Abstract
Initiatives to build supermarkets in low-income areas with relatively poor access to large food retailers (“food deserts”) have been implemented at all levels of government, although evaluative studies have not found these projects to improve diet or weight status for shoppers. Though known to be influential, existing evaluations have neglected in-store social dynamics and shopper behaviors. Surveys and walking interviews were used with shoppers (n = 32) at a supermarket developed through the Pennsylvania Fresh Food Financing Initiative in Philadelphia, PA. Key informant interviews with stakeholders in the supermarket’s development and operations provided additional context to these shopper experiences. Data were collected in July and September 2014 and qualitatively analyzed in NVivo 10.0. Participants described how the retailer helped them adapt or cope with difficult shopping routines and how it presented a reliable high-quality option (in terms of cleanliness, orderliness, and social atmosphere) in contrast to other neighborhood retailers. Health concerns were also identified, especially among those managing chronic disease for themselves or a family member. These issues underscored multiple points of challenge required to adjust shopping and eating behavior. In-store supports that reflect these challenges are warranted to more fully address food deserts and reduce health disparities.
Keywords: Food access, Food deserts, Supermarkets, Healthy food financing
Introduction
A wide body of research has described the environmental contexts in which diet—including food purchasing and consumption—takes shape for individuals and households. Significant associations between the quality of these “food environments,” health behaviors,1 and health outcomes2 have been observed across numerous geographies in the USA and elsewhere, although findings are not uniform across all studies.3 While the causal pathway between food access and diet is not well understood,4 a variety of federal, state, and local initiatives have emerged to incentivize supermarket development in low-income, underserved communities (“food deserts”).5
Existing evaluations of new supermarkets in food deserts have found that residents’ food environment perceptions may improve when new stores open,6 although few show improvement in consumption of healthy foods or health status.6–8 Of studies finding improvements in healthy purchasing, these changes are not attributable to the use of the new retailer.9,10 Evaluations also highlight the importance of in-store environment, including pricing, placement, and promotions, in motivating behavior change,6,11 although none have explored shoppers’ in-store experiences.
Previous qualitative research on food shopping by low-income households, including both observational and interview-based methods, offers specific context for this inquiry. First, studies show how low-income shoppers adapt their grocery trips to a variety of constraints, including issues of time, transportation, physical ability, and income, as well as retailer characteristic factors such as sales or produce quality.12–16 Social forces also affect where and how individuals shop; for instance, one study found that shoppers preferred stores they perceived to be safe and easily accessible but also where other shoppers shared similar racial and income characteristics and where they felt well treated by store staff.12,17 Once within a store, shoppers also exhibit a wide range of individual agency, ranging from very active engagement (i.e., highly planned shopping) to passive (i.e., reactive to marketing),13 and may choose less healthy options despite having nutritional knowledge, given a variety of immediate constraints.14 Taken together, these qualitative findings suggest how low-income shoppers select and utilize stores, including their coping strategies to deal with sub-optimal food shopping options, and provide a more proximal perspective on the complex relationship between food access, diet, and health.
As the aforementioned studies have shown, qualitative, in-store methodologies stand to document human behavior within social and cultural contexts and allow shoppers to articulate the experience of consumer food environments in their own words. While most previous studies considered how different shoppers sort into different types of stores, this study aims to explain how and why consumers select and utilize a particular store, its role in everyday life, and how these dynamics could be meaningful for health. These questions are interrogated by way of walking interviews, representing a novel approach to studying new supermarkets in food deserts.
Methods
This methodology was approved by the University of Pennsylvania Institutional Review Board.
Study Area
A supermarket in Philadelphia, Pennsylvania, agreed to allow research at a store (subsequently referred to as “the case supermarket” or “the store”) developed within the last 5 years through the Pennsylvania Fresh Food Financing Initiative (FFFI). The store was a medium-sized urban supermarket with a surface parking lot and nearby several modes of public transportation. Additionally, it was a “full-service” retailer, offering deli, meat, seafood, and prepared food sections. Nearly half of households in the case supermarket’s Census tract were without a vehicle, and nearly one in three reported participating in the Supplemental Nutrition Assistance Program (SNAP) during the last year.18 The tract was also predominantly African American, nearly double the citywide rate (42.5 % of householders).
Data Collection
Walking Interviews
Walking interviews have been used as a participatory, in-depth field method,19 including studies of consumer food-shopping behavior.13,20 The technique was adapted here to investigate how participants experienced the store environment while they shopped.
Participants were recruited by intercept as they entered the store. Three visual criteria were used to identify eligible customers: (1) individuals who had shopping carts, (2) were not using cell phones or headsets, and (3) were not engaged in conversation. Eligible customers who agreed to participate were asked to sign an informed consent form and offered a $25 gift card as compensation. Interviewing took place over 9 days in July and September 2014, including different times of day, week, and month. Following an initial set of July interviews, additional interviews were conducted in September until thematic saturation was adequately achieved.
