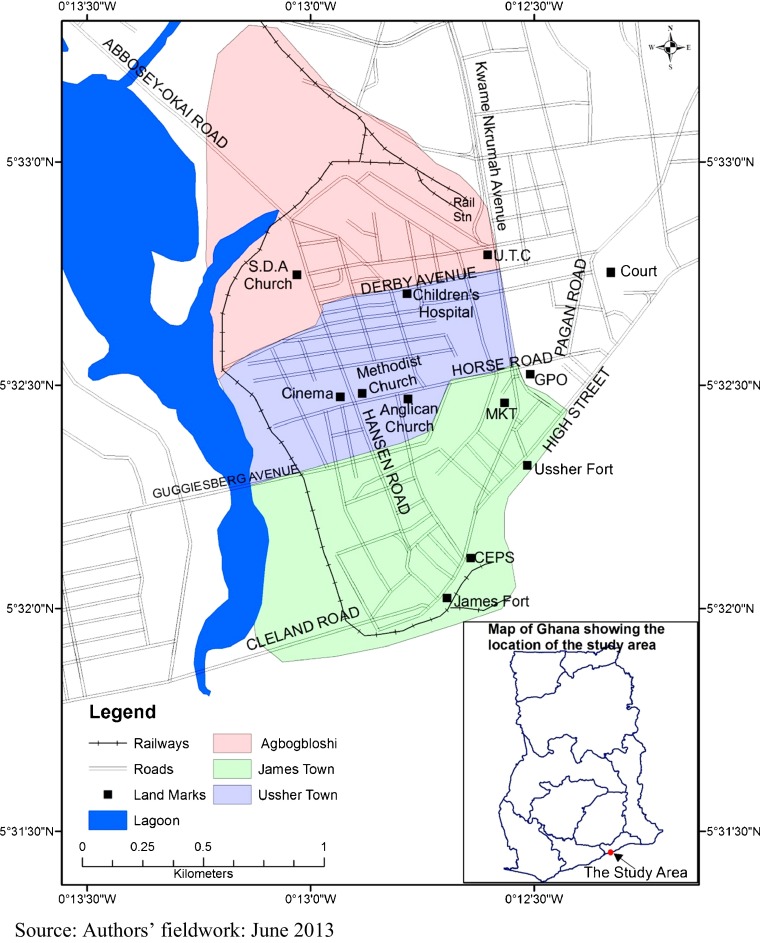
This study was conducted in three urban poor communities: James Town, Ussher Town, and Agbogbloshie all in Accra, Ghana (Fig. 1). The three communities are a typical representation of urban poor communities in Accra. James Town and Ussher Town are among the oldest communities in Accra and are currently ranked among the most densely populated communities in the city.26 James Town and Ussher Town are relatively stable traditional communities organized around social structures such as chieftaincy. These two communities are traditional Ga communities characterized by multiple generations of families living together in large family houses. Recently, people of other ethnicities have moved into these otherwise indigenous Ga communities. Agbogbloshie is also a densely populated suburb of Accra. It is a typical migrant community consisting of several population sub-groups and made up of several different ethnicities most of whom are from Northern Ghana. Some residents of Agbogbloshie trace their roots in the community back to the early 1960s,27 although Agbogbloshie generally has weaker social ties and less organized social structures than James Town and Ussher Town.
FIG. 1.
Location map showing the study area.
Typical of urban poor communities, the study area grapples with problems such as poor health, low levels of education, and high levels of fertility. The major income-generating activity in the study area is fishing; the men go fishing while the women smoke and sell the fish.28,29 Women also engage in other income-generating activities, mainly the preparation and sale of street foods including kenkey (a local staple food made from fermented maize dough) and petty trading. 30,31
Sampling Procedure
To enable easy canvassing during census and survey enumeration, the Ghana Statistical Service has created small nationwide divisions called enumeration areas (EAs).32 There were a total of 80 EAs in the three communities (48 in Usher Town, 24 in James Town, and 8 in Agbogbloshie) which make up the study area. Twenty-eight EAs (16 in Ussher Town, 8 in James Town, and 4 in Agbogbloshie) were systematically sampled from the 80 EAs. A household listing exercise was conducted in the 28 selected EAs. The resulting household listing was used as the sampling frame for the selection of households included in the study. Forty households were systematically sampled in each of the sampled EAs. Females and males aged 15–49 years and 15–59 years, respectively, in the selected households were recruited as eligible participants and interviewed.
Data
Data for this study was collected at the community and individual levels. The EAs served as the geographic scale at which the community level data were collected. Geographic positioning system (GPS) technology was used to collect data on the characteristics of the food environment. The point location of three types of food resources: (1) out-of-home cooked foods, (2) convenience stores, and (3) fruit/vegetable stands or sales points in the selected EAs were geocoded. The type of food(s) sold at each point location was also recorded. Out-of-home cooked foods denote already prepared ready-to-eat foods sold by food vendors. Convenience stores are small stores in the community where processed and pre-packaged foods such as polished rice, refined vegetable oil, and sweetened carbonated beverages are sold. Convenience stores do not typically carry perishable food items such as fruits and vegetables. Non-food items are also sometimes available in these stores. Fruit and vegetable stands or sales points are locations in the community where fruits and vegetables are sold. Data on the location, number, and characteristics of these three types of food resources were collected in the 28 EAs as features of the local food environment.
At the individual level, data on the socio-demographic characteristics and lifestyle behaviors of respondents were collected through a survey. The survey data collection was carried out between 25 November and 22 December 2011 under the second round of data collection for the Population, Health and Poverty Project which is a research project implemented by the Regional Institute for Population at the University of Ghana. The aim of the project is to study demographic, health, and environmental issues in an urban poor developing country context. The project is conducted in the three urban poor communities involved in this present study. Data collection for the project is done periodically at 18-month intervals.
