Abstract
Neurofibromas are slow-growing, painless, benign nerve-sheath tumors. They occur most commonly in the dermis and subcutis and are rarely found in the breast. We report a rare case of a solitary neurofibroma of the breast in a 61-year-old asymptomatic woman.
Case report
A 61-year-old woman presented to our comprehensive breast center for her routine yearly screening mammogram. At the time of the study, she reported no breast-related complaints and no general symptoms, nor any personal or family history of neurofibromatosis. Screening mammography and further mammographic workup (Fig. 1) showed a mass in the right breast.
Figure 1.
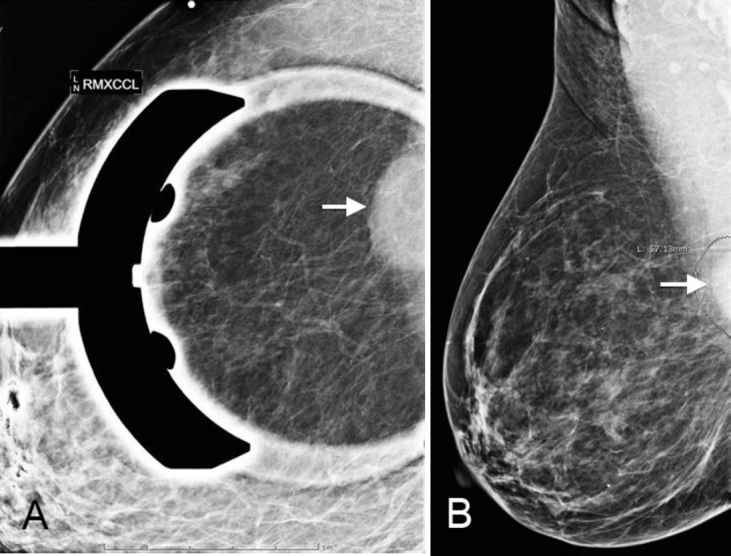
61-year-old female with neurofibroma of the right breast shows a 2.6 cm, equal-density, circumscribed mass (arrow) with partially obscured posterior margins in the posterior right-upper-outer quadrant. A. Craniocaudad view.B. Mediolateral oblique view.
Figure 2 shows the sonographic features of this mass. It was an oval, 2.2 × 1.7 × 1.1 cm, circumscribed, parallel solid mass in the right upper outer quadrant at 10 o’clock, approximately 6 cm from the nipple, corresponding to the mammographic mass. Given the anechoic appearance, circumscribed margins, and posterior acoustic enhancement seen on ultrasound, the mass was thought to likely represent a simple cyst. Aspiration was recommended due to the obscured margins on mammography.
Figure 2, A&B.
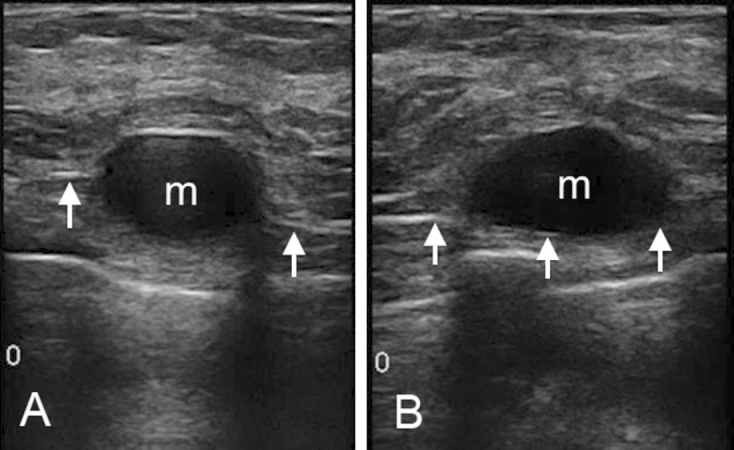
A. 61-year-old female with neurofibroma of the breast. Sonogram of the right breast. Arrows indicate the margin of the pectoralis muscle. The mass (m) abuts the chest wall, but is present within the breast. Parenchymal breast tissue and fat are seen above the mass. B. Parenchymal breast tissue and fat are seen above the mass.