Digital voice recorders and lapel-clipping microphones were used to record interviews. Participants were asked to narrate their shopping trip aloud to the interviewer as they walked throughout the store. Additional prompts were provided as needed to clarify statements and location within the store. For example, if a participant was standing in front of a shelf, the interviewer may have asked, “What are we looking for here?” After participants had proceeded through checkout, a brief (5–10 min) survey was administered and they were given the gift card.
Shopper Survey
Validated measures of food environment perceptions, fruit/vegetable consumption, and readiness to adopt healthier behaviors were adapted to create a composite survey instrument.21–24 Additionally, surveys were used to collect a variety of shopper demographic information and other characteristics.
Field Notes
The interviewer took field notes at the end of each site visit, including notable incidents or circumstances, such as weather conditions or conversations with store staff. These allowed for preliminary identification of shopper patterns, possible methodological improvements, and consideration of when thematic saturation had been achieved.
Stakeholder Interviews
During 2013 and 2014, semi-structured interviews were completed with ten participants who had affiliations with FFFI or had specific knowledge about the case supermarket. Specific to the case supermarket, interviews included a store manager, director of human relations, director of community relations, and local law enforcement official who worked in the neighborhood and used the store as a “home base.” These interviews helped to place the walking interviews—the basis for this paper—within broader, structural contexts.
Data Analysis
Survey Analysis
Survey data were entered into an SPSS (version 22) database. Additional fields were added to document participant’s race and gender (as perceived by the interviewer) and trip duration. The straight line distance between the case supermarket and the intersection nearest to the participant’s home was calculated in ArcGIS 10.1. Descriptive statistics were generated to summarize participant characteristics.
Transcription and Coding
Audio files were transcribed verbatim, and transcripts were used to establish a preliminary list of codes based on recurring themes and concepts.25 Two researchers with qualitative coding experience independently analyzed ten transcripts to create a list of codes and definitions. Following this preliminary code development, codes and definitions were compared and discrepancies were resolved. The researchers returned to ten additional transcripts and applied a closed-coding method in separate NVivo (version 10.0) projects. An NVivo report was generated to document agreement between coders; levels below 70 % were flagged, discussed, and re-coded in a subsequent meeting.
Coding themes included attitudes about the store, food perceptions, shopping logistics, health attitudes, and the type of trip being completed. These themes broadly describe the value of the supermarket in everyday life and health attitudes and behaviors.
Results
Description of Sample
Thirty-two (n = 32) individuals were recruited and signed the consent form. Participants were predominantly women (n = 27) and African Americans (n = 31). Nearly all participants identified themselves as the primary food shoppers for their household (n = 31). Participants voiced very little disagreement in terms of their attitudes and beliefs about healthy eating (see Table 1). Almost three quarters of participants (n = 23) reported receiving SNAP benefits. The majority of participants reported purchasing most of their groceries (n = 22) and fruits and vegetables (n = 20) at the case supermarket.
TABLE 1.
Descriptive statistics from shopper survey
| Valid number | Mean | SD | |
|---|---|---|---|
| Trip duration (minutes) | 32 | 0:29 | 0:14 |
| Trips to case supermarket per month | 32 | 6.8 | 6.5 |
| Household size (persons) | 32 | 2.7 | 2.0 |
| Age (years) | 31 | 53.0 | 12.5 |
| Distance from case supermarket (miles) | 32 | 1.9 | 4.0 |
| Fruit and vegetable consumption (times eaten per week) | 30 | 12.3 | 4.0 |
| My family dislikes the taste of vegetablesa | 30 | 2.3 | 1.1 |