Eligible individuals in the selected households were interviewed using a semi-structured questionnaire through interviewer administered face-to-face interviews. The question modules in the questionnaire included a community, physical activity, and lifestyle behavior module and a seven day dietary recall. The community module assessed crime, social cohesion, and trust among community members. The physical activity and lifestyle behavior modules which were based on the Global Physical Activity Questionnaire and the WHO STEPS approach assessed physical activity, smoking, and alcohol consumption. Dietary intake of the respondents was assessed using a 7-day dietary recall. Weight and height measurements of the respondents were taken using standard procedures.33,34 Weight was recorded to the nearest 0.1 kg using a calibrated Seca scale with respondents dressed in light clothing while height was recorded to the nearest 0.1 of a centimeter with respondents standing upright in the Frankfort horizontal position. The weight and height measures were used to calculate the BMI of the respondents. A total of 916 individuals were interviewed out of which 756 had valid BMI measures, and of these, 51 were underweight according to the standard WHO BMI classifications. The analysis for this paper is based on 657 individuals excluding those who were underweight (n = 51). This exclusion criterion was applied to minimize skewness and obtain a normal distribution on the dependent variable. Ethical approval for this study (# 056/11-12) was granted by the Noguchi Memorial Institute for Medical Research at the University of Ghana.
Variables
Dependent Variable
The outcome variable for this study is the BMI of the study participants which was used as a continuous variable. The BMI of the participants was obtained by dividing the weight (in kilograms) of the respondents by the square of their height (in meters). The BMI method is widely accepted for population level analysis and is used internationally as the standard for defining overweight and obesity in adult populations.35 BMI is a marker of general obesity36 and is the method commonly used to determine obesity in social science research37 even though the measure is criticized for lack of gender-, age-, and ethnicity-based cutoffs tailored to specific populations. 38
Independent Variables
The main independent variables were the measures of the characteristics of the food environment, specifically the number of out-of-home cooked food resources, the number of convenience stores, and the number of fruits and vegetable stands in each EA. The presence of a physical activity space was also included as an independent variable. In this study, physical activity space(s) denote places in the EA outside of people’s homes where community members engage in physical activity. These include both places designated for physical activity (e.g., football parks) and places which are not designated for physical activity but are often reported as being used for physical activity (e.g., the beach and streets/roads turned into a playing field). All such physical activity spaces in the community were geocoded. The EAs were grouped into two based on whether or not there is a physical activity space to examine the relationship between the presence (versus the absence) of a physical activity space and BMI.
Control Variables
The social characteristics of the community including trust among community members, social cohesion, and crime level were included in the analysis as community control variables. Population density per EA was also controlled for as a community control variable. Social cohesion was assessed using a measure of the degree to which respondents agree or disagree about members of the community coming together to help when there is a problem in the community on a scale of 1 (strongly disagree) to 4 (strongly agree). Individual responses were aggregated to the EA level. Social cohesion in the community was assessed as the mean of the EA aggregate value. Community crime level was measured on a scale of 1 (low) to 5 (high). Individual responses were aggregated to the EA level. Community crime level was measured as the mean of the aggregate for each EA. Trust among community members was measured by aggregating individual responses on how much members of the community can be trusted on a scale of 1 (low level of trust among community members) to 5 (high level of trust among community members).
At the individual level, the socio-demographic characteristics (including age, sex, marital status, level of education, type of occupation, and length of stay in the community) and lifestyle behaviors (including dietary diversity, physical activity, sedentary behavior, alcohol consumption, smoking, and rest) of the respondents were included in the analysis as control variables. Age was measured as completed years and used as a continuous variable. Participants were either male or female based on biological sex. Marital status had four categories of never married, married, cohabiting, and formerly married. To assess the influence of changes in dietary behavior as a result of in-migration and acculturation, the study participants were grouped into three categories based on how long they have stayed in the study area. The categories include those who have lived in the community since their birth, those who have lived in the community for less than or up to 10 years, and those who have lived in the community for more than 10 years. Some respondents had no formal education, others had completed primary school, junior secondary school, or senior secondary school while others have completed higher than secondary level education. Some respondents reported not having an occupation while others were professional workers, sales/service personnel, manual workers including those working in agriculture, and those in “other” occupational groupings including students and domestic workers.
Respondents’ physical activity behavior was assessed using a self-report of their work-related and leisure-time physical activity. Based on the intensity of the physical activity involved in the work respondents’ do, the respondents were grouped into those who are not working and those whose work involves no/low, moderate, or high physical activity. Similarly, respondents were grouped into those who did not engage in leisure-time physical activity, those who engaged in moderate and high leisure-time physical activity. Sedentary behavior among the participants was assessed based on the number of hours in a day spent being idle or in activities such as watching television. The number of hours respondents rested/slept a day was also analyzed and used as a continuous variable.
Respondents’ dietary behavior was assessed using their dietary diversity score. The score was computed based on respondents’ report of consuming foods from nine food groups in the last 7 days preceding the survey.39 Respondents smoking status was assessed in terms of frequency of smoking; there were four categories of those who have never smoked, those who smoke daily, those who smoked some days in the last 30 days preceding the survey, and those who smoke but have not smoked in the last 30 days preceding the survey. Alcohol consumption was assessed similarly with four categories of those who have never consumed alcohol, those who consumed alcohol in the last 24 h preceding the survey, those who consume alcohol but not in the last 24 h preceding the survey, and those who consume alcohol but not in the last 30 days preceding the survey.
