Abstract
The objective of this study was to examine the association between externalizing behaviors and indirect violence exposure, assessed both within the household and at the community level, as well as the interaction effect of indirect and direct violence exposure. A sample of parents of children ages 4–15 who have not been referred or enrolled in child welfare (n = 82) were recruited from the greater New Orleans community. Externalizing behavior was assessed with the Child Behavior Checklist (CBCL). The child’s indirect exposure to violence included witnessing community violence, witnessing physical assault, and witnessing fighting or domestic violence at home. Direct exposure to violence included the child experiencing physical aggression from a caregiver. All assessments were based on caregiver reports. To decrease potential for confounding, children were matched for analysis based on age, Hurricane Katrina exposure, and their propensity to be exposed to high indirect violence. Cumulative indirect exposure to violence was significantly positively correlated with CBCL scores. After controlling for key covariates, CBCL externalizing T score increased significantly by approximately 1.25 points for each level increase in indirect violence exposure (β = 1.25, SE = 0.57, p = 0.027). There also was a significant interaction between indirect and direct exposure to violence in the association with CBCL score (β = −0.08, SE = 0.03, p = 0.002). These findings extend previous research by demonstrating that exposure to both direct and cross-contextual indirect violence influences externalizing behaviors in children. Additionally, the findings suggest that community and household social environments are both important targets for interventions designed to decrease externalizing behaviors and improve long-term outcomes for youth at risk of exposure to violence.
Keywords: Childhood exposure to violence, Cumulative exposure to violence, Indirect exposure to violence, Direct exposure to violence, Community violence, Household violence, Child physical aggression, Child externalizing behaviors
Background
Up to 30 % of low-income children exhibit clinical levels of externalizing behaviors,1 which include aggression, irritability, impulsivity, poor emotional control, rule breaking, and increased risk of interpersonal difficulties.2,3 This high prevalence rate is concerning as these behaviors are consistently associated with both short- and long-term negative outcomes. Externalizing behavior in youth is associated with negative outcomes such as decreased effortful control,4 peer rejection,5 and academic underachievement3 in cross-sectional studies. Longitudinal studies have shown that children who exhibit consistent patterns of externalizing behaviors at an early age are at an increased risk for developing conduct disorder and persistent antisocial behaviors,6 high school dropout,7 perpetration of violence,8 and substance abuse9 later in life.
Exposure to violence is an established risk factor associated with elevated externalizing and the related negative developmental trajectories.10,11 Children can be exposed to violence across multiple socio-ecological contexts including in the neighborhood, school, and home.12 In the home, child maltreatment, including neglect, as well as physical and psychological aggression, has consistently been associated with elevated aggressive and externalizing behavior in children and youth.13–17 Even physical aggression by parents that does not rise to the level of abuse, such as corporal punishment, has been associated with increased externalizing, delinquent, and antisocial behavior in childhood and into adulthood.18 While children who act out are at increased risk for experiencing corporal punishment, those who experience corporal punishment are also more likely to act out aggressively.19–21 Many longitudinal studies have demonstrated that the use of corporal punishment raises risk for subsequent increased child aggression, even after controlling for the child’s prior aggressive behavior and other important confounders.22–26
Indirect exposure to violence in childhood plays a key role in the development of externalizing behavior as well. Witnessing violence and aggression in the home is a major risk factor for child aggression and antisocial behavior.17,27–30 Children who live in homes with intimate partner violence (IPV), as well as other physical and verbal fighting in the home between family members, have higher rates of externalizing behaviors as well as clinical disorders.27,28,30–34 Emotion regulation and effortful control, two neurocognitive outcomes linked to externalizing behavior, are also compromised by IPV, with evidence suggesting that parenting can mediate this effect.35 Such effects may be long lasting, with adults who were exposed to IPV and/or experienced physical maltreatment in childhood at increased risk for perpetrating IPV in adulthood.32 More recent studies suggest that beyond behavior, violence exposure within the home may have an impact on children even at the cellular level.36,37
Beyond the family context, there is evidence that indirect exposures to neighborhood-based violence, including witnessing physical assault, shootings, and murder, are associated with externalizing behaviors in youth.38–40 Violence exposure within the neighborhood context including witnessing assault and murder is a predictor of externalizing behaviors in youth, poorer academic achievement, and cognitive difficulties.38–40 Additionally, even if a child has not directly witnessed neighborhood violence, a growing body of evidence shows that parents who witness neighborhood violence are more likely to experience distress, trauma symptoms, and depression, which are linked to child behavior problems via diminished maternal psychological functioning.41–44 Taken together, these studies suggest that violence exposure in a range of different contexts influences child externalizing.
Prior to turning 18 years of age, nearly 66 % of the population in the USA has experienced more than one type of violence, especially in the home.12,45,46 Exposure to one type of violence increases the odds of exposure to other types of violence.47 Dong and colleagues found that a history of physical abuse increased a child’s odds of experiencing another form of abuse from 2.5 (child sexual abuse) to 6.3 (emotional abuse) times.46 Furthermore, children exposed to IPV are more likely to experience direct physical aggression by a caregiver as well.22,48–53 Hence, exposure to one type of direct or indirect violence in the home increases the risk of exposure to other types.
Childhood exposure to violence is often experienced across contexts.54–57 Despite this, very few studies have examined the cumulative impact of youth exposure to cross-contextual (e.g., neighborhood and household violence) violence for children on youth behavior. Even less research has examined these cumulative cross-contextual factors in community-recruited children who have not been referred or enrolled in child welfare. This study is unique in that it explores the association between externalizing behaviors and cross-contextual indirect and direct violence exposure, defined as witnessing and experiencing violence respectively, within a high risk, hard to access, community-recruited sample of Black youth. Research focused on the relationship between exposure to single forms of violence and negative outcomes in children is common.12 Although it is likely that both direct and indirect violence exposures across multiple contexts may contribute both independently and interactively to behavioral outcomes specifically in youth, particularly externalizing behaviors, few studies have directly tested this theory.58–61 Incorporation of such a cumulative risk approach62 into our understanding of the impact of violence exposure on children’s health is paramount. The present analysis builds upon the existing literature linking independent violence exposures to externalizing and examines instead the combined impact of indirect violence exposures across individual, family, and neighborhood contexts. Further, the study explores the differential impact of indirect violence exposure among those who experience direct violence exposure.