| I dislike the taste of vegetablesa | 32 | 1.9 | 0.7 |
| It is hard to include fruits/vegetables in meals when I am tireda | 32 | 2.8 | 1.0 |
| Fruits and vegetables are good for the bodya | 32 | 4.4 | 0.5 |
| I am happy with the quality of groceries in my neighborhooda | 32 | 3.6 | 1.1 |
aPerceptions/attitudes (1 = strongly disagree, 5 = strongly agree)
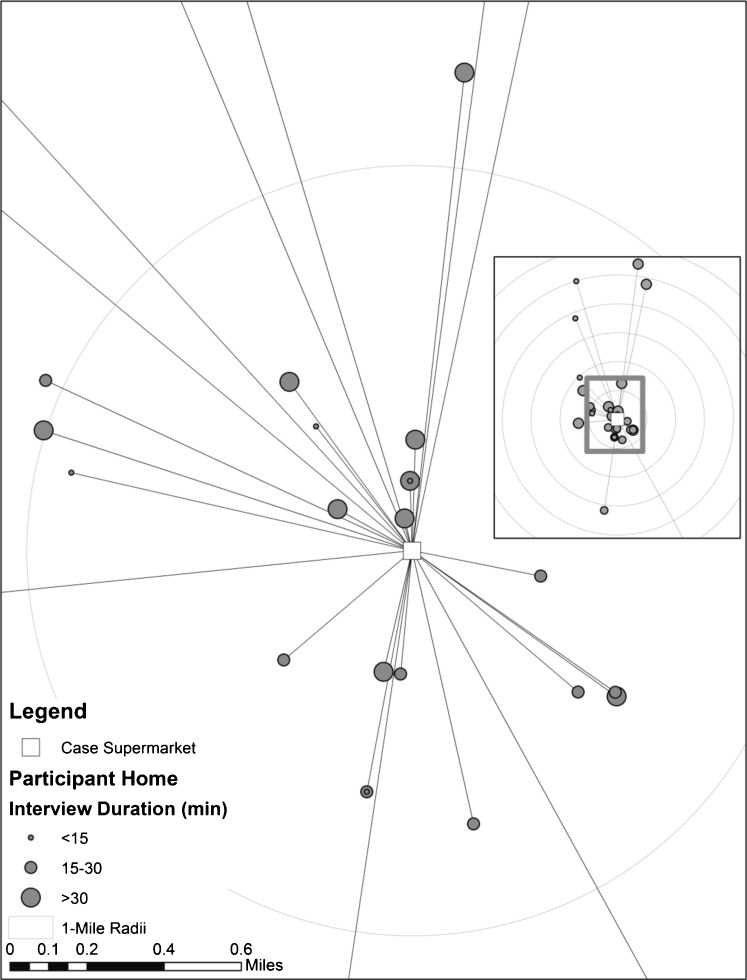
Other participant characteristics are summarized in Table 1, and Fig. 1 provides a spatial representation of several variables. Participant responses were also binned by those who lived within 1 mi (n = 19) and those who did not (n = 13; see Table 2).
FIG. 1.
Participant distance to case supermarket. Participants came from a variety of neighborhoods to shop at the case supermarket, as measured by the street intersections closest to their homes.
TABLE 2.
Participant food environment perceptions
| Distance to participant home | ||
|---|---|---|
| ≤1 mi | >1 mi | |
| Happy with the quality of groceries in my neighborhooda | 89.5 % | 38.5 % |
| Fruits and vegetables are easy to find in my neighborhooda | 78.9 % | 61.5 % |
| Purchase most of groceries at this supermarketb | 89.5 % | 38.5 % |
Calculated from valid responses within distance bins
aMeasured by reporting “agree”/“strongly agree”
bMeasured by reporting “yes”
Role of Case Supermarket in Everyday Life
Many participants mentioned a variety of constraints that influenced their shopping, including their current trip to the case supermarket, as well as methods for coping and the role of the case supermarket in these strategies.
Transportation
Participants cited a variety of strategies for dealing with the complexity of transportation for food shopping. Several participants adjusted the size and quantities of purchases to their transit type. One participant described this practice as using “wisdom” while shopping; in her case, this meant limiting the number of items to allow her to ride a city bus comfortably. Another participant (age 57) employed a similar strategy by using a rolling luggage bag to carry items from the store to work; ultimately, this allowed her to go home after work without grocery shopping. Others who lived nearby also completed smaller shopping trips with the intention of returning later in the day or week.
Several participants coordinated with family, friends, or neighbors to use personal vehicles for shopping. For some, this strategy was not an option, although they still desired the ability to make trips with a vehicle (i.e., not walking or using transit). One participant (51) described how her transportation for food shopping was even more complex before the case supermarket opened: “I had to go further. And pay a hack-man [informal cab driver] to bring me home. Hack-man want like… ten dollars.”
Participants also could use a free shuttle provided by the case supermarket if they spent over $60. Though popular, this service was not without caveats. In the words of one participant (51): “[Y]ou have to spend like a hundred or… close to a hundred, yeah. That’s pretty um… nerve-wracking. You have to stand out there and wait in the heat, and you got ice cream and stuff, while he’s taking other people.” Another participant (61) finished her shopping over an hour before the shuttle started, unfortunately on one of the hottest days of the year: “Aw man, a whole hour to wait. […] Feel that heat already.”
Perhaps the best illustration of the potential complexity of shopping trips came from one participant (51) who had traveled to the case supermarket via multiple forms of public transportation. She was devastated to learn that the shuttle was only offered within a 3-mi radius of the store, derailing her plans for a large shopping trip: “I can’t go shoppin’ here like I want to and I don’t have the transportation and I don’t have the money to pay for no hack driver.” At this point, she pulled out a transit pass, an 8-dollar ticket that provides up to eight rides, to illustrate how her plans were disrupted: “I gotta get on another bus, get on that bus, then I don’t know, it’s like, oh goodness. So… I gotta check out. […] See what we gotta go through. Goin’ shoppin’?” The complexity of this participant’s trip to and from the store dramatically limited her ability to complete the trip as she had hoped.