Methods of Analysis
A combination of spatial and statistical analysis tools was used. The characteristics of the food environment were analyzed using spatial analysis tools including proximity, density and buffer analysis. The spatial data on the features of the food environment were combined with data on individual characteristics from the survey to examine the influence of the food environment on the risk of obesity in a multilevel analysis framework. A two-level random effects model was specified with the community/EA measures of the food environment serving as the main level 2 factors, and the individual characteristics serving as the level 1 factors. The multilevel model was specified in three steps. The first step in the process was the specification of the null model (model 1). The second model (model 2) examined the influence of the characteristics of the food environment controlling for other community variables while the final stage of model specification (model 3) builds on model 2 by including individual socio-demographic characteristics and lifestyle behaviors as individual control variables. Prior to specifying the multilevel models, a bivariate ordinary least squares (OLS) regression model was specified for each of the level 1 predictor variables against BMI to determine which variables were significantly related with BMI. The variables that were found to be significantly associated with BMI were further examined for multicollinearity. The results of the multilevel analysis are presented as beta coefficients and significance set at 95 % (p < 0.05). The spatial analysis was done using ArcGIS version 10.1 while the statistical analysis was carried out in Stata 12.
Results
Characteristics of the food environment
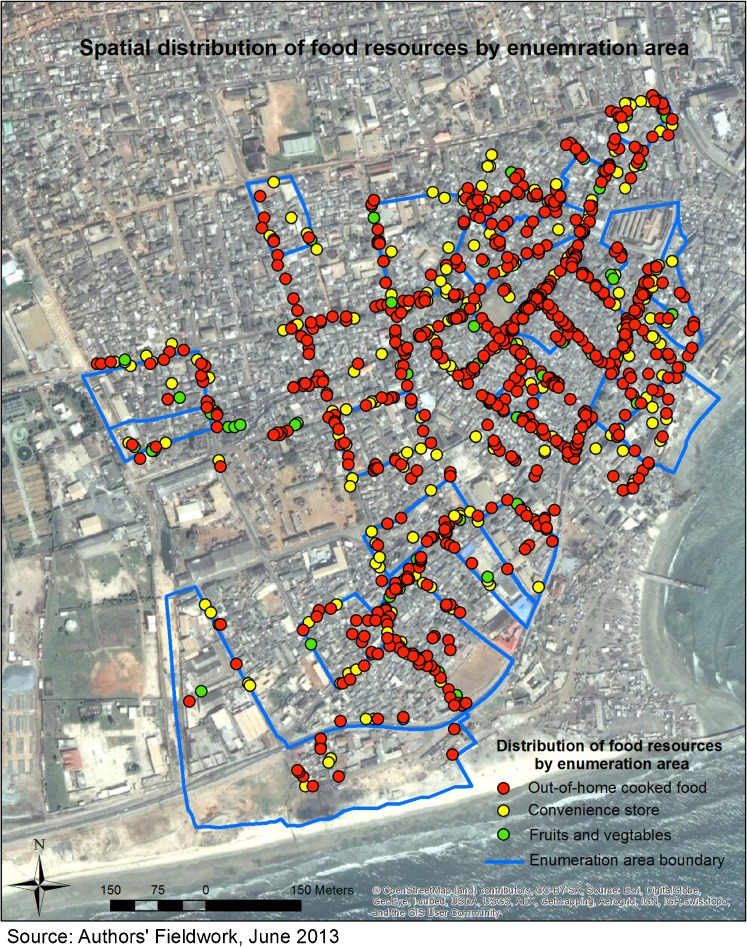
The distribution of the food resources shown in Fig. 2 shows an abundance of options for out-of-home cooked foods and convenience foods but limited options for fruits and vegetables. The results also show that the number of out-of-home food places outweigh that of convenience stores and fruit and vegetable stands/sales points. The distribution of the types of food resources by point location show close proximity of the different food resources to each other with some locations having all three types of food resources at the same location (Fig. 2).
FIG. 2.
Spatial distribution of out-of-home cooked foods, convenience stores and fruits and vegetables stands/sales point by EA.
The most common types of out-of-home cooked foods available in the study area include plain boiled rice, rice boiled with refined vegetable oil, fried rice1, waakye2, and jollof rice3. These rice dishes are mostly made from polished rice and sold with chicken, meat, or fish which are mostly frozen products fried with refined vegetable oil. The sauces that accompany the rice dishes are also prepared with refined vegetable oils, spices, and condiments. Another common category of out-of-home cooked foods available in the study area are local staple foods including fufu,4 banku5, and keneky6. Fufu is served with a variety of soups including tomato soup also called “light soup,” groundnut soup and palm nut soup. Banku and kenkey are typically served with fried fish and an uncooked sauce which is a blended mixture of pepper, tomato, onion, and salt. Banku and kenkey are also sometimes eaten with a stewed sauce or soup. Out-of-home cooked foods were found to be commonly available in the study area throughout the day. Residents are thus exposed to a diversity of out-of-home cooked foods including both healthy options such as staple foods made from whole grain and starchy roots and unhealthy options such as stir-fried polished rice dishes.
The food resources available at convenience stores in the study area can be broadly categorized into two groups: (1) those that require further processing before consumption and (2) those that do not require further processing before consumption. The groups of food resources that require further processing before consumption are foods that need to be cooked before they can be consumed. Such food items include uncooked polished rice, canned tomato paste, refined oils, and canned meat or canned fish products. These food types are processed to preserve and give them a long shelf life. Processing however affects the nutritional quality of these foods while increasing their caloric value. For instance, compared to unpolished rice, polished rice has less complex carbohydrates which increase the energy density of polished rice. The second group of foods which do not require processing before consumption include foods such as refined sugars, sweetened carbonated beverages, e.g., coca cola, white bread, biscuits, and snacks including fried and baked pastries. These food items have high caloric value and their consumption have implications for obesity.
