Abstract
This study aims to define the surgical boundaries of adenoidectomy by demonstrating that recurrence of adenoids and its symptoms can be avoided if a complete adenoidectomy is performed, by following these surgical limits. A prospective descriptive study was carried out at Speciality ENT Hospital, Mumbai, India. Endoscopic adenoidectomy was performed in 83 patients using coblation technology. In all patients, adenoids were removed superiorly till the periosteum over the body of sphenoid; posteriorly till the pharyngobasilar fascia; laterally till fossa of Rosenmuller in the posterior part and till the torus tubarius in the anterior part; and inferiorly till the Passavant’s ridge. The patients were followed up postoperatively and a nasal endoscopy was done at the end of 1 year to look for any recurrence or regrowth of adenoids, so as to determine the efficacy of the procedure. A total of 83 patients underwent adenoidectomy with a mean age of 12.80 years. 12 patients were lost to follow up. Of the remaining 71 patients, no patient showed any evidence of recurrence of adenoid on follow-up nasal endoscopy done at the end of 1 year. Recurrence of adenoid post adenoidectomy is not seen if there is complete removal of adenoids. So it is essential that all adenoid tissue be removed during adenoidectomy. The complete removal of adenoids can be ensured by following the surgical limits of adenoidectomy.
Keywords: Adenoid, Regrowth, Surgical limits, Pharyngobasilar fascia, Coblation
Introduction
Adenoids are an aggregation of lymphoid tissue, present at the junction of the roof and the posterior wall of the nasopharynx. It forms a part of the inner Waldeyer’s ring and acts as a line of defence against inhaled microorganisms and allergens. These adenoids may get repeatedly or chronically infected, leading to adenoiditis and adenoid hypertrophy.
Adenoid hypertrophy causes nasal obstruction and airway problems such as snoring or obstructive sleep apnoea [1], recurrent sinusitis, or eustachian tube dysfunction. There is also reduced ability to smell and taste, hyponasal speech and craniofacial abnormalities [2]. These complications frequently lead to a need for adenoidectomy.
Adenoidectomy is one of the most common ENT surgical procedures performed in the paediatric age group. It is usually performed with an adenoid curette. Nowadays, there has been an increase in use of endoscopes, suction diathermy, coblation and powered instruments so as to minimize complications and improve outcomes [3–6]. The common intra-operative complications encountered are bleeding and injury to Eustachian tubes. Post-operatively, recurrence of adenoids or its symptoms is one of the commonest complications. However, it is not only the technology used, but also the extent of adenoidectomy, that determines the outcome of the surgery and the complications encountered. The true boundaries for the procedure of adenoidectomy are yet to be defined. The aim of this study is to describe the surgical limits of adenoidectomy so as to give an optimal outcome to the patient without any post operative recurrence or regrowth of adenoids.
Materials and Methods
A prospective descriptive study was conducted at Speciality ENT hospital in Mumbai, India from January 2013 to October 2015. All patients having symptomatic adenoid hypertrophy not responding to maximal medical management were included in the study. Patients were excluded if there was any suspicion of lymphoma. Presence of adenoid hypertrophy was confirmed by diagnostic nasal endoscopy. All the patients underwent endoscopic coblation adenoidectomy, and the procedure was performed by the same surgeon in the same hospital setting.
Surgical Technique
The procedure was performed under general anaesthesia with orotracheal intubation. The patient was kept in Trendelenburg position, with the head approximately 15° below horizontal so as to prevent the flow of saline from the coblation wand towards the laryngeal airway. The mouth was opened using a Boyle Davis mouth gag. A red rubber tube was passed through one of the nostrils and brought out through the mouth to elevate the soft palate. Cotton patties soaked in 4 % lignocaine and 1:10,000 adrenaline were used to decongest the nose. In patients aged 4 years and above, a 4 mm, 0° Hopkins rigid endoscope was introduced through the nose to visualize the adenoids. In patients aged <4 years, a 4 mm, 70° Hopkins rigid endoscope was passed through the mouth for visualisation of the adenoids. The EVac® 70 XTRA HP Coblation Wand (smith-nephew) was bent by 30°–40° at the distal one-third, so as to reach the nasopharynx through the oral cavity. The adenoid tissue was removed in layers from anterior to posterior, using the coblation wand. Each layer was removed, starting from its inferior most point and moving superiorly. The limits of adenoidectomy were defined as follows: superiorly till the periosteum over the body of sphenoid; posteriorly till the pharyngobasilar fascia (Fig. 1); laterally till the fossa of Rosenmuller in the posterior part and the torus tubarius in the anterior part; and inferiorly till the Passavant’s ridge. Haemostasis was achieved using the coblation wand. No nasopharyngeal packing was required at the end of the procedure in any case. A follow up nasal endoscopy was done at the end of 1 year, to determine any recurrence of the adenoids.
Fig. 1.
