Abstract
The concentration of total vitamin B12 in serum is not a sufficiently sensitive or specific indicator for the reliable diagnosis of vitamin B12 deficiency. Victor Herbert proposed a model for the staged development of vitamin B12 deficiency, in which holotranscobalamin (HoloTC) is the first indicator of deficiency. Based on this model, a commercial immunoassay has been controversially promoted as a replacement for the total vitamin B12 test. HoloTC is cobalamin (vitamin B12) attached to the transport protein transcobalamin, in the serum, for delivery to cells for metabolism. Although there have been many published reports supporting the claims for HoloTC, the results of some studies were inconsistent with the claim of HoloTC as the most sensitive marker of vitamin B12 deficiency. This review examines the evidence for and against the use of HoloTC, and concludes that the HoloTC immunoassay cannot be used to measure vitamin B12 status any more reliably than total vitamin B12, or to predict the onset of a metabolic deficiency, because it is based on an erroneous hypothesis and a flawed model for the staged development of vitamin B12 deficiency. The author proposes an alternative model for the development of vitamin B12 deficiency.
Electronic supplementary material
The online version of this article (doi:10.1186/s40064-016-2252-z) contains supplementary material, which is available to authorized users.
Keywords: Holotranscobalamin, HoloTC, Active-B12, Vitamin B12, Methylmalonic acid
Background
Herbert’s model
In his Herman Award Lecture of 1986, Victor Herbert proposed his Sequential stages in the development of vitamin B12deficiency (Herbert 1987). Herbert’s hypothesis, describing the Biochemical and hematological sequence of events as negative vitamin B12balance progresses, two decades later formed the basis for the introduction of the commercial holotranscobalamin (HoloTC, Active B12) immunoassay for the diagnosis of vitamin B12 deficiency.
The concentration of total vitamin B12 in serum is not a sufficiently sensitive or specific indicator for the reliable diagnosis of vitamin B12 deficiency (Herbert 1987, 1994; Hølleland et al. 1999; Snow 1999; Oh and Brown 2003; Solomon 2005; Herrmann and Obeid 2008, 2013; Schrempf et al. 2011; Heil et al. 2012). Herbert observed that, as with iron and folate, the range of normal concentrations of serum total vitamin B12 for an individual is narrower than the range of normal for a population (Herbert 1987): “the laboratory test result becomes abnormal for the individual before it exceeds the range of normal for the laboratory”. As observed by Snow “As knowledge has accumulated, the limitations of such tests as serum vitamin levels … have become apparent”.
The two metabolites of vitamin B12, homocysteine (tHcy) and methylmalonic acid (MMA) have been proposed as more sensitive than total serum vitamin B12, for the diagnosis of vitamin B12 deficiency (Hølleland et al. 1999; Snow 1999; Oh and Brown 2003). In support of the use of these metabolites Oh and Brown say that “use of a low serum vitamin B12 level as the sole means of diagnosis may miss up to one half of patients with actual tissue B12 deficiency”. In advocating the use of methylmalonic acid, Hølleland et al. state that “Our data emphasize the poor diagnostic utility of low and low-normal s-cobalamin assay results and call for more sensitive and specific markers of cobalamin deficiency. s-MMA meets these criteria”. Solomon (2005) differed, finding that methylmalonic acid and homocysteine were also unreliable for the diagnosis of vitamin B12 deficiency.
Even now, after decades of research, there is still no agreed gold-standard test for vitamin B12 deficiency. As recently stated by Aparicio-Ugarriza et al. (2014): “There is no consensus in the literature about cut-off points for blood vitamin B12 reference ranges and its associated metabolites.” It is against the background of this unmet need that the holotranscobalamin (HoloTC, Active B12) immunoassay has been offered as a solution.
Holotranscobalamin (HoloTC) is cobalamin (vitamin B12) attached to the transport protein transcobalamin (TC), in the serum, for delivery to cells for metabolism. The absorption and transport of vitamin B12 is described in detail in Neale (1990). Recent developments in understanding the role of HoloTC in the assimilation and metabolism of vitamin B12 are explained in detail by Quadros (2010). Fedosov (2010, 2013) has produced a mathematical model for the biochemical markers of vitamin B12 deficiency, including HoloTC.
Herbert proposed serum holotranscobalamin (HoloTC) as an earlier and more sensitive indicator of vitamin B12 deficiency than total vitamin B12 (Herbert 1987, 1994). According to Herbert (1994): “Low concentrations of holoTCII occur before low concentrations of total serum vitamin B-12 or before deficiency”. This is based on two properties of HoloTC; the small percentage of total vitamin B12 existing as HoloTC, and the short half-life of HoloTC. According to Herbert (1994), HoloTC comprises only 20 % of serum total vitamin B12; this metabolically active portion is carried to all cells on the transport protein transcobalamin (TC). The remaining 80 % (holohaptocorrin, HoloHC) is the metabolically inert component carried on the liver storage protein haptocorrin (HC). According to Herbert (1994), HoloTC has a short half-life of only 6 min compared to 240 h for HoloHC. There is disagreement about the actual half-life of HoloTC, as discussed later in this review, but the consensus is that it is far shorter than that of HoloHC.
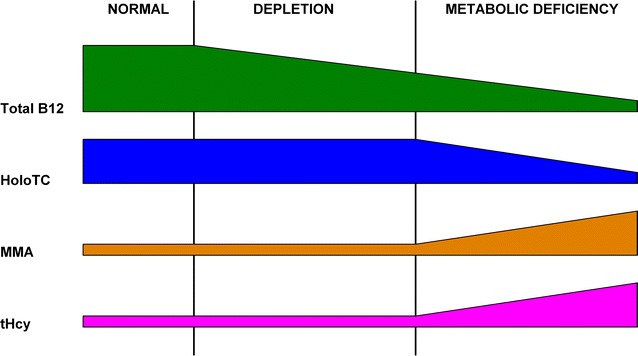
According to Herbert’s 1986 model (Herbert 1987), vitamin B12 deficiency develops in a sequence of four distinct stages, with changes in specific biochemical and haematological markers defining the borders between them (Fig. 1; Table 1). The earliest sign of vitamin B12 deficiency is marked by the change from Normal to Negative B12Balance, with HoloTC concentration falling from >22 to <15 pmol/L, and TC saturation falling from >5 to <5 %. Haematology is normal for the first two stages; initial abnormal haematology, in the form of neutrophil hypersegmentation, appears in stage 3; overtly abnormal haematology in the form of neutrophil hypersegmentation, macroovalocytes, elevated MCV and low haemoglobin, appears in stage 4. MMA is possibly increased in stage three and definitely increased in stage four.
Fig. 1.
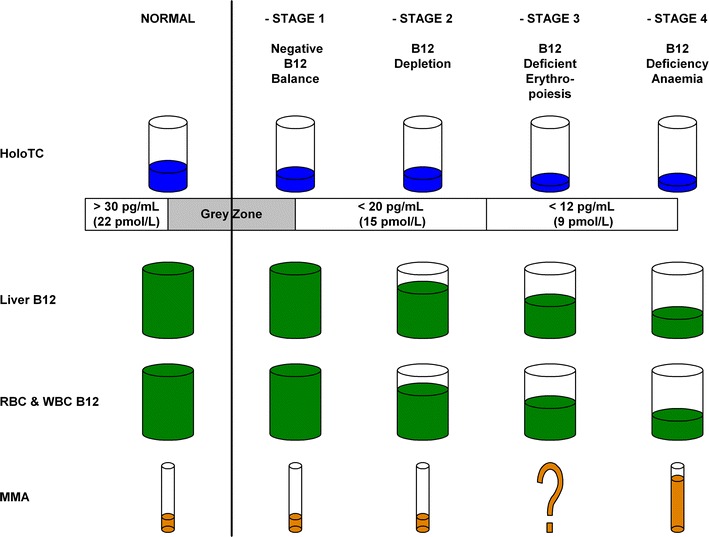
Herbert’s 1986 model for sequential stages in the development of vitamin B12 deficiency. This simplified model was derived from Herbert (1987)
Table 1.
Herbert’s hypothesis—differences between 1986 and 1994 models
| Analyte | Model | Deficiency stage | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| 1986 | Normal | Negative B12 balance | B12 depletion | B12-deficient erythropoiesis | B12-deficiency anaemia | |
| 1994 | Normal | Early negative B12 balance | B12 depletion | Damaged metabolism: B12-deficient erythropoiesis | Clinical damage: B12-deficiency anemia | |
| HoloTC (pmol/L) | 1986 | >22 | <15 | <15 | <9 | <9 |
| HoloTC (pmol/L) | 1994 | >37 | <30 | <30 | <30 | <30 |
| TC saturation (%) | 1986 | >5 | <5 | <2 | <1 | <1 |
| TC saturation (%) | 1994 | >5 | <4 | <4 | <4 | <4 |
| HoloHC (pmol/L) | 1986 | >111 | >111 | <111 | <74 | <74 |
| HoloHC (pmol/L) | 1994 | >133 | >133 | <111 | <74 | <74 |
| MMA high | 1986 | No | No | No | ? | Yes |
| MMA high | 1994 | No | No | No | ? | Yes |
| tHcy high | 1986 | – | – | – | – | – |
| tHcy high | 1994 | No | No | No | Yes | Yes |
From his 1986 model, Herbert concluded that “By measuring holo TC II one can diagnose negative vitamin B-12 balance, a stage which precedes the stage of B-l2 depletion”, and thus proposed HoloTC to be more sensitive than total serum vitamin B12 as an indicator of the onset of vitamin B12 deficiency. Herzlich and Herbert (1988) stated: “The data suggest low holo TC II indicates negative B12 balance early in the development of tissue depletion of B12 … We believe that this parameter provides a new tool for assessing nutritional status in equivocal states”. Wickramasinghe and Fida (1993) supported Herbert’s hypothesis, concluding that “Our data support the model of developing B12 deficiency proposed by Herbert and his colleagues and their view that a proper study of B12 values should include not only measurements of total serum B12 but also of holoTCII concentration”. Neale (1990) more cautiously commented on the hypothesis: “A reduction in the circulating concentration of holo-TCII may be the earliest sign of vitamin B12 deficiency. This potentially important observation awaits confirmation”.
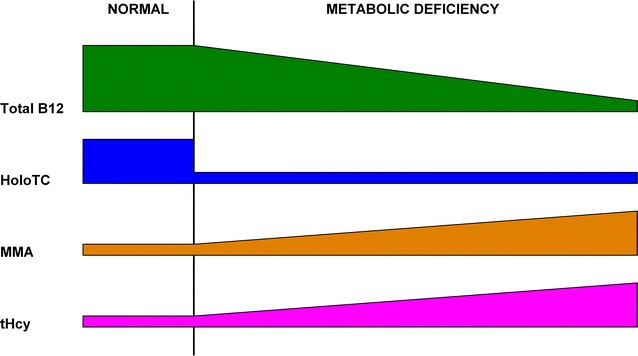
Herbert modified his model in 1990 and again in 1994 (Herbert 1994), adding two Positive Balance stages before the Normal stage, and changing the HoloTC and TC thresholds (Fig. 2; Table 1). Homocysteine, the second metabolite of vitamin B12, is included in this revised model. These changes broaden the range of analytes considered while reducing the relative differences in analyte concentrations, particularly HoloTC concentration and TC saturation, between stages. The range of HoloTC concentration thresholds has been reduced significantly, with the difference between normal and deficient conditions much less clear.
Fig. 2.