Transportation complexity was not limited to those without a personal vehicle. Even among individuals who drove themselves to the store, issues such as the price of gasoline or the physical challenge of carrying groceries up apartment stairs at home also affected how participants framed their shopping trips. A few participants also described situations where they were unable or unwilling to drive, although a vehicle was available: one because of a recently revoked driver’s license and the other possibly because of her declining eyesight (identified during other interactions throughout the store). Thus, while private vehicles posed a potentially important resource for grocery shopping, their utility was not uniform across all participants.
Price Comparisons
Price comparisons between stores were common. One participant (46) offered a frequently echoed description of this strategy: “[T]hey give us sales items in front of our door every week, so I go to each store and see what’s on sale and compare prices. So, like I buy certain stuff out here […] you know, the stuff that I know is gonna cost more at another store, I come here and get it on sale.” Other shoppers already knew about prices at other stores, including a nearby chain pharmacy: “Now, across the street it’s $3.49. Over here, it’s $3.33. So, it’s a deal!”
Nonetheless, this strategy had logistical limits. In the words of one participant (63) as she contemplated paying a few cents more for small item: “You don’t save no money be runnin’ all around and I gotta, and I’m goin’ back home.” Another participant suggested that nearby stores ran similar sales simultaneously, raising the importance of convenience: “Like I said, dependin’ on where you like or which is easier for you to get to, when they have a sale like this, usually so does all the other stores.”
Participants also designated certain types of items to certain types of retailers. Several shoppers who felt the case supermarket’s prices were high compared to other retailers (usually supermarkets but sometimes dollar stores or meat markets) would only buy limited quantities or types of items like meat or fish, leaving those purchases to other retailers. In the words of one participant (36): “Yeah, I come here, like to get things spur of the moment. Little things. But um, I don’t buy meat from over the butcher… They too high.” Alternatively, the wide assortment of name brand products offered by this supermarket appeared to be an enticing factor compared to other, perhaps cheaper, neighborhood stores.
Comparative Superiority
Many participants compared the case supermarket to other retailers that were not as favorable in terms of store cleanliness and reliability. As described by one participant: “This store stays pretty clean, you know? When they say they have something on sale, most of the time they have it… It’s not like them other stores.” Another participant (63) agreed with the sentiment that the case supermarket was uniquely clean: “I don’t like to go in a market and see that the floors haven’t been scrubbed, or… it have smells. […] [I]t seems like they really… They make a point to make it sparkle. So when you come in, it’s lit up. And another thing, this is in the community and like I said, senior citizens shop in here. It used to be, one time, you would only seem ‘em at Acme.”
Similarly, one participant shopping with SNAP benefits was not willing to compromise on her perception of freshness for lower prices. As she shopped with her elementary school-age son, she contrasted the case supermarket to a new discount supermarket nearby: “Yeah, so a lot of people go there now. Because it’s way cheaper. But I can't… I’m a picky person, so I have to go where I know the food is fresh, you know? Even if it’s a, a franchise, I don’t know that it’s fresh.” Others extended this concept to food safety; as expressed by one participant: “[Y]ou gotta be careful where you get your meats at. Cause it’ll make you sick.” Notably, participants differed in their assessment of precisely how the case supermarket’s prices compared to other stores.
Positive Social Interactions
Participants described positive interpersonal experiences in the case supermarket. According to one participant: “[E]verybody here’s nice, really. Everybody, they always treat you nice. If you ask a question, they’ll stop […]. [I]f somethin’s not right, then they’ll call somebody.” Similar to cleanliness and orderliness, this positive social quality was held in contrast to other retailers. For instance: “I’ve been in a couple markets that’s really rude… But this one is really, this one is actually… ok with me.” As another example of a positive social perception, one participant (65) described making trips to the case supermarket as way to pass the time: “I live alone. So basically, all my spare time, I’m at home. […] But when I’m just at home, and nothing else to do, and I start thinking negatively, I’ll say I know, I can go to the supermarket, they love me there.”
Health Attitudes
Several participants mentioned health in several ways, including awareness of health and nutrition, identification of specific items or behaviors (i.e., “low sodium”) that were important for health, and descriptions of the challenge of adopting and maintaining health-promoting behaviors.