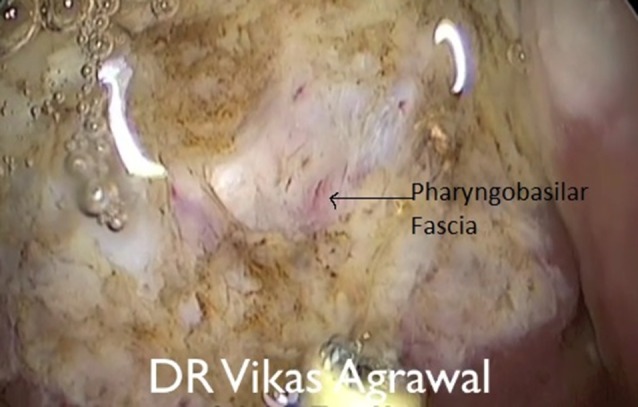
Delineating pharyngobasilar fascia
Results
A total of 83 patients underwent adenoidectomy from January 2013 till October 2014. The youngest patient was aged 2 years 2 months and the oldest was aged 40 years with a mean age of 12.80 years. 30 patients were female and 53 patients were male. The approximate intra-operative blood loss was 2–3 ml. There was no reactionary or secondary haemorrhage, or any foul smelling discharge in any of the patients At the end of 1 year, a nasal endoscopy was done to check for any recurrence of adenoids. Out of the 83 patients, 12 patients did not return for the follow up endoscopy. No recurrence of adenoid tissue was found in any of the other 71 patients at the end of 1 year.
Discussion
Regrowth of adenoids after adenoidectomy, which is a very common ENT procedure, is well known [7–10]. Joshua et al. [9] found recurrence of adenoids in patients with recurring symptoms post adenoidectomy. However, Lesiskas et al. [11] were of the view that recurrence of symptoms post adenoidectomy were rhinogenic in origin. Tubal tonsils have also been implicated for causing persistent symptoms post adenoidectomy [12, 13]. In some patients the symptoms may advocate a repeat surgical procedure [13–15].
Since after conventional curettage adenoidectomy, approximately 39 % patients have residual adenoids [16], endoscope assisted and powered instrument assisted adenoidectomies have been recommended [16–18]. However, in spite of using these techniques regrowth of adenoids is seen [15]. There have been no studies which completely describe the limits of surgical adenoidectomy so as to ensure complete removal of adenoids. This study aims to define the surgical boundaries of adenoidectomy by demonstrating that it is not just the technique of adenoidectomy used, but the extent of adenoidectomy which determines the regrowth of adenoids and recurrence of symptoms.
The adenoid is a mass of mucosa associated lymphoid tissue present in the nasopharynx arising from its roof and the posterior wall. The superior constrictor muscles are absent in this region and the space between the skull base and the superior constrictor muscle is filled by the pharyngeal aponeurosis formed by the pharyngobasilar fascia. Superiorly the adenoids are limited by the sphenoid bone. Laterally, we have the fossa of Rosenmuller, the torus tubarius and the lateral pharyngeal wall which limit the growth of adenoids. In our study, in every case of adenoidectomy, we removed the adenoids superiorly till the periosteum over the body of sphenoid; posteriorly till the pharyngobasilar fascia; laterally till fossa of Rosenmuller in the posterior part and till the torus tubarius in the anterior part; and inferiorly till the Passavant’s ridge (Fig. 2). A follow up nasal endoscopy was done at the end of 1 year, and no patient showed any recurrence of adenoid or its symptoms.
Fig. 2.
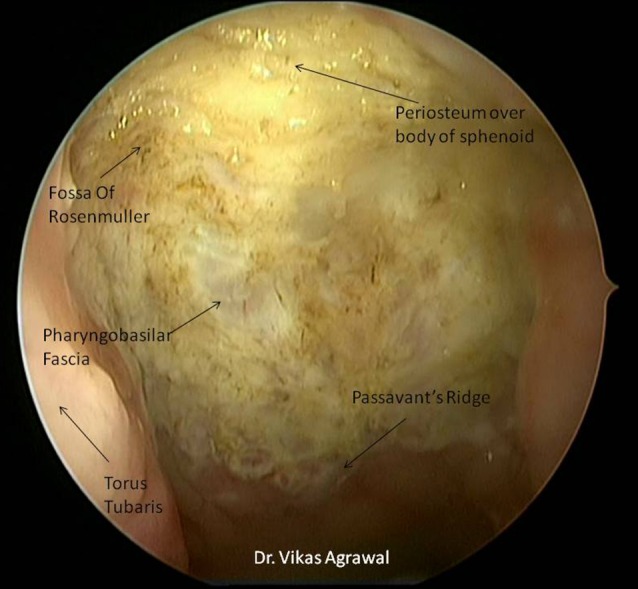
Surgical boundaries of adenoidectomy
Conclusion
Recurrence of symptoms post adenoidectomy is due to presence of adenoid remnants which can regrow. Ensuring a complete removal of adenoids can help avoid this complication. There was no recurrence of adenoid in any patient when the surgical limits of adenoidectomy as described in this study were followed. Therefore, superiorly the periosteum over the body of sphenoid; posteriorly the pharyngobasilar fascia; laterally the fossa of Rosenmuller in the posterior part and the torus tubarius in the anterior part; and inferiorly the Passavant’s ridge can be considered as surgical limits of adenoidectomy.