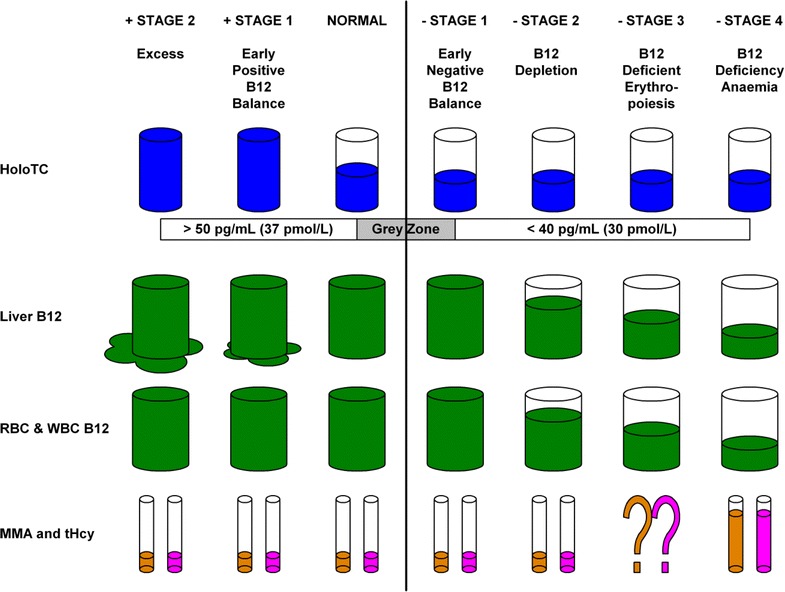
Herbert’s (1994) model for sequential stages in the development of vitamin B12 deficiency. This simplified model was derived from Herbert (1994)
The most important effect of the reduction in the range of HoloTC concentration thresholds is in the diagnosis of the very earliest progression from normality to deficiency; the detection of Negative vitamin B12Balance (Table 1). In Herbert’s original 1986 model, HoloTC concentration needs to fall from >22 to <15 pmol/L, to progress from Normal to Negative Vitamin B12Balance, a fall of 33 %. In the revised model of 1994, HoloTC concentration needs to fall from >37 to <30 pmol/L, to progress from Normal to Early Negative Vitamin B12Balance, a fall of 20 %. Because of the smaller percentage fall in HoloTC required to change from normal to abnormal in the revised model, despite the absolute value of the differences between these stages remaining the same, the diagnosis of Negative Vitamin B12Balance now requires greater precision and accuracy in the individual assay and greater certainty of the HoloTC cut-off levels.
Commercialisation of the HoloTC immunoassay
Commercialisation of the HoloTC test commenced when the company Axis-Shield of Norway, and the University of Aarhus in Denmark, participated in a joint venture: Project E! 2263—HOLOTC “Development Of Diagnostic Test For Holotc”, from April 2000 to February 2005 (Eureka 2000). The stated objective of the project was to develop a new test that is simple and reliable for the diagnosis of vitamin B12 deficiency. Nexo et al. (2002b), from the University of Aarhus, reported a new method for measurement of HoloTC. Ulleland et al. (2002), sponsored by Axis-Shield, reported having developed the first reliable assay for HoloTC.
The HoloTC test as an alternative to the total vitamin B12 assay was further supported, from October 2002 to March 2006, by the European Union demonstration project: QLK3-CT-2002-01775 “Demonstration of the clinical utility of holotc as an early marker of vitamin b12 deficiency” (European Union 2002). The project was coordinated by the University of Aarhus in Denmark; other participants were Axis-Shield and the University of Bergen in Norway, the University of Oxford in the UK and Trinity College Dublin in Ireland. The stated aims of the project were to: “demonstrate the analytical performance of this assay in 4 countries; to show its superiority to conventional methods for assessment of vitamin B12 status; and to demonstrate its value in older patients with depression or dementia”.
As the commercial partner in the development of the HoloTC immunoassay, Axis-Shield has published several documents in support of the HoloTC test as an alternative to the total vitamin B12 assay (Axis-Shield 2007a, b, 2012, 2014a, b). In their presentation of February 2007, Axis-Shield cites Herbert’s model for the sequential development of vitamin B12 deficiency. A modified version of Herbert’s (1994) hypothesis, as a simplified diagram, was provided to support the claim that HoloTC is a more sensitive indicator of vitamin B12 deficiency than is total vitamin B12. The same diagram was used by Ralph Green in his detailed presentation to the Specialty Labs Web Conference of December 2007, when supporting the case for using HoloTC for the diagnosis of vitamin B12 deficiency (Green 2007).
Based on Herbert’s models, in which the HoloTC concentration falls as the vitamin B12 status progresses from Normal to Negative Vitamin B12Balance as the first evidence of deficiency, Axis-Shield (2007a) claims that “Active-B12 levels react early in the process” and “Active-B12 levels are low in patients with biochemical signs of vitamin B12 deficiency”.
Axis-Shield (2007a) cites Herrmann et al. (2003a), saying “Data suggests improved identification of B12 deficient patients with Active-B12 compared to total serum B12”.
Axis-Shield initially marketed their own immunoassay kit for HoloTC, then formed partnerships with manufacturers of automated immunoassay analysers. In 2006 Axis-Shield marketed their RIA (radioimmunoassay) kit for HoloTC (Axis-Shield 2007b), the first commercially available test for holotranscobalamin. In 2007 Abbott Laboratories, in partnership with Axis-Shield, commenced marketing their MEIA (Microparticle Enzyme Immunoassay) for assay of HoloTC on the AxSYM analyser (Abbott Laboratories 2006; Axis-Shield and Abbott Laboratories 2006a, b, 2007a, b; Brady et al. 2007, 2008). Pry (2006), for Abbott Laboratories, presented Holo Transcobalamin; A Predictor of Vitamin B12Status. Brady et al. (2008), employees of Axis-Shield, stated that “The AxSYM Active B12 assay allows rapid, precise, sensitive, specific, and automated measurement of human holoTC in serum and plasma”. In 2011 Abbott Laboratories broadened the application for the HoloTC kit to include their automated Architect high-throughput immunoassay analyser (Abbott Laboratories 2011). IBL International (2013) markets an enzyme-immunoassay (ELISA) kit, and Siemens is currently developing a HoloTC kit for use on their ADVIA Centaur immunoassay system.
Review
Summary of original research and previous reviews
Results from previous original research, for HoloTC sensitivity and specificity compared to total vitamin B12, are summarised in Table 2. Many authors concluded that HoloTC is an earlier and more sensitive indicator of the onset of vitamin B12 deficiency than total vitamin B12 (Table 3, column 1). Other original studies have concluded that there is no significant improvement in sensitivity of HoloTC in comparison to total vitamin B12 (Table 3, column 2). Quotations from original reports are available in tables in Microsoft Excel spreadsheet file, Additional file 3.
Table 2.
Sensitivity and specificity—HoloTC versus B12—original research data
| Reference | Sensitivity | Specificity | Cut-off | AUC |
|---|---|---|---|---|
| Bamonti et al. (2010) | 0.74 | 0.52 | HoloTC < 40 pmol/L | 0.75 |
| Clarke et al. (2007) (definite deficiency) | 0.771 versus 0.757 | 0.761 versus 0.724 | MMA > 0.75 μmol/L | 0.85 versus 0.76 |
| Clarke et al. (2007) (probable deficiency) | 0.647 versus 0.626 | 0.792 versus 0.748 | MMA > 0.45 μmol/L | 0.79 versus 0.87 |
| Goringe et al. (2006) | HoloTC < 38 pmol/L | 0.75 versus 0.72 | ||
| Heil et al. (2012) | 0.83 versus 0.64 | 0.60 versus 0.64 | MMA > 0.45 μmol/L | 0.78 versus 0.70 |
| Herrmann et al. (2003a) | 0.87 versus 0.45 | 0.75 versus 0.98 | MMA > 0.271 μmol/L | 0.879 versus 0.836 |
| Herrmann and Obeid (2013) | 0.72 versus 0.72 | 0.54 versus 0.41 | MMA > 0.300 μmol/L | 0.714 versus 0.632 |
| Hvas and Nexo (2003) | 1.0 | 0.89 | ||
| Hvas and Nexo (2005) | MMA > 0.75 μmol/L | 0.90 versus 0.85 | ||
| Lindemans et al. (2007) | MMA > 0.26 μmol/L | 0.80 versus 0.68 | ||
| Lloyd-Wright et al. (2003) | MMA > 0.75 μmol/L | 0.87 versus 0.86 | ||
| Miller et al. (2006) | holoTC < 35 pmol/L | 0.828 versus 0.816 | ||
| Obeid and Herrmann (2007a) | 0.72 | MMA > 0.300 μmol/L | 0.71 versus 0.60 | |
| Palacios et al. (2013) | 0.44 versus 0.20 | 0.94 versus 0.94 | HoloTC < 35 pmol/L | 0.75 versus 0.69 |
| Schrempf et al. (2011) | 0.563 versus 0.662 | 0.505 versus 0.621 | MMA > 47 μg/L | 0.66 versus 0.72 |
| Scott et al. (2007) | MMA > 0.75 μmol/L | 0.85 versus 0.75, 0.74, 0.72 | ||
| Valente et al. (2011) | 0.55 versus 0.33 | 0.96 versus 0.95 | Red cell cobalamin <33 pmol/L | 0.90 versus 0.80 |
Clarke et al. (2007) compared the HoloTC immunoassay to two assay methods for total vitamin B12: Beckman and Centaur
Scott et al. (2007) compared the HoloTC immunoassay to three assay methods for total vitamin B12: Beckman, Centaur and micro assays
AUC, area under ROC curve for HoloTC or total vitamin B12; ROC curve, Receiver Operating Characteristic = sensitivity versus (1 − specificity) = true positive versus false positive (Miller et al. 2006); Cut-off, analyte and cut-off value used to define vitamin B12 deficiency
Table 3.
Sensitivity and specificity—HoloTC versus B12—original research conclusions
| Positive conclusions | Negative or neutral conclusions |
|---|---|
| Augoustides-Savvopoulou et al. (2007) | Al Aisari et al. (2010) |
| Bhat et al. (2009) | Chen et al. (2005) |
| Black et al. (2006) | Clarke et al. (2007) |
| Bor et al. (2004) | Goringe et al. (2006) |
| Čabarkapa et al. (2007) | Loikas et al. (2003) |
| Fragasso et al. (2012) | Loikas (2007) |
| Heil et al. (2012) | Miller et al. (2006) |
| Herrmann et al. (2003a) | Nilsson et al. (2004) |
| Herrmann et al. (2005) | Palacios et al. (2013) |
| Herrmann and Obeid (2013) | Remacha et al. (2014) |
| Hvas and Nexo (2003) | Schrempf et al. (2011) |
| Hvas and Nexo (2005) | Sobczyńska-Malefora et al. (2014) |
| Lee et al. (2009) | van Asselt et al. (2003) |
| Lindemans et al. (2007) | |
| Lindgren et al. (1999) | |
| Lloyd-Wright et al. (2003) | |
| Lobreglio et al. (2008) | |
| Morkbak et al. (2007) | |
| Nexo et al. (2002a) | |
| Obeid and Herrmann (2007a) | |
| Scott et al. (2007) | |
| Serefhanoglu et al. (2008) | |
| Sikaris (2010) | |
| Valente et al. (2011) | |
| Vanpoucke et al. (2007) | |
| Woo et al. (2010) |
Positive, neutral or negative conclusions are as understood by this author to be the intention of authors of cited article
Quotations from original reports are available in tables in Microsoft Excel spreadsheet file, Additional file 3
In March 2012, a group of nine internationally recognised experts issued an Expert’s Consensus Statement in support of the use of the HoloTC test: “Emerging evidence indicates that holotranscobalamin (Active-B12) is a more reliable marker of a patient’s B12 status than is serum vitamin B12” (Herrmann et al. 2012) (Table 4). However, there is not consensus between all experts, as demonstrated by a report on the NHANES (National Health and Nutrition Survey) roundtable on biomarkers of vitamin B12 status (Yetley et al. 2011). The report recommended total vitamin B12 as the marker for circulating vitamin B12 because of the need for additional performance studies of the HoloTC test.
Table 4.
Signatories to “Expert’s Consensus Statement”
| Signatory | Institution |
|---|---|
| Wolfgang Herrmann | Saarland University |
| Rima Obeid | Saarland University |
| Ralph Green | University of California |
| Donald Jacobsen | Cleveland Clinic |
| Dominic Harrington | St. Thomas’ Hospital |
| Per Magne Ueland | University of Bergen |
| Jan Lindemans | Erasmus Medical Center |
| Ebba Nexø | Aarhus University Hospital |
| Anne Molloy | Trinity College Dublin |
From Herrmann et al. (2012)
Consensus Statement: “Emerging evidence indicates that holotranscobalamin (Active-B12) is a more reliable marker of a patient’s B12 status than is serum vitamin B12”
Reviews, presentations, commentary and letters, on the use of HoloTC as an earlier and more sensitive indicator of vitamin B12 deficiency than total vitamin B12, have been mixed. Several authors supported the claim that HoloTC was superior (Green 2011; Greibe et al. 2012; Nexo and Hoffmann-Lücke 2011). Others raised concerns about the clinical utility of the test (Carmel 2002, 2011, 2012; Devalia 2006; Devalia et al. 2014; Hvas and Nexo 2006; Oberley and Yang (2013). Herrmann et al. (2003b) and Herrmann and Obeid (2007, 2008) recommended the combined use of methylmalonic acid (MMA) and HoloTC. Questioning the superiority of the HoloTC test, Carmel (2002) stated that “what low holo-TC concentrations really tell us remains elusive.”