Methods
Sample
Children, ages 5–15 years old, were recruited from the greater New Orleans, LA, area to take part in a cross-sectional study designed to examine the association of neighborhood and family conditions on child health (N = 120). Families were recruited through schools and street outreach techniques, including ethnographic mapping and targeted sampling.63 Recruitment neighborhoods were identified using the community identification process, a mapping method to record epidemiological indicators of the prevalence and incidence of community violence and other selected social and health conditions.64 Interested families contacted the research site to schedule an appointment.
The sample was restricted to Black children as the overarching goal of the parent study was to take the approach of race and class as independent and interactive factors that may play a role in health disparities and in this case, in child behavioral outcomes. One such approach in this framework is to examine socioeconomic and other risk factors within racial groups,65 which was done in our case. Furthermore, given the substantial percentage of Black participants in the cohort (>95 % Black), between-racial comparisons were impossible.
The propensity for being exposed to violence was estimated by propensity scores,66 calculated by obtaining the predicted probability of exposure to any secondary violence (as described below), based on potential confounders such as household socioeconomic status (maternal education and income), marital status, household chaos, maternal and child age, sex, and maternal adverse childhood life events. Children were matched 2:1, based on age within a year, exposure to Hurricane Katrina, and propensity score within 0.05 caliper. The final matched sample included in this analysis was 82 children based on matched pairs and externalizing behavior data availability. Children without externalizing behavior data (n = 9) did not differ significantly (p > 0.05) from children with data on these measures based on potential confounders or predictors of telomere length.
Data
Maternal caregivers provided information about multiple levels of the child’s social ecology (i.e., household and neighborhood) using an interview-assisted computer survey administered face-to-face at the research site (Questionnaire Development System, QDS, Nova Research, Bethesda, MD). Trained interviewers recorded oral responses on the computer.
Measures
Child Externalizing:
The primary outcome of interest was externalizing behaviors, assessed with the Child Behavior Checklist (CBCL).67 Chronbach’s alpha for the externalizing behavior scales is .94 and the test-retest reliability of r = 0.92.67 The CBCL is completed by a parent or caregiver who rates the presence and frequency of certain behaviors on a three-point scale ranging from 0 (not true) to 2 (often true). The time period is the last 6 months for children ages 6–18, and 2 months for children ages 18 months−5 years. This standardized instrument yields scores on two broad-band scales of internalizing and externalizing, scores on DSM-IV-oriented scales, and empirically based syndrome scales that reflect emotional and behavioral problems and symptoms. Externalizing behaviors include attention problems, aggressive behavior, and rule-breaking actions. Behavior scales yield a score of total behavioral problems. Scores are summed and then converted to normalized T scores.67 The T score for externalizing behavior was examined as a continuous variable.
Violence Exposure
Indirect Exposure:
Indirect exposure to violence was based on reports of witnessed violence in the community and home. This was determined by five dicohotomous items adapted from the minor and major life events from the Preschool Age Psychiatric Assessment (PAPA)68 including whether the child had witnessed: community violence; someone get killed, hurt very badly, or die; physical assault resulting in injury or death of someone close to him/her including the primary caregiver; physical or verbal fighting at home; or a friend or family member get hurt or mistreated.
Direct Exposure:
The Conflict Tactics Scale—parent child version (CTSPC), a well-validated instrument for measuring physical aggression against children,69 was used to measure direct violence exposure. The caregiver was asked if she had shaken, hit on the bottom with a hard object, spanked, slapped, or pinched the child. For each of these items, the caregiver indicated if she had used the method: 0 = never, 1 = once in the past year, 2 = twice in the past year, 3 = three to five times in the past year, 4 = six to 10 times in the past year, 5 = 11 to 20 times in the past year, 6 = more than 20 times in the past year, or 7 = yes but not in the past year. Items scored as 7 = yes but not in the past year were recoded as 0, and mean scores for all items were calculated and then added for a total score between 0 and 75.
The primary exposure of interest was indirect (witnessing) exposure to violence for the child. Direct (experiencing) exposure to violence was considered a key predictor of externalizing behavior and also a potential moderator in the indirect exposure-externalizing behavior relation. A continuous variable for indirect violence exposure was created based on the summary score of the aforementioned five dichotomous variables measuring indirect exposure (witnessing) to violence, weighed by each variable’s contribution to the indirect violence exposure score based on factor loadings from polychoric factor analysis. The resulting indirect exposure to violence score ranged from 0 to 8.5 with a median of 2.2 (±2.4). For descriptive purposes, the indirect violence exposure scale was categorized by tertiles (≤25th, 26–74th, and ≥75th percentiles). Direct exposure to violence was examined as a continuous variable by measuring the frequency of physical aggression. Longitudinal studies have shown that children who exhibit consistent patterns of externalizing behaviors at an early age are at an increased risk for developing conduct disorder and persistent antisocial behaviors incidents in the past year.
Key covariates or potential confounders included socio-demographics: child age, sex, maternal education, pre-natal maternal smoking, maternal marital status, living with both biological parents, and having a primary caregiver change at least once during the child’s life. The sample was limited to the self-reported race of Black. Maternal education was categorized into less than a high school degree, or a high school degree or more.
