Abstract
To study and compare the outcomes of the endoscopic versus microscopic approach to Myringoplasty in 60 patients. In this prospective study, the outcomes of 60 ears of 60 patients (40 male and 20 female) who underwent Myringoplasty were evaluated. The age range of the patients was 15–55 years. Group 1 underwent Myringoplasty with an endoscopic technique (n = 30), and Group 2 underwent Myringoplasty with the conventional microscopic technique (n = 30). A temporalis fascia graft was used in both groups. The outcomes were analyzed in terms of the hearing gain, duration of surgery, graft success rate and advantages and disadvantages of endoscopic versus microscopic approach to Myringoplasty. In both groups, the postoperative air-bone gap (ABG) was significantly lower than the preoperative ABG. There were no significant differences between the preoperative and postoperative ABG values (in dB) in either group. The mean operative duration in Group 1 (96.32 min) was significantly lower than that in Group 2 (136.09 min). In the preoperative evaluation of patients in Group 1 had small, medium, large perforations are 16 (53 %), 12 (40 %), and 02 (7 %), respectively. In Group 2, had small, medium, large perforations are 12 (40 %), 15 (50 %), and 03 (10 %), respectively. Perforations (wet ear) were detected in 10 (33 %), 06 (20 %), and 04 (12 %) of the patients in Group 1 at postoperative months 1, 3, and 6, respectively. Perforations (wet ear) were detected 09 (30 %), 06 (20 %) and 03 (10 %) patients in Group 2 at postoperative months 1, 3, and 6. At 6 months postoperatively, there were smaller perforations and reduced rate of perforations as compared to 1st and 3rd month in Group 1 and Group 2. The difference between the perforation conditions (larger vs. smaller) was not significant in either group. The preoperative and postoperative increases in the ABG were associated. At the end of 6 months all (100 %) patients in the Group 1 rated their cosmetic result as excellent as compared in the Group 2. Unlike the microscope, the endoscope is easily transportable and hence is ideal for use in ear surgery camps conducted in remote places. In patients undergoing Myringoplasty, especially if the external ear canal is narrow and the anterior canal wall is prominent, the endoscopic and microscopic approaches appear to give equal results in terms of easy visualization of the entire tympanic membrane and no requirement for extra intervention to evaluate the ossicular system. A shorter operative duration and excellent cosmetic result is an advantage of the endoscopic Myringoplasty technique.
Keywords: Endoscopic myringoplasty, Microscopic myringoplasty, Operative duration
Introduction
Chronic Suppurative Otitis Media is a chronic infection of the middle ear cleft. There are two types of Chronic Suppurative Otitis Media, the safe type and unsafe type Wullstein [3]. The safe type has central perforation and the complications are less and not dangerous. The Unsafe type is because of the Attico antral disease with Attic or Posterior Marginal Perforation. The Intracranial complications in this type are due to the bone eroding properties of the Grannulations and Cholesteatoma.
The main treatment for the safe type of Chronic Suppurative Otitis Media is medical. If the perforation is not healing and the deafness is persistent, it requires the Surgical Closure of the perforation by Myringoplasty, by using temporalis fascia graft Glasscock [2]. The Unsafe type requires Surgical Treatment, Mastoidectomy of various types depending on the disease process.
Advantages of endoscopic myringoplasty
This surgical procedure fulfils the criteria of minimally invasive surgical procedure.
Equipment is portable
It is cost effective.
Disadvantages
Since the non dominant hand is used to hold the endoscope only one hand is available for surgery.
Learning curve is very steep.
Aim of the Study
To determine the advantages and disadvantages of endoscope as compared to microscope in myringoplasty surgery and to compare the results of both groups.
Materials and Methods
The cases for this study were taken from the Inpatient cases of the Department of Otorhinolaryngology, Govt. General Hospital, Nizamabad, Telangana, during the period from Jan 2013 to Dec 2014 (2 years).
30 cases were taken for this study under each group.
Inclusion Criteria
Patients having small, medium and large dry central perforation of tympanic membrane.
Patients not having evidence of active infection of nose, throat and
Para nasal sinuses.