HoloTC problems
There are four problematic aspects of HoloTC, where there are major differences between authors: the value of the half-life of HoloTC; the correlation between HoloTC and total vitamin B12; sensitivity of HoloTC to recent absorption of vitamin B12; the value of HoloTC cut-off to detect negative vitamin B12 balance. The latter two differences are the most important because they raise the questions of what it is that HoloTC concentration actually indicates, and whether or not it is possible to use it to reliably detect the early onset of vitamin B12 deficiency.
Half-life
Although the proponents of HoloTC, as an early indicator of vitamin B12 deficiency, cite the shorter half-life of HoloTC compared to HoloHC as a factor, there is no general agreement on the absolute value (Table 5). In supporting their case for HoloTC, Axis-Shield (2007b) states: “The markedly shorter half-life for HoloTC of 1–2 hours versus 9 days for HoloHC makes a decrease of HoloTC one of the earliest markers of cobalamin deficiency”; Herbert (1994) gives values of 6 min for HoloTC and 240 h for HoloHC. Whether the half-life of HoloTC is minutes or hours is not significant compared to the generally agreed 240 h for HoloHC. Therefore, although the differences between authors are considerable and should be resolved, they do not invalidate the case for using HoloTC.
Table 5.
Half-life of HoloTC
| Reference | Half-life HoloTC |
|---|---|
| Axis-Shield (2007b) | 1–2 h |
| Bor et al. (2004) | 1–12 h |
| Carmel and Agrawal (2012) | Minutes |
| Chatthanawaree (2011) | 1 h |
| Chen et al. (2005) | Few hours |
| Green (2007) | 6 min |
| Herbert (1994) | 6 min |
| Herrmann et al. (2003a) | 6 min |
| Hvas et al. (2005) | 1–2 h |
| Lindgren et al. (1999) | 1–2 h |
| Loikas et al. (2003) | 60 min |
| Quadros (2010) | 1–2 h |
| von Castel-Roberts et al. (2007) | 18 h |
Correlation with total vitamin B12
The correlation between HoloTC and total vitamin B12 concentrations, in reports of original research, varies widely between authors (Table 6). Bamonti et al. (2010) reported a weak correlation (r = 0.42) whereas Augoustides-Savvopoulou et al. (2007) reported a very strong correlation (r = 0.882). Although most researchers reported a single value for r, there were notable exceptions. Herrmann and Obeid (2013) reported separate values of r for low or high values of total vitamin B12 (r = 0.524 for low B12; r = 0.403 for high B12). Refsum et al. (2006) reported separate values for male and female subjects (r = 0.65 for male; r = 0.61 for female). The differences between findings, for correlation coefficient, are important because they reflect different sensitivity and/or specificity relationships between HoloTC and total vitamin B12. A very high correlation, over a wide range of values, would imply that HoloTC could not detect the onset of vitamin B12 deficiency any earlier than total vitamin B12. However, a very low correlation would not necessarily mean that HoloTC is a more sensitive marker of the transition from normal to negative vitamin B12 balance.
Table 6.
Correlation between total vitamin B12 and HoloTC
| Reference | HoloTC versus B12 correlation coefficient (r) |
|---|---|
| Al Aisari et al. (2010) | 0.765 |
| Augoustides-Savvopoulou et al. (2007) | 0.882 |
| Bamonti et al. (2010) | 0.42 |
| Čabarkapa et al. (2007) | 0.53 |
| Chen et al. (2005) | 0.45 |
| Clarke et al. (2007) | 0.61 |
| Fragasso et al. (2012) | 0.64 |
| Goringe et al. (2006) | 0.63 (r2 = 0.397) |
| Herrmann et al. (2003a) | 0.75 |
| Herrmann and Obeid (2013) | 0.577 (whole), 0.524 (low B12), 0.403 (high B12) |
| Hvas and Nexo (2005) | 0.71 |
| Lee et al. (2009) | 0.6591 |
| Lloyd-Wright et al. (2003) | 0.75 |
| Lobreglio et al. (2008) | 0.495 |
| Loikas et al. (2003) | 0.80 |
| Loikas (2007) | 0.78 |
| Nexo et al. (2002b) | 0.45 |
| Palacios et al. (2013) | 0.65 |
| Refsum et al. (2006) | 0.65 (male), 0.61 (female) |
| Schrempf et al. (2011) | 0.577–0.637 |
| Scott et al. (2007) | 0.5 |
| Vanpoucke et al. (2007) | 0.53 (r2 = 0.28) |
Sensitivity to recent absorption
The reported sensitivity of the HoloTC concentration to recent absorption of vitamin B12 varies between authors (Table 7), leading to the important question about whether HoloTC concentration indicates long-term status or recent absorption of vitamin B12 or both. Axis-Shield and Abbott Laboratories (Axis-Shield and Abbott Laboratories 2006a, 2007a; Axis-Shield 2007a) cite Chen et al. (2005), stating that HoloTC reflects vitamin B12 status “independent of recent absorption of the vitamin”. Chen et al. (2005) actually concluded that “Metabolic cobalamin status is a major determinant of serum holo-TC II. Absorption status may have mild influence as well”. Axis-Shield (2012) cite Nexo: “newly absorbed vitamin B12 occurs as holoTC, and therefore an increase in holoTC upon oral loading with vitamin B12 can be used to judge the capacity for uptake of the vitamin”. Several authors found the issue to be problematic (Bamonti et al. 2010; Loikas 2007; Carmel 2002, 2012). Bamonti et al. (2010) cited the conflicting findings of Chen et al. (2005) and Bor et al. (2004). Loikas (2007) commented on the apparently contradictory promotion of HoloTC as “the most sensitive and specific indicator of early vitamin B12 deficiency” and the proposed use of HoloTC as “a marker of vitamin B12 absorption”, concluding that “Reconciling these two phenomena is problematic because, although frequently coexisting, they are not identical”. In his editorial, Carmel (2002) observed that “The favoured hypotheses have been that low holo-TC is either an early sign of general cobalamin insufficiency or specific evidence of decreased absorption of cobalamin. The distinction between these two very separate explanations has blurred, particularly as advocacy became more enthusiastic, but it is not an idle distinction. This central issue and many other questions need resolution”.
Table 7.
Sensitivity to recent absorption
| Reference | Dependence on recent absorption |
|---|---|
| Axis-Shield and Abbott Laboratories (2006a) | Independent |
| Axis-Shield and Abbott Laboratories (2007a) | Independent |
| Axis-Shield (2007a) | Independent |
| Axis-Shield (2012) | Dependent |
| Bamonti et al. (2010) | Problematic |
| Bhat et al. (2009) | Dependent |
| Bor et al. (2004) | Dependent |
| Bor et al. (2005) | Dependent |
| Carmel (2002) | Problematic |
| Carmel (2012) | Problematic |
| Chen et al. (2005) | Both? |
| Green (2011) | Both |
| Hvas et al. (2005) | Independent |
| Hvas et al. (2007) | Dependent |
| IBL International (2013) | Independent |
| Lindgren et al. (1999) | Dependent |
| Loikas (2007) | Problematic |
| Morkbak et al. (2005) | Dependent |
| Nexo et al. (2002a) | Dependent |
| Nexo and Hoffmann-Lücke (2011) | Both |
| Robinson et al. (2011) | Both |
| von Castel-Roberts et al. (2007) | Dependent |
Quotations from original reports are available in tables in Microsoft Excel spreadsheet file, Additional file 3
No agreed cut-off
Another important problem is that there is no agreement on a single value for the cut-off level for the minimum concentration of HoloTC, as required to distinguish between normal vitamin B12 status and the first stage of deficiency (Table 8). Morkbak et al. (2005) quoted a range of 11–41 pmol/L for eight European studies, stating: “There is no consensus concerning the choice of reference intervals for holoTC”. According to Heil et al. (2012): “large discrepancies exist with regard to the choice of cut-off value for HoloTC (range 20–45 pmol/L), which makes data interpretation difficult”. In their review, Aparicio-Ugarriza et al. (2014) found that, in 69 studies between 1992 and 2014, researchers quoted HoloTC concentration cut-offs from 20 to 50 pmol/L.
Table 8.
HoloTC reference intervals and cut-offs
| Reference | Reference interval (pmol/L) | Cut-off (pmol/L) |
|---|---|---|
| Abbott Laboratories (2006) | 37 | |
| Abbott Laboratories (2011) | 35 | |
| Al Aisari et al. (2010) | 9–123 | |
| Aparicio-Ugarriza et al. (2014) | 20–50 (literature review) | |
| Augoustides-Savvopoulou et al. (2007) | 35 | |
| Axis-Shield and Abbott Laboratories (2006a) | 35 | |
| Axis-Shield (2007a) | 35 | |
| Axis-Shield (2007b) | 37 | |
| Bamonti et al. (2010) | 40 | |
| Black et al. (2006) | 23–100 | |
| Brady et al. (2007) | 35 | |
| Chen et al. (2005) | 46–356 | 30 |
| Clarke et al. (2007) | 45 | |
| Fragasso et al. (2012) | 35 | |
| Goringe et al. (2006) | 16 (diagnostic), 38 (laboratory) | |
| Green (2007, 2011) | 35 | |
| Heil et al. (2012) | 32 | |
| Herbert (1987) | 22 | |
| Herbert (1994) | 37 | |
| Herrmann et al. (2003a, b, 2005) | 35 | |
| Herrmann and Obeid (2007) | 40–70 “Grey zone” | |
| Herrmann and Obeid (2008) | 35 | |
| Herrmann and Obeid (2013) | 22–76 “Grey zone” | |
| Herrmann et al. (2003a) | 35 | |
| Herrmann et al. (2005) | 35 | |
| Hooshmand et al. (2012) | 35 | |
| Hvas and Nexo (2003) | 50 | |
| Hvas and Nexo (2005) | 40 | |
| Lee et al. (2009) | 42.48 | |
| Lindemans et al. (2007) | 20–122 | |
| Lindgren et al. (1999) | 35–160 | |
| Lloyd-Wright et al. (2003) | <25 likely, >50 unlikely B12 deficiency | |
| Lobreglio et al. (2008) | 35 | |
| Loikas et al. (2003, 2007a, b) | 37 | |
| Loikas (2007) | 37–171 | |
| Miller et al. (2006) | 35 | |
| Morkbak et al. (2005) | 40, 11–41 (literature review) | 37 |
| Morkbak et al. (2007) | 40–150 | |
| Nexo et al. (2002a) | 40–150 | |
| Nexo et al. (2002b) | 40–150 | |
| Nexo and Hoffmann-Lücke (2011) | 40–200 | |
| Obeid and Herrmann (2007a, 2007b) | 35 | |
| Palacios et al. (2013) | 35 | |
| Pry (2006) | 37 | |
| Refsum et al. (2006) | 42–157 | |
| Remacha et al. (2014) | 33.5 | |
| Schrempf et al. (2011) | 42 | |
| Serefhanoglu et al. (2008) | 37 | |
| Sobczyńska-Malefora et al. (2014) | 25–50 “poor predictor MMA” | |
| Valente et al. (2011) | 20–30 “indeterminate zone” | 20 |
| van Asselt et al. (2003) | 38–113 | |
| Vanpoucke et al. (2007) | 37 | |
| Woo et al. (2010) | 35 |
Furthermore, several researchers quote a grey zone, or indeterminate range of cut-off values for HoloTC concentration (Table 8). Herrmann and Obeid (2007) quote a grey zone for HoloTC cut-offs, of 40–70 pmol/L; they later changed this to 23–75 pmol/L (Herrmann and Obeid 2013). Lloyd-Wright et al. (2003) say that deficiency is likely for a HoloTC concentration <25 pmol/L, and unlikely for >50 pmol/L, leaving an indeterminate range of 25–50 pmol/L. Sobczyńska-Malefora et al. (2014) found that HoloTC concentrations in the range of 25–50 pmol/L could not be used to predict the vitamin B12 status as defined by MMA concentration. Valente et al. (2011) reported an indeterminate zone of 20–30 pmol/L for HoloTC concentrations. In their BJH guideline, Devalia et al. (2014) recommended that “Serum holotranscobalamin has the potential as a first-line test, but an indeterminate ‘grey area’ may still exist”.
The HoloTC test appears to suffer from a similar limitation to that found for total vitamin B12; the range of normal values for an individual is much narrower than the range of normal for a population (Herbert 1987). According to McCaddon et al. (2003), referring to the HoloTC test: “the dispersion of values for any individual will span only a small part of any reference interval”.
The absence of an agreement on a single cut-off value for HoloTC, for diagnosis of vitamin B12 deficiency, is inconsistent with a widely stated reason for supporting the use of this test in place of total vitamin B12: that there is a wide indeterminate range for total vitamin B12. In promoting their HoloTC assay, Axis-Shield (2007a) state this inadequacy of the total vitamin B12 test: “There is a grey zone between approximately 151–300 pmol/L B12 where there is likely to be misclassification of B12 status if relying on total serum B12 alone.” If there is no universally agreed single cut-off value for a minimum HoloTC concentration, this test appears to have the same flaw as total vitamin B12. Is it possible to reliably detect the early onset of vitamin B12 deficiency, i.e. the transition between Herbert’s sequential stages from Normal to Early Negative B12Balance, if there is no agreed single cut-off value for HoloTC?