Data Analysis
Univariate, bivariate, and multivariate analyses were performed using SAS version 9.3 (Cary, NC). Bivariate analyses examined crude associations as well as potential confounders between the different types of exposure to violence and externalizing behavior, including likelihood ratio chi-square, Fisher’s exact test, and Spearman’s or Pearson’s rank-order correlation coefficients. Covariates significantly associated with both indirect exposure to violence and externalizing behavior and changed the estimate between violence exposure and externalizing behavior by more than 10 %, as well as those considered theoretically important, were included in the multivariate model. Multivariate analysis included linear regression, for externalizing behavior total score (continuous), and also included testing for interaction between indirect violence exposure and physical aggression. Thirty-eight percent of enrolled families had more than one child participate (range 1–5); therefore, to account for correlation between siblings or children living in the same household and matched pairs, generalized estimating equations (GEE) analyses were employed using an unstructured correlation structure. The analysis controlled for above listed covariates. Two-way interaction between indirect and direct violence exposure was tested in the regression model and significant interaction represented visually in graphs at one standard deviation above and below the mean and with examination of significant differences using simple-slopes method.70 Collinearity diagnostics were performed.
Results
Respondent and child characteristics are presented in Table 1. The mean age of children was 10.28 years (range = 5–15 years). Approximately half of the children in the sample (56.10 %) were female. Approximately three fourths of mothers had a high school degree or more. Mean household income varied, with 30.8 % of the sample reporting a monthly income of $2499 or less. Total externalizing scores ranged from 0.00 to 47.00, with a mean of 7.44. T scores for externalizing behavior ranged from 33.00 to 83.00, with a mean of 50.32.
TABLE 1.
Characteristics of NSPAC sample by level of indirect violence (N = 82)
| Total N (%) | Low violence exposure (<3 types) N (%) | Medium violence exposure (3–5 types) N (%) | High violence exposure (>5 types) N (%) | |
|---|---|---|---|---|
| Sex of child | ||||
| Male | 36 (43.90) | 8 (42.11) | 25 (52.08) | 3 (20.00) |
| Female | 46 (56.10) | 11 (57.89) | 23 (47.92) | 12 (80.00) |
| Mother’s educational background | ||||
| Less than a high school degree | 21 (25.61) | 4 (21.05)* | 12 (25.00)* | 5 (33.33)* |
| High school degree or more | 61 (74.39) | 15 (78.95)* | 36 (75.00)* | 10 (66.67)* |
| Smoking during pregnancy | ||||
| Yes | 11 (13.41) | 1 (5.26) | 8 (16.67) | 2 (13.33) |
| No | 71 (86.59) | 18 (94.74) | 40 (83.33) | 13 (86.67) |
| Child caregiver change (at least once within lifetime) | ||||
| Yes | 15 (18.29) | 4 (21.05) | 8 (16.67) | 3 (20.00) |
| No | 67 (81.71) | 15 (78.95) | 40 (83.33) | 12 (80.00) |
| Child lives with both biological parents | ||||
| Yes | 10 (12.20) | 3 (15.79) | 6 (12.50) | 1 (6.67) |
| No | 72 (87.80) | 16 (84.21) | 42 (87.50) | 14 (93.33) |
| Mean, range, SD | ||||
| Child’s age | 10.28 | 9.42 | 10.61 | 10.24 |
| 5.00–15.00 | 5.00–15.00 | 6.00–15.00 | 5.00–15.00 | |
| 2.93 | 3.40 | 2.94 | 2.76 | |
| Chaos | 28.16 | 24.85 | 27.46 | 34.16 |
| 15.00–56.00 | 15.00–39.00 | 15.00–49.00 | 18.00–56.00 | |
| 8.76 | 6.78 | 8.23 | 9.77 | |
| Maternal adverse childhood experiences (ACE) | 2.80 | 0.95 | 3.20 | 3.94 |
| 0.00–8.00 | 0.00–5.00 | 0.00–8.00 | 2.00–6.00 | |
| 2.12 | 1.32 | 2.10 | 1.30 | |
| CBCL externalizing behavior T score | 51.31 | 49.00 | 48.84 | 54.68 |
| 33.00–83.00 | 33.00–71.00 | 33.00–83.00 | 33.00–78.00 | |
| 13.09 | 14.53 | 14.02 | 11.12 | |
| CBCL externalizing behavior total score | 8.43 | 7.00 | 7.53 | 9.87 |
| 0.00–47.00 | 0.00–22.00 | 0.00–47.00 | 0.00–37.00 | |
| 9.62 | 8.53 | 10.81 | 8.75 | |
Characterized by tertiles: ≤25th, 26–74th, and ≥75th percentiles
*p < 0.05, based on likelihood ratio chi-square or Fisher’s exact test
All of the children in our sample had experienced at least one form of violence. A majority of children experienced physical aggression (72.00 %). Approximately one third witnessed community violence (35.37 %) or a friend or family member get hurt or mistreated (34.57 %). Children who experienced physical aggression in the home had greater average externalizing behavior scores. The association between cumulative indirect violence exposure and externalizing behavior T score remained significant after matching on age and Hurricane Katrina exposure, and controlling for key covariates (Table 2). CBCL externalizing T score increased significantly by approximately 1.25 points for each level increase in indirect violence exposure (β = 1.25, SE = 0.57, p = 0.027). Crudely, cumulative indirect violence exposure explained 5 % of the variance in externalizing behavior score; when considering additional covariates, 17.8 % of the variance in externalizing behavior was explained.
TABLE 2.