Fruits and vegetables were the least common type of food resource in the study area. Fruits such as oranges, pineapple, water melon, apple, and black berries and vegetables such as tomatoes, onions, cabbage, and carrots were among the most common types of fruits and vegetables available in the study communities when fruits and vegetables were found.
Characteristics of Study Participants
The study participants were overweight on average with an average BMI of 25.58 kg/m2. Females had a higher BMI on average than their male counterparts (Table 1). Similarly, a higher proportion of females compared to males were overweight (27.04 versus 18.87 %) and a far higher proportion were obese compared to males (30.42 versus 4.64 %). Participants were aged about 31 years on average (Table 1). The sample consists of slightly more females than males. About two in five of the study participants have never been married while about a quarter were married. About every four in ten of the participants have lived in the study area since they were born while a little less than a third have lived in the community for less than or up to 10 years and about an equal proportion have lived in the community for more than 10 years. Almost half of the participants have completed junior high school while about a quarter have completed senior high school. On one hand, less than one tenth of the participants have completed tertiary level of education and on the other hand a similar proportion have not had any formal education. About one in ten of the participants reported not working in any occupation while about two fifths work as sales/service personnel and close to three in ten are involved in manual occupations including agriculture.
TABLE 1.
Community and individual level characteristics
| BMI distribution | |
|---|---|
| Continuous | Mean (standard deviation) |
| Total sample | 25.58 (6.00) kg/m2 |
| Females | 27.49 (6.88) kg/m2 |
| Males | 23.34 (3.69) kg/m2 |
| Overweight | Percentage |
| Total sample | 23.29 |
| Females | 27.04 |
| Males | 18.87 |
| Obese | Percentage |
| Total sample | 18.57 |
| Females | 30.42 |
| Males | 4.64 |
| Community/EA level characteristics | Mean (standard deviation) |
| Crime level | 3.37 (0.56) |
| Social cohesion | 2.73 (0.20) |
| Trust among community members | 2.33 (0.15) |
| Population density (people per square meter *100) | 8.22 (5.74) |
| Individual level characteristics | |
| Continuous variables | Mean (standard deviation) |
| Age | 31.45 (10.46) |
| Dietary diversity score | 6.88 (1.78) |
| Hours of rest a day | 7.45 (1.77) |
| Categorical Variables | Percentage |
| Sex | |
| Male | 45.97 |
| Female | 54.03 |
| Marital status | |
| Never married | 38.20 |
| Married | 24.66 |
| Cohabiting | 20.09 |
| Formerly married | 17.05 |
| Length of stay in the community | |
| Since birth | 43.23 |
| ≤10 years | 29.22 |
| >10 years | 27.55 |
| Highest level of education attained | |
| No education | 5.78 |
| Primary | 19.03 |
| Middle/Junior High School | 44.90 |
| Secondary/Senior High School | 25.72 |
| Tertiary | 4.57 |
| Occupation | |
| No occupation | 11.72 |
| Professional | 8.22 |
| Sales/Services | 42.77 |
| Manual | 28.01 |
| Other | 9.28 |
| Work-related physical activity | |
| Not working | 20.40 |
| Low activity | 27.70 |
| Moderate activity | 43.53 |
| Highly activity | 8.37 |
| Leisure-time physical activity | |
| Low activity | 64.23 |
| Moderate activity | 23.59 |
| High activity | 12.18 |
| Number of hours spent in sedentary activity | |
| <1 | 19.63 |
| 1–3 | 46.27 |
| >3 | 34.09 |
| Smoking status | |
| Never smoked | 82.65 |
| Smokes daily | 2.44 |
| Smoked some days in the last 30 days | 10.96 |
| Ever smoked but not in the last 30 days | 3.96 |
| Alcohol consumption | |
| Never consumed alcohol | 35.46 |
| Consumed alcohol in the last 24 h | 18.11 |
| Consumes alcohol but not in the last 24 h | 21.61 |
| Consumes alcohol but not in the last 30 days | 24.81 |
| Total % (N) | 100.0 (657) |
A small proportion (8 %) of the respondents reported that the work they do involves high levels of physical activity while a little over a quarter reported their work involving low levels of physical activity (Table 1). For about 44 % of the sample, their work involves moderate levels of physical activity. About two thirds of the respondents indicated that they do not engage in leisure-time physical activity while about a quarter engage in moderate energy tasking leisure-time physical activity. Only about 12 % of the participants reported engaging in leisure-time physical activities that involve high levels of energy. More than two fifths of the participants spend 1 to 3 h of the day in sedentary activity while about one third spend more than 3 h of the day being idle. Smoking among the study sample was low; more than four in five of the participants indicated that they have never smoked. Alcohol consumption on the other hand is more common compared to smoking.
The Food Environment and Obesity
The random effects component of the multilevel model (model 1 Table 2) shows that the BMI of the respondents is influenced by factors at both the community and individual levels. The results in model 2 shows that independent of individual characteristics and lifestyle behaviors, increasing number of out-of-home cooked foods is associated with a reduction in BMI. This relationship persisted even after the socio-demographic characteristics and lifestyle behaviors of the individuals were controlled for. Out-of-home cooked foods and convenience stores were observed to significantly influence BMI after controlling for individual and community characteristics (model 3 Table 2). The results show that each additional out-of-home cooked food place located in the EA decreases BMI by approximately 0.1 kg/m2 while each additional convenience store increases BMI by about 0.2 kg/m2. The number of fruit and vegetable sales point did not show a statistically significant association with BMI. The presence of a physical activity space in the EA was associated with a 0.2 kg/m2 reduction in BMI although this was not statistically significant. Increasing community crime level was found to be associated with a 1.2 kg/m2 increase in BMI.