Potential for data manipulation to promote HoloTC
Area Under Curve (AUC)
Where the Area Under Curve (AUC) is reported for Receiver Operating Characteristic (ROC) curves, the selection of the reference analyte and value of the reference cut-off determines the relative areas under the curve (Table 2). For example, Heil et al. (2012) produced three ROC curves where different cut-off levels of MMA were used to define vitamin B12 deficiency, demonstrating how the choice of reference cut-off level determines the difference in AUC for HoloTC compared to total vitamin B12. With the lowest MMA cut-off, of >0.32 µmol/L, the AUC was 0.70 for HoloTC, compared to 0.63 for total vitamin B12. At their preferred MMA cut-off, of >0.45 µmol/L, the AUC was 0.78 for HoloTC, compared to 0.70 for total vitamin B12. When the MMA cut-off was increased to >0.77 µmol/L, the AUC was 0.92 for HoloTC, compared to 0.73 for total vitamin B12.
By increasing the MMA cut-off, the difference in AUC between HoloTC and total vitamin B12 is increased (Heil et al. 2012, Figure 1), improving the apparent performance of HoloTC, but many more vitamin B12 deficient patients will be misdiagnosed as normal. The next stage of the process, selection of the total vitamin B12 and HoloTC cut-offs, is a trade-off between sensitivity and specificity (Heil et al. 2012, Figure 4).
The trade-off between sensitivity and specificity
As noted by this author (Golding 2016), it is possible to alter the apparent relative sensitivity of any pair of analytes by selectively changing the cut-off value of one or both of them. As demonstrated in that experiment, selecting different cut-off values for total vitamin B12 changed the relative sensitivities of HoloTC and total vitamin B12; the same applies to the cut-off value for HoloTC. When the HoloTC cut-off is increased, the sensitivity to vitamin B12 deficiency is increased, but the specificity of the test is reduced, increasing the number of false positive results. Conversely, if the HoloTC cut-off is decreased, the specificity of the test is increased, but the sensitivity of the test is reduced, increasing the number of false negative results.
From their ROC charts, Heil et al. (2012, Figure 3) selected MMA > 0.45 µmol/L to define vitamin B12 deficiency. With a HoloTC cut-off value of <21 pmol/L, the specificity was impressively high at 88 % but the sensitivity was only 64 % (Heil et al. 2012, Figure 4b). By selecting the best trade-off between sensitivity and specificity for HoloTC, with a HoloTC cut-off value of <32 pmol/L, they obtained an impressive HoloTC sensitivity of 83 % but a specificity of only 60 %. To overcome this problem, as did Herrmann and Obeid (2007, 2008), the authors suggest using MMA as a secondary test to confirm vitamin B12 deficiency in cases where HoloTC is <32 pmol/L. This approach would have failed to detect any vitamin B12 deficiency in the subject of this author’s experiment (Golding 2016) because, despite overt metabolic disturbance evident from raised MMA concentration, and the onset of severe symptoms including peripheral neuropathy, HoloTC concentration never fell below 33 pmol/L.
Contrary findings
The results of several studies did not support the claims that HoloTC is a significantly earlier marker of vitamin B12 deficiency than total B12 (Clarke et al. 2007; Palacios et al. 2013; Schrempf et al. 2011; Miller et al. 2006; Remacha et al. 2014). This author, in his single-subject self-experiment, reported no significant difference in response between HoloTC and total vitamin B12 (Golding 2016).
Contrary to Heil et al., Schrempf et al. (2011) reported a lower AUC for HoloTC than for total vitamin B12; 0.563 versus 0.662 (Table 2). Their study was conducted on neuropsychiatric patients with vitamin B12 deficiency defined by MMA > 47 µg/L (40 µmol/L). The authors presented the ROC curves for three patient groups: all patients; those with classic vitamin B12 deficiency (subacute combined degeneration and/or peripheral neuropathy); those with peripheral neuropathy only. In each grouping, the AUC for total vitamin B12 was greater than for HoloTC (Schrempf et al. 2011, Figure 1).
Based on their ROC results, in which the AUCs for HoloTC and total vitamin B12 were 0.828 and 0.816 respectively, Miller et al. (2006) concluded that “HoloTC and total vitamin B12 have equal diagnostic accuracy in screening for metabolic vitamin B12 deficiency”. They also reported correlations between their results, for HoloTC and total vitamin B12, which were not consistent with Herbert’s model. For example, some patients with normal HoloTC (>35 pmol/L) were low in total vitamin B12 (<148 pmol/L).
As observed by Herrmann and Obeid (2013), in reporting results of their investigation of the biological markers of vitamin B12 deficiency, “The shape of the ROC curve illustrates that the holoTC test is not sufficient to separate between deficient and non-deficient individuals with high reliability”.
Remacha et al. (2014) investigated 106 patients with total vitamin B12 concentration ≤200 pmol/L, defining low HoloTC as a concentration <33.5 pmol/L and high MMA as a concentration >0.40 µmol/L. Of the 31 patients with normal HoloTC concentrations, 13 had high levels of MMA; of the 75 patients with low HoloTC concentrations, 27 had normal MMA. Remacha et al. reported that “HoloTC was not decreased in one-third of patients with low Cbl, but MMA/Hcy levels were elevated in half of them, reflecting Cbl deficiency.”
The problems with Herbert’s model
The absence of an agreed single value for the HoloTC cut-off, together with uncertainty about whether HoloTC represents recent absorption of vitamin B12 or long-term status or both, must raise questions about Herbert’s hypothesis. Some of the most recent original research challenges Herbert’s model for the “Sequential stages in the development of vitamin B12 deficiency”. In reporting their original research results, Remacha et al. (2014) commented that “These data do not support holoTC as the earliest marker of Cbl deficiency and challenge the classification in stages of Cbl deficiency”.
In Herbert’s revised 1994 model (Herbert 1994), the change from Normal to Early Negative Vitamin B12Balance is marked by a fall in HoloTC concentration from >37 to <30 pmol/L. Even if it is assumed that such a highly precise and accurate routine clinical assay is possible, there remain two major unresolved fundamental problems with Herbert’s hypothesis.
Firstly, as raised by several authors, there is uncertainty about what HoloTC actually represents (Table 7). Does HoloTC concentration indicate recent absorption of vitamin B12, long-term body store or both? As stated by Chen et al. (2005): “The concept that a test can be used to diagnose both deficiency and malabsorption is problematic because the 2 defects are not identical. If holo-TC II truly reflects both processes, holo-TC II changes would perforce lose all diagnostic specificity for either process”. For the HoloTC immunoassay to have any clinical value in detecting the earliest onset of vitamin B12 deficiency, as Herbert intended, it would need to be either sensitive only to long-term status or be performed after a well-defined period of fasting.
Secondly, the model demands the reliable detection of a change in HoloTC concentration far smaller than the reported range of cut-off values (Table 8). As noted by Sobczyńska-Malefora et al. (2014), “there has been little consensus with regard to the assigned cut-off to discriminate between replete and deficient states”. Herbert’s required change in HoloTC concentration from >37 to <30 pmol/L, to detect the earliest onset of vitamin B12 deficiency, is inconsistent with the reported range of cut-off values from 20 to 50 pmol/L. Furthermore, the use of various grey zones, for HoloTC concentration (Table 8), is inconsistent with Herbert’s hypothesis in which Early Negative Vitamin B12Balance is detected by a universally agreed, and closely specified, fall in HoloTC concentration.
Why Herbert’s model is flawed
Herbert’s model for the staged development of vitamin B12 deficiency is based on his erroneous hypothesis that HoloTC will always be the first analyte to respond to a deficiency, and that a minimum normal concentration of HoloTC may be universally defined. How Herbert developed his hypothesis, and why it is flawed, is best explained by examining the process of gastrointestinal absorption and transport of vitamin B12 in humans.
Normal gastrointestinal absorption of vitamin B12
Figure 3 is a simplified diagram containing the main elements of the process of gastrointestinal absorption and transport of vitamin B12 in humans. In a healthy person, stomach acid separates food vitamin B12 from protein; haptocorrin (HC) from saliva then binds with the free vitamin B12 to form the holohaptocorrin (HoloHC) (Loikas 2007, Figure 2.4). The increased pH in the duodenum causes the vitamin B12 to be released from the HC; intrinsic factor (IF), produced by parietal cells in the stomach, combines with the vitamin B12 in the duodenum to produce IF-B12 (Loikas 2007, Figure 2.4). The IF is then degraded in the terminal ileum, producing free vitamin B12 (Seetharam and Yammani 2003, Figure 1; Andrès et al. 2004, Figure 1; Loikas 2007, Figure 2.4).
Fig. 3.
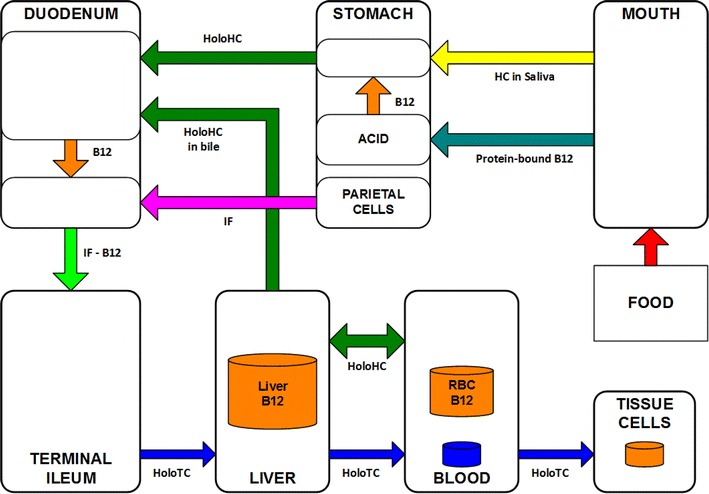
Vitamin B12 gastrointestinal absorption. Derived from Seetharam and Yammani (2003, Figure 1), Andrès et al. (2004, Figure 1) and Loikas (2007, Figure 2.4)
There is no consensus on the exact location of the production of HoloTC and HoloHC.
According to Seetharam and Yammani (2003, Figure 1), and Andrès et al. (2004, Figure 1), the free B12 is bound to TC in the ileum to form HoloTC; they show HoloHC in the portal vein but do not say how or where it is formed. Quadros (2010) states that “The IF-Cbl absorbed in the distal ileum appears in the circulation bound to TC”, implying that all of the free B12 is bound to TC to form HoloTC; it is unclear from this whether the free B12 binds to the TC in the ileum or in the circulation. According to Furger (2012) “In the blood plasma Cbl is bound either to HC or TC, where only TC is responsible for the Cbl uptake into cells”; again, it is unclear where the binding takes place. If all of the free vitamin B12 in the ileum is bound to TC, regardless of whether the binding takes place in the ileum or in the circulation, then the HoloHC in the circulation must ultimately be produced from vitamin B12 freed from the HoloTC.
The HoloTC enters the general circulation from where it is delivered to cells for metabolism (Seetharam and Yammani 2003, Figure 1; Andrès et al. 2004, Figure 1; Loikas 2007, Figure 2.4; Quadros 2010; Furger 2012).
The HoloHC is passed, via the portal vein, to the liver where the vitamin B12 is separated from the HC and stored in the liver (Seetharam and Yammani 2003, Figure 1). When HoloTC is required for metabolism, some of the vitamin B12 stored in the liver is bound to HC and recycled via the bile (Seetharam and Yammani 2003, Figure 1; Loikas 2007, Figure 2.4).
Normal enterohepatic recycling of vitamin B12
Of crucial importance to this entire gastrointestinal absorption process is the enterohepatic recycling of the vitamin B12, shown in Fig. 3 as the transfer of HoloHC from the liver to the duodenum, in the bile. This recycling is not only essential for the efficient maintenance of the body store of vitamin B12; it is the means by which the serum concentration of HoloTC is regulated. The rate of transfer to the duodenum of HoloHC in bile, and the IF from the parietal cells, controls the rate of HoloTC production.
This enterohepatic recycling process is shown, as a feedback control system, in Fig. 4. Here, the Input to the system is the intrinsic factor; the system Output is the HoloTC. The Process is the production of IF-B12 from the IF and vitamin B12 in the duodenum, and the binding of the B12 freed from IF in the terminal ileum with transcobalamin (TC) to produce holotranscobalamin (HoloTC). For the purposes of this discussion, the liver vitamin B12 store is not part of the input but considered to be a constant in the short-term. The Feedback signals control the rate of the process; details of the nature of these signals are beyond the scope of this review.