Exclusion Criteria
Patients having hearing loss of sensori neural type or mixed type.
Ossicular abnormality in pre-op or during surgery.
Patient with clinical and radiological evidence of attico-antral disease.
Patients with history of previous surgery for chronic otitis media.
All the patients who presented with signs and symptoms suggesting tubo tympanic type of CSOM were submitted to an assessment protocol, based on a guided history taking, specific physical exam (otoscopy), and subjected to audiogram. During history taking, the patients were questioned about disease onset, and if they had undergone previous otologic surgeries.
Pure tone threshold audiometry has become the standard behavioral procedure for describing audiometry sensitivity, therefore, pure tone audiometry had been used for assessment of hearing level in this study.
The Audiometer, Elcon 3N3 Multi was used in this study and was manual as shown in the Fig. 1.
Fig. 1.

Audiometer, Elcon 3N3 Multi
The test was performed in acoustically treated room with no ambience noise. The audiometry was done following standard protocol. Patient was explained about the procedure before audiometry and adequate time was taken for testing.
The technique followed was Carhart and Jerger’s technique which is mostly used (technique of 5 up and 10 down method).
For calculation of average of hearing loss (air conduction threshold) three frequencies were selected. They were, 500, 1000 and 2000 Hz. These frequencies were selected because they represent speech frequency range and elevation of threshold in these frequencies will be clinically significant.
Air bone gap calculated by subtracting average bone conduction threshold from average air conduction threshold.
The operations are performed under local anesthesia using a microscope with a lens of 250 mm. In all of the cases post auricular approach was used.In all cases temporalis fascia graft was harvested and underlay grafting done.
All the patients are followed after surgery on the 7th and 14th post operative days. The audiogram was done on between 12 and 24 weeks to assess the outcome i.e. the improvement of hearing objectively.
Observations and Results
In the present study, the patients were selected from those presenting to the Department of ENT, Head and Neck Surgery, Govt. General Hospital, Nizamabad, Telangana for prospective study during the period from Jan 2013 to Dec 2014.
60 cases were examined, dividing into two groups and each group containing 30 cases were selected for the study.
A period of 24 months was taken for the study.
- EAM
Endoscope assisted myringoplasty
- MM
Microscopic myringoplasty
As per the Table 1, The age of the patients ranged from 15 to 55 years. Majority (70 %) 0f our patients were in their second and third decades of life.
Table 1.
Showing the age distribution among two groups
| Age | MM | EAM |
|---|---|---|
| 15–25 | 12 (40 %) | 07 (25 %) |
| 26–35 | 09 (30 %) | 13 (42 %) |
| 36–45 | 05 (17 %) | 08 (26 %) |
| Above 45 | 04 (13 %) | 02 (7 %) |
As per the observations made on sex incidence showed in Table 2, the male patients predominated over their female counterparts in this series, the exact number being 40 (i.e. 66 %) made while female patients were only 20 (34 %) in number.
Table 2.
Showing the sex incidence
| Sex | MAM | EAM |
|---|---|---|
| Male | 18 (60 %) | 22 (73 %) |
| Female | 12 (40 %) | 8 (27 %) |
As per the Table 3, it was observed that among the 60 cases those were studied, small and medium size perforation was seen in 55 cases. i.e., 90 % of all the cases taken for the study.
Table 3.