TABLE 2.
Results of a random effects model examining the influence of the local food environment on BMI controlling for community characteristics and individual socio-demographic characteristics and lifestyle behaviors
| Model 1 (Null model) |
Model 2 (Unadjusted model) |
Model 3 (adjusted model) | |
|---|---|---|---|
| Fixed effects component | |||
| Community/EA (Level-2) factors | |||
| Number of out-of-home cooked foods | −0.090* | −0.075* | |
| Number of convenience stores | 0.202+ | 0.168* | |
| Number of fruit and vegetable sales point | 0.091 | 0.080 | |
| Presence of physical activity space [Absent] | −1.053 | −0.181 | |
| Crime level | 1.422+ | 1.190* | |
| Social cohesion | 0.556 | 0.757 | |
| Trust among community members | 2.865 | 2.616 | |
| Population density | 3.912 | 5.249 | |
| Individual (Level-1) factors | |||
| Age | 0.157*** | ||
| Sex [Male] | |||
| Female | 4.109*** | ||
| Marital status [Never married] | |||
| Married | −0.054 | ||
| Cohabiting | 0.453 | ||
| Formerly married | 0.457 | ||
| Length of stay in the community [Since birth] | |||
| ≤ 10 years | −1.730** | ||
| > 10 years | −0.493 | ||
| Highest level of education attained [No education] | |||
| Primary | 2.271* | ||
| Middle/Junior High School | 1.218 | ||
| Secondary/Senior High School | 1.360 | ||
| Tertiary | 1.882 | ||
| Occupation [No occupation] | |||
| Professional | 0.454 | ||
| Sales/Services | −0.257 | ||
| Manual | −0.970 | ||
| Other | −0.751 | ||
| Work-related physical activity [Not working] | |||
| Low activity | 0.424 | ||
| Moderate activity | 0.515 | ||
| Highly activity | 1.469 | ||
| Leisure-time physical activity [Low activity] | |||
| Moderate activity | 0.295 | ||
| High activity | −0.331 | ||
| Number of hours spent in sedentary activity [<1] | |||
| 1-3 | −0.078 | ||
| > 3 | 0.526 | ||
| Hours of rest a day | 0.158 | ||
| Dietary diversity score | 0.190 | ||
| Alcohol consumption [Never consumed alcohol] | |||
| Consumed alcohol in the last 24 h | −0.178 | ||
| Consumes alcohol but not in the last 24 h | −0.101 | ||
| Consumes alcohol but not in the last 30 days | 0.231 | ||
| Smoking status [Never smoked] | |||
| Smokes daily | −0.577 | ||
| Smoked some days in the last 30 days | −1.346+ | ||
| Ever smoked but not in the last 30 days | −0.278 | ||
| Random effects component | |||
| Intra-EA variance | 1.480 | 1.494 | 0.479 |
| Individual variance | 34.723 | 34.549 | 26.994 |
+ P < 0.10;*P < 0.05;**P < 0.01;***P < 0.001
Of all the individual characteristics included in the model, age, sex, length of stay in the community, and level of education were the only significant predictors of BMI (model 3 Table 2). Each additional increase in the age of respondents was associated with an approximate 0.2 kg/m2 increase in their BMI. Compared to being a male, being a female was associated with a 4.1 kg/m2 increase in BMI. Having lived in the community for less than or up to 10 years was associated with a 1.7 kg/m2 reduction in BMI compared to having lived in the community since birth. The results with regards to education reveals a 2.3 kg/m2 increase in BMI for those who have completed primary level education compared to their counterparts who have no formal education (model 3 Table 2).
Discussion
The distribution of food resources, particularly the abundance of out-of-home cooked foods is a characteristic feature of the food environment in urban poor communities. In the current study, the local food environment presents more options for high caloric foods from convenience stores and prepared food stands and limited options for foods such as fruits and vegetables. A similar pattern of distribution of food resources has been found in both developed and developing country context. Bodor et al. (2010)40 found that in New Orleans, households tended to have much greater number of small food stores and convenience foods in their neighborhoods than supermarkets. Similarly, in other urban poor communities in Africa such as informal settlements in black South Africa, Micklesfield et al. (2013)41 report that informal food vendors who sell less varied and inexpensive food of poor quality are the most convenient places to obtain out-of-home cooked food. A previous study conducted in the same area as the current study revealed that 30 % of calories consumed by respondents were from street foods,30 indicating that street foods is a key source of respondents’ caloric needs. This food resource distribution bears on the findings at the multilevel stage of the analysis where increasing number of convenience stores was found to be associated with an increase in BMI. The food environment in the study area may contribute to the obesity burden by providing access to energy dense food options such as convenience foods. 3
The study findings support the hypothesized positive relationship between convenience stores and BMI. The food resources available in convenience stores are mostly processed foods with high caloric value.42 These foods are typically obesogenic and this may explain why having more convenience stores in the study area is associated with increasing BMI. In urban poor areas such as the setting for this study, the availability of convenience foods increases the susceptibility of residents to obesity. This is because in such areas, convenience foods tend to be more common and less expensive than fresh food options such as fruits and vegetables.42–44 The limited options for healthy foods and the availability and affordability of unhealthy options such as convenience foods potentially explain why increasing number of convenience stores in the study area contribute to increasing BMI.