Fig. 4.
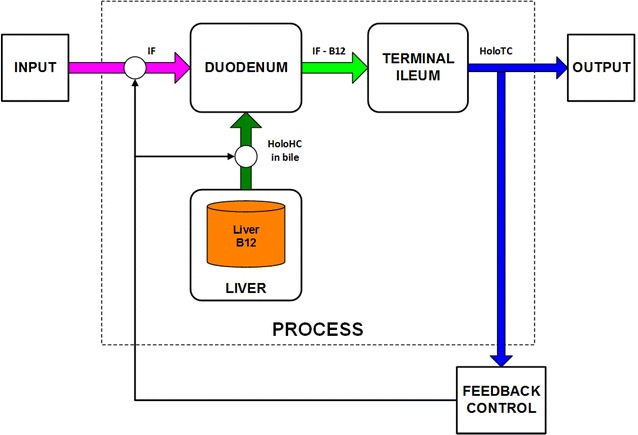
HoloTC feedback control. Derived from Seetharam and Yammani (2003, Figure 1), Andrès et al. (2004, Figure 1) and Loikas (2007, Figure 2.4)
Failure of enterohepatic recycling and HoloTC production
If any one of the elements of this feedback control system suddenly fails entirely, the enterohepatic recycling will stop immediately, and no HoloTC will be produced; for example, if the supply of intrinsic factor or production of bile suddenly stops or if the terminal ileum or duodenum are removed. Under these circumstances, Herbert’s hypothesis would be expected to hold true in one respect; the fall in HoloTC would be an early indicator of a vitamin B12 deficiency. The HoloHC has a far longer half-life than the HoloTC in serum, and there is a large store of vitamin B12 in the liver and red-cells, so HoloHC would fall much more slowly than HoloTC.
It is important to note that only a disturbance of the IF input, or of elements within this HoloTC feedback system, will affect its short-term performance. Assuming that the liver vitamin B12 store is full, any failure ahead the input of IF, or after the output of HoloTC will have no short-term effect on the production of HoloTC. This means that HoloTC will not be an early responder for all causes of vitamin B12 deficiency; if the enterohepatic cycle is not disrupted, HoloTC would remain normal until the liver store of HoloHC is exhausted.
HoloTC response depends on cause of vitamin B12 deficiency
The following discussion is based on this author’s interpretation of available information about the operation of the vitamin B12 enterohepatic cycle, and the response of total vitamin B12, HoloTC, tHcy and MMA for different causes of vitamin B12 deficiency. Human experimentation is needed to investigate the actual responses of the analytes under these various conditions.
According to Herbert (1987, 1994), there are six possible causes of vitamin B12 deficiency; three inadequacies and three excesses. These conditions, and their effect on the HoloTC feedback system, are listed in Table 9. A seventh very common cause of vitamin B12 deficiency, food-cobalamin malabsorption, was reported by Carmel (1995) and reviewed by Andrès et al. (2004); this is shown in Table 9 as a fourth inadequacy.
Table 9.
Causes of vitamin B12 deficiency, and short-term effect on HoloTC production
| Cause of vitamin B12 deficiency | Classification | Short-term effect on HoloTC production? |
|---|---|---|
| Inadequate dietary intake | Inadequacy | No |
| Defective gastrointestinal absorption (other than food-cobalamin absorption) | Inadequacy | Yes? |
| Defective gastrointestinal absorption (food-cobalamin malabsorption) | Inadequacy | No |
| Inadequate cellular utilization (deficiency of a cobalamin coenzyme) | Inadequacy | No |
| Increased requirement (pregnancy or hyperthyroidism) | Excess | No |
| Increased excretion (alcoholism) | Excess | No |
| Increased destruction (nutrient or drug interactions) | Excess | No, unless intrinsic factor destroyed |
A suddenly inadequate dietary intake, for example commencing a vegan diet, will not affect the enterohepatic cycle because it does not affect the input of intrinsic factor into the cycle until the store of HoloHC is exhausted i.e. it occurs ahead of the cycle. Similarly, the onset of inadequate utilization in the cells also will not affect the production of HoloTC i.e. it occurs after the cycle. In either case, Herbert’s model will not apply because total vitamin B12 will fall before HoloTC responds, and MMA and tHcy will commence to increase immediately after HoloTC falls below normal for the individual.
An increased requirement, increased excretion or increased destruction, would tend to cause an increase in the rate of enterohepatic recycling to maintain the serum concentration of HoloTC; if all else is equal, the cycle will continue to produce HoloTC until the supply of stored HoloHC is consumed. Again, Herbert’s model will not hold true because total vitamin B12 will fall before HoloTC responds, and MMA and tHcy will commence to increase immediately after HoloTC falls below normal for the individual.
One inadequacy, gastrointestinal malabsorption, affecting the supply of intrinsic factor, production of bile or absorption of the IF-B12, has the potential to halt HoloTC production. HoloTC is likely to be a fast responder to a rapid failure such as the removal of the relevant part of the stomach, containing the parietal cells, or the removal of the duodenum or terminal ileum. In this case, however, MMA and tHcy would be expected to almost immediately increase above normal for the individual, so there would be no period when HoloTC is depleted without any metabolic disturbance, and Herbert’s model would not hold true.
If there is a gradual failure of supply of intrinsic factor to the input, in the case of Pernicious Anaemia where the autoimmune disease causes antibodies to attack the parietal cells or intrinsic factor or other slowly developing problem with gastrointestinal vitamin B12 absorption, the metabolic disturbance would again commence immediately but MMA and tHcy would increase more slowly. Again, because there would be no period when HoloTC is depleted without any metabolic disturbance, Herbert’s model would not apply.
The very common case of food-cobalamin malabsorption, where gastric atrophy occurs during ageing, was first identified after Herbert proposed his model (Carmel 1995; Andrès et al. 2004). This case would be similar to that of inadequate dietary intake, where the enterohepatic cycle is not disturbed because there is no effect on the input of intrinsic factor into the cycle until the liver store of HoloHC is exhausted. Because the deficiency occurs ahead of the cycle, there would be no period when HoloTC is depleted without any metabolic disturbance, so Herbert’s model would not hold true. If the slow onset of vitamin B12 deficiency in this case does cause HoloTC to fall significantly, and remain depleted before other analytes react, the published experimental results should demonstrate this. According to Andrès et al. (2004), >60 % of cases of vitamin B12 deficiency in the elderly are caused by food-cobalamin malabsorption. The studies reported by Miller et al. (2006), Clarke et al. (2007), Schrempf et al. (2011), Palacios et al. (2013) and Remacha et al. (2014) all involved aged patients, so the majority were therefore likely to have their vitamin B12 deficiency caused by food-cobalamin malabsorption. If Herbert’s model applied to those patients, HoloTC should have been reported as significantly more sensitive than total vitamin B12, but this was not the case in those studies.
An alternative hypothesis
Introduction
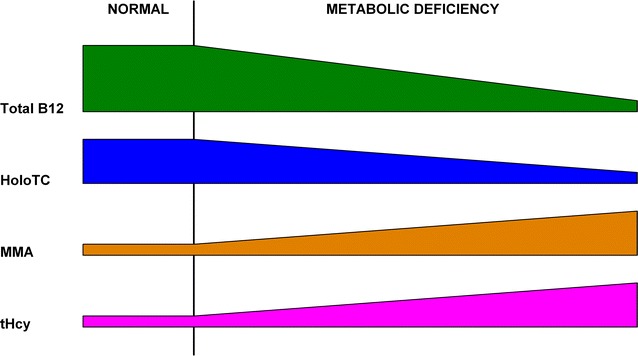
This author proposes an alternative model (Fig. 5) in which the earliest onset of vitamin B12 deficiency, or the transition from Normal to Early Negative Vitamin B12Balance, is not defined by a fall in HoloTC concentration from above one universally specified level to below another. Instead, vitamin B12 deficiency is defined by a change, in total vitamin B12, HoloTC or metabolite concentrations, from what is normal for the individual.
Fig. 5.
Alternative model for the development of vitamin B12 deficiency. Total B12, serum total vitamin B12 concentration; HoloTC, serum holotranscobalamin concentration; MMA, plasma methylmalonic acid concentration; tHcy, plasma total homocysteine concentration
Stages of development of vitamin B12 deficiency
The alternative model for the development of vitamin B12 deficiency contains only three stages: Normal; Depletion; Metabolic Deficiency (Fig. 5). The Normal stage is defined as the condition in which the intake, and the internal processing, for an individual provides sufficient vitamin B12 to sustain all of their metabolic requirements and maintain their body store of vitamin B12. The Depletion stage, marked by the commencement of a long-term fall in serum total vitamin B12 concentration, is defined as the condition in which the intake, or the internal processing, for an individual does not provide sufficient vitamin B12 to sustain all of their metabolic requirements, which are then maintained by depleting their body store of vitamin B12. The Metabolic Deficiency stage, marked by the commencement of a fall in the HoloTC concentration and an increase in either MMA or tHcy or both metabolites, is defined as the condition in which the depleted body store of vitamin B12, or the internal processing, for an individual is insufficient to sustain all of their metabolic requirements.
Cellular storage of vitamin B12 and potential delays in metabolic response to fall in HoloTC
Herbert (1994) stated: “holoTCII will always be low before there is a rise in methylmalonate or homocysteine if that rise is due to a vitamin B-12 deficiency.” This alternative model proposes an additional principle; that any fall in HoloTC, to below normal for the individual, must result in a disturbed metabolism and a rise in the metabolites. How quickly this happens depends on how much vitamin B12 is stored in the cells; this varies between cell types; some cells, including nerve cells and some blood cells, have very small vitamin B12 stores. For example, as stated by Herbert (1994) “Lack of delivery of vitamin B-12 to the glial cells of the brain quickly wipes out their small vitamin B-12 stores, after which they become vitamin B-12 deficient”.
This alternative hypothesis therefore assumes that, for at least some cell types, there will be no significant delay between the fall in HoloTC concentration to below normal for the individual, and the rise in MMA and/or tHcy. This is consistent with Herbert (1987) where, in referring to the timing of a fall in HoloTC and the development of neutrophil hypersegmentation, he states that: “when one follows individuals from B-12 normality into the earliest stages of B-12 deficiency, one discovers that both fall almost together in the individual. The amount of B-12 on the B-12 delivery protein transcobalamin II falls sharply and, at almost the same time (probably fractionally later), DNA synthesis becomes subnormal in the granulocytes.” Even if not all cells are affected immediately, and if the MMA and/or tHcy are not yet measurably abnormally high, the metabolism for some cell types has been disturbed. Thus in this alternative model, almost immediately after the HoloTC production falls below normal for any reason, the Depletion stage ends and the Metabolic Deficiency stage commences.
Dependence of timing of HoloTC response on cause of vitamin B12 deficiency
The magnitude and speed of any change in HoloTC concentration depends on the cause of the onset of vitamin B12 deficiency, as well as individual variables involved in the absorption, transport and utilization of vitamin B12. Three possible cases of disruption to the enterohepatic cycle are considered here: failure only after exhaustion of vitamin B12 liver store; instantaneous failure; gradual failure. The following discussion is based on this author’s hypothesis about how the response of total vitamin B12, HoloTC, tHcy and MMA depends on the cause of vitamin B12 deficiency. Human experimentation is needed to validate this model.
Failure only after exhaustion of vitamin B12 liver store
When there is no short-term disruption to the enterohepatic cycle, HoloTC concentration will be maintained until there is insufficient holohaptocorrin remaining to sustain HoloTC production. This case contains all stages of the general model, as shown in Fig. 5, where there is a significant Depletion period before the eventual failure of the enterohepatic cycle leads to the onset of Metabolic Deficiency. The total vitamin B12 falls, but HoloTC, MMA and tHcy remain normal, during the Depletion period. When the liver store of HoloHC is consumed, Metabolic Deficiency commences, with the HoloTC concentration falling and the MMA and tHcy increasing. This case applies where the failure is outside of the HoloTC feedback control loop (Fig. 4), for example when the vitamin B12 deficiency is caused by reduction in intake, or reduction in the utilization of the vitamin B12 in the cells because of a defect in the intracellular cobalamin metabolism. Another, very common, example of this case is food-cobalamin malabsorption where vitamin B12 bound to food protein cannot be released because of hypochlorhydria due to gastric atrophy (Carmel 1995; Andrès et al. 2004). This common cause of vitamin B12 deficiency in the elderly is not the same as pernicious anaemia because production of intrinsic factor is not affected; the patient is able to absorb unbound vitamin B12. Examples of such cases consistent with this alternative model, where vitamin B12 deficiency was likely to be caused by gradual loss of gastric acid production, were those whose subjects were elderly (Miller et al. 2006; Clarke et al. 2007; Schrempf et al. 2011; Palacios et al. 2013; Remacha et al. 2014).