Final multivariate models: association between indirect exposure to violence and externalizing behavior (N = 82)
| Outcome: externalizing behavior T score | |||
| Beta coefficient (β) | Standard Error (SE) | p value | |
| Indirect exposure to violence (continuous) | 1.25 | 0.57 | 0.027 |
| Sex (male vs. female) | 4.57 | 2.43 | 0.060 |
| Mother’s education (<H.S to H.S. or more) | 10.11 | 2.67 | <0.001 |
| Smoked during pregnancy (Yes) | 5.77 | 6.47 | 0.373 |
| Lives with both biological parents (Yes) | 6.09 | 6.16 | 0.323 |
| Had a change in primary caregiver at least once in the child’s lifetime (Yes) | 4.73 | 4.89 | 0.334 |
| R-square | 17.8 % | ||
| Outcome: externalizing behavior T score interaction model with direct violence | |||
| Beta coefficient (β) | Standard Error (SE) | p value | |
| Indirect exposure to violence × physical aggression (continuous) | −0.08 | 0.03 | 0.002 |
| Indirect exposure to violence | 2.09 | 0.59 | <0.001 |
| Physical discipline | 0.30 | 0.10 | 0.002 |
| Sex (male vs. female) | 3.47 | 2.52 | 0.169 |
| Mother’s education (<H.S. to H.S. or more) | 9.55 | 2.37 | <0.0001 |
| Smoked during pregnancy (Yes) | 6.46 | 6.51 | 0.321 |
| Lives with both biological parents (Yes) | 6.21 | 5.80 | 0.284 |
| Had a change in primary caregiver at least once in the child’s lifetime (Yes) | 4.69 | 4.48 | 0.295 |
| R-square | 23.7 % | ||
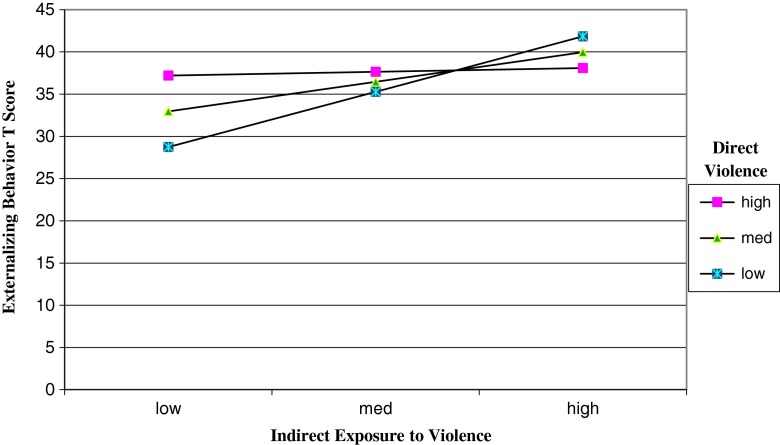
As shown in Fig. 1, there was a significant interaction between indirect exposure to violence (witnessed violence) and direct exposure to violence (caregiver physical aggression against the child) in the association with externalizing behavior T score (β = −0.08, SE = 0.03, p = 0.002). Among children with lower levels of indirect violence exposure (1 standard deviation below the mean per simple slopes), the levels of externalizing behavior were highest among children with high levels of direct violence exposure, whereas among children with higher levels of indirect violence exposure, the levels of externalizing behavior were highest among children with lower levels of direct exposure. Among children experiencing high levels of indirect violence exposure, the differences in externalizing behavior by direct exposure were lower than differences among children with lower levels of indirect violence exposure. The impact of indirect violence exposure was greatest among children with lower levels of direct violence (β = 4.20, SE = 0.56, p < 0.0001), compared to the impact of indirect violence among children with medium to high levels of direct violence (β = 2.58, SE = 0.63, p < 0.0001). This interaction explained an additional 5.9 %.
FIG. 1.
Externalizing behavior by indirect exposure to violence—moderation by direct violence exposure.
Discussion
This study reveals a robust association between cumulative indirect exposure to violence and externalizing behavior, with differing results based on children’s exposure to direct violence. This study extends previous research in children that has demonstrated a link between direct and indirect exposures to violence and child externalizing behaviors. The majority of previous studies have focused on the link between singular violence exposures and externalizing behaviors,47 failing to effectively capture the typical multiple violence exposure experienced by today’s children. This study addresses this important gap and focuses on cumulative violence exposure, measured across contexts, as both independent and interactive risk factors for externalizing behavior in children.
Our results corroborate previous research on the association between externalizing behaviors and exposure to direct violence in youth, as measured by caregiver physical aggression as well as harsh parenting or physical discipline.16,18,22–24,71,72 Additionally, results support research on the association between externalizing behaviors and exposure to indirect violence, including witnessing neighborhood violence.73,74 Results also extend previous findings to include examination of the interaction between direct and indirect violence exposures. While we observed a significant positive association between indirect exposure to violence and externalizing behavior, this relation varied by the level of direct violence exposure as measured by physical discipline. The impact of high indirect exposure on externalizing behavior was greater among children with lower levels of direct violence exposure. This may potentially be explained by some desensitization to indirect exposure to violence when physical aggression in the home is high or vice versa.75,76 Additionally, it could be explained by co-morbidity issues including a higher likelihood of suffering from depression or internalizing behavior among children with high exposure to violence.39,77
Desensitization is a gradual reduction or emotional numbing in responsiveness to an arousal-eliciting stimulus as a function of repeated exposure.76 Repeat exposure to violence may impact the neurobiological pathways related to threat perception, potentially altering an individual’s response and reaction to threat not only when exposed to violence, but on a day to day basis as well.78 While direct and indirect exposures are not equivalent, the high level of relational, direct physical discipline toward a child may evoke some level of desensitization to other forms of violence resulting in a greater impact of direct violence with less additive effects with indirect. Such desensitization has been shown in Black youth exposed to community violence,79 with a curvilinear relation between community violence exposures. In our current sample, we found no significant curvilinear or quadratic relation between indirect or direct violence and externalizing behavior; however, desensitization may also vary by behavioral conditions.
Additionally, our findings related to the cross-contextual effects of violence exposure provide novel information relevant to preventive intervention efforts seeking to decrease the lasting negative effects of violence exposure among children. Hickman and colleagues suggest that it may be the mix of the type of exposure experiences that has the greatest negative effect on children.61 Although we did not have longitudinal data, our results suggest there may be a strong impact of cumulative indirect violence exposure on externalizing behavior in children, as well as a significant effect of direct violence exposure (e.g., physical aggression). Findings are consistent with past research indicating that multiple types of violence exposure, experienced both within the family and in the neighborhood80,81 both co-occur and multiplicatively contribute to behavior.