Size of the perforation
| Size of perforation | MAM | EAM |
|---|---|---|
| Small | 12 (40 %) | 16 (53 %) |
| Medium | 15 (50 %) | 12 (40 %) |
| Large | 03 (10 %) | 02 (7 %) |
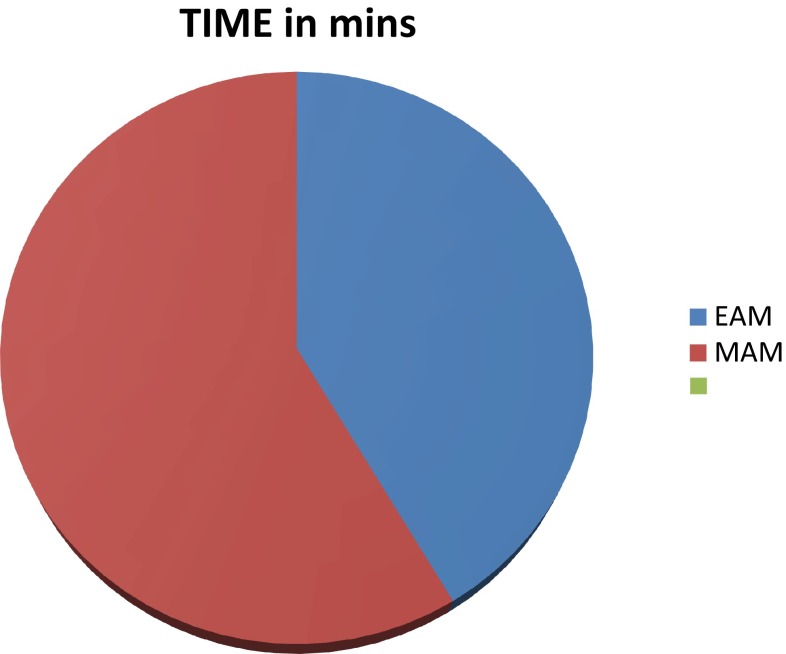
As per Fig. 2, it was observed that endoscope assisted myrigoplasty required an average 96.32 min (range of 80–120 min) and microscopic myringoplasty required an average of 136.09 min (range of 110–160 min).
Fig. 2.
Time taken in minutes
Microscopic Myringoplasty
As per the Table 4, In microscopic myringoplasty group it is observed that 12 cases (40 %) had an average conductive hearing loss of 11–20 dB and 18 cases (60 %) had an average conductive hearing loss of 21–30 dB. Almost 100 % of group had an average conductive hearing loss of range 11–30 dB.
Table 4.
.
| Average CHL (dB) | MAM | EAM | ||
|---|---|---|---|---|
| Pre-op | Post-op | Pre-op | Post-op | |
| 0–10 | 0 (0 %) | 7 (25 %) | 0 (0 %) | 14 (46 %) |
| 11–20 | 12 (40 %) | 19 (65 %) | 12 (40 %) | 13 (44 %) |
| 21–30 | 18 (60 %) | 3 (10 %) | 15 (50 %) | 3 (10 %) |
| 31–40 | 0 (0 %) | 0 (0 %) | 3 (10 %) | 0 (0 %) |
Post operatively in the same group after 6 months follow up we noticed improvement with decrease in average conductive hearing loss with 07 cases (25 %) having an average between 0–10 dB and 19 cases (65 %) having an average of 11–20 dB conductive hearing loss. Almost 90 % of post operative group has an improvement in conductive hearing loss with average between 0 and 20 dB conductive hearing loss.
Endoscope Assisted Myringoplasty
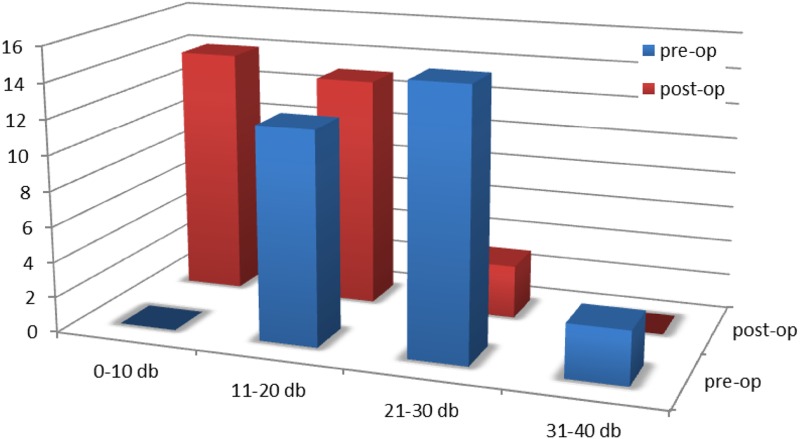 In endoscope assisted myringoplasty group it is observed that 12 cases (40 %) had an average conductive hearing loss of 11–20 dB and 15 cases (50 %) had an average conductive hearing loss of 21–30 dB. Almost 90 % of the group had an average conductive hearing loss of range 11–30 dB.