Pursuing Healthier Options
Some shoppers described their choices of specific items based on certain health criteria such as sugar or sodium content or tried to avoid or modulate their purchases of items that were not reduced sugar or reduced sodium. For instance, one participant (63) described her affinity for a specific brand of juice: “I always get my cranberry juice here, too. […] I always get my Apple and Eve, cause they don’t have the added sugar.” Another middle-aged participant spent several minutes searching for a specific package of pretzels with reduced sodium, contemplating alternatives aloud: “Let me see if this is what I want. […] I like the lightly salted. […] Sodium content… [reading the nutrition label]. Don’t you know I know sodium. So I just have to scrape ‘em.”
Though fewer in number, some participants were also clear about their pursuit of less healthy items, such as candy or a slice of cheesecake, categorically referred to as “junk food.” For these individuals, purchases were made with awareness that certain items were unhealthy (“junk”) and could be reliably found inside the store.
Managing Conditions for Self or Others
Most participants who described motivations for selecting healthier items cited a need or desire to manage a chronic condition, including diabetes (n = 3), hypertension (n = 3), or other health issues (n = 8), either for themselves or a family member. Explanations of chronic disease management often began as participants selected items with lower sodium or sugar content. For instance, after describing her strong preference for lightly salted pretzels, one participant elaborated on this motivation and connected it to a chronic health condition: “[Y]ou know, these are better because they don’t have as much salt contents on em. But um, you know, people of color, we have high blood pressure, so we have to watch for stuff like that.”
Health considerations extended beyond sodium and sugar. One participant (67) described a particular supplement he needed: “I’m a dialysis patient, so I need proteins. […] I have a protein drink that I get from here also. Believe it or not, they have it.” Another participant (25) indicated that her choice of breakfast cereal was motivated by a desire to lower her cholesterol. Yet, another participant was purchasing tonic water at the recommendation of her doctor in order to curb painful, diabetes-related leg cramps, while another (51) described a connection between diet and anxiety: “I have certain little stuff goin’ on in the house, like anxiety and my heart be like… And I drink smoothies and eat right and I feel better and I can tell this is playin’ a part and a role in helpin’ me feel better in my health.”
Challenge of Change
Several participants spoke about the challenge of improving their diet, especially to manage chronic health conditions. One participant described these choices in the context of a recent medical procedure: “I just had a heart scare… I just had a stent put in. […] So a lot of the stuff I need to cut out. But I’m doin’ pretty good, and I’ve cut out fried foods and you know… It’s gonna be a process for me.” After describing her “addiction” to potato chips, another participant spoke about her struggle with diet management as a diabetic: “I haven’t 100 percent mastered my eating habits. Um, I want to do better… It is hard. […] [I]t’s scary when um I uh see an individual, you know, uh who is missing a foot, a toe, and really I get scared.”
The efforts of family members to improve their diets also revealed challenges. For instance, although one participant was aware of how sodium could contribute to her husband’s high blood pressure, points of tension emerged throughout the shopping trip: “[Y]ou want me to get my regular kind? Seasoning salt? Something I don’t need to get?” Yet, at another point, the same participant discussed snack options with her husband: “You want the ones with no salt? No salt? Who eats chips with no salt?” For this couple, negotiations between health awareness and behavior took place across multiple aisles and products.
Discussion
Assist or Modulate Coping Strategy
For many, the logistics of grocery shopping are made more challenging by income constraints. Fastidious caution over budgets, sometimes down to the penny, dominated the in-store decision-making for some shoppers. Others, perhaps less guarded in their perusal of the supermarket aisles, faced upsetting results at checkout, sometimes setting aside items “for later.” After shopping, many participants had to follow complicated or inconvenient routes home, groceries in tow. The exacerbating effects of trip complexity appeared to turn what otherwise could be inconveniences into potentially large disturbances.
In light of these logistical challenges, the case supermarket represented a substantive contribution to the task of buying groceries. The location of the store presented an opportunity to shop closer to home or on the way to/from work, enabling a variety of trip types that would otherwise be unworkable or unreasonable. For example, many participants made smaller but more frequent trips to deal with challenges transporting groceries home, a strategy that is consistent with previous findings.15 Some reported having to previously travel much further, often by public transit, to enjoy a similar level of supermarket access or quality, also consistent with other studies.12,15,16 For many, without the case supermarket, shopping would be worse: more complex, inconvenient, or costly (in time or other resources).
Clean, Safe, and Friendly: A Cosmopolitan Canopy Food Environment
Sociologist Elijah Anderson uses the term “cosmopolitan canopy” to describe urban spaces where otherwise guarded city dwellers connect with one another under social controls of civility and good behavior, in contrast to more standard controls of indifference and wariness of strangers.26 Anderson’s socio-environmental construct appears relevant here. As in previous research, participants in this study valued the case supermarket for elements of physical and social civility12–17: it was clean, bright, and even “sparkling;” it was safe and orderly, reliable, and well stocked; it accommodated the needs of the elderly; and it allowed customers to feel respected and well treated. All of these elements were drawn in contrast to experiences elsewhere; in neighborhoods where this type of food shopping is not the norm, there may be unique opportunities for intervention within these “cosmopolitan canopies.”