Despite several strengths of the study, limitations also exist. First, this is a small and relatively homogenous convenience sample, making it less generalizable. However, the sample was derived in a highly innovative fashion allowing recruitment of an otherwise difficult to reach population—a non-clinical, high-risk, and geographically diverse sample. Second, given that the majority of children in this sample experienced Hurricane Katrina (67 % of the families indicated living in New Orleans at the time), this is likely a highly traumatized sample of children, which also decreases generalizability. We did match by exposure to Katrina in an effort to control for this effect. Third, the study included maternal self-reported measures of the key outcome and exposures, with the potential for recall and social desirability biases. Fourth, no assessment of the frequency of exposures or age at the time of exposures was collected, limiting our ability to determine the impact of exposure across developmental stages. We also did not have data on potential direct violence exposure beyond physical aggression, or any exposure at school, another potentially frequent source of direct violence exposure. Additionally, our study would have been strengthened by adding child-reported exposure to violence as well, given that it might be more accurate than parents’, especially for older youth.82,83 Child self-report on exposure to violence, greater detail on the timing and frequency of violence exposure, the relations between these factors and externalizing behavior, and the impact of positive socio-ecological contexts on behavior must be explored to inform intervention and programming. When combined with our current findings, these future steps would be expected to substantially advance our understanding of how much each type of exposure to violence contributes to externalizing behaviors.
These findings offer novel insight into the interactive pathways linking direct and indirect violence exposure to externalizing that is expected to assist in the development of novel intervention approaches to mitigating the lasting cumulative impact of violence exposure in a child’s environment. As few studies have addressed the risk for externalizing behaviors due to cumulative violence exposure, it is an important next research step to expand our understanding of the reciprocal relation between cumulative violence exposure and externalizing behaviors.59,61 Further, an individual’s temperament or personality traits, as well as social support and a variety of other factors including age and gender, are also likely moderators of the relationship between both acute and chronic stressors, such as exposure to violence and externalizing behaviors, and should be examined. Finally, there should be an emphasis on identification of potential sources of buffering for the effects of exposure to violence.61 Early detection and prevention of violence exposure and interventions to mitigate its impact on child development are essential to minimize the long-term psychological, socio-emotional, biological, and economic impacts of violence.
Acknowledgments
This study was supported by grants from the National Institutes of Health (NIH; R01ES020447 and P60AA009803-RC5 to Dr. Theall, and R21MH094688 and R01MH101533 to Dr. Drury) and Centers for Disease Control and Prevention (CDC, R01CE002327 to Dr. Taylor).
Compliance with Ethical Standards
This study was approved by the Tulane University Health Sciences Center Institutional Review Board.
References
- 1.Ştefan CA, Miclea M. A preliminary efficiency study of a multifocused prevention program for children with deficient emotional and social competencies. Procedia - Soc Behav Sci. 2010;5:127–139. doi: 10.1016/j.sbspro.2010.07.061. [DOI] [Google Scholar]
- 2.Achenbach TM, Edelbrock CS. The classification of child psychopathology: a review and analysis of empirical efforts. Psychol Bull. 1978;85(6):1275–1301. doi: 10.1037/0033-2909.85.6.1275. [DOI] [PubMed] [Google Scholar]
- 3.Hinshaw SP. Externalizing behavior problems and academic underachievement in childhood and adolescence: causal relationships and underlying mechanisms. Psychol Bull. 1992;111(1):127–155. doi: 10.1037/0033-2909.111.1.127. [DOI] [PubMed] [Google Scholar]
- 4.Murray K, Kochanska G. Effortful control: factor structure and relation to externalizing and internalizing behaviors. J Abnorm Child Psychol. 2002;30(5):503–514. doi: 10.1023/A:1019821031523. [DOI] [PubMed] [Google Scholar]
- 5.Wood JJ, Cowan PA, Baker BL. Behavior problems and peer rejection in preschool boys and girls. J Genet Psychol. 2002;163(1):72–88. doi: 10.1080/00221320209597969. [DOI] [PubMed] [Google Scholar]
- 6.Barker E, Maughan B. Differentiating early-onset persistent versus childhood-limited conduct problem youth. Am J Psychiatr. 2009;166(8):900–908. doi: 10.1176/appi.ajp.2009.08121770. [DOI] [PubMed] [Google Scholar]
- 7.McLeod JD, Kaiser K. Childhood emotional and behavioral problems and educational attainment. Am Sociol Rev. 2004;69(5):636–658. doi: 10.1177/000312240406900502. [DOI] [Google Scholar]
- 8.Farrington DP. Childhood aggression and adult violence: early precursors and later life outcomes. In: Pepler DJ, Rubin RH, editors. The development and treatment of childhood aggression. Hillsdale, NJ: Lawrence Erlbaum Associates; 1991. [Google Scholar]
- 9.King SM, Iacono WG, McGue M. Childhood externalizing and internalizing psychopathology in the prediction of early substance use. Addiction. 2004;99(12):1548–1559. doi: 10.1111/j.1360-0443.2004.00893.x. [DOI] [PubMed] [Google Scholar]