In endoscope assisted myringoplasty group it is observed that 12 cases (40 %) had an average conductive hearing loss of 11–20 dB and 15 cases (50 %) had an average conductive hearing loss of 21–30 dB. Almost 90 % of the group had an average conductive hearing loss of range 11–30 dB.
Post operatively in the same group after 6 months follow up we noticed improvement with decrease in average conductive hearing loss with 14 cases (46 %) having an average between 0 and 10 dB and 13 cases (44 %) having an average of 11–20 dB conductive hearing loss. Almost 90 % of post operative group has an improvement in conductive hearing loss with average between 0 and 20 dB conductive hearing loss.
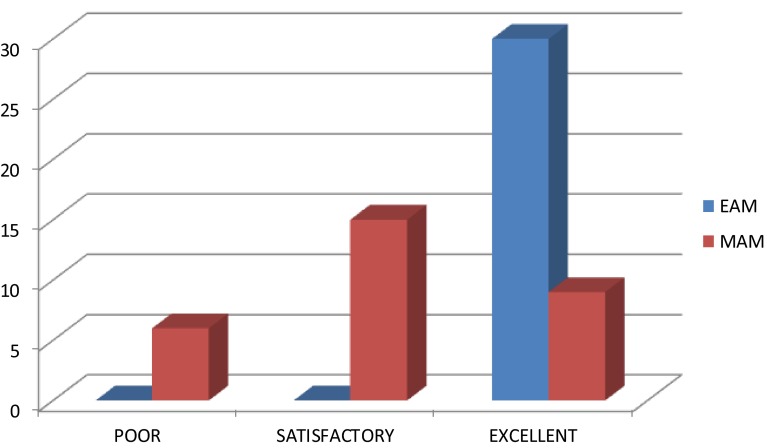
As per Fig. 3, at the end of 6 months, all (100 %) patients in the endoscope group rated their cosmetic result as excellent, where as in the microscope group 06 (20 %) patients rated their cosmetic result as poor, 15 (50 %) rated the cosmetic result as satisfactory and 9 (30 %) patients rated their cosmetic result as excellent.
Fig. 3.
Subjective cosmetic result
Objective analysis revealed that in endoscope group none (0 %) of the patients had a visible scar, whereas in the microscope group 21 (70 %) patients had a visible scar and in 09 (30 %) patients the scar was not visible.
Endoscope Assisted Myringoplasty
Microscopic Myringoplasty
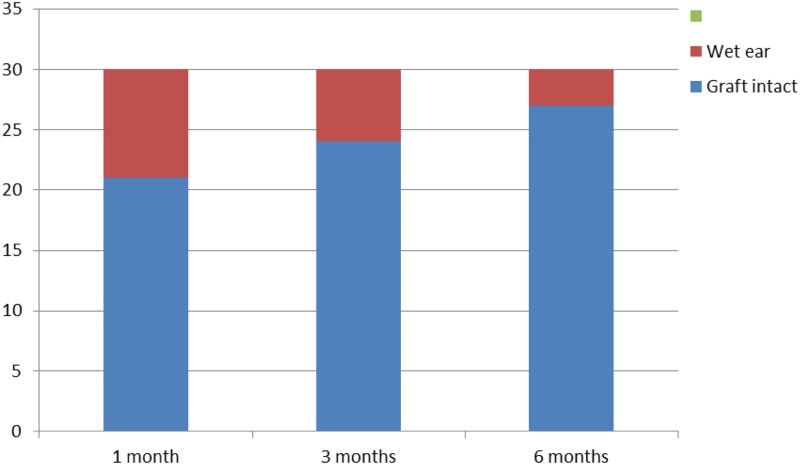
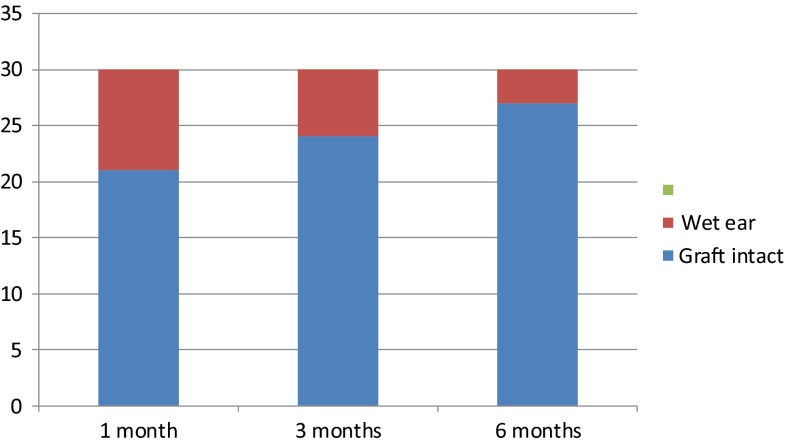 As per
Table 5, At 6 months follow up 26 (88 %) patients had a successful outcome in the endoscope group and 27 (90 %) patients had a successful outcome in microscope group.