Eight days after her initial presentation, the patient underwent attempted aspiration of the mass (Fig. 3) under sonographic guidance. No fluid was obtained during the aspiration attempt. The mass was then determined to be solid, and ultrasound-guided core biopsy of the mass was performed using a spring-loaded needle system (Fig. 4).
Figure 3.
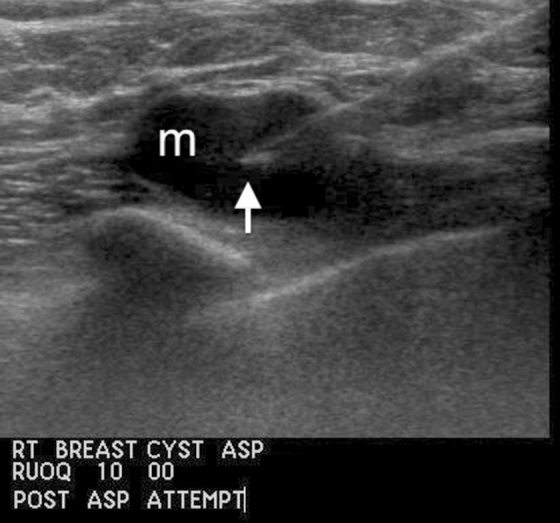
61-year-old female with neurofibroma of the breast. Sonogram of the right breast, showing an aspiration needle (arrow) within the mass (m).
Figure 4.
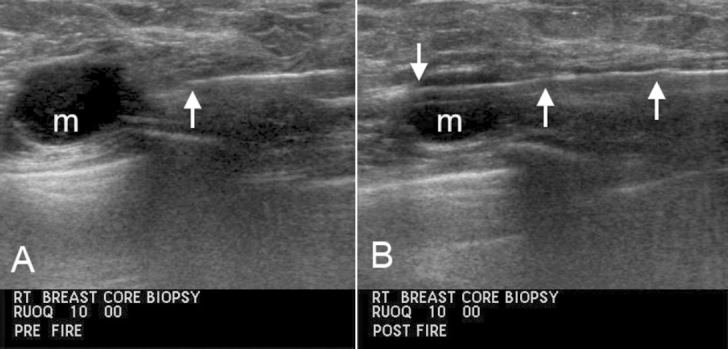
61-year-old female with neurofibroma of the breast. A. Pre-fire core biopsy image. The needle tip (arrow) is within the breast at the leading edge of the mass (m). The mass is clearly seen to be located within the breast, with normal breast parenchyma surrounding the mass. B. Post-fire core biopsy image with the needle (arrows) passing through the mass (m). The needle passes through breast tissue, then through the mass, confirming the location of the mass within the breast.
During core biopsy, the patient experienced significant pain during each pass of the needle through the mass. No pain was elicited while the needle was positioned within the breast tissue surrounding the mass.
The core-biopsy specimens consisted of multiple cylindrical fragments of white, focally hemorrhagic soft tissue, 1.5 cm in aggregate size. Microscopically, the biopsy revealed a circumscribed, moderately cellular spindle-cell neoplasm, abutting a portion of skeletal muscle (Fig. 5).
Figure 5.