- 10.Sroufe LA, Carlson EA, Levy AK, Egeland B. Implications of attachment theory for developmental psychopathology. Dev Psychopathol. 1999;11(1):1–13. doi: 10.1017/S0954579499001923. [DOI] [PubMed] [Google Scholar]
- 11.Appleyard K, Egeland B, van Dulmen MH, Sroufe LA. When more is not better: the role of cumulative risk in child behavior outcomes. J Child Psychol Psychiatry. 2005;46(3):235–245. doi: 10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- 12.Finklehor D, Ormrod RK, Turner HA. Poly-victimization: a neglected component in child victimization. Child Abuse Negl. 2007;31(1):7–26. doi: 10.1016/j.chiabu.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Manly JT, Oshri A, Lynch M, Herzog M, Wortel S. Child neglect and the development of externalizing behavior problems: associations with maternal drug dependence and neighborhood crime. Child Maltreat. 2013;18(1):17–29. doi: 10.1177/1077559512464119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim J, Cicchetti D. Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. J Child Psychol Psychiatry. 2010;51(6):706–716. doi: 10.1111/j.1469-7610.2009.02202.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.English DJ, Thompson R, Graham JC, Briggs EC. Toward a definition of neglect in young children. Child Maltreat. 2005;10(2):190–206. doi: 10.1177/1077559505275178. [DOI] [PubMed] [Google Scholar]
- 16.Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373(9657):68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- 17.Hughes HM, Parkinson D, Vargo M. Witnessing spouse abuse and experiencing physical abuse: a “double whammy”? J Fam Violence. 1989;4(2):197–209. doi: 10.1007/BF01006629. [DOI] [Google Scholar]
- 18.Gershoff ET. Corporal punishment by parents and associated child behaviors and experiences: a meta-analytic and theoretical review. Psychol Bull. 2002;128(4):539–579. doi: 10.1037/0033-2909.128.4.539. [DOI] [PubMed] [Google Scholar]
- 19.Day RD, Peterson GW, McCracken C. Predicting spanking of younger and older children by mothers and fathers. J Marriage Fam. 1998;60(1):79–94. doi: 10.2307/353443. [DOI] [Google Scholar]
- 20.Belsky J. The determinants of parenting: a process model. Child Dev. 1984;55(1):83–96. doi: 10.2307/1129836. [DOI] [PubMed] [Google Scholar]
- 21.Beauchaine TP, Webster-Stratton C, Reid MJ. Mediators, moderators, and predictors of 1-year outcomes among children treated for early-onset conduct problems: a latent growth curve analysis. J Consult Clin Psychol. 2005;73(3):371–388. doi: 10.1037/0022-006X.73.3.371. [DOI] [PubMed] [Google Scholar]
- 22.Taylor CA, Manganello JA, Lee SJ, Rice JC. Mothers’ spanking of 3-year-old children and subsequent risk of children’s aggressive behavior. Pediatrics. 2010;125(5):e1057–e1065. doi: 10.1542/peds.2009-2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berlin LJ, Ispa JM, Fine MA, et al. Correlates and consequences of spanking and verbal punishment for low-income white, African American, and Mexican American toddlers. Child Dev. 2009;80(5):1403–1420. doi: 10.1111/j.1467-8624.2009.01341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grogan-Kaylor A. Corporal punishment and the growth trajectory of children’s antisocial behavior. Child Maltreat. 2005;10(3):283–292. doi: 10.1177/1077559505277803. [DOI] [PubMed] [Google Scholar]
- 25.Lee SJ, Taylor CA, Altschul I, Rice JC. Parental spanking and subsequent risk for child aggression in father-involved families of young children. Child Youth Serv Rev. 2013;35(9):1476–1485. doi: 10.1016/j.childyouth.2013.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.MacKenzie MJ, Nicklas E, Brooks-Gunn J, Waldfogel J. Spanking and children’s externalizing behavior across the first decade of life: evidence for transactional processes. J Youth Adolesc. 2015;44(3):658–669. doi: 10.1007/s10964-014-0114-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Edleson JL. Children’s witnessing of adult domestic violence. J Interpersonal Violence. 1999;14(8):839–870. doi: 10.1177/088626099014008004. [DOI] [Google Scholar]
- 28.Fantuzzo JW, DePaola LM, Lambert L, Martino T, Anderson G, Sutton S. Effects of interparental violence on the psychological adjustment and competencies of young children. J Consult Clin Psychol. 1991;59(2):258. doi: 10.1037/0022-006X.59.2.258. [DOI] [PubMed] [Google Scholar]
- 29.Holt S, Buckley H, Whelan S. The impact of exposure to domestic violence on children and young people: a review of the literature. Child Abuse Negl. 2008;32(8):797–810. doi: 10.1016/j.chiabu.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 30.Wolfe DA, Crooks CV, Lee V, McIntyre-Smith A, Jaffe PG. The effects of children’s exposure to domestic violence: a meta-analysis and critique. Clin Child Fam Psychol Rev. 2003;6(3):171–187. doi: 10.1023/A:1024910416164. [DOI] [PubMed] [Google Scholar]
- 31.Evans SE, Davies C, DiLillo D. Exposure to domestic violence: a meta-analysis of child and adolescent outcomes. Aggress Violent Behav. 2008;13(2):131–140. doi: 10.1016/j.avb.2008.02.005. [DOI] [Google Scholar]
- 32.Ehrensaft MK, Cohen P, Brown J, Smailes E, Chen H, Johnson JG. Intergenerational transmission of partner violence: a 20-year prospective study. J Consult Clin Psychol. 2003;71(4):741–753. doi: 10.1037/0022-006X.71.4.741. [DOI] [PubMed] [Google Scholar]
- 33.Margolin G. Effects of witnessing violence on children. In: Trickett PK, Schellenbach CJ, editors. Violence against children in the family and in the community. Washington DC: American Psychological Association; 1998. pp. 57–101. [Google Scholar]