As per
Table 5, At 6 months follow up 26 (88 %) patients had a successful outcome in the endoscope group and 27 (90 %) patients had a successful outcome in microscope group.
Table 5.
.
| EAM | MAM | |||
|---|---|---|---|---|
| Graft intact | Wet ear | Graft intact | Wet ear | |
| 1 month | 20 (68 %) | 10 (32 %) | 21 (70 %) | 09 (30 %) |
| 3 months | 24 (80 %) | 06 (20 %) | 24 (80 %) | 06 (20 %) |
| 6 months | 26 (88 %) | 04 (12 %) | 27 (90 %) | 03 (10 %) |
Differences between two groups were not statistically significant in terms of success rate and complication rate (wet ear).
Discussion
This study was undertaken with the objective of determining the advantages & disadvantages of endoscope when compared to the conventional operating microscope in myringoplasty surgery. The Endoscope Assisted Myringoplasty is advantageous. Similar results were seen in a study by Patil [10]. El-Guindy [8] in a study revealed that the Endoscopic Myringoplasty gives almost the same results in closure of perforation as in Microscopic Myringoplasty.
Variations of external auditory canal like stenosis, tortuosity, bony overhangs etc. hamper the view of tympanic membrane when visualized through microscope. Therefore a need to manipulate the patients head or the microscope repeatedly to visualize all the parts of tympanic membrane. Sometimes,in spite of manipulation, tympanic membrane will not be fully visualized and canaloplasty has to be done. This in turn may increase the operation time, Wullstien [5].
In sharp contrast, the endoscope brings the surgeon’s eye to the tip of the scope.The wide angle of zero degree scope visualizes the entire tympanic membrane. There is no need to frequently adjust the patients head or to do canaloplasty thereby saving operative time—Rosenberg [11] and Jadav et al. [13].
Similar observations were made in two separate studies by Tarabichi [1] and Usami et al. [9].
With angled endoscopes Raj and Meher [6], reported that it is possible to visualize other structures like round window niche, Eustachian tube orifice, incudo stapedial joint.
By avoiding post aural incision in Endoscopic Myringoplasty there is less dissection of normal tissues, less intra operative bleeding, less incidence of post operative pain and better cosmetic result. Avoiding post aural route also reduces chance of auricular displacement and asymmetry of pinna.
In 2008 Mohindra et al. [7] did 49 cases of myringoplasty and six cases of ossiculoplasties through the transcanal route using rigid endoscopes
Our observation has found that positioning the graft was much easier and faster with the endoscope as it gives a wide angled view which includes the entire tympanic membrane, the graft and medial end of external auditory canal.
Unlike the microscope, the endoscope is easily transportable and hence is ideal for use in ear surgery in camps conducted in remote places.
The disadvantage of endoscopic ear surgery is one handed technique. Scope has to be held in one hand and other hand is free to operate and this becomes cumbersome when there is excessive bleeding, which can be managed easily in microscope assisted ear surgery where one hand can be used to suction the blood and simultaneously the other hand can be used to operate. We confirm these observations which were reported in studies by Tarabichi [1] and Karhuketoet al. [12]. This problem can be solved by developing a stand for endoscope which will fix it in desired position so that both the hands will be free to operate.