Compliance with Ethical standards
Conflict of interest
Vikas Agrawal, Pranay Kumar Agarwal and Aniruddh Agrawal declares that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Ravindran VK. Adeno-tonsillar hypertrophy as a cause of sleep apnoea syndrome. Med J Malaysia. 1983;38(2):164–166. [PubMed] [Google Scholar]
- 2.Linder-Aronson S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the denition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl. 1970;265:1–132. [PubMed] [Google Scholar]
- 3.Benninger M, Walner D. Coblation: improving outcomes for children following adenotonsillectomy. Clin Cornerstone. 2007;9(Suppl 1):S13–S23. doi: 10.1016/S1098-3597(07)80005-6. [DOI] [PubMed] [Google Scholar]
- 4.Hartley BEJ, Papsin BC, Albert DM. Suction diathermy adenoidectomy. Clin Otolaryngol Allied Sci. 1998;23(4):308–309. doi: 10.1046/j.1365-2273.1998.00148.x. [DOI] [PubMed] [Google Scholar]
- 5.Huang H-M, Chao M-C, Chen Y-L, Hsiao H-R. A combined method of conventional and endoscopic adenoidectomy. Laryngoscope. 1998;108(7):1104–1106. doi: 10.1097/00005537-199807000-00028. [DOI] [PubMed] [Google Scholar]
- 6.Koltai PJ, Kalathia AS, Stanislaw P, Heras HA. Power-assisted adenoidectomy. Arch Otolaryngol Head Neck Surg. 1997;123(7):685–688. doi: 10.1001/archotol.1997.01900070023004. [DOI] [PubMed] [Google Scholar]
- 7.Kim SY, Lee WH, Rhee CS, Lee CH, Kim JW. Regrowth of the adenoids after coblation adenoidectomy: cephalometric analysis. Laryngoscope. 2013;123(10):2567–2572. doi: 10.1002/lary.23984. [DOI] [PubMed] [Google Scholar]
- 8.Fischer L. Recurring adenoids in children. J Am Med Assoc LVIII. 1912;2:106–107. doi: 10.1001/jama.1912.04260010108016. [DOI] [Google Scholar]
- 9.Joshua B, Bahar G, Sulkes J, Shpitzer T, Raveh E. Adenoidectomy: long-term follow-up. Otolaryngol Head Neck Surg. 2006;135(4):576–580. doi: 10.1016/j.otohns.2006.05.027. [DOI] [PubMed] [Google Scholar]
- 10.Buchinsky FJ, Lowry MA, Isaacson G. Do adenoids regrow after excision? Otolaryngol Head Neck Surg. 2000;123(5):576–581. doi: 10.1067/mhn.2000.110727. [DOI] [PubMed] [Google Scholar]
- 11.Lesinskas E, Drigotas M. The incidence of adenoidal regrowth after adenoidectomy and its effect on persistent nasal symptoms. Eur Arch Otorhinolaryngol. 2009;266(4):469–473. doi: 10.1007/s00405-008-0892-5. [DOI] [PubMed] [Google Scholar]
- 12.Emerick KS, Cunningham MJ. Tubal tonsil hypertrophy: a cause of recurrent symptoms after adenoidectomy. Arch Otolaryngol Head Neck Surg. 2006;132(2):153–156. doi: 10.1001/archotol.132.2.153. [DOI] [PubMed] [Google Scholar]
- 13.Monroy A, Behar P, Brodsky L. Revision adenoidectomy—a retrospective study. Int J Pediatr Otorhinolaryngol. 2008;72(5):565–570. doi: 10.1016/j.ijporl.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Liapi A, Dhanasekar G, Turner NO. Role of revision adenoidectomy in paediatric otolaryngological practice. J Laryngol Otol. 2006;120(3):219–221. doi: 10.1017/S0022215106005585. [DOI] [PubMed] [Google Scholar]
- 15.Sapthavee A, Bhushan B, Penn E, Billings KR. A comparison of revision adenoidectomy rates based on techniques. Otolaryngol Head Neck Surg. 2013;148(5):841–846. doi: 10.1177/0194599813477830. [DOI] [PubMed] [Google Scholar]
- 16.Havas T, Lowinger D. Obstructive adenoid tissue: an indication for powered-shaver adenoidectomy. Arch Otolaryngol Head Neck Surg. 2002;128(7):789–791. doi: 10.1001/archotol.128.7.789. [DOI] [PubMed] [Google Scholar]
- 17.Cannon CR, Replogle WH, Schenk MP. Endoscopic-assisted adenoidectomy. Otolaryngol Head Neck Surg. 1999;121(6):740–744. doi: 10.1053/hn.1999.v121.a98201. [DOI] [PubMed] [Google Scholar]
- 18.Di Rienzo BL, Angelone A, Mattei A, Ventura L, Lauriello M. Paediatric adenoidectomy: endoscopic coblation. Acta Otorhinolaryngol Ital. 2012;32(2):124–129. [PMC free article] [PubMed] [Google Scholar]