The relationship between out-of-home cooked foods and BMI was opposite of what was expected. Instead of a positive relationship between increasing number of out-of-home cooked food places and BMI, a reverse relationship was found. Out-of-home cooked foods often contribute to weight gain and obesity because these foods are generally more salty, fatty, energy dense and of less nutritional quality compared to home cooked foods.45 However, the inverse relationship between the number of out-of-home cooked food places and BMI found in this study suggests that increasing number of out-of-home cooked food places may not necessarily contribute to weight gain as has been reported in other studies. 25
The out-of-home cooked foods available in the study area consist of a variety of different food types including traditional staple foods and western type foods. Most of the traditional staple foods are made from whole unpolished ingredients which may make them less obesogenic.46 Also, even though the out-of-home cooked foods are being sold commercially, their preparation may not be different from how home cooked foods are prepared especially in the context of the study area. The out-of-home cooked foods were also prepared with ingredients used for home food preparation. The out-of-home cooked foods in the study area may thus not have obesogenic characteristics typical of commercially prepared foods. There is the need for further research to examine the relationship between out-of-home cooked foods and obesity among the study population. Such studies should focus on examining the caloric and nutritional composition of the out-of-home cooked foods available in the study area and whether or not these foods contribute to weight gain.
The presence of a physical activity space was associated with a reduction in BMI although this relationship was not statistically significant. This finding is similar to the findings of Mendes et al. (2013)47 among an urban population in Belo Horizonte in Brazil. In their study, Mendes et al. found that even though the presence of parks/public squares/places for practicing physical activity was associated with lower prevalence ratios for overweight/obesity, the relationship was not statistically significant. In the current study, crime level was found to be a significant predictor of BMI as has been reported in several other studies.17,43 This finding, however, contradicts that of a study conducted among adults in Nigeria where perception of high crime rate was not significantly related to overweight among participants who resided in neighborhoods of low socio-economic status. 48
The length of stay at a host location is an important determinant of the relationship between migration and health-related outcomes such as obesity49 and is often used as a surrogate measure of acculturation. Migrants from low and middle income countries who move to high income countries appear to be more susceptible to overweight and obesity than their local counterparts.50 In sub-Saharan Africa, people who move from a rural area to a more urbanized area have been found to be at higher risk of obesity.25 Weight gain among migrants appear to increase significantly over 10–15 years post migration.49 The findings of this study support the relationship between migration and obesity. Individuals who have moved into and stayed in the study area for less than or up to 10 years had significantly lower BMI than those who have lived in the study area since birth.
This study is among few studies that examines the relationship between the food environment and obesity in the sub-Saharan African context. The results suggest that conditions in the local environment contribute to increasing BMI in urban poor settings. The result may be applicable to other similar urban poor settings in sub-Saharan Africa. The study findings could have been influenced by a number of limitations that are worth noting. Firstly, the study cannot establish causation due to the use of cross sectional data. The results thus establish associations rather than causation. Secondly, the study area is fairly homogenous, thus there may not be large variations among the EAs. Thirdly, the number of Level 2 units is small (N = 28) and may not be large enough to detect significant effects. Additionally, the distance from each respondent to various food resource and physical activity locations could not be determined because their exact location in the EA was unknown even though the EA in which they reside was known. These limitations notwithstanding, the findings from this study provide evidence that characteristics of the food environment are associated with BMI in the sub-Saharan African context. Future monitoring of the food and built environment is critical to understand both the trends in these environmental changes as well as longer-term effects of exposure.
Conclusion
The results of this study demonstrate that beyond individual characteristics, community characteristics contribute to body mass index among urban poor residents of Accra. The findings of this study affirm the stance that obesity is an outcome of a complex interaction between factors operating at different levels, at the community and individual levels in the case of this study. Research on obesity and interventions aimed at reducing obesity in sub-Saharan Africa, particularly in urban poor settings, needs to focus not only on individual characteristics but also on factors in the community environment that increases the risk of obesity.
Acknowledgments
The authors are grateful to the International Development Research Centre (IDRC) for funding support through the African Adaptation Research Centre Initiative grant awarded to the Regional Institute for Population Studies at the University of Ghana (Climate Change Adaptation Research Training Capacity for Development (CCARTCD) Project. Component Number: 106548-001.). We are also grateful to the Carolina Population Center for institutional support. We are especially grateful to Professor Phil Morgan (Director), Professor Carolyn Halpern (Director, Training Program) and Jan Hendrickson-Smith (Associate Director of Training Program) of the Carolina Population Center at the University of North Carolina, Chapel Hill. Many thanks to Philip McDaniels, GIS Librarian at the Davis Library, at The University of North Carolina, Chapel Hill for immense technical support with the spatial data analysis. We would also like to thank Charles Som for technical guidance on the spatial data collection, the team of fieldworkers who helped with data collection, and the respondents who participated in the study.
Footnotes
Boiled rice stir-fried with vegetables, sausage and eggs
Rice and beans boiled together
Rice cooked in tomato sauce
A pounded starchy staple made from plantain and cassava
Cooked corn and cassava dough
Steamed corn dough
Contributor Information
Fidelia A. A. Dake, Email: phydeliadake@gmail.com, Email: faadake@st.ug.edu.gh
Amanda L. Thompson, althomps@email.unc.edu
Shu Wen Ng, Email: shuwen@unc.edu.
Samuel Agyei-Mensah, Email: samensah@ug.edu.gh.
Samuel N. A. Codjoe, Email: scodjoe@ug.edu.gh
References
- 1.World Health Organization. Controlling the global obesity epidemic. Available at http://www.who.int/nutrition/topics/obesity/en/. Accessed 05 Aug. 2015.