Another disadvantage of endoscope is that even a small amount of blood can totally obscure the view of operative field. Meticulous haemostasis is therefore a must in endoscopic ear surgery. Arm fatigue by the weight of the scope, neck strain and back ache can be solved by developing a stand for scope.
Endoscope provides monocular vision which leads to loss of depth perception compared to the binocular vision provided by microscope and this will be noticed more by a beginner. Extra care to be taken to ascertain that the graft had been lifted enough to make contact with edges of perforation, Raj et al. [4]
Endoscopic ear surgery requires investment in endoscope, camera and monitor. But for a surgeon doing endoscopic sinus surgeries, there will be no added cost as same scope,camera and monitor can be used for ear surgeries as well.
Conclusion
The wide angle, telescopic, magnified view of the endoscope overcomes most of the disadvantages of the microscope.
In our study, the success rate of endoscope assisted myringoplasty was comparable to that of microscopic myringoplasty. In terms of cosmosis, The scar by endoscopic myringoplasty is invisible.
Loss of depth perception and one handed technique are some of the disadvantages of the endoscope that can be easily overcome with practice. Endoscope is ideal for ear surgery in camps held in remote places.
We feel that endoscope has a definite place in myringoplasty.
Compliance with Ethical Standards
Conflict of interest
The authors of this article declare that he/she has no conflict of interest.
Human and Animal Rights
Animals were not involved in this study.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Tarabichi M. Endoscopic middle ear surgery. Ann Otol Rhinol Laryngol. 1999;108:39–46. doi: 10.1177/000348949910800106. [DOI] [PubMed] [Google Scholar]
- 2.Glasscock ME. Tympanic membrane grafting with fascia; overlay vs. undersurface technique. Laryngoscope. 1973;83(5):754–770. doi: 10.1288/00005537-197305000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Wullstein H. The restoration of the function of the middle ear, in chronic otitis media. Ann Otol Rhinol Laryngol. 1956;65:1020–1041. doi: 10.1177/000348945606500416. [DOI] [PubMed] [Google Scholar]
- 4.Raj A, Meher R. Endoscopic transcanal myringoplasty—a study. Indian J Otolaryngol Head Neck Surg. 2001;53(1):47–49. doi: 10.1007/BF02910979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wullstien H. Technic and early results of tympanoplasty. Monatsschr Ohrenheilkd Laryngorhinol. 1953;87(4):308–311. [PubMed] [Google Scholar]
- 6.Raj A, Meher R. Endoscopic transcanal myringoplasty—a study. Indian J Otolaryngol Head Neck Surg. 2001;53:47–49. doi: 10.1007/BF02910979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohindra S, Panda NK. Ear surgery without microscope; is it possible. Indian J Otolaryngol Head Neck Surg. 2010;62(2):138–141. doi: 10.1007/s12070-010-0033-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Guindy A. Endoscopic transcanal myringoplasty. J Laryngol Otol. 1992;106:493–495. doi: 10.1017/S0022215100119966. [DOI] [PubMed] [Google Scholar]
- 9.Usami S, Iijima N, Fujita S, et al. Endoscope-assisted myringoplasty. Otorhinolaryngology. 2001;63:287–290. doi: 10.1159/000055759. [DOI] [PubMed] [Google Scholar]
- 10.Patil RN. Endoscopic tympanoplasty—definitely advantageous (preliminary reports) Asian J Ear Nose Throat. 2003;25:9–13. [Google Scholar]
- 11.Rosenberg SI. Endoscopic otologic surgery. Otolaryngol Clin North Am. 1996;29:291–300. [PubMed] [Google Scholar]
- 12.Karhuketo TS, Ilomaki JH, Puhakka HJ. Tympanoscope-assisted myringoplasty. Otorhinolaryngology. 2001;63:353–358. doi: 10.1159/000055773. [DOI] [PubMed] [Google Scholar]
- 13.Jadav SP, et al. Endoscope assisted myringoplasty. Singap Med J. 2009;50(5):510. [PubMed] [Google Scholar]