- 34.Moylan CA, Herrenkohl TI, Sousa C, Tajima EA, Herrenkohl RC, Russo MJ. The effects of child abuse and exposure to domestic violence on adolescent internalizing and externalizing behavior problems. J Fam Violence. 2010;25(1):53–63. doi: 10.1007/s10896-009-9269-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gustafsson HC, Cox MJ, Blair C. Maternal parenting as a mediator of the relationship between intimate partner violence and effortful control. J Fam Psychol. 2012;26(1):115–123. doi: 10.1037/a0026283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shalev I, Moffitt TE, Sugden K, et al. Exposure to violence during childhood is associated with telomere erosion from 5 to 10 years of age: a longitudinal study. Mol Psychiatry. 2013;18(5):576–581. doi: 10.1038/mp.2012.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Drury SS, Mabile E, Brett ZH, et al. The association of telomere length with family violence and disruption. Pediatrics. 2014;134(1):e128–137. doi: 10.1542/peds.2013-3415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schwab-Stone ME, Ayers TS, Kasprow W, et al. No safe haven: a study of violence exposure in an urban community. J Am Acad Child Adolesc Psychiatry. 1995;34(10):1343–1352. doi: 10.1097/00004583-199510000-00020. [DOI] [PubMed] [Google Scholar]
- 39.Schwab-Stone M, Chen C, Greenberger E, Silver D, Lichtman J, Voyce C. No safe haven. II: the effects of violence exposure on urban youth. J Am Acad Child Adolesc Psychiatry. 1999;38(4):359–367. doi: 10.1097/00004583-199904000-00007. [DOI] [PubMed] [Google Scholar]
- 40.Margolin G, Gordis EB. Children’s exposure to violence in the family and community. Curr Dir Psychol Sci. 2004;13(4):152–155. doi: 10.1111/j.0963-7214.2004.00296.x. [DOI] [Google Scholar]
- 41.Linares LO, Heeren T, Bronfman E, Zuckerman B, Augustyn M, Tronick E. A mediational model for the impact of exposure to community violence on early child behavior problems. Child Dev. 2001;72(2):639. doi: 10.1111/1467-8624.00302. [DOI] [PubMed] [Google Scholar]
- 42.Downey G, Coyne JC. Children of depressed parents: an integrative review. Psychol Bull. 1990;108(1):50–76. doi: 10.1037/0033-2909.108.1.50. [DOI] [PubMed] [Google Scholar]
- 43.Conger RD, Patterson GR, Ge X. It takes two to replicate: a mediational model for the impact of parents’ stress on adolescent adjustment. Child Dev. 1995;66(1):80–97. doi: 10.2307/1131192. [DOI] [PubMed] [Google Scholar]
- 44.Fauber RL, Long N. Children in context: the role of the family in child psychotherapy. J Consult Clin Psychol. 1991;59(6):813–820. doi: 10.1037/0022-006X.59.6.813. [DOI] [PubMed] [Google Scholar]
- 45.Turner HA, Finkelhor D, Ormrod R, et al. Family context, victimization, and child trauma symptoms: variations in safe, stable, and nurturing relationships during early and middle childhood. Am J Orthopsychiatry. 2012;82(2):209–219. doi: 10.1111/j.1939-0025.2012.01147.x. [DOI] [PubMed] [Google Scholar]
- 46.Dong M, Anda RF, Felitti VJ, et al. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse Negl. 2004;28(7):771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 47.Finkelhor D, Turner, H., Ormrod, R., Hamby, S., & Kracke, K. Polyvictimization: children’s exposure to multiple types of violence, crime, and abuse. Juvenile Justic Bulletin: US Department of Justice, Office of Justice Programs, Office of Juvenile Justic and Delinquency Prevention. 2011; 1-11.
- 48.Taylor CA, Guterman NB, Lee SJ, Rathouz PJ. Intimate partner violence, maternal stress, nativity, and risk for maternal maltreatment of young children. Am J Public Health. 2009;99(1):175–183. doi: 10.2105/AJPH.2007.126722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kelleher KJ, Hazen AL, Coben JH, et al. Self-reported disciplinary practices among women in the child welfare system: association with domestic violence victimization. Child Abuse Negl. 2008;32(8):811–818. doi: 10.1016/j.chiabu.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 50.Taylor CA, Lee SJ, Guterman NB, Rice JC. Use of spanking for 3-year-old children and associated intimate partner aggression or violence. Pediatrics. 2010;126(3):415–424. doi: 10.1542/peds.2010-0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lynch M, Cicchetti D. An ecological-transactional analysis of children and contexts: the longitudinal interplay among child maltreatment, community violence, and children’s symptomatology. Dev Psychopathol. 1998;10(2):235–257. doi: 10.1017/S095457949800159X. [DOI] [PubMed] [Google Scholar]
- 52.Hartley CC. The co-occurrence of child maltreatment and domestic violence: examining both neglect and child physical abuse. Child Maltreat. 2002;7(4):349–358. doi: 10.1177/107755902237264. [DOI] [PubMed] [Google Scholar]
- 53.Appel AE, Holden GW. The co-occurrence of spouse and physical child abuse: a review and appraisal. J Fam Psychol. 1998;12(4):578. doi: 10.1037/0893-3200.12.4.578. [DOI] [Google Scholar]
- 54.King KE, Morenoff JD, House JS. Neighborhood context and social disparities in cumulative biological risk factors. Psychosom Med. 2011;73(7):572–579. doi: 10.1097/PSY.0b013e318227b062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Evans GW, Kim P, Ting AH, Tesher HB, Shannis D. Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Dev Psychol. 2007;43(2):341–351. doi: 10.1037/0012-1649.43.2.341. [DOI] [PubMed] [Google Scholar]
- 56.Morales JR, Guerra NG. Effects of multiple context and cumulative stress on urban children’s adjustment in elementary school. Child Dev. 2006;77(4):907–923. doi: 10.1111/j.1467-8624.2006.00910.x. [DOI] [PubMed] [Google Scholar]
- 57.Rutter M, Garmezy N, Rutter M. Stress, coping and development in children. In: Garmezy N, Rutter M, editors. Stress, coping and development: some issues. New York, NY: McGraw-Hill; 1983. [Google Scholar]
- 58.Plybon LE, Kliewer W. Neighborhood types and externalizing behavior in urban school-age children: tests of direct, mediated, and moderated effects. J Child Fam Stud. 2001;10(4):419–437. doi: 10.1023/A:1016781611114. [DOI] [Google Scholar]