Given the vast complexity and likely stress associated with food shopping trips in low-income, low-mobility neighborhoods, we come to understand the new store as a possible support structure within individual coping strategies. Existing research has described how shoppers in low-income neighborhoods navigate poor quality food environment in light of constraints and preferences, although this study posits that the case supermarket may also function as a socially supportive structure as a civil and convenient resource. Remembering one participant’s characterization of “shopping with wisdom,” it may be easier to be wise while shopping under a cosmopolitan canopy.
Health Awareness and Change
Health proved to be a critical theme for many shoppers in this study. Some participants were keenly aware of the healthfulness of food products, especially those who were actively managing a chronic disease for themselves or others through diet. These participants still described the challenge of changing old habits, despite their desire to change and avoid negative health consequences. If a causal model is considered of new supermarkets affecting resident health outcomes, these individuals are well within the stage of adopting and maintaining positive health behaviors, yet multiple issues remain in this process.
A variety of participant interactions underscored how changes needed to manage a chronic condition—for most, high blood pressure or diabetes—represented multiple points of challenge, many of which have been identified by previous health research.27 For example, the participant who, while aware of her husband’s condition and its relationship to diet, questioned or undermined his attempts to pursue healthier options. For another participant, managing diabetes was described as an ongoing struggle with food; grocery shopping afforded her some measures of control, although she still faced frequent in-store temptations. These participants demonstrate how, for many with chronic illnesses, there is a plurality of changes and choices that are subject to incentives and barriers, especially in the supermarket environment.
The challenge of making healthy choices and systematically repeating them was no small task within the context of old habits, limited budgets, preferences, and social factors, including the influence of family. Previous research has illuminated ways to address many of these challenges to healthy eating, including point-of-purchase interventions, although their application to food desert supermarkets appears to be limited and reliant largely on the initiative of individual store operators.5,28–35 Nonetheless, participants in this study were presented with and did sometimes choose certain healthier options in the supermarket, contextualizing these decisions within larger health concerns. It is also relevant to consider if shopping under the case supermarket “canopy,” with its associated favorable social structures, presents opportunities to lessen these challenges.
Limitations
This research design has limitations. It is possible that participants purchased healthier items in response to the presence of a researcher; favorability bias is difficult to completely avoid in this and other types of individual-level food environment research. However, bias may be limited here: the interview was a brief and unexpected encounter, limiting a participant’s ability to adjust behaviors; most participants faced firm limits in terms of time or budget, and the most explicit priming about health came from the survey, which was reserved for after shopping was complete.
The study also presents a single case of a new supermarket in a food desert. It is possible, if not likely, that individuals respond in different ways to different types of stores. Indeed, all participants were store adopters (though of varying degrees), excluding a subset of potential customers that chose to shop elsewhere. Future studies are needed in different cities and stores to validate, amend, or challenge themes identified here.
Future Directions
While current research is not optimistic about the ability of new supermarkets to influence positive health outcomes, retailers may still play a role in addressing diet-related disease. Anecdotal examples of health-oriented supermarkets5 suggest that new retailers can and sometimes do explicitly consider health, employing health promotions (conscious decision-making) and nudges (subliminal decision-making) to influence consumer purchasing.29,36,37 Corresponding health and wellness trends in the supermarket industry, including elements such as retail dietitians, nutritional labeling, health screenings, cooking classes, and healthy checkout lanes, may help create more health-promoting in-store environments.5,38
As this study has shown, the accessibility and convenience of a neighborhood supermarket can make meaningful contributions to the everyday lives of low-income shoppers. Importantly, this study also conceptualizes an in-store etiology of chronic disease, whereby shoppers carry the daily burden of managing diet-related illness, and that these decisions are difficult and multi-dimensional. Should new supermarkets in food deserts aim to assist shoppers in improving health, these realities must be more fully incorporated as a multi-level health intervention, including available and novel in-store supports for health behavior change, building upon the existing contributions to everyday life.
Acknowledgments
The author would like to acknowledge the feedback of Drs. Amy Hillier, Rosemary Frasso, Allison Karpyn, and Samina Raja, and Ms. Eliza Whiteman for her comments and assistance with qualitative coding. Store management provided vital support for the study by allowing access to their customers and facility. Partial support for Dr. Chrisinger was provided by a National Science Foundation Graduate Research Fellowship and National Institutes of Health Ruth L. Kirschstein Institutional National Research Service Award (T32-HL007034).