Instantaneous failure
If the production of HoloTC suddenly halts, because of an instantaneous failure of the enterohepatic cycle, for example as a result of the surgical removal of the parietal cells of the stomach, an extreme case of the proposed model will apply. As shown in Fig. 6, the sudden loss of HoloTC will cause an almost immediate metabolic disturbance and a rise in the concentration of MMA and/or HoloTC. Thus, there will be no Depletion period in this case, because MMA and/or tHcy will respond almost instantaneously to the fall in HoloTC concentration, and the Metabolic Deficiency stage commences almost immediately.
Fig. 6.
Instantaneous failure of enterohepatic recycling. Total B12, serum total vitamin B12 concentration; HoloTC, serum holotranscobalamin concentration; MMA, plasma methylmalonic acid concentration; tHcy, plasma total homocysteine concentration
Gradual failure
Figure 7 illustrates the case where the production of HoloTC gradually fails, for example as a result of loss of parietal cell function due to the autoimmune disease pernicious anaemia. As for the case of instantaneous failure, there is no Depletion period, and the Metabolic Deficiency stage commences almost immediately, because MMA and/or tHcy will start to increase immediately after the HoloTC concentration falls below the normal level for the individual. The difference in this case is that the rate of change of the analytes will be slower than when the supply of intrinsic factor is suddenly stopped.
Fig. 7.
Gradual failure of enterohepatic recycling. Total B12, serum total vitamin B12 concentration; HoloTC, serum holotranscobalamin concentration; MMA, plasma methylmalonic acid concentration; tHcy, plasma total homocysteine concentration
Consequences of questioning Herbert’s model
Questioning of Herbert’s hypothesis that HoloTC is the most sensitive marker of Early Negative Vitamin B12Balance, or his model for the sequential stages in the development of vitamin B12 deficiency, is likely to raise strong objections.
Firstly, any model that is based on changes from individual normal analyte concentrations, instead of comparison with a universally accepted population normal, conflicts with the dogma that there must be a gold-standard test for vitamin B12 deficiency; either HoloTC or one a yet to be discovered.
Secondly, any model that requires a comparison of current analyte concentrations with a patient’s own normal levels would require proactive testing of all persons at risk, before the onset of any symptoms, to obtain their individual healthy baseline concentrations. Herbert himself suggested proactive testing, saying “serum holoTCIl should be measured every 5 y starting at age 55 because gradual loss of the ability to absorb vitamin B-12 occurs in everyone in a genetically determined, age-dependent pattern.” (Herbert 1994).
A potential alternative to obtaining a longitudinal record for individuals at risk is the use of an algorithm to combine the results of a one-off test of all four analytes into a single parameter. A mathematical model for this has been devised and described in detail by Fedosov (2010), and further tested and refined (Fedosov 2013; Fedosov et al. 2015; Brito et al. 2016). This author is cautious about this approach because, as with all other current methods, it might apply well to a population but not necessarily to an individual. This would need extensive testing on a wide range of subjects, for various causes of vitamin B12 deficiency, before it could be validated.
Summary and conclusion
Axis-Shield and others, in promoting the commercialisation of the HoloTC immunoassay, have relied on Herbert’s erroneous hypothesis that “Ho1oTCII falls below the bottom of its normal range long before total serum vitamin B-12 … falls below the bottom of its normal range”, and his flawed model for the staged development of vitamin B12 deficiency (Herbert 1994).
Herbert’s model is flawed because it assumes that a normal minimum concentration for HoloTC may be universally defined. As with total vitamin B12, evidenced by the failure to find such a single cut-off value for HoloTC and instead the discovery of a wide grey zone for HoloTC, the range of normal for an individual is much smaller than for the population. As stated by Herbert (1994): “What is normal for one is not normal for another”.
Herbert’s hypothesis, that HoloTC will respond early to vitamin B12 depletion, before the onset of a clinical deficiency, is erroneous because it does not take into account how enterohepatic recycling regulates the HoloTC concentration. Where the cause of vitamin B12 deficiency does not disrupt the enterohepatic cycle, HoloTC will not be an early responder to a deficiency; there will be a Depletion period, in which total vitamin B12 falls, but HoloTC and the metabolites will only respond after the liver store is exhausted. When the cause of vitamin B12 deficiency does disrupt the enterohepatic cycle, the HoloTC will be an early responder but there will be no Depletion period; the metabolites will respond quickly when HoloTC falls below normal for the individual.
The HoloTC immunoassay cannot be used to measure vitamin B12 status any more reliably than total vitamin B12, or to predict the onset of a metabolic deficiency, because it is based on an erroneous hypothesis and a flawed model for the staged development of vitamin B12 deficiency.
Acknowledgements
I thank the reviewers for taking the time to read my manuscript and prepare their reports.
Competing interests
The sole author declares that he has no competing interests.
Data availability
PDF and PowerPoint copies of Figures 1 to 7 are available for download in Additional files 1 and 2 respectively. A Microsoft Excel file, containing tables of data relating to references, is available for download in Additional file 3.
Additional files
10.1186/s40064-016-2252-z Figures 1 to 7, High-resolution images.
10.1186/s40064-016-2252-z Figures 1 to 7, High-resolution slides.
10.1186/s40064-016-2252-z Reference Data, tables.
References
- Abbott Laboratories . Why HoloTC? Wiesbaden: Abbott Laboratories Inc; 2006. [Google Scholar]
- Abbott Laboratories . ARCHITECT Active-B12. Wiesbaden: Abbott Laboratories Inc; 2011. [Google Scholar]
- Al Aisari F, Al-Hashmi H, Mula-Abed WA. Comparison between serum holotranscobalamin and total vitamin B12 as indicators of vitamin B12 status. Oman Med J. 2010;25(1):9–12. doi: 10.5001/omj.2010.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrès E, Loukili NH, Noel E, Kaltenbach G, Abdelgheni MB, Perrin AE, Noblet-Dick M, Maloisel F, Schlienger JL, Blicklé JF. Vitamin B12 (cobalamin) deficiency in elderly patients. CMAJ. 2004;171(3):251–259. doi: 10.1503/cmaj.1031155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aparicio-Ugarriza R, Palacios G, Alder M, González-Gross M. A review of the cut-off points for the diagnosis of vitamin B12 deficiency in the general population. Clin Chem Lab Med. 2014;53(8):1149–1159. doi: 10.1515/cclm-2014-0784. [DOI] [PubMed] [Google Scholar]
- Augoustides-Savvopoulou P, IBannou H, Gkouliavoudi S (2007) Holotranscobalamin and homocysteine as markers of cobalamin status in infants. In: Abstract P6 presented at 6th Conference on Homocysteine Metablolism, World Congress on Hyperhomocysteinemia, Saarbruecken
- Axis-Shield . Active-B12 (holotranscobalamin) clinical background and product information. Dundee: Axis-Shield Diagnostics Ltd; 2007. [Google Scholar]
- Axis-Shield . Axis-Shield HoloTC RIA. Dundee: Axis-Shield Diagnostics Ltd; 2007. [Google Scholar]
- Axis-Shield (2012) Vitamin B12 Symposium, Nancy, France. http://www.active-b12.com/Meetings/B12Symposium. Accessed 2 Dec 2014
- Axis-Shield (2014a) What is Active-B12? http://www.active-b12.com/What-Is-Active-B12. Accessed 2 Dec 2014
- Axis-Shield (2014b) Clinical utility—correlation between Active-B12 and Total B12. http://www.active-b12.com/Clinical-Utility. Accessed 2 Dec 2014
- Axis-Shield and Abbott Laboratories . AxSYM® Active-B12 (holotranscobalamin) Wiesbaden and Dundee: Abbott Laboratories Inc and Axis-Shield Diagnostics Ltd; 2006. [Google Scholar]
- Axis-Shield and Abbott Laboratories . Active-B12 (holotranscobalamin): the next level of B12 testing. Wiesbaden and Dundee: Abbott Laboratories Inc and Axis-Shield Diagnostics Ltd; 2006. [Google Scholar]
- Axis-Shield and Abbott Laboratories . AxSYM® Active-B12 (holotranscobalamin) package insert. Wiesbaden and Dundee: Abbott Laboratories Inc and Axis-Shield Diagnostics Ltd; 2007. [Google Scholar]
- Axis-Shield and Abbott Laboratories . Active-B12 (Holotranscobalamin) Publication Abstracts 2007. Wiesbaden and Dundee: Abbott Laboratories Inc and Axis-Shield Diagnostics Ltd; 2007. [Google Scholar]
- Bamonti F, Moscato GA, Novembrino C, Gregori D, Novi C, De Giuseppe R, Galli C, Uva V, Lonati S, Maiavacca R. Determination of serum holotranscobalamin concentrations with the AxSYM active B(12) assay: cut-off point evaluation in the clinical laboratory. Clin Chem Lab Med. 2010;48(2):249–253. doi: 10.1515/CCLM.2010.032. [DOI] [PubMed] [Google Scholar]
- Bhat DS, Thuse NV, Lubree HG, Joglekar CV, Naik SS, Ramdas LV, Johnston C, Refsum H, Fall CH, Yajnik CS. Increases in plasma holotranscobalamin can be used to assess vitamin B-12 absorption in individuals with low plasma vitamin B-12. J Nutr. 2009;139(11):2119–2123. doi: 10.3945/jn.109.107359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black M, Tam C, Whitehead S, Bailey M, Dunster K, Leaver C, Cole-Sinclair M, George P, Schneider HG (2006) Holotranscobalamin—a novel marker for vitamin B12 deficiency—clinical utility? In: Proceedings of the Australasian Association of Clinical Biochemists’ 44th Annual Scientific Conference. Clin Biochem Rev 27 S(ii), p S32
- Bor MV, Nexø E, Hvas AM. Holo-transcobalamin concentration and transcobalamin saturation reflect recent vitamin B12 absorption better than does serum vitamin B12. Clin Chem. 2004;50(6):1043–1049. doi: 10.1373/clinchem.2003.027458. [DOI] [PubMed] [Google Scholar]
- Bor MV, Cetin M, Aytaç S, Altay C, Nexo E. Nonradioactive vitamin B12 absorption test evaluated in controls and in patients with inherited malabsorption of vitamin B12. Clin Chem. 2005;51(11):2151–2155. doi: 10.1373/clinchem.2005.055509. [DOI] [PubMed] [Google Scholar]
- Brady J, Wilson L, McGregor L, Vazquez M, Valente E, Orning L (2007) Direct assay for the quantitative assessment of holo-transcobalamin in serum and plasma. Axis-Shield Diagnostics Ltd, Dundee, Scotland and Axis-Shield ASA, Oslo, Norway
- Brady J, Wilson L, McGregor L, Valente E, Orning L. Active B12: a rapid, automated assay for holotranscobalamin on the Abbott AxSYM analyzer. Clin Chem. 2008;54(3):567–573. doi: 10.1373/clinchem.2007.096784. [DOI] [PubMed] [Google Scholar]