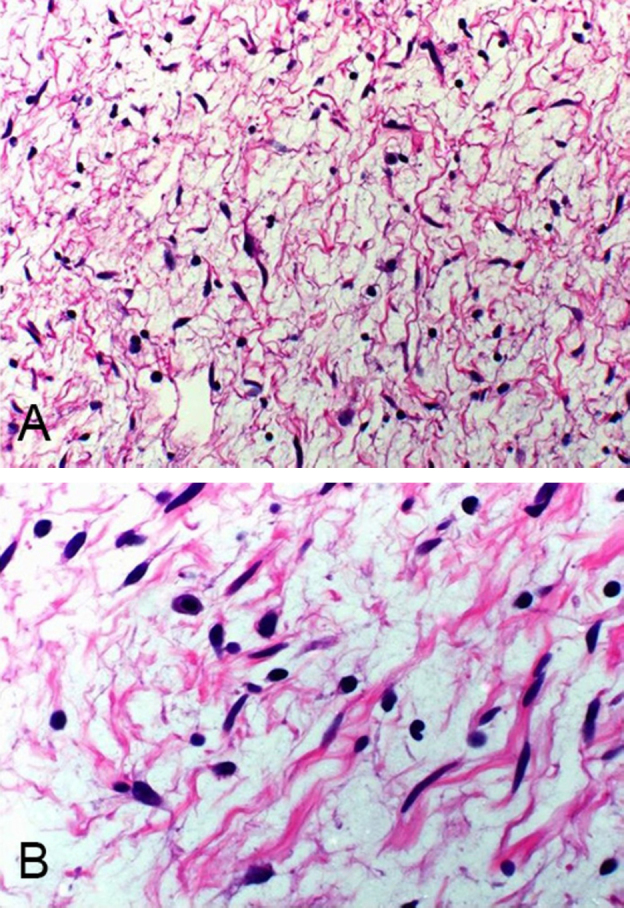
A&B. 61-year-old female with neurofibroma of the breast. A and B. Hematoxylin and eosin stains at intermediate power.
The spindle cells had markedly elongated nuclei with a wavy configuration and pointed ends, many reactive with S-100 protein (Fig. 6). The stroma was myxoid in appearance and contained a network of collagen fibers and mast cells. No mitoses or necrosis were seen, and the mass was confined to the breast tissue. A histologic diagnosis of neurofibroma was made.
Figure 6.
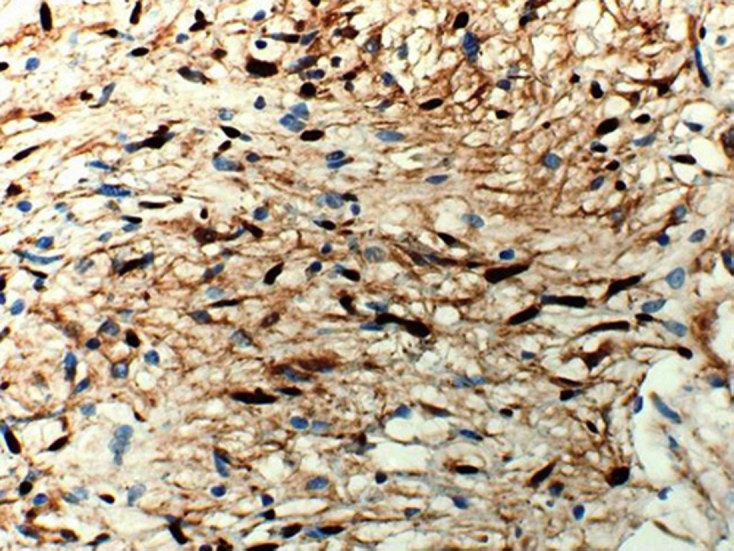
61-year-old female with neurofibroma of the breast. Immunostain at high power, showing many cells reactive with S-100 protein (darker cells).
Discussion
The myxoid stroma of this mass may at least be partially responsible for its sonographic appearance as a hypoechoic lesion with distal acoustic enhancement. These sonographic features resemble those of a cyst, and may be cause for misdiagnosis.
Neurofibromas are benign nerve-sheath tumors that were first described by Smith in 1849 and later by von Recklinghausen in 1882 (1). They are relatively common in both sexes and can occur at any age (2). They are slow-growing, and the majority are painless. Most neurofibromas occur as solitary lesions in the dermis or subcutis, are distributed evenly over the body surface, and occur very rarely in breast tissue (3, 4). Only a few cases of breast neurofibromas have been reported, both in men and women—excluding neurofibromas in the presence of neurofibromatosis (von Recklinghausen’s disease), which is considered a separate disease process (1, 2, 7, 8, 9).