References
- 1.Morland K, Wing S, Diez RA. The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. Am J Public Health. 2002;92:1761–7. doi: 10.2105/AJPH.92.11.1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holsten JE. Obesity and the community food environment: a systematic review. Public Health Nutr. 2009;12:397–405. doi: 10.1017/S1368980008002267. [DOI] [PubMed] [Google Scholar]
- 3.Lee H. The role of local food availability in explaining obesity risk among young school-aged children. Soc Sci Med. 2012;74:1193–203. doi: 10.1016/j.socscimed.2011.12.036. [DOI] [PubMed] [Google Scholar]
- 4.Caspi CE, Kawachi I, Subramanian SV, Adamkiewicz G, Sorensen G. The relationship between diet and perceived and objective access to supermarkets among low-income housing residents. Soc Sci Med. 2012;75:1254–62. doi: 10.1016/j.socscimed.2012.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chrisinger, BW, If you build it, will they come, and what will they eat? Investigating supermarket development in food deserts. Dissertations available from ProQuest. Paper AAI370943. 2015. Available from: http://repository.upenn.edu/dissertations/AAI3709431. Accessed 1 Jan 2015.
- 6.Cummins S, Flint E, Matthews SA. New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff. 2014;33:283–91. doi: 10.1377/hlthaff.2013.0512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lucan SC, Hillier A, Schechter CB, Glanz K. Objective and self-reported factors associated with food-environment perceptions and fruit-and-vegetable consumption: a multilevel analysis. Prev Chronic Dis. 2014. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3970773/. Accessed 10 Dec 2015. [DOI] [PMC free article] [PubMed]
- 8.Sohi I, Bell BA, Liu J, Battersby SE, Liese AD. Differences in food environment perceptions and spatial attributes of food shopping between residents of low and high food access areas. J Nutr Educ Behav. 2014;46:241–9. doi: 10.1016/j.jneb.2013.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dubowitz T, Ghosh-Dastidar M, Cohen DA, Beckman R, Steiner ED, Hunter GP, et al. Diet and perceptions change with supermarket introduction in a food desert, but not because of supermarket use. Health Aff. 2015;34:1858–68. doi: 10.1377/hlthaff.2015.0667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ulrich V, Hillier A, DiSantis KI. The impact of a new nonprofit supermarket within an urban food desert on household food shopping. Med Res Arch [Internet]. 2015. Available from: http://www.journals.ke-i.org/index.php/index/article/view/236. Accessed 17 Dec 2015.
- 11.Ghosh-Dastidar B, Cohen D, Hunter G, Zenk SN, Huang C, Beckman R, et al. Distance to store, food prices, and obesity in urban food deserts. Am J Prev Med. 2014;47:587–95. doi: 10.1016/j.amepre.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cannuscio CC, Hillier A, Karpyn A, Glanz K. The social dynamics of healthy food shopping and store choice in an urban environment. Soc Sci Med. 2014;122:13–20. doi: 10.1016/j.socscimed.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 13.Thompson C, Cummins S, Brown T, Kyle R. Understanding interactions with the food environment: an exploration of supermarket food shopping routines in deprived neighbourhoods. Health Place. 2013;19:116–23. doi: 10.1016/j.healthplace.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Zachary DA, Palmer AM, Beckham SW, Surkan PJ. A framework for understanding grocery purchasing in a low-income urban environment. Qual Health Res. 2013;23:665–78. doi: 10.1177/1049732313479451. [DOI] [PubMed] [Google Scholar]
- 15.Munoz-Plaza CE, Morland KB, Pierre JA, Spark A, Filomena SE, Noyes P. Navigating the urban food environment: challenges and resilience of community-dwelling older adults. J Nutr Educ Behav. 2013;45:322–31. doi: 10.1016/j.jneb.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 16.Munoz-Plaza CE, Filomena S, Morland KB. Disparities in food access: inner-city residents describe their local food environment. J Hunger Environ Nutr. 2008;2:51–64. doi: 10.1080/19320240801891453. [DOI] [Google Scholar]
- 17.Zenk SN, Schulz AJ, Israel BA, Mentz G, Miranda PY, Opperman A, et al. Food shopping behaviours and exposure to discrimination. Public Health Nutr. 2014;17:1167–76. doi: 10.1017/S136898001300075X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.U.S. Census Bureau. Selected economic characteristics, 2009–2013 5-year American community survey [Internet]. 2013. Available from: http://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk. Accessed 10 Dec 2015.
- 19.Miaux S, Drouin L, Morency P, Paquin S, Gauvin L, Jacquemin C. Making the narrative walk-in-real-time methodology relevant for public health intervention: towards an integrative approach. Health Place. 2010;16:1166–73. doi: 10.1016/j.healthplace.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 20.Frasso R. Walking interviews: speaking with consumers while they shop where they live. APHA; 2014. Available from: https://apha.confex.com/apha/142am/webprogram/Paper311652.html. Accessed 10 Dec 2015.