- Brito A, Verdugo R, Hertrampf E, Miller JW, Green R, Fedosov SN, Shahab-Ferdows S, Sanchez H, Albala C, Castillo JL, Matamala JM, Uauy R, Allen LH. Vitamin B-12 treatment of asymptomatic, deficient, elderly Chileans improves conductivity in myelinated peripheral nerves, but high serum folate impairs vitamin B-12 status response assessed by the combined indicator of vitamin B-12 status. Am J Clin Nutr. 2016;103(1):250–257. doi: 10.3945/ajcn.115.116509. [DOI] [PubMed] [Google Scholar]
- Čabarkapa V, Stošić Z, Žeravica R, Ilinčić B, Filipović A. The importance of holotranscobalamin measurement. J Med Biochem. 2007;26(3):227–230. [Google Scholar]
- Carmel R. Malabsorption of food cobalamin. Baillieres Clin Haematol. 1995;8(3):639–655. doi: 10.1016/S0950-3536(05)80224-0. [DOI] [PubMed] [Google Scholar]
- Carmel R. Measuring and interpreting holo-transcobalamin (holo-transcobalamin II) Clin Chem. 2002;48(3):407–409. [PubMed] [Google Scholar]
- Carmel R. Biomarkers of cobalamin (vitamin B-12) status in the epidemiologic setting: a critical overview of context, applications, and performance characteristics of cobalamin, methylmalonic acid, and holotranscobalamin II. Am J Clin Nutr. 2011;94(1):348S–358S. doi: 10.3945/ajcn.111.013441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carmel R. Holotranscobalamin: not ready for prime time. Clin Chem. 2012;58(3):643–645. doi: 10.1373/clinchem.2011.174516. [DOI] [PubMed] [Google Scholar]
- Carmel R, Agrawal YP. More on failures of cobalamin assays in pernicious anemia. N Engl J Med. 2012;367(16):1570. doi: 10.1056/NEJMc1204070. [DOI] [PubMed] [Google Scholar]
- Chatthanawaree W. Biomarkers of cobalamin (vitamin B12) deficiency and its application. J Nutr Health Aging. 2011;15(3):227–231. doi: 10.1007/s12603-010-0280-x. [DOI] [PubMed] [Google Scholar]
- Chen X, Remacha AF, Sardà MP, Carmel R. Influence of cobalamin deficiency compared with that of cobalamin absorption on serum holo-transcobalamin II. Am J Clin Nutr. 2005;81(1):110–114. doi: 10.1093/ajcn/81.1.110. [DOI] [PubMed] [Google Scholar]
- Clarke R, Sherliker P, Hin H, Nexo E, Hvas AM, Schneede J, Birks J, Ueland PM, Emmens K, Scott JM, Molloy AM, Evans JG. Detection of vitamin B12 deficiency in older people by measuring vitamin B12 or the active fraction of vitamin B12, holotranscobalamin. Clin Chem. 2007;53(5):963–970. doi: 10.1373/clinchem.2006.080382. [DOI] [PubMed] [Google Scholar]
- Devalia V. Diagnosing vitamin B-12 deficiency on the basis of serum B-12 assay. BMJ. 2006;333(7564):385–386. doi: 10.1136/bmj.333.7564.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devalia V, Hamilton MS, Molloy AM, the British Committee for Standards in Haematology Guidelines for the diagnosis and treatment of cobalamin and folate disorders. Br J Haematol. 2014 doi: 10.1111/bjh.12959. [DOI] [PubMed] [Google Scholar]
- Eureka (2000) Development of diagnostic test for HoloTC. Project E! 2263—HOLOTC. http://www.eurekanetwork.org/project/-/id/2263. Accessed 13 Jan 2015
- European Union (2002) Demonstration of the clinical utility of holotc as an early marker of vitamin B12 deficiency. Project reference: QLK3-CT-2002-01775. http://cordis.europa.eu/project/rcn/69759_en.html. Accessed 2 Dec 2014
- Fedosov SN. Metabolic signs of vitamin B(12) deficiency in humans: computational model and its implications for diagnostics. Metabolism. 2010;59(8):1124–1138. doi: 10.1016/j.metabol.2009.09.036. [DOI] [PubMed] [Google Scholar]
- Fedosov SN. Biochemical markers of vitamin B12 deficiency combined in one diagnostic parameter: the age-dependence and association with cognitive function and blood hemoglobin. Clin Chim Acta. 2013;422:47–53. doi: 10.1016/j.cca.2013.04.002. [DOI] [PubMed] [Google Scholar]
- Fedosov SN, Brito A, Miller JW, Green R, Allen LH. Combined indicator of vitamin B12 status: modification for missing biomarkers and folate status and recommendations for revised cut-points. Clin Chem Lab Med. 2015;53(8):1215–1225. doi: 10.1515/cclm-2014-0818. [DOI] [PubMed] [Google Scholar]
- Fragasso A, Mannarella C, Ciancio A, Scarciolla O, Nuzzolese N, Clemente R, Vitullo E, Sacco A (2012) Holotranscobalamin is a useful marker of vitamin B12 deficiency in alcoholics. Sci World J 2012:128182. doi:10.1100/2012/128182 [DOI] [PMC free article] [PubMed]
- Furger E (2012) Structural and functional characterisation of the cobalamin transport protein haptocorrin, Thesis, ETH Zurich. http://e-collection.library.ethz.ch/eserv/eth:6531/eth-6531-02.pdf. Accessed 21 March 2016
- Golding PH. Experimental vitamin B12 deficiency in a human subject—a longitudinal investigation of the performance of the holotranscobalamin (HoloTC, Active-B12) immunoassay. SpringerPlus. 2016;5:184. doi: 10.1186/s40064-016-1740-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goringe A, Ellis R, McDowell I, Vidal-Alaball J, Jenkins C, Butler C, Worwood M. The limited value of methylmalonic acid, homocysteine and holotranscobalamin in the diagnosis of early B12 deficiency. Haematologica. 2006;91(2):231–234. [PubMed] [Google Scholar]
- Green R (2007) Active B12—the next level of B12 testing. Specialty Labs Web Conference. 13 Dec 2007
- Green R. Indicators for assessing folate and vitamin B-12 status and for monitoring the efficacy of intervention strategies. Am J Clin Nutr. 2011;94(2):666S–672S. doi: 10.3945/ajcn.110.009613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greibe E, Arendt J, Nexo E. More on failures of cobalamin assays in pernicious anemia. N Engl J Med. 2012;367(16):1569–1570. doi: 10.1056/NEJMc1210169. [DOI] [PubMed] [Google Scholar]
- Heil SG, de Jonge R, de Rotte MC, van Wijnen M, Heiner-Fokkema RM, Kobold AC, Pekelharing JM, Adriaansen HJ, Sanders E, Trienekens PH, Rammeloo T, Lindemans J. Screening for metabolic vitamin B12 deficiency by holotranscobalamin in patients suspected of vitamin B12 deficiency: a multicentre study. Ann Clin Biochem. 2012;49(2):184–189. doi: 10.1258/acb.2011.011039. [DOI] [PubMed] [Google Scholar]
- Herbert V. The 1986 Herman award lecture. Nutrition science as a continually unfolding story: the folate and vitamin B-12 paradigm. Am J Clin Nutr. 1987;46(3):387–402. doi: 10.1093/ajcn/46.3.387. [DOI] [PubMed] [Google Scholar]
- Herbert V. Staging vitamin B-12 (cobalamin) status in vegetarians. Am J Clin. 1994;59(5 Suppl):1213S–1222S. doi: 10.1093/ajcn/59.5.1213S. [DOI] [PubMed] [Google Scholar]
- Herrmann W, Obeid R (2007) Role of cobalamin in human metabolism and modern tools diagnosing its status. In: Abstract P18 presented at 6th Conference on Homocysteine Metablolism, World Congress on Hyperhomocysteinemia, Saarbruecken
- Herrmann W, Obeid R. Causes and early diagnosis of vitamin B12 deficiency. Dtsch Arztebl Int. 2008;105(40):680–685. doi: 10.3238/arztebl.2008.0680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann W, Obeid R. Utility and limitations of biochemical markers of vitamin B12 deficiency. Eur J Clin Invest. 2013;43(3):231–237. doi: 10.1111/eci.12034. [DOI] [PubMed] [Google Scholar]
- Herrmann W, Obeid R, Schorr H, Geisel J. Functional vitamin B12 deficiency and determination of holotranscobalamin in populations at risk. Clin Chem Lab Med. 2003;41(11):1478–1488. doi: 10.1515/CCLM.2003.227. [DOI] [PubMed] [Google Scholar]
- Herrmann W, Schorr H, Obeid R, Geisel J. Vitamin B-12 status, particularly holotranscobalamin II and methylmalonic acid concentrations, and hyperhomocysteinemia in vegetarians. Am J Clin Nutr. 2003;78(1):131–136. doi: 10.1093/ajcn/78.1.131. [DOI] [PubMed] [Google Scholar]
- Herrmann W, Obeid R, Schorr H, Geisel J. The usefulness of holotranscobalamin in predicting vitamin B12 status in different clinical settings. Curr Drug Metab. 2005;6(1):47–53. doi: 10.2174/1389200052997384. [DOI] [PubMed] [Google Scholar]
- Herrmann et al (2012) Expert’s Consensus Statement. Axis-Shield Diagnostics Ltd, Dundee
- Herzlich B, Herbert V. Depletion of serum holotranscobalamin II. An early sign of negative vitamin B12 balance. Lab Invest. 1988;58(3):332–337. [PubMed] [Google Scholar]
- Hølleland G, Schneede J, Ueland PM, Lund PK, Refsum H, Sandberg S. Cobalamin deficiency in general practice. Assessment of the diagnostic utility and cost-benefit analysis of methylmalonic acid determination in relation to current diagnostic strategies. Clin Chem. 1999;45(2):189–198. [PubMed] [Google Scholar]
- Hooshmand B, Solomon A, Kåreholt I, Rusanen M, Hänninen T, Leiviskä J, Winblad B, Laatikainen T, Soininen H, Kivipelto M. Associations between serum homocysteine, holotranscobalamin, folate and cognition in the elderly: a longitudinal study. J Intern Med. 2012;271(2):204–212. doi: 10.1111/j.1365-2796.2011.02484.x. [DOI] [PubMed] [Google Scholar]
- Hvas AM, Nexo E. Holotranscobalamin as a predictor of vitamin B12 status. Clin Chem Lab Med. 2003;41(11):1489–1492. doi: 10.1515/CCLM.2003.228. [DOI] [PubMed] [Google Scholar]
- Hvas AM, Nexo E. Holotranscobalamin—a first choice assay for diagnosing early vitamin B deficiency? J Intern Med. 2005;257(3):289–298. doi: 10.1111/j.1365-2796.2004.01437.x. [DOI] [PubMed] [Google Scholar]
- Hvas AM, Nexo E. Diagnosis and treatment of vitamin B12 deficiency—an update. Haematologica. 2006;91(11):1506–1512. [PubMed] [Google Scholar]
- Hvas AM, Gravholt CH, Nexo E. Circadian variation of holo-transcobalamin (holo-TC) and related markers. Clin Chem Lab Med. 2005;43(7):760–764. doi: 10.1515/CCLM.2005.130. [DOI] [PubMed] [Google Scholar]
- Hvas AM, Morkbak AL, Nexo E. Plasma holotranscobalamin compared with plasma cobalamins for assessment of vitamin B12 absorption; optimisation of a non-radioactive vitamin B12 absorption test (CobaSorb) Clin Chim Acta. 2007;376(1–2):150–154. doi: 10.1016/j.cca.2006.08.009. [DOI] [PubMed] [Google Scholar]
- IBL International . Active-B12 (Holotranscobalamin) ELISA. Hamburg: IBL International GMBH; 2013. [Google Scholar]
- Lee YK, Kim HS, Kang HJ. Holotranscobalamin as an indicator of vitamin B12 deficiency in gastrectomized patients. Ann Clin Lab Sci. 2009;39(4):361–366. [PubMed] [Google Scholar]
- Lindemans J, Griffioen P, van Wijnen M, Sanders E, Rammeloo T, Reiner-Fokkema RM, Muller Kobold AC, Pekelharing JP, Adriaansen HJ, Trienekens P, de Jonge R (2007) Holo-Transcobalamin: more or less than total vitamin B12? A multicenter study. In: Poster presented at the Euromedlab—17th IFCC-FESCC European Congress of Clinical Chemistry and Laboratory Medicine, Amsterdam
- Lindenbaum J, Healton EB, Savage DG, Brust JC, Garrett TJ, Podell ER, Marcell PD, Stabler SP, Allen RH. Neuropsychiatric disorders caused by cobalamin deficiency in the absence of anemia or macrocytosis. N Engl J Med. 1988;318(26):1720–1728. doi: 10.1056/NEJM198806303182604. [DOI] [PubMed] [Google Scholar]
- Lindgren A, Kilander A, Bagge E, Nexø E. Holotranscobalamin—a sensitive marker of cobalamin malabsorption. Eur J Clin Invest. 1999;29(4):321–329. doi: 10.1046/j.1365-2362.1999.00446.x. [DOI] [PubMed] [Google Scholar]
- Lloyd-Wright Z, Hvas AM, Møller J, Sanders TA, Nexø E. Holotranscobalamin as an indicator of dietary vitamin B12 deficiency. Clin Chem. 2003;49(12):2076–2078. doi: 10.1373/clinchem.2003.020743. [DOI] [PubMed] [Google Scholar]