- 59.Mrug S, Windle M. Prospective effects of violence exposure across multiple contexts on early adolescents’ internalizing and externalizing problems. J Child Psychol Psychiatry. 2010;51(8):953–961. doi: 10.1111/j.1469-7610.2010.02222.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mrug S, Loosier PS, Windle M. Violence exposure across multiple contexts: individual and joint effects on adjustment. Am J Orthopsychiatry. 2008;78(1):70–84. doi: 10.1037/0002-9432.78.1.70. [DOI] [PubMed] [Google Scholar]
- 61.Hickman LJ, Jaycox LH, Setodji CM, et al. How much does “how much” matter? Assessing the relationship between children’s lifetime exposure to violence and trauma symptoms, behavior problems, and parenting stress. J Interpersonal Violence. 2013;28(6):1338–1362. doi: 10.1177/0886260512468239. [DOI] [PubMed] [Google Scholar]
- 62.Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychol Bull. 2013;139(6):1342–1396. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- 63.Watters JK, Biernacki P. Targeted sampling: options for the study of hidden populations. Soc Probl. 1989;36(4):416–430. doi: 10.2307/800824. [DOI] [Google Scholar]
- 64.Tashima N, Crain C, O’Reilly K, Elifson CS. The community identification (CID) process: a discovery model. Qual Health Res. 1996;6(1):23–48. doi: 10.1177/104973239600600103. [DOI] [Google Scholar]
- 65.Kawachi I, Daniels N, Robinson DE. Health disparities by race and class: why both matter. Health Aff. 2005;24(2):343–352. doi: 10.1377/hlthaff.24.2.343. [DOI] [PubMed] [Google Scholar]
- 66.Oaks J, Kaufman J. Methods in social epidemiology. San Francisco, CA: Jossey-Bass; 2006. [Google Scholar]
- 67.Achenbach TM, Rescorla L. Manual for the ASEBA school-age forms & profiles: an integrated system of multi-informant assessment. Burlington, VT: ASEBA; 2001. [Google Scholar]
- 68.Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, Angold A. Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA) J Am Acad Child Adolesc Psychiatry. 2006;45(5):538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- 69.Straus MA, Hamby SL. Measuring physical & psychological maltreatment of children with the conflict tactics scales. In: Kantor GK, Jasinski JL, editors. Out of the darkness: contemporary research perspectives on family violence. Thousand Oaks, CA: Sage; 1997. [Google Scholar]
- 70.Aiken LS, West SG, & Reno RR. Multiple regression: testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991.
- 71.Latimer K, Wilson P, Kemp J, et al. Disruptive behaviour disorders: a systematic review of environmental antenatal and early years risk factors. Child Care Health Dev. 2012;38(5):611–628. doi: 10.1111/j.1365-2214.2012.01366.x. [DOI] [PubMed] [Google Scholar]
- 72.Beauchaine TP, Webster-Stratton C, Reid MJ. Mediators, moderators, and predictors of 1-year outcomes among children treated for early-onset conduct problems: a latent growth curve analysis. J Consult Clin Psychol. 2005;73(3):371. doi: 10.1037/0022-006X.73.3.371. [DOI] [PubMed] [Google Scholar]
- 73.Herrenkohl TI, Lee J, Hawkins JD. Risk versus direct protective factors and youth violence: seattle social development project. Am J Prev Med. 2012;43(2):S41–S56. doi: 10.1016/j.amepre.2012.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Farrell AD, Mehari KR, Kramer-Kuhn A, Goncy EA. The impact of victimization and witnessing violence on physical aggression among high-risk adolescents. Child Dev. 2014;85(4):1694–1710. doi: 10.1111/cdev.12215. [DOI] [PubMed] [Google Scholar]
- 75.Salzinger S, Feldman RS, Stockhammer T, Hood J. An ecological framework for understanding risk for exposure to community violence and the effects of exposure on children and adolescents. Aggress Violent Behav. 2002;7(5):423–451. doi: 10.1016/S1359-1789(01)00078-7. [DOI] [Google Scholar]
- 76.Ng-Mak DS, Salzinger S, Feldman RS, Stueve C. Pathologic adaptation to community violence among inner-city youth. Am J Orthopsychiatry. 2004;74(2):196. doi: 10.1037/0002-9432.74.2.196. [DOI] [PubMed] [Google Scholar]
- 77.Fitzpatrick KM. Exposure to violence and presence of depression among low-income, African-American youth. J Consult Clin Psychol. 1993;61(3):528–531. doi: 10.1037/0022-006X.61.3.528. [DOI] [PubMed] [Google Scholar]
- 78.LeDoux J. Rethinking the emotional brain. Neuron. 2012;73(4):653–676. doi: 10.1016/j.neuron.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gaylord-Harden NK, Cunningham JA, Zelencik B. Effects of exposure to community violence on internalizing symptoms: does desensitization to violence occur in African American youth? J Abnorm Child Psychol. 2011;39(5):711–719. doi: 10.1007/s10802-011-9510-x. [DOI] [PubMed] [Google Scholar]
- 80.Leventhal T, Brooks-Gunn J. Children and youth in neighborhood contexts. Curr Dir Psychol Sci. 2003;12(1):27–31. doi: 10.1111/1467-8721.01216. [DOI] [Google Scholar]
- 81.Leventhal T, Brooks-Gunn J. The neighborhoods they live in: the effects of neighborhood residence on child and adolescent outcomes. Psychol Bull. 2000;126(2):309–337. doi: 10.1037/0033-2909.126.2.309. [DOI] [PubMed] [Google Scholar]
- 82.Selner-O’Hagan MB, Kindlon DJ, Buka SL, Raudenbush SW, Earls FJ. Assessing exposure to violence in urban youth. J Child Psychol Psychiatry Allied Discip. 1998;39(2):215–224. doi: 10.1111/1469-7610.00315. [DOI] [PubMed] [Google Scholar]
- 83.Litrownik A, Newton R, Hunter W, English D, Everson M. Exposure to family violence in young at-risk children: a longitudinal look at the effects of victimization and witnessed physical and psychological aggression. J Fam Violence. 2003;18(1):59–73. doi: 10.1023/A:1021405515323. [DOI] [Google Scholar]