The radiological appearance of neurofibromas is variable and is known to depend on their histopathological characteristics. In general, neurofibromas appear as oval or round lesions with circumscribed margins on both mammography and ultrasound imaging. On ultrasound, they appear as hypoechoic lesions with posterior acoustic enhancement, resembling a cyst, which may cause misdiagnosis. On MRI, they demonstrate high signal intensity on T2-weighted images, especially if the tumor has a myxoid matrix. They may demonstrate either nonenhancement or gradual enhancement following contrast-material injection (10).
Grossly, neurofibromas are white-gray, soft, and well circumscribed but not encapsulated (2, 5). They vary in shape and in size, most measuring between 1 cm and 2 cm (6). However, depending on their location, they can become extremely large and may also be polypoid or fusiform in shape (5). Microscopically, neurofibromas are formed by a combined proliferation of all the elements of a peripheral nerve, Schwann cells being the most predominant (5). Most contain interlacing bundles of cells with elongated, wavy, and dark-staining nuclei with pointed ends and slender cytoplasmic processes (2, 3, 5). These cells are arranged closely and separated by mucoid material. Most are immunoreactive for S-100 protein and, in keeping with their benign behavior, lack significant mitotic activity and necrosis (2, 5).
From a pathological point of view, the main differential diagnosis for this tumor is a schwannoma, which can be differentiated from neurofibroma by the presence of Verocay bodies, Antoni A and B areas, and a more diffuse and uniform S-100 staining pattern. These features were all absent in our case. Other entities that should be considered include fibroadenoma, phyllodes tumor, malignant peripheral nerve sheath tumor, and myofibroblastoma.
Footnotes
Published: November 10, 2012
References
- 1.Sherman JE, Smith JW. Neurofibromas of the breast and nipple areolar area. Ann Plast Surg. 1981;7:302–307. doi: 10.1097/00000637-198110000-00010. [PubMed] [DOI] [PubMed] [Google Scholar]
- 2.Jeyartena DS, Oriolowo A, Smith ME, Watkins RM. Solitary neurofibroma in the male breast. World J Surg Oncol. 2007;5:23. doi: 10.1186/1477-7819-5-23. [PubMed] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weiss SW, Goldblum JR. Benign tumors of peripheral nerves. In: Enzinger, Weiss’s, editors. Soft tissue tumours. 4th ed. Mosby; St. Louis, MO: 2001. pp. 1111–1208. [Google Scholar]
- 4.Fletcher CDM. Diagnostic histopathology of tumours. 2nd ed. Churchill Livingstone; Edinburgh: 2000. Peripheral neuroectodermal tumors; pp. 1679–1711. [Google Scholar]
- 5.Houston M. Rosai and Ackerman’s Surgical pathology. 9th ed. Mosby; Philadelphia, PA: 2004. Neurofibroma; pp. 2266–2269. [Google Scholar]
- 6.Ironside JW, Moss TH, Louis DN, Lowe JS, Weller RO, editors. Diagnostic pathology of nervous system tumours. Churchill Livingston; London: 2002. Neurofibroma; pp. 439–444. [Google Scholar]
- 7.Lakuy D, Petraru DM, Ancar V, Kelemen J. Giant neurofibroma of the pectoral region including the breast. Rom J Morphol Embryol. 1990;36(3-4):213–215. [PubMed] [PubMed] [Google Scholar]
- 8.Narayan AS, Rao KP. Neurofibroma of the breast. J Indian Med Assoc. 1968;50:375–376. [PubMed] [PubMed] [Google Scholar]
- 9.Hock YL, Mohamid W. Myxoid neurofibroma of the male breast: fine needle aspiration cytodiagnosis. Cytopathology. 1995;6:44–47. doi: 10.1111/j.1365-2303.1995.tb00007.x. [PubMed] [DOI] [PubMed] [Google Scholar]
- 10.Gokalp G, Hakyemez B, Kizilkaya E, Haholu A. Myxoid neurofibromas of the breast: mammographical, sonographical and MRI appearances. Br J Radiol. 2007;80(958):e234–e237. doi: 10.1259/bjr/33539044. [PubMed] [DOI] [PubMed] [Google Scholar]