- Lobreglio GB, Gatto A, Cardinali R, Fiorentino D, Rizzo G, Pappaccogli L, Sparascio M (2008) Holotranscobalamin (Holo-TC) for diagnosing early vitamin B12 deficiency. In: Abstract 1012 presented at the 13th Congress of the European Hematology Association, Haematologica 93(s1), p 403
- Loikas S (2007) Vitamin B12 deficiency in the aged: laboratory diagnosis, prevalence and clinical profile, Thesis. University of Turku. https://www.doria.fi/bitstream/handle/10024/29134/D775.pdf?sequence=1. Accessed 21 March 2016
- Loikas S, Löppönen M, Suominen P, Møller J, Irjala K, Isoaho R, Kivelä SL, Koskinen P, Pelliniemi TT. RIA for serum holo-transcobalamin: method evaluation in the clinical laboratory and reference interval. Clin Chem. 2003;49(3):455–462. doi: 10.1373/49.3.455. [DOI] [PubMed] [Google Scholar]
- Loikas S, Koskinen P, Irjala K, Löppönen M, Isoaho R, Kivelä SL, Pelliniemi TT. Vitamin B12 deficiency in the aged: a population-based study. Age Ageing. 2007;36(2):177–183. doi: 10.1093/ageing/afl150. [DOI] [PubMed] [Google Scholar]
- Loikas S, Koskinen P, Irjala K, Löppönen M, Isoaho R, Kivelä SL, Pelliniemi TT. Renal impairment compromises the use of total homocysteine and methylmalonic acid but not total vitamin B12 and holotranscobalamin in screening for vitamin B12 deficiency in the aged. Clin Chem Lab Med. 2007;45(2):197–201. doi: 10.1515/CCLM.2007.028. [DOI] [PubMed] [Google Scholar]
- McCaddon A, Hudson P, McCracken C, Ellis R, McCaddon A. Biological variation of holo-transcobalamin in elderly individuals. Clin Chem. 2003;49(9):1542–1544. doi: 10.1373/49.9.1542. [DOI] [PubMed] [Google Scholar]
- Miller JW, Garrod MG, Rockwood AL, Kushnir MM, Allen LH, Haan MN, Green R. Measurement of total vitamin B12 and holotranscobalamin, singly and in combination, in screening for metabolic vitamin B12 deficiency. Clin Chem. 2006;52(2):278–285. doi: 10.1373/clinchem.2005.061382. [DOI] [PubMed] [Google Scholar]
- Morkbak AL, Heimdal RM, Emmens K, Molloy A, Hvas AM, Schneede J, Clarke R, Scott JM, Ueland PM, Nexo E. Evaluation of the technical performance of novel holotranscobalamin (holoTC) assays in a multicenter European demonstration project. Clin Chem Lab Med. 2005;43(10):1058–1064. doi: 10.1515/CCLM.2005.185. [DOI] [PubMed] [Google Scholar]
- Morkbak AL, Hvas AM, Milman N, Nexo E. Holotranscobalamin remains unchanged during pregnancy. Longitudinal changes of cobalamins and their binding proteins during pregnancy and postpartum. Haematologica. 2007;92(12):1711–1712. doi: 10.3324/haematol.11636. [DOI] [PubMed] [Google Scholar]
- Neale G. B12 binding proteins. Gut. 1990;31(1):59–63. doi: 10.1136/gut.31.1.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nexo E, Hoffmann-Lücke E. Holotranscobalamin, a marker of vitamin B-12 status: analytical aspects and clinical utility. Am J Clin Nutr. 2011;94(1):359S–365S. doi: 10.3945/ajcn.111.013458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nexo E, Hvas AM, Bleie Ø, Refsum H, Fedosov SN, Vollset SE, Schneede J, Nordrehaug JE, Ueland PM, Nygard OK. Holo-transcobalamin is an early marker of changes in cobalamin homeostasis. A randomized placebo-controlled study. Clin Chem. 2002;48(10):1768–1771. [PubMed] [Google Scholar]
- Nexo E, Christensen AL, Hvas AM, Petersen TE, Fedosov SN. Quantification of holo-transcobalamin, a marker of vitamin B12 deficiency. Clin Chem. 2002;48(3):561–562. [PubMed] [Google Scholar]
- Nilsson K, Isaksson A, Gustafson L, Hultberg B. Clinical utility of serum holotranscobalamin as a marker of cobalamin status in elderly patients with neuropsychiatric symptoms. Clin Chem Lab Med. 2004;42(6):637–643. doi: 10.1515/CCLM.2004.109. [DOI] [PubMed] [Google Scholar]
- Obeid R, Herrmann W. Holotranscobalamin in laboratory diagnosis of cobalamin deficiency compared to total cobalamin and methylmalonic acid. Clin Chem Lab Med. 2007;45(12):1746–1750. doi: 10.1515/CCLM.2007.361. [DOI] [PubMed] [Google Scholar]
- Obeid R, Herrmann W (2007b) Can holotranscobalamin replace total serum cobalamin in laboratory diagnosis of cobalamin deficiency? In: Abstract P29 presented at 6th Conference on Homocysteine Metablolism, World Congress on Hyperhomocysteinemia, Saarbruecken
- Oberley MJ, Yang DT. Laboratory testing for cobalamin deficiency in megaloblastic anemia. Am J Hematol. 2013;88(6):522–526. doi: 10.1002/ajh.23421. [DOI] [PubMed] [Google Scholar]
- Oh R, Brown DL. Vitamin B12 deficiency. Am Fam Physician. 2003;67(5):979–986. [PubMed] [Google Scholar]
- Palacios G, Sola R, Barrios L, Pietrzik K, Castillo MJ, González-Gross M. Algorithm for the early diagnosis of vitamin B12 deficiency in elderly people. Nutr Hosp. 2013;28(5):1447–1452. doi: 10.3305/nh.2013.28.5.6821. [DOI] [PubMed] [Google Scholar]
- Pry T (2006) Holotranscobalamin; a predictor of vitamin B12 status. In: Presentation to AACB Industry Workshops Wednesday
- Quadros EV. Advances in the understanding of cobalamin assimilation and metabolism. Br J Haematol. 2010;148(2):195–204. doi: 10.1111/j.1365-2141.2009.07937.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Refsum H, Johnston C, Guttormsen AB, Nexo E. Holotranscobalamin and total transcobalamin in human plasma: determination, determinants, and reference values in healthy adults. Clin Chem. 2006;52(1):129–137. doi: 10.1373/clinchem.2005.054619. [DOI] [PubMed] [Google Scholar]
- Remacha AF, Sardà MP, Canals C, Queraltò JM, Zapico E, Remacha J, Carrascosa C. Role of serum holotranscobalamin (holoTC) in the diagnosis of patients with low serum cobalamin. Comparison with methylmalonic acid and homocysteine. Ann Hematol. 2014;93(4):565–569. doi: 10.1007/s00277-013-1905-z. [DOI] [PubMed] [Google Scholar]
- Robinson DJ, O’Luanaigh C, Tehee E, O’Connell H, Hamilton F, Chin AV, Coen R, Molloy AM, Scott J, Cunningham CJ, Lawlor BA. Associations between holotranscobalamin, vitamin B12, homocysteine and depressive symptoms in community-dwelling elders. Int J Geriatr Psychiatry. 2011;26(3):307–313. doi: 10.1002/gps.2530. [DOI] [PubMed] [Google Scholar]
- Schrempf W, Eulitz M, Neumeister V, Siegert G, Koch R, Reichmann H, Storch A. Utility of measuring vitamin B12 and its active fraction, holotranscobalamin, in neurological vitamin B12 deficiency syndromes. J Neurol. 2011;258(3):393–401. doi: 10.1007/s00415-010-5764-4. [DOI] [PubMed] [Google Scholar]
- Scott JM, Molloy AM, Archbold P, Linton T, Schneede J, Ueland PM, Orning L, Valente E, Clarke R and Nexo E (2007) Clinical utility of holoTC compared to three currently used assays to determine vitamin B12 status. In: Abstract P32 presented at 6th Conference on homocysteine metablolism, World Congress on Hyperhomocysteinemia, Saarbruecken
- Seetharam B, Yammani RR. Cobalamin transport proteins and their cell-surface receptors. Expert Rev Mol Med. 2003;5(18):1–18. doi: 10.1017/S1462399403006422. [DOI] [PubMed] [Google Scholar]
- Serefhanoglu S, Aydogdu I, Kekilli E, Ilhan A, Kuku I. Measuring holotranscobalamin II, an early indicator of negative vitamin B12 balance, by radioimmunoassay in patients with ischemic cerebrovascular disease. Ann Hematol. 2008;87(5):391–395. doi: 10.1007/s00277-007-0406-3. [DOI] [PubMed] [Google Scholar]
- Sikaris K (2010) Melbourne pathology approaches to vitamin B12 deficiency, Dr Ken Sikaris. Axis-Shield. http://www.active-b12.com/sites/default/files/Dr%20Sikaris%20Testimonial.pdf. Accessed 2 Dec2014
- Snow CF. Laboratory diagnosis of vitamin B12 and folate deficiency: a guide for the primary care physician. Arch Intern Med. 1999;159(12):1289–1298. doi: 10.1001/archinte.159.12.1289. [DOI] [PubMed] [Google Scholar]
- Sobczyńska-Malefora A, Gorska R, Pelisser M, Ruwona P, Witchlow B, Harrington DJ. An audit of holotranscobalamin (“Active” B12) and methylmalonic acid assays for the assessment of vitamin B12 status: application in a mixed patient population. Clin Biochem. 2014;47(1–2):82–86. doi: 10.1016/j.clinbiochem.2013.08.006. [DOI] [PubMed] [Google Scholar]
- Solomon LR. Cobalamin-responsive disorders in the ambulatory care setting: unreliability of cobalamin, methylmalonic acid, and homocysteine testing. Blood. 2005;105(3):978–985. doi: 10.1182/blood-2004-04-1641. [DOI] [PubMed] [Google Scholar]
- Ulleland M, Eilertsen I, Quadros EV, Rothenberg SP, Fedosov SN, Sundrehagen E, Orning L. Direct assay for cobalamin bound to transcobalamin (holo-transcobalamin) in serum. Clin Chem. 2002;48(3):526–532. [PubMed] [Google Scholar]
- Valente E, Scott JM, Ueland PM, Cunningham C, Casey M, Molloy AM. Diagnostic accuracy of holotranscobalamin, methylmalonic acid, serum cobalamin, and other indicators of tissue vitamin B12 status in the elderly. Clin Chem. 2011;57(6):856–863. doi: 10.1373/clinchem.2010.158154. [DOI] [PubMed] [Google Scholar]
- van Asselt DZ, Thomas CM, Segers MF, Blom HJ, Wevers RA, Hoefnagels WH. Cobalamin-binding proteins in normal and cobalamin-deficient older subjects. Ann Clin Biochem. 2003;40(1):65–69. doi: 10.1258/000456303321016187. [DOI] [PubMed] [Google Scholar]
- Vanpoucke H, Martens F, Lomecky M, Blankenstein MA (2007) Comparison of 3 automated assays for total vitamin B12 with measurement of Holotranscobalamin as a marker for vitamin B12 deficiency. In: Poster presented at the 6th Conference on Homocysteine Metablolism, World Congress on Hyperhomocysteinemia, Saarbruecken
- von Castel-Roberts KM, Morkbak AL, Nexo E, Edgemon CA, Maneval DR, Shuster JJ, Valentine JF, Kauwell GP, Bailey LB. Holo-transcobalamin is an indicator of vitamin B-12 absorption in healthy adults with adequate vitamin B-12 status. Am J Clin Nutr. 2007;85(4):1057–1061. doi: 10.1093/ajcn/85.4.1057. [DOI] [PubMed] [Google Scholar]
- Wickramasinghe SN, Fida S. Correlations between holo-transcobalamin II, holo-haptocorrin, and total B12 in serum samples from healthy subjects and patients. J Clin Pathol. 1993;46(6):537–539. doi: 10.1136/jcp.46.6.537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo KS, Kim KE, Park JS, Park JI, Han JY. Relationship between the Levels of Holotranscobalamin and Vitamin B12. Korean J Lab Med. 2010;30(2):185–189. doi: 10.3343/kjlm.2010.30.2.185. [DOI] [PubMed] [Google Scholar]
- Yetley EA, Pfeiffer CM, Phinney KW, Bailey RL, Blackmore S, Bock JL, Brody LC, Carmel R, Curtin LR, Durazo-Arvizu RA, Eckfeldt JH, Green R, Gregory JF, 3rd, Hoofnagle AN, Jacobsen DW, Jacques PF, Lacher DA, Molloy AM, Massaro J, Mills JL, Nexo E, Rader JI, Selhub J, Sempos C, Shane B, Stabler S, Stover P, Tamura T, Tedstone A, Thorpe SJ, Coates PM, Johnson CL, Picciano MF. Biomarkers of vitamin B-12 status in NHANES: a roundtable summary. Am J Clin Nutr. 2011;94(1):313S–321S. doi: 10.3945/ajcn.111.013243. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
PDF and PowerPoint copies of Figures 1 to 7 are available for download in Additional files 1 and 2 respectively. A Microsoft Excel file, containing tables of data relating to references, is available for download in Additional file 3.