- 2.Steyn PN, Mchiza ZJ. Obesity and the nutrition transition in sub-Saharan Africa. Ann N Y Acad Sci. 2014;1311:88–101. doi: 10.1111/nyas.12433. [DOI] [PubMed] [Google Scholar]
- 3.Caballero B. The global epidemic of obesity: an overview. Epidemiol Rev. 2007;29:1–5. doi: 10.1093/epirev/mxm012. [DOI] [PubMed] [Google Scholar]
- 4.Semba RD. Nutrition and Ophthalmology. Totowa, New Jersey: Humana Press Inc.; 2007. pp. 219–40. [Google Scholar]
- 5.Huang TT-K, Glass TA. Transforming research strategies for understanding and preventing obesity. JAMA. 2008;300:1811–3. doi: 10.1001/jama.300.15.1811. [DOI] [PubMed] [Google Scholar]
- 6.Cohen-Cole E, Fletcher JM. Is obesity contagious? Social networks vs. environmental factors in the obesity epidemic. J Health Econ. 2008;27:1382–7. doi: 10.1016/j.jhealeco.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Tremblay A, Perusse L, Bouchard C. Energy balance and body weight stability: impact of gene-environment interactions. Br J Nutr. 2004;92(Suppl 1):S63–6. doi: 10.1079/BJN20041144. [DOI] [PubMed] [Google Scholar]
- 8.Feng J, Glass AT, Curriero FC, Stewart FW, Schwartz SB. The built environment and obesity: a systematic review of the epidemiologic evidence. Health Place. 2010;16:175–90. doi: 10.1016/j.healthplace.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Hill JO, Peters CJ. Environmental contributions to the obesity epidemic. Science. 1998;280:1371–4. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- 10.Popkin BM. The nutrition transition in low-income countries: an emerging crisis. Nutr Rev. 1994;52:285–98. doi: 10.1111/j.1753-4887.1994.tb01460.x. [DOI] [PubMed] [Google Scholar]
- 11.Popkin BM. An overview of the nutrition transition and its health implications: the bellagio meeting. Public Health Nutr. 2002;5:93–103. doi: 10.1079/phn2001280. [DOI] [PubMed] [Google Scholar]
- 12.Voster HH. The emergence of cardiovascular disease during urbanization of Africans. Public Health Nutr. 2002;5:239–43. doi: 10.1079/phn2001299. [DOI] [PubMed] [Google Scholar]
- 13.Vorster HH, Kruger A, Margetts BM. The nutrition transition in Africa: can it be steered into a more positive direction? Nutrients. 2011;3:429–41. doi: 10.3390/nu3040429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.BeLue R, Okoror AT, Iwelunmor J, et al. An overview of cardiovascular risk factor burden in sub-Saharan African countries: a socio-cultural perspective. Global Health. 2009;5:10. doi: 10.1186/1744-8603-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ding D, Gebel K. Built environment, physical activity, and obesity: what have we learned from reviewing the literature? Health Place. 2012;18:100–5. doi: 10.1016/j.healthplace.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 16.Papas MA, Alberg AJ, Ewing R, Helzlsouer JK, Gary TL, Klassen AC. The built environment and obesity. Epidemiol Rev. 2007;29:129–43. doi: 10.1093/epirev/mxm009. [DOI] [PubMed] [Google Scholar]
- 17.Gordon-Larsen P, Nelson CM, Page P, Popkin BM. Inequality in the built environment underlies key health disparities in physical activity and obesity. Pediatrics. 2006;117:417–25. doi: 10.1542/peds.2005-0058. [DOI] [PubMed] [Google Scholar]
- 18.Cummins S, Macintyre S. Food environments and obesity-neighborhood or nation? Int J Epidemiol. 2006;35:100–4. doi: 10.1093/ije/dyi276. [DOI] [PubMed] [Google Scholar]
- 19.Ali AT, Crowther NJ. Factors predisposing to obesity: a review of the literature. JEMDSA. 2009;14(2):81–4. [Google Scholar]
- 20.Reel JJ, Badger BK. From food deserts to food swamps: health education strategies to improve food environments in urban areas. J Obes Weight Loss Ther. 2014;S4:002. [Google Scholar]
- 21.Salois MJ. Obesity and diabetes, the built environment and the ‘local’ food economy in the United States, 2007. Econ Hum Biol. 2012;10:35–42. doi: 10.1016/j.ehb.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 22.Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place. 2009;15:491–5. doi: 10.1016/j.healthplace.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fielding EJ, Simon PA. Food deserts or food swamps? Arch Intern Med. 2011;171(13):1171–2. doi: 10.1001/archinternmed.2011.279. [DOI] [PubMed] [Google Scholar]
- 24.Scott A, Chinwe SE, Clottey NE, Thomas JG. Obesity in sub-Saharan Africa: development of an ecological theoretical framework. Health Promot Int. 2012;28(1):4–15. doi: 10.1093/heapro/das038. [DOI] [PubMed] [Google Scholar]
- 25.Abubakari RA, Lauder W, Agyemang C, Jones M, Kirk A, Bhopal RS. Prevalence and time trends in obesity among adult West African populations: a meta-analysis. Obes Rev. 2008;9:297–311. doi: 10.1111/j.1467-789X.2007.00462.x. [DOI] [PubMed] [Google Scholar]
- 26.Mahama SA, Acheampong AT, Peprah OB, Boafo AY. Preliminary report for Ga Mashie urban design lab. Millennium Cities Initiative. The Earth Institute at Columbia University and The University of Ghana. 2011.
- 27.Codjoe SNA, Owusu G, Burkett V. Perception, experience, and indigenous knowledge of climate change and variability: the case of Accra, a sub-Saharan African city. Reg Environ Chang. 2014;14:369–83. doi: 10.1007/s10113-013-0500-0. [DOI] [Google Scholar]
- 28.Ghana Statistical Servvice. 2014. 2010 Population and Housing Census. District Analytical Report, Accra Metropolitan. Available at [http://www.statsghana.gov.gh/docfiles/2010_District_Report/Greater%20Accra/AMA.pdf]. Accessed on 6 Aug. 2015.