- 21.Chuan Ling AM, Horwath C. Perceived benefits and barriers of increased fruit and vegetable consumption: validation of a decisional balance scale. J Nutr Educ. 2001;33:257–65. doi: 10.1016/S1499-4046(06)60289-3. [DOI] [PubMed] [Google Scholar]
- 22.Henry H, Reicks M, Smith C, Reimer K, Atwell J, Thomas R. Identification of factors affecting purchasing and preparation of fruit and vegetables by stage of change for low-income African American mothers using the think-aloud method. J Am Diet Assoc. 2003;103:1643–6. doi: 10.1016/j.jada.2003.09.039. [DOI] [PubMed] [Google Scholar]
- 23.Kim DJ, Holowaty EJ. Brief, validated survey instruments for the measurement of fruit and vegetable intakes in adults: a review. Prev Med. 2003;36:440–7. doi: 10.1016/S0091-7435(02)00040-3. [DOI] [PubMed] [Google Scholar]
- 24.Mainvil LA, Lawson R, Horwath CC, McKenzie JE, Hart I. Validated scales to assess adult decisional balance to eat more fruits and vegetables. Appetite. 2010;55:454–65. doi: 10.1016/j.appet.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 25.MacQueen KM, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. Field Methods. 1998;10:31–6. doi: 10.1177/1525822X980100020301. [DOI] [Google Scholar]
- 26.Anderson E. The cosmopolitan canopy. Ann Am Acad Pol Soc Sci. 2004;595:14–31. doi: 10.1177/0002716204266833. [DOI] [Google Scholar]
- 27.Kelly S, Martin S, Kuhn I, Cowan A, Brayne C, Lafortune L. Barriers and facilitators to the uptake and maintenance of healthy behaviours by people at mid-life: a rapid systematic review. PLoS ONE. 2016;11:e0145074. doi: 10.1371/journal.pone.0145074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gittelsohn J, Song H-J, Suratkar S, Kumar MB, Henry EG, Sharma S, et al. An urban food store intervention positively affects food-related psychosocial variables and food behaviors. Health Educ Behav [Internet]. 2009. Available from: http://heb.sagepub.com/content/early/2009/11/03/1090198109343886. Accessed 28 Nov 2015. [DOI] [PubMed]
- 29.Gittelsohn J, Lee K. Integrating educational, environmental, and behavioral economic strategies may improve the effectiveness of obesity interventions. Appl Econ Perspect Policy. 2013;35:52–68. doi: 10.1093/aepp/pps044. [DOI] [Google Scholar]
- 30.Phipps EJ, Kumanyika SK, Stites SD, Singletary SB, Cooblall C, DiSantis KI. Buying food on sale: a mixed methods study with shoppers at an urban supermarket, Philadelphia, Pennsylvania, 2010–2012. Prev Chronic Dis [Internet]. 2014. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4157594/. Accessed 28 Nov 2015. [DOI] [PMC free article] [PubMed]
- 31.Phipps EJ, Braitman LE, Stites SD, Singletary SB, Wallace SL, Hunt L, et al. Impact of a rewards-based incentive program on promoting fruit and vegetable purchases. Am J Public Health. 2014;105:166–72. doi: 10.2105/AJPH.2013.301752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Foster GD, Karpyn A, Wojtanowski AC, Davis E, Weiss S, Brensinger C, et al. Placement and promotion strategies to increase sales of healthier products in supermarkets in low-income, ethnically diverse neighborhoods: a randomized controlled trial. Am J Clin Nutr. 2014;99:1359–68. doi: 10.3945/ajcn.113.075572. [DOI] [PubMed] [Google Scholar]
- 33.Cohen DA, Lesser LI. Obesity prevention at the point of purchase. Obes Rev 2016; Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 34.Milliron B-J, Woolf K, Appelhans BM. A point-of-purchase intervention featuring in-person supermarket education affects healthful food purchases. J Nutr Educ Behav. 2012;44:225–32. doi: 10.1016/j.jneb.2011.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–72. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 36.Galizzi MM. What is really behavioral in behavioral health policy? And does it work? Appl Econ Perspect Policy. 2014; ppt036.
- 37.Thaler RH, Sunstein CR. Libertarian paternalism. Am Econ Rev. 2003;93:175. doi: 10.1257/000282803321947001. [DOI] [Google Scholar]
- 38.Prevention Magazine Research Department, Food Marketing Institute Research Department, Rodale. Shopping for Health 2013 [Internet]. 2013. Available from: http://www.fmi.org/docs/default-source/2012-health-wellness-conference-presentations/shopping-for-health-2013.pdf?sfvrsn=2. Accessed 25 Jun 2014.