- 29.Razzu G. Urban redevelopment, cultural heritage, poverty and redistribution; the case of Old Accra and Adawaso House. Habitat Int. 2005;29:399–419. doi: 10.1016/j.habitatint.2003.12.002. [DOI] [Google Scholar]
- 30.Maxwell M, Levin C, Amar-Klemesu M, Ruel M, Morris S, Ahiadeke C. Urban livelihoods and food and nutrition security in Greater Accra, Ghana. International Food Policy Research Institute, Noguchi Memorial Institute for Medical Research and The World Health Organization. 2000.
- 31.Levin CE, Ruel MT, Morris SS, Maxwell DG, Armar-Klemesu M, Ahiadeke C. Working women in an urban setting: traders, vendors and food security in Accra. World Dev. 1999;27(11):1977–91. doi: 10.1016/S0305-750X(99)00096-0. [DOI] [Google Scholar]
- 32.Weeks JR, Getis A, Hill AG, Agyei-Mensah S, Rain D. Neighborhoods and fertility in Accra, Ghana: an AMEOBA-based Approach. Ann Assoc Am Geogr. 2010;100(3):558–78. doi: 10.1080/00045601003791391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sultana T, Karim MN, Ahmed T, Hossain MI. Assessment of under nutrition of Bangladeshi adults using anthropometry: can body mass index be replaced by mid-upper-arm-circumference? PLoS One. 2015;2015:e0121456. doi: 10.1371/journal.pone.0121456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luo X, Wang Y, Wang Z, et al. The mediating effect of body mass index on the relationship between cigarette smoking and atopic sensitization in Chinese adults. Int J Environ Res Public Health. 2015; 12(3): 3381–94. [DOI] [PMC free article] [PubMed]
- 35.World Health Organization. Obesity and Overweight. 2006. Available at http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed 17 Oct. 2008.
- 36.Steyn K, Damasceno A, et al. Lifestyle and related risk factors for chronic diseases. In: Jamison DT, Feachem RG, Makogoba WM, et al., editors. Disease and Mortality in Sub-Saharan Africa. Washington DC: The World Bank; 2006. pp. 247–64. [PubMed] [Google Scholar]
- 37.Faskunger J, Eriksson U, Johansson S, Sundquist K, Sundquist J. Risk of obesity in immigrants compared with Swedes in two deprived neighborhoods. BMC Public Health. 2009 doi: 10.1186/1471-2458-9-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bhurosy T, Jeewon R. Pitfalls of using body mass index (BMI) in assessment of obesity risk. Curr Res Nutr Food Sci. 2013;1(1):71–6. doi: 10.12944/CRNFSJ.1.1.07. [DOI] [Google Scholar]
- 39.Kennedy G, Ballard T, Dop M. Guidelines for measuring household and individual dietary diversity. Nutrition and Consumer Protection Division, Food and Agriculture Organization of the United Nations. 2010:1–60.
- 40.Bodor JN, Rice JC, Farley TA, Swalm MC, Rose D. The association between obesity and urban food environments. J Urban Health. 2010;87(5):771–81. doi: 10.1007/s11524-010-9460-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Micklesfield LK, Lambert EV, Hume JD, et al. Socio-cultural, environmental and behavioral determinants of obesity in black South African women. Cardiovasc J Afr. 2013;24(9/10):369–75. doi: 10.5830/CVJA-2013-069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Renzaho A. Fat, rich and beautiful: changing socio-cultural paradigms associated with obesity risk, nutritional status and refugee children from sub-Saharan Africa. Health Place. 2004;10:105–13. doi: 10.1016/S1353-8292(03)00051-0. [DOI] [PubMed] [Google Scholar]
- 43.Nugent R. Chronic disease in developing countries: health and economic burden. Ann NY Acad Sci. 2008;1136:70–9. doi: 10.1196/annals.1425.027. [DOI] [PubMed] [Google Scholar]
- 44.Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93:S9–30. doi: 10.1210/jc.2008-1595. [DOI] [PubMed] [Google Scholar]
- 45.Finkelstein EA, Ruhm CJ, Kosal KM. Economic causes and consequences of obesity. Annu Rev Publ Health. 2005;26:239–57. doi: 10.1146/annurev.publhealth.26.021304.144628. [DOI] [PubMed] [Google Scholar]
- 46.Popkin BM, Adair SL, Ng SW. Then and now: global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70(1):3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mendes LL, Nogueira H, Padez C, Ferrao M, Valesquez-Melendez G. Individual and environmental factors associated for overweight in urban Brazilian Population. BMC Public Health. 2013;13:988. doi: 10.1186/1471-2458-13-988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Oyeyemi AL, Adegoke BO, Oyeyemi AY, Deforche B, Bourdeauhuji DI, Sallis FJ. Environmental factors associated with overweight among adults in Nigeria. Int J Behav Nutr Phys Act. 2012;9:32. doi: 10.1186/1479-5868-9-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Delavari M, Sonderlund LA, Swinburn B, Mellor D, Renhazo A. Acculturation and obesity among migrant populations in high income countries—a systematic review. BMC Public Health. 2013;13:458. doi: 10.1186/1471-2458-13-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gadd M, Sundquist J, Johansson S. Do migrants have an increased prevalence of unhealthy behaviors and risk factors for coronary heart disease? Eur J Cardiovasc Prev Rehabil. 2005;12(6):535–41. doi: 10.1097/00149831-200512000-00004. [DOI] [PubMed] [Google Scholar]